Libman-Sacks endocarditis: Difference between revisions
Sara Mohsin (talk | contribs) |
Sara Mohsin (talk | contribs) No edit summary |
||
| (181 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Libman-Sacks endocarditis}} | |||
{{CMG}} {{AE}} {{S.M.}} | |||
{{ | |||
{{CMG}} {{AE}}{{S.M.}} | |||
{{SK}} Nonbacterial thrombotic endocarditis (NBTE), Marantic endocarditis, Verrucous endocarditis | {{SK}}: Nonbacterial thrombotic endocarditis (NBTE), Marantic endocarditis, Verrucous endocarditis | ||
==Overview== | ==Overview== | ||
'''Libman-Sacks endocarditis''' is a form of nonbacterial [[endocarditis]] that is seen in [[lupus erythematosus|systemic lupus erythematosus]]. | '''Libman-Sacks endocarditis''' (LSE) is a form of [[nonbacterial thrombotic endocarditis]] ([[Non-bacterial thrombotic endocarditis|NBTE]]) that is considered to be the most [[Common-cause and special-cause|common]] [[cardiac]] manifestation seen in [[patients]] with [[lupus erythematosus|systemic lupus erythematosus]]. LSE is a [[Term logic|term]] [[Usage analysis|used]] for [[sterile]] and verrucous [[Vegetation (pathology)|vegetations]] around the [[heart valves]] mostly [[Affect|affecting]] the [[Mitral valve|mitral]] and [[aortic]] [[heart valves]] but other [[Valves of the heart|valves]] may also be involved. [[Valvular]] involvement in LSE may [[lead]] to [[Valvular heart disease|valvular]] [[regurgitation]], [[aortic insufficiency]], [[Thromboembolic event|thromboembolic]] [[Cerebrovascular event|cerebrovascular events]], and increased [[RiskMetrics|risk]] of [[infective endocarditis]]. It is also usually [[Association (statistics)|associated]] with the other [[autoimmune diseases]] such as [[antiphospholipid syndrome]] ([[Antiphospholipid syndrome|APS]]) and some [[malignancies]]. [[Secondary]] [[Antiphospholipid syndrome|APS]] has a higher [[rate]] of [[cardiac]] involvement as [[Comparability|compared]] to primary [[Antiphospholipid syndrome|APS]], mostly due to the [[autoimmune]] [[causes]] [[Related changes|related]] to the [[SLE]]. LSE can be [[Complication (medicine)|complicated]] by [[embolic]] [[cerebrovascular disease]], superimposed [[infective endocarditis]], and [[Peripheral Arterial Disease|peripheral]] [[arterial embolism]]. It is also [[Association (statistics)|associated]] with increased [[mortality]], hence, early [[Recognition sequence|recognition]] of LSE and [[Appropriate Use Criteria|appropriate]] [[Treatment groups|treatment]] are of [[Significant figure|significant]] [[Importance sampling|importance]] in [[Prevention (medical)|preventing]] any further [[complications]]. | ||
==Historical Perspective== | ==Historical Perspective== | ||
*In 1924, the two American [[Physician|physicians]] Emanuel Libman, and Benjamin Sacks, working at [[Mount Sinai Hospital, New York]], [[Description logic|described]] the Libman-Sacks [[endocarditis]] for the first [[Time constant|time]], hence, it's named after them. They first [[Presenting symptom|presented]] the complete [[clinical]] [[Picture thinking|picture]] of it with or without [[skin lesions]] and [[Description logic|described]] it as unusual [[Nonbacterial thrombotic endocarditis|non-bacterial endocarditis]] with verrucous [[Vegetation (pathology)|vegetations]] adherent to the [[endocardium]]. <ref>Libman E, Sacks B: A hitherto undescribed form of valvular and mural endocarditis. Arch Intern Med 1924; 33: 701-37.</ref><ref name="Libman1924">{{cite journal|last1=Libman|first1=Emanuel|title=A HITHERTO UNDESCRIBED FORM OF VALVULAR AND MURAL ENDOCARDITIS|journal=Archives of Internal Medicine|volume=33|issue=6|year=1924|pages=701|issn=0003-9926|doi=10.1001/archinte.1924.00110300044002}}</ref> | *In 1888, Zeigler was the first one to [[Description logic|describe]] [[Non-bacterial thrombotic endocarditis|NBTE]], and called it "thromboendocarditis" at that [[Time constant|time]]. | ||
*In 1924, the two American [[Physician|physicians]] Emanuel Libman, and Benjamin Sacks, working at [[Mount Sinai Hospital, New York]], [[Description logic|described]] the Libman-Sacks [[endocarditis]] for the first [[Time constant|time]], hence, it's named after them. They first [[Presenting symptom|presented]] the complete [[clinical]] [[Picture thinking|picture]] of it with or without [[skin lesions]] and [[Description logic|described]] it as unusual [[Nonbacterial thrombotic endocarditis|non-bacterial endocarditis]] with verrucous [[Vegetation (pathology)|vegetations]] adherent to the [[endocardium]].<ref>Libman E, Sacks B: A hitherto undescribed form of valvular and mural endocarditis. Arch Intern Med 1924; 33: 701-37.</ref><ref name="Libman1924">{{cite journal|last1=Libman|first1=Emanuel|title=A HITHERTO UNDESCRIBED FORM OF VALVULAR AND MURAL ENDOCARDITIS|journal=Archives of Internal Medicine|volume=33|issue=6|year=1924|pages=701|issn=0003-9926|doi=10.1001/archinte.1924.00110300044002}}</ref> | |||
*In 1936, Gross and Friedberg finally coined the [[Term logic|term]] "[[Non-bacterial thrombotic endocarditis|nonbacterial thrombotic endocarditis]]" ([[Non-bacterial thrombotic endocarditis|NBTE]]) for [[Marantic endocarditis|marantic]]/verrucous [[endocarditis]]. | |||
*In 1983, Graham [[Hughes syndrome|Hughes]] [[Description logic|described]] the [[antiphospholipid antibody syndrome]] for the first [[Time series|time]] while [[Working area|working]] as a [[rheumatologist]] at St Thomas [[Hospital]]. He named it [[anticardiolipin syndrome]] (also known as [[Hughes syndrome]] named after him) and [[Description logic|described]] it has the following three [[Characteristic function (probability theory)|characteristics]]:<ref>https://patient.info/doctor/libman-sacks-endocarditis#ref-14</ref> | *In 1983, Graham [[Hughes syndrome|Hughes]] [[Description logic|described]] the [[antiphospholipid antibody syndrome]] for the first [[Time series|time]] while [[Working area|working]] as a [[rheumatologist]] at St Thomas [[Hospital]]. He named it [[anticardiolipin syndrome]] (also known as [[Hughes syndrome]] named after him) and [[Description logic|described]] it has the following three [[Characteristic function (probability theory)|characteristics]]:<ref>https://patient.info/doctor/libman-sacks-endocarditis#ref-14</ref> | ||
**[[Venous]] and/or [[arterial thrombosis]] | **[[Venous]] and/or [[arterial thrombosis]] | ||
| Line 28: | Line 17: | ||
**[[Presenting symptom|Presence]] of [[antiphospholipid antibodies]] | **[[Presenting symptom|Presence]] of [[antiphospholipid antibodies]] | ||
*In 1985, the [[Association (statistics)|association]] between Libman-Sacks [[endocarditis]] and [[antiphospholipid antibody syndrome]] was noted for the first time. | *In 1985, the [[Association (statistics)|association]] between Libman-Sacks [[endocarditis]] and [[antiphospholipid antibody syndrome]] was noted for the first time. | ||
*In 1989, four [[Group (sociology)|groups]] highlighted a [[Probability|probable]] role of [[antiphospholipid antibodies]] in the [[pathogenesis]] of [[valvular heart disease]] in [[SLE]] [[patients]]. | |||
==Pathophysiology== | ==Pathophysiology== | ||
*The | ===Pathology=== | ||
*The [[pathology]] of Libman-Sacks [[endocarditis]] is the same as [[Non-bacterial thrombotic endocarditis|nonbacterial thrombotic endocarditis]] except that focal [[necrosis]] (seen in the form of [[hematoxylin]] [[Body|bodies]]) is only found in Libman-Sacks [[endocarditis]]. | |||
* Just like [[Non-bacterial thrombotic endocarditis|NBTE]], Libman-Sacks [[endocarditis]] [[Development (biology)|develops]] due to the [[endothelial]] damage and subsequent [[Exposure effect|exposure]] of the sub-[[endothelial]] [[connective tissue]] to the [[Circulation|circulating]] [[platelets]]. | |||
*The factors involved in the [[pathogenesis]] can be [[Division (biology)|divided]] into the ones [[Initiation factors|initiating]] the Libman-Sacks [[endocarditis]] and the subsequent [[Development (biology)|development]] of [[Vegetation (pathology)|vegetations]].<ref>https://www.pathologyoutlines.com/topic/heartnontumornoninfecendo.html</ref> | |||
{| class="wikitable" | |||
|+Factors responsible for the initiation of Libman-Sacks endocarditis | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Initiation factor}} | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Description}} | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Immune complexes]]''' | |||
| | |||
* Libman-Sacks [[endocarditis]] is especially a prototype. | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Hypoxia]]''' | |||
| | |||
* It was [[Study arms|studied]] by Nakanishi et al to be one of the factors in a [[rodent]] [[model]]. | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Hypercoagulability]]''' | |||
| | |||
* Trousseau was the first one to note the [[Association (statistics)|association]] between [[thrombosis]] and [[malignancy]]. | |||
===Pathology=== | *[[Histological]] [[evidence]] of [[disseminated intravascular coagulation]] ([[Disseminated intravascular coagulation|DIC]]) is also found in the 50% of [[patients]] with [[Non-bacterial thrombotic endocarditis|NBTE]]. | ||
* | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Carcinomatosis]]''' | |||
|Following [[carcinomas]] are commonly [[Association (statistics)|associated]] with [[Non-bacterial thrombotic endocarditis|NBTE]] and Libman-Sacks [[endocarditis]]: | |||
*[[Mucin]] [[Product (biology)|producing]] [[adenocarcinomas]] of: | |||
**[[Gastrointestinal tract|GIT]] | |||
**[[Ovaries]] | |||
**[[Lungs]] | |||
*[[Acute promyelocytic leukemia]] | |||
|} | |||
* The [[Vegetation (pathology)|vegetations]] in Libman-Sacks [[endocarditis]] are formed from the strands consisting of the following four components: | |||
**[[Fibrin]] | |||
**[[Neutrophils]] | |||
**[[Lymphocytes]] | |||
**[[Histiocyte]]s | |||
*Most commonly [[Affect|affected]] [[valve]] is the [[mitral valve]] with the [[Vegetation (pathology)|vegetations]] involving the [[ventricular]] and [[atrial]] [[Surface area|surface]] of the [[valve]]. | |||
*The [[lesions]] of Libman-Sacks [[endocarditis]] [[Rare|rarely]] [[lead]] to any [[Significant figure|significant]] [[valvular dysfunction]] and they only [[Rare|rarely]] [[Embolisation|embolize]].<ref name="pmid31558998">{{cite journal| author=Mohammadi Kebar Y, Avesta L, Habibzadeh A, Hemmati M| title=Libman-Sacks endocarditis in patients with systemic lupus erythematosus with secondary antiphospholipid syndrome. | journal=Caspian J Intern Med | year= 2019 | volume= 10 | issue= 3 | pages= 339-342 | pmid=31558998 | doi=10.22088/cjim.10.3.339 | pmc=6729157 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31558998 }} </ref><ref name="pmid28515823">{{cite journal| author=Murtaza G, Iskandar J, Humphrey T, Adhikari S, Kuruvilla A| title=Lupus-Negative Libman-Sacks Endocarditis Complicated by Catastrophic Antiphospholipid Syndrome. | journal=Cardiol Res | year= 2017 | volume= 8 | issue= 2 | pages= 57-62 | pmid=28515823 | doi=10.14740/cr534e | pmc=5421487 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28515823 }} </ref><ref name="pmid20331896">{{cite journal| author=Bouma W, Klinkenberg TJ, van der Horst IC, Wijdh-den Hamer IJ, Erasmus ME, Bijl M et al.| title=Mitral valve surgery for mitral regurgitation caused by Libman-Sacks endocarditis: a report of four cases and a systematic review of the literature. | journal=J Cardiothorac Surg | year= 2010 | volume= 5 | issue= | pages= 13 | pmid=20331896 | doi=10.1186/1749-8090-5-13 | pmc=2859362 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20331896 }} </ref><ref name="pmid26152222">{{cite journal| author=Bai Z, Hou J, Ren W, Guo Y| title=Diagnosis and surgical treatment for isolated tricuspid Libman-Sacks endocarditis: a rare case report and literatures review. | journal=J Cardiothorac Surg | year= 2015 | volume= 10 | issue= | pages= 93 | pmid=26152222 | doi=10.1186/s13019-015-0302-1 | pmc=4494164 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26152222 }} </ref><ref name="pmid30422459">{{cite journal| author=| title=StatPearls | journal= | year= 2019 | volume= | issue= | pages= | pmid=30422459 | doi= | pmc= | url= }} </ref><ref name="pmid24925796">{{cite journal| author=Wang Y, Ma C, Yang J, Liu S, Zhang Y, Zhao L et al.| title=Libman-sacks endocarditis exclusively involving the tricuspid valve in a patient with systemic lupus erythematosus. | journal=J Clin Ultrasound | year= 2015 | volume= 43 | issue= 4 | pages= 265-267 | pmid=24925796 | doi=10.1002/jcu.22180 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24925796 }} </ref><ref name="pmid21404907">{{cite journal| author=Perier P, Jeserich M, Vieth M, Pohle K, Hohenberger W, Diegeler A| title=Mitral valve reconstruction in a patient with Libman-Sacks endocarditis: a case report. | journal=J Heart Valve Dis | year= 2011 | volume= 20 | issue= 1 | pages= 103-6 | pmid=21404907 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21404907 }} </ref><ref name="pmid28054901">{{cite journal| author=Bani Hani A, Abu-Abeeleh M, Al Kharabsheh MM, Qabba'ah L| title=Libman-Sacks Endocarditis with Unusual Large Size Vegetation Involving the Mitral Valve. | journal=Heart Surg Forum | year= 2016 | volume= 19 | issue= 6 | pages= E294-E296 | pmid=28054901 | doi=10.1532/hsf.1612 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28054901 }} </ref> | |||
===Gross pathology=== | |||
*[[Vegetation (pathology)|Vegetations]] in Libman-Sacks [[endocarditis]] have the following [[Typical set|typical]] [[Features (pattern recognition)|features]]: | |||
**Small | |||
**Friable | |||
**[[White (mutation)|White]] or tan [[Mass|masses]] | |||
**< 1 [[Centimeter|cm]] in [[diameter]] | |||
**[[Irregular lesion|Irregular]] | |||
**Broad [[Base|based]] | |||
**Usually involve the [[Line|lines]] along the [[valve]] [[Closure (psychology)|closure]] on leaflets (which may be [[normal]] or previously damaged) | |||
**Vary from tiny [[lesions]] to [[Large-print|large]], exuberant [[Mass|masses]] | |||
{| class="wikitable" | |||
|+Allen and Sirota macroscopic classification of NBTE | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Type of NBTE}} | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Features}} | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Type 1 | |||
| | |||
* Small | |||
* < 3 [[Millimeter|mm]] | |||
* Univerrucal | |||
* Firmly attached to the valve | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Type 2 | |||
| | |||
*[[Large-print|Large]] | |||
* > 3 [[Millimeter|mm]] | |||
* Univerrucal | |||
*[[Adhesion|Adherent]] to the [[valve]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Type 3 | |||
| | |||
* Small | |||
* 1 - 3 [[Millimeter|mm]] | |||
* Multiverrucal | |||
* Friable | |||
|} | |||
{| | |||
| | |||
[[File:Libman-Sacks-Endocarditis-The-presence-of-vegetations-predisposes-patients-to-bacterial.png|thumb|550px|none|Libman Sacks Endocarditis. The presence of vegetations predisposes patients to bacterial endocarditis. [https://www.researchgate.net/figure/Libman-Sacks-Endocarditis-The-presence-of-vegetations-predisposes-patients-to-bacterial_fig3_221929537 Source: Brigden et al,1960.]]] | |||
| | |||
[[File:Libman-sacks-endocarditis.jpg|thumb|250px|none|Libman-Sacks endocarditis. [http://medical-dictionary.thefreedictionary.com/_/viewer.aspx?path=MosbyMD&name=libman-sacks-endocarditis.jpg&url=http%3A%2F%2Fmedical-dictionary.thefreedictionary.com%2FLibman-Sacks%2Bendocarditis Source: Kumar et al, 2010/Courtesy Dr. Fred Schoen, Department of Pathology, Brigham and Women's Hospital]]] | |||
| | |||
|} | |||
===Microscopic Pathology=== | |||
*[[Vegetation (pathology)|Vegetations]] in Libman-Sacks [[endocarditis]] consist of [[Degeneration|degenerating]] [[platelets]] interwoven with the [[fibrin strands]] and form a bland, featureless [[eosinophilic]] [[mass]] except for a few trapped [[leukocytes]]. | |||
*Following three [[Stages of human development|stages]] have been [[Description logic|described]] in the [[Evolution (disambiguation)|evolution]] of [[Vegetation (pathology)|vegetations]] in Libman-Sacks [[endocarditis]]:<ref>https://emedicine.medscape.com/article/155230-workup#showall</ref> | |||
{| class="wikitable" | |||
|+ | |||
Stages of evolution of vegetations in Libman-Sacks endocarditis | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Stage}} | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Description}} | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Stages of human development|Stage]] 1 ([[Active Living|active]] [[verrucae]]) | |||
| | |||
* Consists of [[fibrin]] clumps on and within the [[valvular]] leaflet [[tissue]] (focally [[necrotic]]), along with [[plasma cells]] and [[lymphocytes]]. | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Stages of human development|Stage]] 2 ([[Combination reaction|Combined]] [[Active Living|active]] and [[Healing|healed]] [[lesions]]) | |||
| | |||
* Contains [[fibrous]], [[Vascularity|vascularized]] [[tissue]] adjacent to [[necrotic]] and [[fibrinous]] [[Area|areas]]. | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Stages of human development|Stage]] 3 ([[Healing|Healed]] [[lesions]]) | |||
| | |||
* Consists of [[dense]], [[fibrous]], and [[Vascularity|vascularized]] [[tissue]]. | |||
|} | |||
{| | |||
| | |||
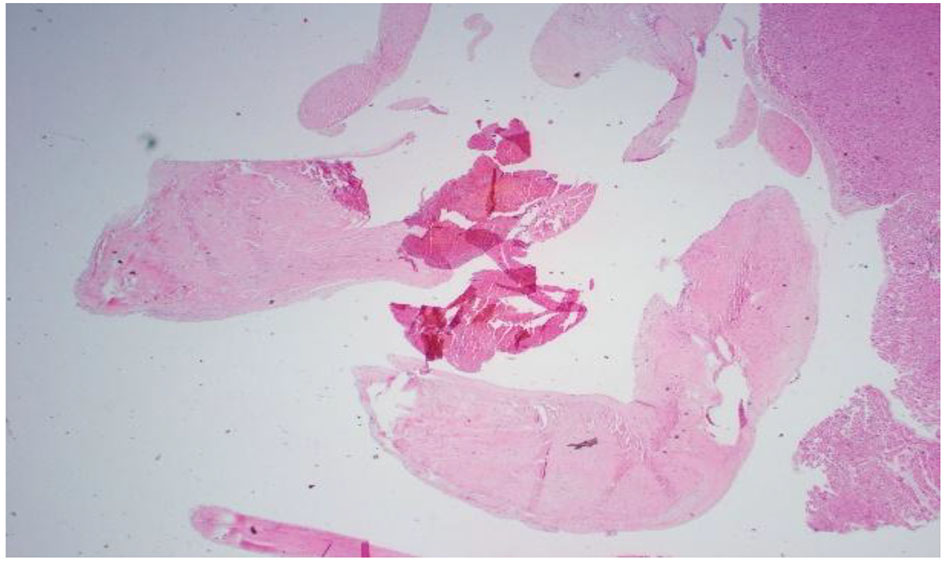
[[File:Cr534e-g004.jpg|thumb|200px|none|Pathology slide of mitral valve vegetation. Lots of necrosis: 10 cm circumference vegetation. Mitral valve tissue shows focal necrosis. No bacterial or fungal organisms were present. [https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
| | |||
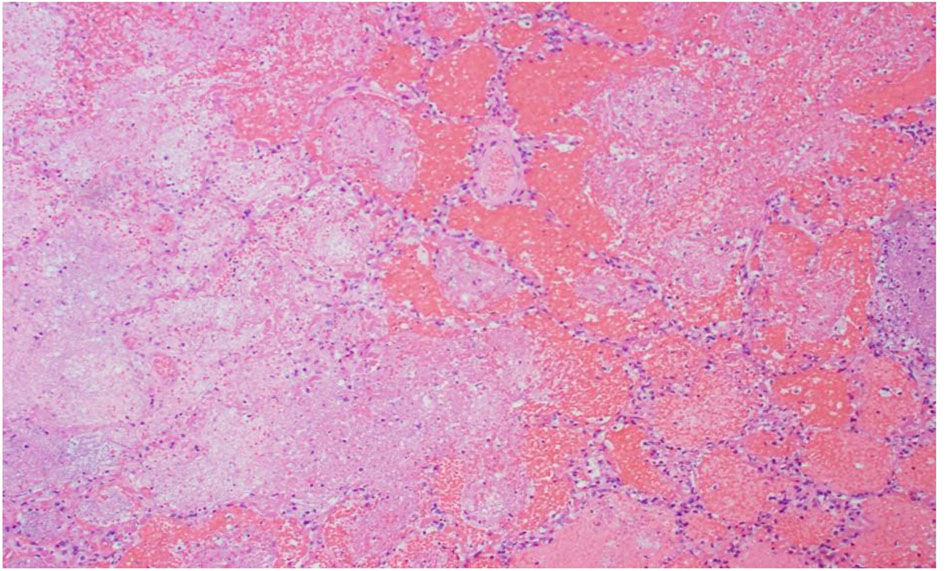
[[File:Cr534e-g005.jpg|thumb|200px|none|R lung, high power: emboli and large necrotic infarcted tissue. [https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
| | |||
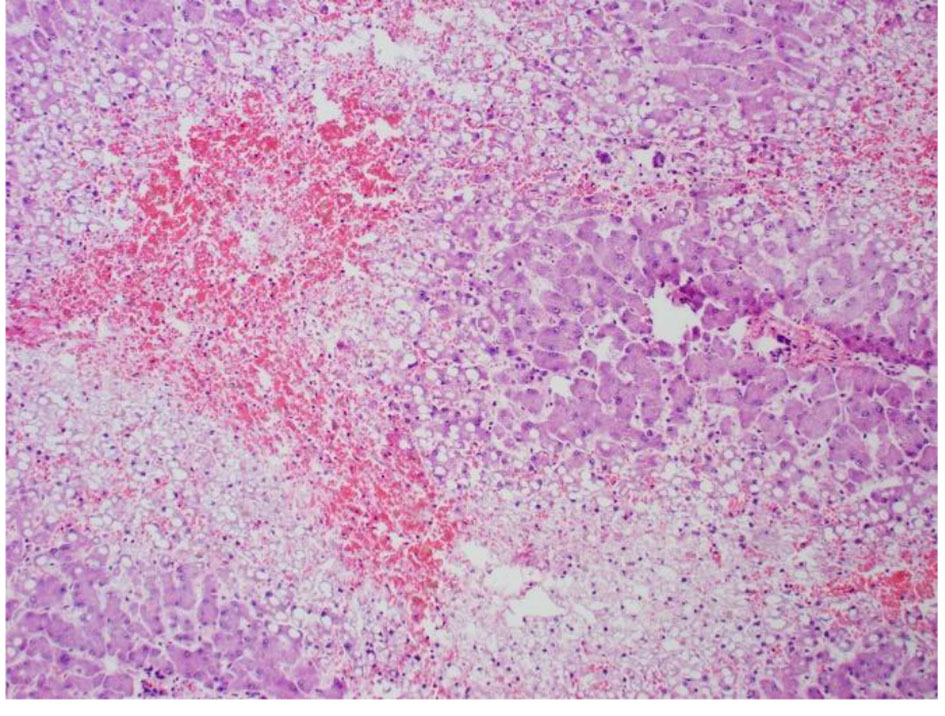
[[File:Cr534e-g006.jpg|thumb|200px|none|Low power of the liver: lots of steatosis and congestion, necrosis. [https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
| | |||
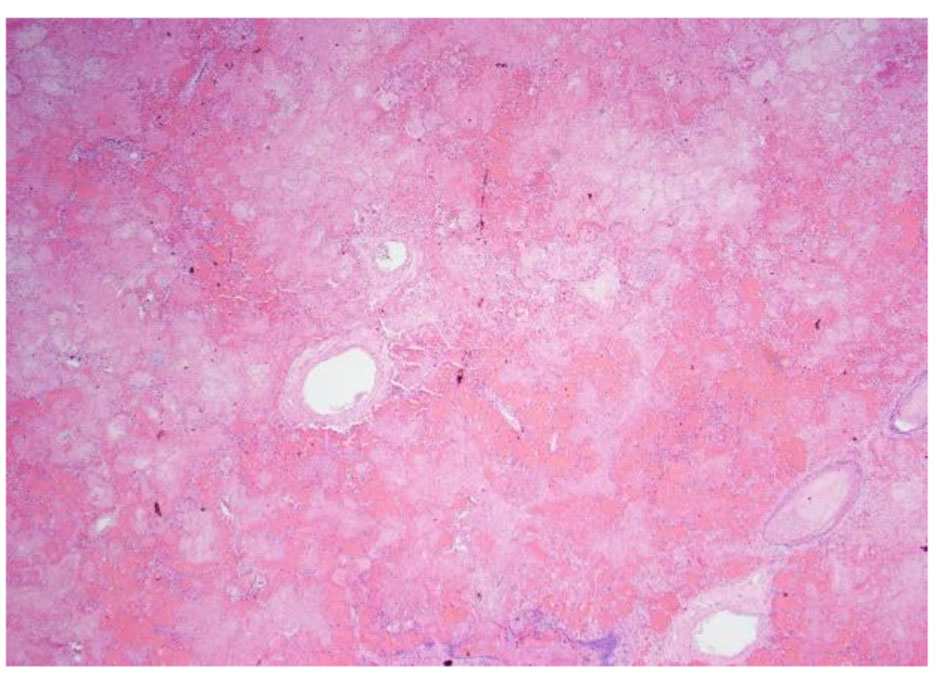
[[File:Cr534e-g007.jpg|thumb|200px|none|High power pathology slide of the liver showing lots of steatosis, congestion, and necrosis. [https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
| | |||
[[File:Cr534e-g008.jpg|thumb|200px|none|Low power pathology slide of the lung showing emboli and necrotic tissue.[https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
|} | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
*Approximately 1 out of 10 [[SLE]] [[patients]] have [[Vegetation (pathology)|vegetations]] [[Association (statistics)|associated]] with Libman-Sacks [[endocarditis]].[[Presenting symptom|Presence]] of these [[Vegetation (pathology)|vegetations]] is [[Indicative conditional|indicative]] of the [[Association (statistics)|association]] with the following:<ref>https://patient.info/doctor/libman-sacks-endocarditis#ref-14</ref> | *Approximately 1 out of 10 [[SLE]] [[patients]] have [[Vegetation (pathology)|vegetations]] [[Association (statistics)|associated]] with Libman-Sacks [[endocarditis]]. [[Presenting symptom|Presence]] of these [[Vegetation (pathology)|vegetations]] is [[Indicative conditional|indicative]] of the [[Association (statistics)|association]] with the following:<ref>https://patient.info/doctor/libman-sacks-endocarditis#ref-14</ref><ref name="pmid17602939">{{cite journal| author=Moyssakis I, Tektonidou MG, Vasilliou VA, Samarkos M, Votteas V, Moutsopoulos HM| title=Libman-Sacks endocarditis in systemic lupus erythematosus: prevalence, associations, and evolution. | journal=Am J Med | year= 2007 | volume= 120 | issue= 7 | pages= 636-42 | pmid=17602939 | doi=10.1016/j.amjmed.2007.01.024 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17602939 }} </ref> | ||
**[[Systemic lupus erythematosus|Lupus]] duration | **[[Systemic lupus erythematosus|Lupus]] duration | ||
**[[Disease]] [[Activity (chemistry)|activity]] | **[[Disease]] [[Activity (chemistry)|activity]] | ||
| Line 49: | Line 158: | ||
*These [[positive]] findings are five to nine [[Timespan|times]] more [[Frequentism|frequently]] found in [[Womens Pack|women]] than [[men]]. | *These [[positive]] findings are five to nine [[Timespan|times]] more [[Frequentism|frequently]] found in [[Womens Pack|women]] than [[men]]. | ||
*Libman-sacks [[endocarditis]] typically occurs in [[Young adult|young]] [[Womens Pack|women]], however, [[children]] can be [[Rare|rarely]] involved. | *Libman-sacks [[endocarditis]] typically occurs in [[Young adult|young]] [[Womens Pack|women]], however, [[children]] can be [[Rare|rarely]] involved. | ||
*[[Non-bacterial thrombotic endocarditis|Nonbacterial thrombotic endocarditis]] ([[Non-bacterial thrombotic endocarditis|NBTE]]) is a [[rare]] [[condition]] most often found [[Postmortem studies|postmortem]] | *[[Non-bacterial thrombotic endocarditis|Nonbacterial thrombotic endocarditis]] ([[Non-bacterial thrombotic endocarditis|NBTE]]) is a [[rare]] [[condition]] which is most often found during 0.9% to 1.6% of the [[Postmortem studies|postmortem]] [[Study design|studies]].<ref name="pmid998478">{{cite journal| author=Deppisch LM, Fayemi AO| title=Non-bacterial thrombotic endocarditis: clinicopathologic correlations. | journal=Am Heart J | year= 1976 | volume= 92 | issue= 6 | pages= 723-9 | pmid=998478 | doi=10.1016/s0002-8703(76)80008-7 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=998478 }} </ref><ref name="pmid4682494">{{cite journal| author=Rosen P, Armstrong D| title=Nonbacterial thrombotic endocarditis in patients with malignant neoplastic diseases. | journal=Am J Med | year= 1973 | volume= 54 | issue= 1 | pages= 23-9 | pmid=4682494 | doi=10.1016/0002-9343(73)90079-x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4682494 }} </ref><ref name="pmid17535760">{{cite journal| author=Llenas-García J, Guerra-Vales JM, Montes-Moreno S, López-Ríos F, Castelbón-Fernández FJ, Chimeno-García J| title=[Nonbacterial thrombotic endocarditis: clinicopathologic study of a necropsy series]. | journal=Rev Esp Cardiol | year= 2007 | volume= 60 | issue= 5 | pages= 493-500 | pmid=17535760 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17535760 }} </ref><ref name="pmid11761501">{{cite journal| author=Eiken PW, Edwards WD, Tazelaar HD, McBane RD, Zehr KJ| title=Surgical pathology of nonbacterial thrombotic endocarditis in 30 patients, 1985-2000. | journal=Mayo Clin Proc | year= 2001 | volume= 76 | issue= 12 | pages= 1204-12 | pmid=11761501 | doi=10.4065/76.12.1204 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11761501 }} </ref><ref name="pmid20397972">{{cite journal| author=Mazokopakis EE, Syros PK, Starakis IK| title=Nonbacterial thrombotic endocarditis (marantic endocarditis) in cancer patients. | journal=Cardiovasc Hematol Disord Drug Targets | year= 2010 | volume= 10 | issue= 2 | pages= 84-6 | pmid=20397972 | doi=10.2174/187152910791292484 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20397972 }} </ref><ref name="pmid3548296">{{cite journal| author=Lopez JA, Ross RS, Fishbein MC, Siegel RJ| title=Nonbacterial thrombotic endocarditis: a review. | journal=Am Heart J | year= 1987 | volume= 113 | issue= 3 | pages= 773-84 | pmid=3548296 | doi=10.1016/0002-8703(87)90719-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3548296 }} </ref> | ||
*[[Non-bacterial thrombotic endocarditis|NBTE]] [[Affect|affects]] every [[age]] [[Group (sociology)|group]] but most commonly involves [[patients]] between the [[Fourth period|fourth]] and eighth decades of [[life]] with no [[Sex (activity)|sex]] predilection.<ref name="pmid17522239">{{cite journal| author=el-Shami K, Griffiths E, Streiff M| title=Nonbacterial thrombotic endocarditis in cancer patients: pathogenesis, diagnosis, and treatment. | journal=Oncologist | year= 2007 | volume= 12 | issue= 5 | pages= 518-23 | pmid=17522239 | doi=10.1634/theoncologist.12-5-518 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17522239 }} </ref> | |||
*[[Non-bacterial thrombotic endocarditis|NBTE]] most commonly [[Affect|affects]] [[patients]] with [[systemic lupus erythematosus]] and advanced [[malignancy]]. | |||
*According to one [[autopsy]] [[Study arms|study]], [[patients]] with [[Underlying representation|underlying]] [[malignancy]] have a higher [[rate]] (1.25%) of [[Non-bacterial thrombotic endocarditis|NBTE]] as [[Comparability|compared]] to [[Generalization|general]] [[population]] (0.2%).<ref name="pmid1851590">{{cite journal| author=González Quintela A, Candela MJ, Vidal C, Román J, Aramburo P| title=Non-bacterial thrombotic endocarditis in cancer patients. | journal=Acta Cardiol | year= 1991 | volume= 46 | issue= 1 | pages= 1-9 | pmid=1851590 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1851590 }} </ref> | |||
*[[Non-bacterial thrombotic endocarditis|NBTE]] is found at higher [[rates]] in [[patients]] with [[adenocarcinoma]] ([[Example 1|e.g]]., [[lung]], [[Colon (anatomy)|colon]], [[ovary]], [[biliary]] and [[prostate]]) (2.7%) as [[Comparability|compared]] to other [[malignancies]] (0.47%), with the highest [[rates]] [[Observation|observed]] in [[patients]] with [[mucin]]-[[Secrete|secreting]] and [[pancreatic adenocarcinoma]] (10%).<ref name="pmid1851590">{{cite journal| author=González Quintela A, Candela MJ, Vidal C, Román J, Aramburo P| title=Non-bacterial thrombotic endocarditis in cancer patients. | journal=Acta Cardiol | year= 1991 | volume= 46 | issue= 1 | pages= 1-9 | pmid=1851590 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1851590 }} </ref><ref name="pmid15919332">{{cite journal| author=Borowski A, Ghodsizad A, Cohnen M, Gams E| title=Recurrent embolism in the course of marantic endocarditis. | journal=Ann Thorac Surg | year= 2005 | volume= 79 | issue= 6 | pages= 2145-7 | pmid=15919332 | doi=10.1016/j.athoracsur.2003.12.024 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15919332 }} </ref> | |||
*[[Observational studies]] in [[patients]] with [[systemic lupus erythematosus]] have [[Reporting results|reported]] 6% to 11% [[prevalence]] [[rates]] with [[transthoracic echocardiography]], with higher [[rates]] (43%) [[Observation|observed]] with more [[Sensitivity|sensitive]] [[Transesophageal echocardiography (TEE)|transesophageal echocardiography]].<ref name="pmid8875919">{{cite journal| author=Roldan CA, Shively BK, Crawford MH| title=An echocardiographic study of valvular heart disease associated with systemic lupus erythematosus. | journal=N Engl J Med | year= 1996 | volume= 335 | issue= 19 | pages= 1424-30 | pmid=8875919 | doi=10.1056/NEJM199611073351903 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8875919 }} </ref><ref name="pmid18085739">{{cite journal| author=Roldan CA, Qualls CR, Sopko KS, Sibbitt WL| title=Transthoracic versus transesophageal echocardiography for detection of Libman-Sacks endocarditis: a randomized controlled study. | journal=J Rheumatol | year= 2008 | volume= 35 | issue= 2 | pages= 224-9 | pmid=18085739 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18085739 }} </ref> | |||
==Risk Factors== | |||
*Following table shows important [[risk factors]] for the [[Development (biology)|development]] of Libman-Sacks [[endocarditis]]: | |||
{| class="wikitable" | |||
|+Risk factors for the development of Libman-Sacks endocarditis | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Risk factor}} | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Details}} | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Advanced [[Stages of human development|stage]] [[malignancy]] | |||
|Advanced [[Stages of human development|stage]] [[malignancies]] such as: | |||
*[[Solid]] [[Organ (anatomy)|organ]] [[malignancy]] | |||
*[[Hematological malignancy]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Chronic (medicine)|Chronic]] [[diseases]] | |||
|[[Chronic (medicine)|Chronic]] [[diseases]] such as: | |||
* | *[[Tuberculosis]] | ||
*[[AIDS]] | |||
* | *[[Uremia]] | ||
|- | |||
* | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Connective tissue disorders]] with [[hypercoagulable state]] | ||
| | |||
*[[SLE]] [[patients]] who are [[positive]] for [[antiphospholipid antibodies]]. | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Trauma]] | |||
|[[Trauma]] due to: | |||
* Indwelling [[pulmonary]] [[catheter]] | |||
*[[Central venous catheter]] | |||
*[[Late effect]] of [[radiation therapy]] | |||
*[[Snake bite]] | |||
|} | |||
==Natural History, Complications and Prognosis== | ==Natural History, Complications and Prognosis== | ||
===Complications=== | ===Complications=== | ||
*Systemic emboli may occur but | *[[Systemic embolization|Systemic emboli]] may occur in Libman-Sacks [[endocarditis]] but not very commonly with the [[RiskMetrics|risk]] being much higher with [[mitral stenosis]] and subsequent [[atrial fibrillation]]. | ||
*It is difficult to [[Prediction|predict]] the [[Underlying representation|underlying]] [[etiology]] in case of a [[stroke]] occurrence in LSE, whether it is due to [[Systemic embolization|systemic emboli]] or the [[Underlying representation|underlying]] [[pathology]] of [[SLE]] or [[Antiphospholipid syndrome|APS]]. | |||
* | *[[Valvular disease]] in LSE can [[lead]] to the [[heart failure]]. | ||
*Valvular disease can lead to heart failure. | *Double-[[Valvular heart disease|valve]] Libman-Sacks [[endocarditis]] involving both [[Mitral valve|mitral]] and [[aortic valves]] can [[lead]] to [[ventricular fibrillation]] and [[cardiac arrest]].<ref name="pmid21720477">{{cite journal| author=Tanawuttiwat T, Dia M, Hanif T, Mihailescu M| title=Double-valve Libman-Sacks endocarditis causing ventricular fibrillation cardiac arrest. | journal=Tex Heart Inst J | year= 2011 | volume= 38 | issue= 3 | pages= 295-7 | pmid=21720477 | doi= | pmc=3113142 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21720477 }} </ref> | ||
* | *There's 1% to 2% [[chance]] of [[congenital heart block]] (usually [[Complete heart block|complete]],or [[First degree heart block|1st]] or [[2nd degree heart block|2nd degree]]) in a [[baby]] of mother with [[SLE]] [[Association (statistics)|associated]] with anti-Ro/SS-A ([[Sjögren's syndrome]] [[antigen]] A) [[autoantibodies]] with a 16% [[Recurrence plot|recurrence]] [[rate]]. [[Fluorinated]] [[steroids]] that do not cross the [[placenta]] may be beneficial in [[Prevention|preventing]] the [[congenital heart block]]. | ||
===Prognosis=== | ===Prognosis=== | ||
*All the SLE patients have a shorter life span. | *All of the [[SLE]] [[patients]] have got a shorter [[life span]]. | ||
*The major cause of mortality in SLE patients | *The occurrence of [[cardiovascular]] [[Event generator|events]] is the major [[Causes|cause]] of [[mortality]] in [[SLE]] [[patients]] as [[SLE]] is a [[risk factor]] for [[premature]] & accelerated [[coronary atherosclerosis]] and [[CAD]] ([[coronary artery disease]]) due to the following [[Association (statistics)|associated]] [[Factor Analysis|factors]]: | ||
**Hypertension | **[[Hypertension]] | ||
**Hyperlipidemia | **[[Hyperlipidemia]] | ||
**Chronic inflammation | **[[Chronic inflammation]] | ||
**Chronic glucocorticoids use | **[[Chronic (medicine)|Chronic]] [[glucocorticoids]] [[Usage analysis|use]] | ||
==Diagnosis== | |||
*[[Diagnosis]] of Libman-Sacks [[endocarditis]] requires a high [[Degree (angle)|degree]] of [[clinical]] suspicion especially in [[patients]] who don't [[Improving agent|improve]] [[Clinical|clinically]] after being [[Treatment Planning|treated]] for [[infective endocarditis]].<ref name="pmid18421506">{{cite journal| author=Ménard GE| title=Establishing the diagnosis of Libman-Sacks endocarditis in systemic lupus erythematosus. | journal=J Gen Intern Med | year= 2008 | volume= 23 | issue= 6 | pages= 883-6 | pmid=18421506 | doi=10.1007/s11606-008-0627-8 | pmc=2517866 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18421506 }} </ref> | |||
*Mckay and Wahler [[Proposition|proposed]] the following [[Triad (anatomy)|triad]] for the [[diagnosis]] of [[Non-bacterial thrombotic endocarditis|NBTE]]: | |||
{| class="wikitable" | |||
|+ | |||
| colspan="2" style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Mckay and Wahler triad for diagnosis of NBTE}} | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |1: | |||
| | |||
*[[Presenting symptom|Presence]] of a [[disease]] [[Process (anatomy)|process]] known to be [[Association (statistics)|associated]] with [[Non-bacterial thrombotic endocarditis|NBTE]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |2: | |||
| | |||
*[[Presenting symptom|Presence]] of [[heart murmur]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |3: | |||
| | |||
*[[Evidence]] of multiple [[Systemic embolization|systemic emboli]] | |||
|} | |||
==History and Symptoms== | |||
*Mostly [[patients]] with Libman-Sacks [[endocarditis]] are [[asymptomatic]]. | |||
*There may be the [[Features (pattern recognition)|features]] of [[valvular disease]] if [[valves]] are severely [[Affect|affected]] with the [[mitral valve disease]] being more common than the [[aortic valve disease]]. | |||
*[[Valvular]] [[regurgitation]] is more [[Frequentist|frequent]] than the [[valvular stenosis]]. | |||
*Unusually, the [[Tricuspid valve|tricuspid]] or [[pulmonary valves]] are involved. | |||
*[[Systemic embolization|Systemic embolism]] may also occur with the [[Effect size|effects]] [[Dependent variable|depending]] upon the [[Destination spa|destination]] of the [[emboli]] with the [[brain]] and [[kidneys]] being more [[Likelihood|likely]] involved. | |||
*[[Emboli]] can also [[lead]] to the [[Blocking (statistics)|blockage]] of peripheral [[circulation]]. | |||
*The [[Vegetation (pathology)|vegetations]] in Libman-Sacks [[endocarditis]] are mostly [[sterile]] but [[secondary]] [[infective endocarditis]] can also occur. | |||
*There may or may not be the [[Typical set|typical]] [[SLE]] [[Features (pattern recognition)|features]] with the [[Characteristic impedance|characteristic]] [[butterfly rash]], [[fever]], and [[arthritis]] or the [[Antiphospholipid syndrome|APS]] [[Features (pattern recognition)|features]], including [[Recurrence plot|recurrent]] [[miscarriages]]. | |||
{| class="wikitable" | |||
|+Common manifestations of patients with Libman-Sacks endocarditis | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Manifestation}} | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Description}} | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Heart failure]] | |||
|[[Heart failure]] can occur [[secondary]] to the [[valvular dysfunction]] (most commonly [[mitral regurgitation]]), [[Lead|leading]] to the following [[Signs and Symptoms|signs and symptoms]]: | |||
*[[Dyspnea]] | |||
*[[Orthopnea]] | |||
*[[Paroxysmal nocturnal dyspnea]] | |||
*[[Peripheral edema]] | |||
*[[Lethargy]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Cerebrovascular disease|Cerebrovascular]] [[embolism]]<ref name="pmid24029368">{{cite journal| author=Roldan CA, Sibbitt WL, Qualls CR, Jung RE, Greene ER, Gasparovic CM | display-authors=etal| title=Libman-Sacks endocarditis and embolic cerebrovascular disease. | journal=JACC Cardiovasc Imaging | year= 2013 | volume= 6 | issue= 9 | pages= 973-83 | pmid=24029368 | doi=10.1016/j.jcmg.2013.04.012 | pmc=3941465 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24029368 }} </ref> | |||
|[[Cerebrovascular disease|Cerebrovascular]] [[embolism]] can [[Presenting symptom|present]] as any of the following: | |||
* Focal [[Weakness (medical)|weakness]] | |||
* Focal [[numbness]] | |||
*[[Memory loss]] | |||
*[[Vision loss]] | |||
*[[Dysphagia]] | |||
*[[Dysphasia]] | |||
*[[Dysarthria]] | |||
*[[Seizures]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Systemic]] [[thromboembolism]] | |||
|[[Systemic]] [[thromboembolism]] can [[Causes|cause]] any of the following: | |||
*[[Pain]] | |||
*[[Periphery|Peripheral]] [[Cold|coldness]] | |||
*[[Periphery|Peripheral]] [[numbness]] | |||
*[[Acute (medicine)|Acute]] [[abdominal]] [[syndromes]] [[Causes|causing]]: | |||
**[[Abdominal pain]] | |||
**[[Vomiting]] | |||
**[[Left upper quadrant abdominal pain|Left upper quadrant pain]] (due to [[splenic infarct]] from [[embolization]]) | |||
**[[Flank pain]] ( due to [[embolus to the kidney]]) | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Secondary]] [[infective endocarditis]] | |||
|[[Secondary]] [[infective endocarditis]] can [[Presenting symptom|present]] as: | |||
*[[Fever]] | |||
*[[Night sweats]] | |||
*[[Weight loss]] | |||
*[[Lethargy]] | |||
*[[Chest pain]] | |||
|} | |||
==Physical Examination== | ==Physical Examination== | ||
*A patient of Libman-Sacks endocarditis can present with any of the | *A [[patient]] of Libman-Sacks [[endocarditis]] can [[Presenting symptom|present]] with any of the [[Signs and Symptoms|signs and symptoms]] shown in the following table: | ||
= | {| class="wikitable" | ||
|+Physical examination findings in a patient of Libman-Sacks endocarditis | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Pathology}} | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Physical examination finding}} | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Left ventricular hypertrophy]]<ref>https://www.medscape.com/answers/241381-7641/what-are-signs-of-left-ventricular-hypertrophy-lvh-in-cardiac-exam-of-hypertension-high-blood-pressure</ref><ref name="pmid11499746">{{cite journal| author=Okin PM, Devereux RB, Nieminen MS, Jern S, Oikarinen L, Viitasalo M | display-authors=etal| title=Relationship of the electrocardiographic strain pattern to left ventricular structure and function in hypertensive patients: the LIFE study. Losartan Intervention For End point. | journal=J Am Coll Cardiol | year= 2001 | volume= 38 | issue= 2 | pages= 514-20 | pmid=11499746 | doi=10.1016/s0735-1097(01)01378-x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11499746 }} </ref><ref name="pmid4227953">{{cite journal| author=Pinto IJ, Nanda NC, Biswas AK, Parulkar VG| title=Tall upright T waves in the precordial leads. | journal=Circulation | year= 1967 | volume= 36 | issue= 5 | pages= 708-16 | pmid=4227953 | doi=10.1161/01.cir.36.5.708 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4227953 }} </ref><ref name="pmid12392827">{{cite journal| author=Okin PM, Devereux RB, Fabsitz RR, Lee ET, Galloway JM, Howard BV | display-authors=etal| title=Quantitative assessment of electrocardiographic strain predicts increased left ventricular mass: the Strong Heart Study. | journal=J Am Coll Cardiol | year= 2002 | volume= 40 | issue= 8 | pages= 1395-400 | pmid=12392827 | doi=10.1016/s0735-1097(02)02171-x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12392827 }} </ref><ref name="pmid25170097">{{cite journal| author=Shah AS, Chin CW, Vassiliou V, Cowell SJ, Doris M, Kwok TC | display-authors=etal| title=Left ventricular hypertrophy with strain and aortic stenosis. | journal=Circulation | year= 2014 | volume= 130 | issue= 18 | pages= 1607-16 | pmid=25170097 | doi=10.1161/CIRCULATIONAHA.114.011085 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25170097 }} </ref><ref name="pmid11078306">{{cite journal| author=Mehta A, Jain AC, Mehta MC, Billie M| title=Usefulness of left atrial abnormality for predicting left ventricular hypertrophy in the presence of left bundle branch block. | journal=Am J Cardiol | year= 2000 | volume= 85 | issue= 3 | pages= 354-9 | pmid=11078306 | doi=10.1016/s0002-9149(99)00746-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11078306 }} </ref> | |||
|[[Left ventricular hypertrophy|LVH]] can [[Presenting symptom|present]] as any of the following: | |||
==Imaging | *[[Displacement]] of [[apex beat]] | ||
===Echocardiography=== | *[[Enlarged left ventricle|Enlarged]] and [[Sustained release|sustained]] [[apical impulse]] | ||
*Echocardiography | *[[S4|S<sub>4</sub>]] | ||
* | *[[S2|S<sub>2</sub>]] (due to [[aortic root]] [[dilatation]]) | ||
= | *[[ECG]] findings of [[Left ventricular hypertrophy|LVH]] include: | ||
*CXR may show | **Increased [[QRS axis and voltage|QRS voltage]] | ||
*Calcification of lesions is | **Increased [[QRS duration]] ([[Wide QRS complex tachycardias|widened QRS]] [[Association (statistics)|associated]] with complete or incomplete [[Left bundle branch block|LBBB]]) | ||
==Other Diagnostic | **[[Left axis deviation]] ([[Horizontal correlation|horizontal]]/frankly leftward (≥-30º) [[QRS axis]] in the [[frontal plane]] [[Lead|leads]] or [[normal]]/[[Vertical direction|vertical]] [[axis]]) | ||
**[[Right axis deviation]] | |||
**[[Repolarization]] [[abnormalities]] such as [[ST depression|ST depressions]] and [[T wave inversions]] in [[Lead|leads]] with [[Relatively compact|relatively]] [[Taller than average|tall]] [[R waves]] (referred to as '''[[Left ventricle|LV]] "[[Strain (biology)|strain]]" [[pattern]]''' or '''"[[Left ventricular hypertrophy|LVH]] with [[Association (statistics)|associated]] [[ST]]-[[T wave]] [[abnormalities]]"''') | |||
**Prominent '''[[positive]]''' [[T waves]] in the [[lateral]] [[chest]] [[Lead|leads]] | |||
**[[Left atrial]] [[Abnormality (behavior)|abnormality]] has the following two important major [[Presenting symptom|presentations]]: | |||
***Increased duration of [[P waves]] (≥120 [[Millisecond|milliseconds]]) in the [[limb leads]] | |||
***[[Biphasic]] [[P waves]] with a prominent negative (terminal) component (≥40 [[Millisecond|milliseconds]] in duration and/or ≥1 mV in depth) in [[V1-morph|V1]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Congestive heart failure]] | |||
|[[Physical examination]] findings of [[CHF]] include: | |||
*[[Dyspnea]] | |||
*[[Orthopnea]] | |||
*[[Paroxysmal nocturnal dyspnea]] | |||
*[[Peripheral edema]] | |||
*[[Lethargy]] | |||
*[[Rales]] on [[lung examination]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Infective endocarditis]] ([[IE]])<ref>https://emedicine.medscape.com/article/216650-clinical</ref><ref name="pmid29238103">{{cite journal| author=Jingushi N, Iwata M, Terasawa T| title=Clinical features of patients with infective endocarditis presenting to the emergency department: a retrospective case series. | journal=Nagoya J Med Sci | year= 2017 | volume= 79 | issue= 4 | pages= 467-476 | pmid=29238103 | doi=10.18999/nagjms.79.4.467 | pmc=5719206 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29238103 }} </ref><ref name="pmid23574121">{{cite journal| author=Hoen B, Duval X| title=Clinical practice. Infective endocarditis. | journal=N Engl J Med | year= 2013 | volume= 368 | issue= 15 | pages= 1425-33 | pmid=23574121 | doi=10.1056/NEJMcp1206782 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23574121 }} </ref><ref name="pmid26341945">{{cite journal| author=Cahill TJ, Prendergast BD| title=Infective endocarditis. | journal=Lancet | year= 2016 | volume= 387 | issue= 10021 | pages= 882-93 | pmid=26341945 | doi=10.1016/S0140-6736(15)00067-7 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26341945 }} </ref> | |||
|[[Infective endocarditis|IE]] can [[Presenting symptom|present]] as: | |||
*[[Fever]] | |||
*[[Rigors]] | |||
*[[Night sweats]] | |||
*[[Headache]] | |||
*[[Myalgias]] | |||
*[[Anorexia]] | |||
*[[Malaise]] | |||
*[[Shortness of breath]] | |||
*[[Cough]] | |||
*[[Joint pains]] | |||
*[[Presenting symptom|Presence]] of a [[new]] or [[Change detection|changing]] [[heart murmur]] in 80% to 85% of [[patients]] (due to [[aortic insufficiency]], [[tricuspid regurgitation]] or [[mitral regurgitation]]) | |||
*[[Widened pulse pressure]] (due to [[aortic insufficiency]]) | |||
*[[Petechiae]] (10% to 40% of [[patients]]) | |||
*[[Osler's nodes]] (7% to 10% of [[patients]]) | |||
*[[Janeway lesions]] (6% to 10% of [[patients]]) | |||
*[[Splinter hemorrhages]] (5% to 15% of [[patients]]) | |||
*[[Evidence]] of [[embolization]] | |||
*[[Conjunctival hemorrhage]] | |||
*[[Roth's spot|Roth's spots]] in [[retina]] | |||
*Poor [[oral hygiene]] | |||
*[[Teeth]] might have [[periodontitis]], [[plaque]] or [[calculus]] | |||
*[[Gingivitis]] | |||
*[[Splenomegaly]] (15% to 30% [[patients]]) | |||
*[[Left upper quadrant abdominal pain|Left upper quadrant pain]] (due to [[splenic infarct]] from [[embolization]]) | |||
*[[Flank pain]] (due to [[embolus to the kidney]]) | |||
*[[Stroke]] and [[Focal neurologic signs|focal neurologic findings]] (due to [[septic emboli]]) | |||
*[[Seizures]] | |||
*[[Intracranial hemorrhage]] | |||
*[[Signs]] of a [[brain abscess]] | |||
*[[Gangrene]] of [[fingers]] | |||
*[[Back pain]] (due to [[vertebral osteomyelitis]]) | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Mitral valve disease]]<ref name="HojnikGeorge1996">{{cite journal|last1=Hojnik|first1=Maja|last2=George|first2=Jacob|last3=Ziporen|first3=Lea|last4=Shoenfeld|first4=Yehuda|title=Heart Valve Involvement (Libman-Sacks Endocarditis) in the Antiphospholipid Syndrome|journal=Circulation|volume=93|issue=8|year=1996|pages=1579–1587|issn=0009-7322|doi=10.1161/01.CIR.93.8.1579}}</ref> | |||
| | |||
* High-[[Pitch|pitched]] “blowing” [[holosystolic murmur]] of '''[[mitral regurgitation]]''' (more common) which is best [[Hearing|heard]] at the [[apex of the heart]] with the [[patient]] in left [[lateral]] [[decubitus]] [[Position effect|position]]. | |||
* Mid-[[diastolic]], rumbling [[Heart murmur|murmur]] of '''[[mitral stenosis]] ('''with or without an [[Austin Flint murmur]]). | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Aortic valve disease]] | |||
| | |||
*[[Early diastolic murmur]] of [[Aortic regurgitation|'''aortic''' '''regurgitation''']] | |||
*[[Widened pulse pressure]] due to [[aortic insufficiency]] | |||
* Bobbing of the [[uvula]] ([[new]]-onset [[aortic regurgitation]]) | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Tricuspid valve disease]] | |||
| | |||
*[[Holosystolic murmur]] of [[Tricuspid regurgitation|'''tricuspid''' '''regurgitation''']] | |||
|} | |||
==Laboratory Findings== | |||
{| class="wikitable" | |||
|+ | |||
!! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Laboratory Investigations in Libman-Sacks Endocarditis}} | |||
! style="background: #4479BA; width: 200px;" ! | {{fontcolor|#FFF|Laboratory test findings}} | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Blood culture]] | |||
| | |||
* It is important to rule out the coexisting [[infective endocarditis]] and other [[infectious]] [[etiologies]] by taking multiple [[blood cultures]]. | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[SLE]] [[Investigational product|investigations]] | |||
(Immunological assays) | |||
| | |||
*[[Investigational product|Investigations]] for [[SLE]] are [[positive]] including: | |||
**[[Antinuclear antibodies]] ([[SLE]] [[Screening test|screening]]) | |||
**[[Anti-dsDNA antbodies|Anti-dsDNA antibodies]] ([[SLE]] [[Confirmatory factor analysis|confirmation]] and to [[Monitor role|monitor]] the progress of [[disease]] and [[lupus nephritis]]) | |||
** Anti-Smith [[antibodies]] | |||
**Anti-RNP | |||
**[[Antiphospholipid antibodies]] | |||
**[[Anticardiolipin antibodies]] ([[Association (statistics)|associated]] with an increased [[RiskMetrics|risk]] of [[cardiac]] [[abnormalities]]) | |||
**Anti-Ro/SSA | |||
**Anti-La/SSB | |||
**[[False-positive test result|False-positive]] [[serology]] in the form of [[Venereal disease research laboratory (VDRL) test|VDRL]] is also common in [[SLE]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Complete blood count|CBC]] | |||
| | |||
*[[Complete blood count|CBC]] may show: | |||
**[[Neutrophilia]] | |||
**[[Anemia]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Study design|Studies]] to rule out [[Disseminated intravascular coagulation|DIC]] | |||
| | |||
*[[Prothrombin time (PT)|Prothrombin time]] | |||
*[[Partial thromboplastin time]] | |||
*[[Fibrinogen]] | |||
*[[Thrombin time]] | |||
*[[D dimer|D-dimer]] | |||
*[[Cross-linked enzyme aggregate|Cross-linked]] [[fibrin degradation products]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Polymerase chain reaction]] ([[Polymerase chain reaction|PCR]]) | |||
| | |||
*[[Polymerase chain reaction|PCR]] is a rapid and [[Reliability (statistics)|reliable]] [[Method of Factors|method]] to [[Detection theory|detect]] the [[culture-negative endocarditis]] by fastidious [[organisms]]. | |||
|} | |||
<br /> | |||
==Imaging Findings== | |||
{| class="wikitable" | |||
|+ | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Imaging tests in Libman-Sacks Endocarditis}} | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Imagining Findings}} | |||
|- | |||
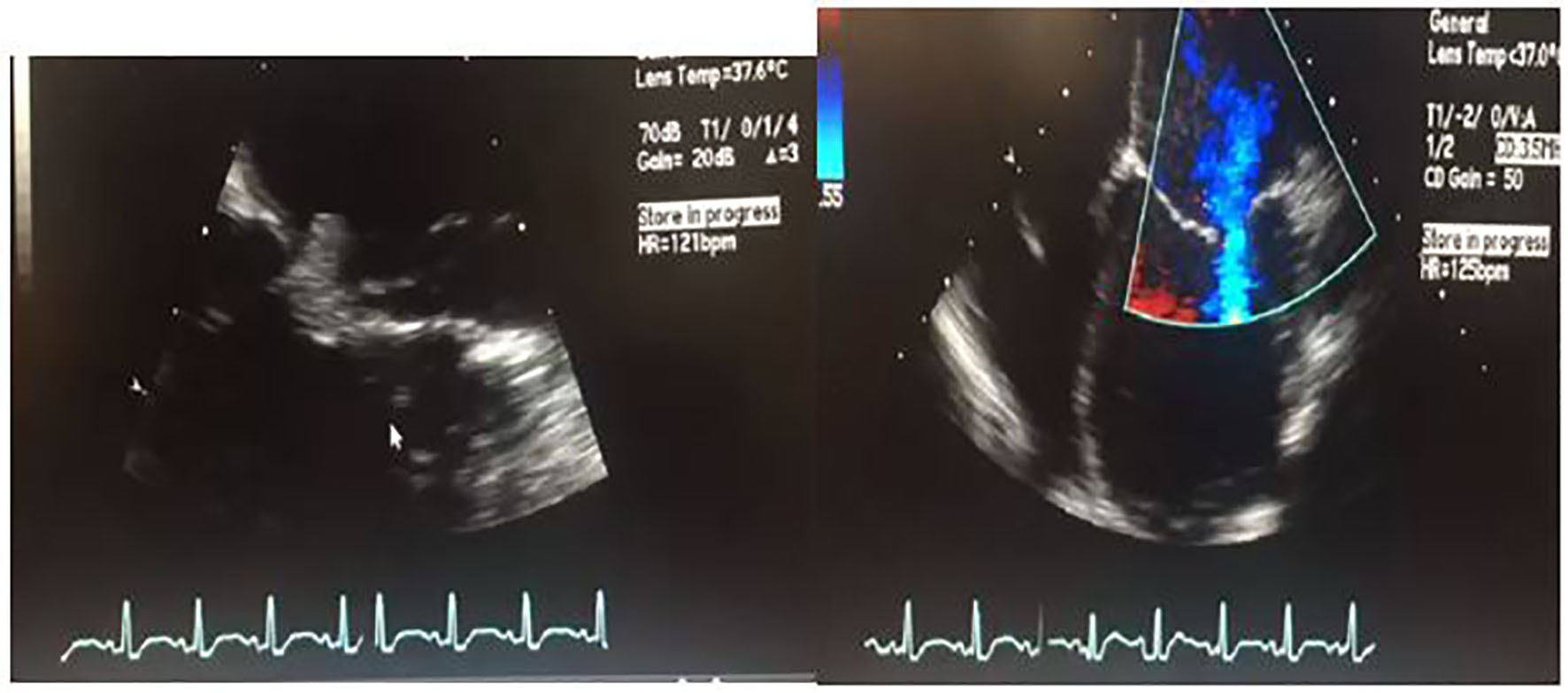
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Echocardiography]]<ref name="pmid25807885">{{cite journal| author=Roldan CA, Tolstrup K, Macias L, Qualls CR, Maynard D, Charlton G | display-authors=etal| title=Libman-Sacks Endocarditis: Detection, Characterization, and Clinical Correlates by Three-Dimensional Transesophageal Echocardiography. | journal=J Am Soc Echocardiogr | year= 2015 | volume= 28 | issue= 7 | pages= 770-9 | pmid=25807885 | doi=10.1016/j.echo.2015.02.011 | pmc=4592775 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25807885 }} </ref><ref name="pmid18085739">{{cite journal| author=Roldan CA, Qualls CR, Sopko KS, Sibbitt WL| title=Transthoracic versus transesophageal echocardiography for detection of Libman-Sacks endocarditis: a randomized controlled study. | journal=J Rheumatol | year= 2008 | volume= 35 | issue= 2 | pages= 224-9 | pmid=18085739 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18085739 }} </ref><ref name="pmid19763069">{{cite journal| author=Roldan CA| title=Diagnostic value of transesophageal echocardiography in Libman-Sacks endocarditis. | journal=Minerva Cardioangiol | year= 2009 | volume= 57 | issue= 4 | pages= 467-81 | pmid=19763069 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19763069 }} </ref> | |||
| | |||
*[[Echocardiography]] is the key [[diagnostic test]] for Libman-Sacks [[endocarditis]] (although it doesn't [[Detection theory|detect]] all the [[lesions]]). | |||
*[[Transesophageal echocardiography (TEE)|Transesophageal echocardiography]] is [[superior]] to [[transthoracic echocardiography]] but it is an [[invasive]] [[procedure]]. | |||
*As Libman-Sacks [[endocarditis]] is commonly [[Complication (medicine)|complicated]] by [[embolic]] [[cerebrovascular disease]], hence, [[Accuracy|accurate]] [[Detection theory|detection]] of its [[Vegetation (pathology)|vegetations]] may [[lead]] to early [[therapy]] and [[prevention]] of the [[Association (statistics)|associated]] [[complications]]. | |||
*Although the [[Two-dimensional echocardiography|two-dimensional]] [[Transesophageal echocardiography (TEE)|transesophageal echocardiography]] ([[2D echocardiography|2D-TEE]]) has a higher [[diagnostic]] [[Value (mathematics)|value]] for the [[Detection theory|detection]] of Libman-Sacks [[Vegetation (pathology)|vegetations]], but the three-[[Dimensional analysis|dimensional]] [[Transesophageal echocardiography (TEE)|TEE]] (3D-[[Transesophageal echocardiography (TEE)|TEE]]) has the following benefits over [[Two dimensional echocardiography|2D-TEE]]: | |||
**Improved [[Detection theory|detection]] | |||
**Improved [[Characterization (mathematics)|characterization]] | |||
**Improved [[clinical]] [[Correlation|correlations]] of Libman-Sacks [[Vegetation (pathology)|vegetations]] | |||
**Provides [[Clinical|clinically]] [[Relevance|relevant]] [[Addition reaction|additive]] [[Information science|information]] [[Complement|complementing]] the [[Two dimensional echocardiography|2D-TEE]] for the [[Characterization (mathematics)|characterization]], [[Detection theory|detection]], and [[Association (statistics)|association]] with the [[cerebrovascular disease]] of Libman-Sacks [[endocarditis]]. | |||
{| | |||
| | |||
[[File:Cr534e-g002.jpg|thumb|400px|none|2D transesophageal ultrasound. Image on the left shows a thickened mitral valve with a 1 cm vegetation that can be seen on the anterior mitral leaflet. Image on the right is a four-chamber color flow Doppler view showing biventricular dilatation, severe left ventricular dysfunction. For orientation purposes, left ventricle is the bottom right chamber. Video of both views is attached as a supplementary file. [https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
| | |||
|} | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Chest X-ray|Chest X-Ray]] | |||
| | |||
*[[Chest X-ray|CXR]] may show any of the following findings: | |||
**[[Cardiomegaly]] | |||
**[[Pulmonary congestion]] (in case of severe [[disease]]) | |||
**[[Calcification]] of the [[lesions]] (uncommon) | |||
|- | |||
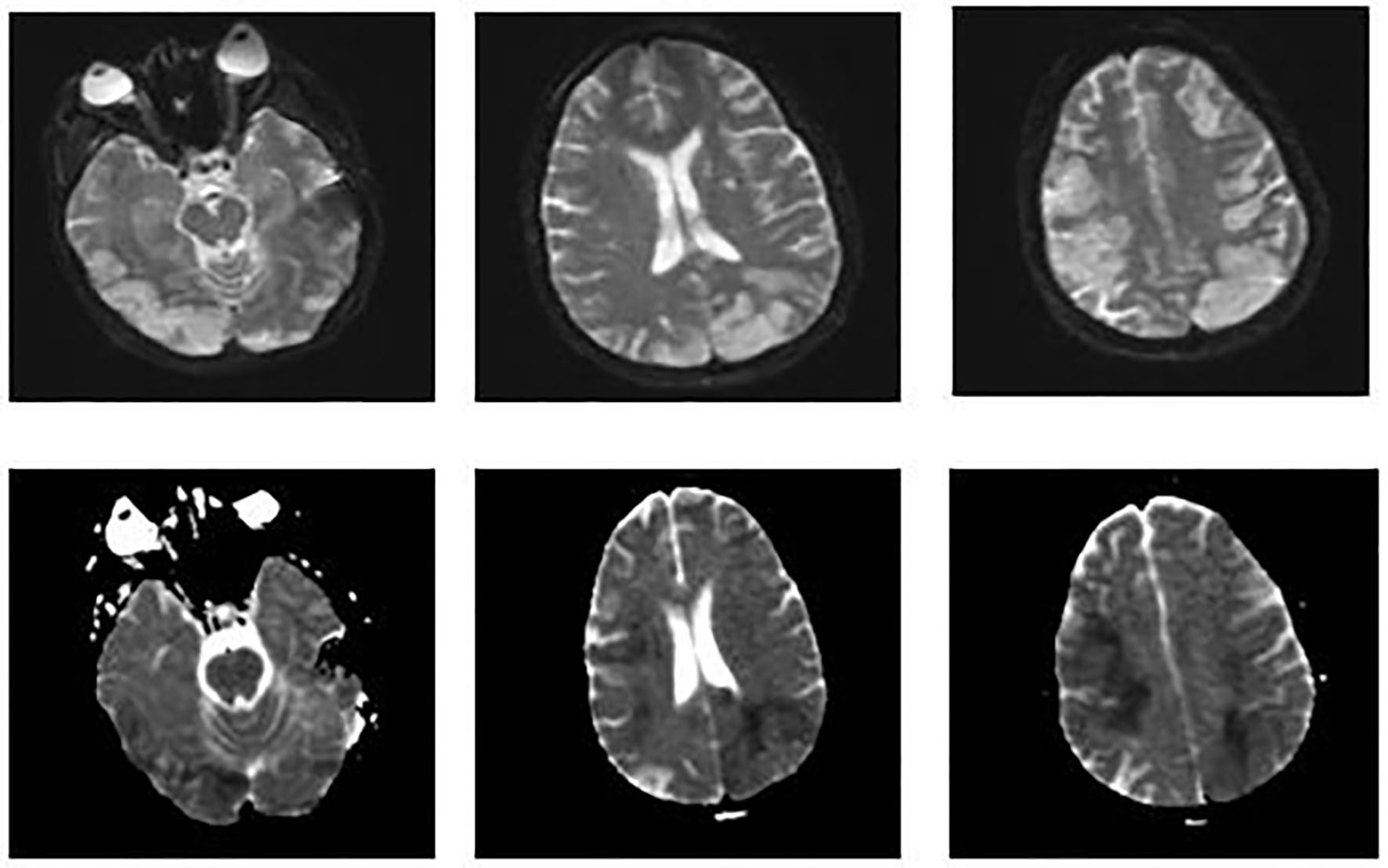
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[MRI]]<ref>https://radiopaedia.org/articles/libman-sacks-endocarditis-1?lang=us</ref> | |||
| | |||
* According to the ongoing [[current]] [[Study arms|studies]], [[4D]]-[[flow]] [[Magnetic resonance imaging|MRI]] [[imaging]] is considered as a promising useful [[Noninvasive test|noninvasive tool]] [[Comparability|compared]] to the [[Traditional medicine|traditional]] [[Transesophageal echocardiography (TEE)|TEE]] for evaluating the following: | |||
**[[Abnormal]] [[flow]] [[Pattern|patterns]] | |||
**[[Ventricular]] [[Dimension|dimensions]] | |||
**[[Stroke volume]] | |||
**[[Region of interest|Regional]] [[myocardial]] [[Function (biology)|function]] | |||
{| | |||
| | |||
[[File:Cr534e-g003.jpg|thumb|400px|none|MRI of the brain. Images on the top show increased signal on diffusion weighted imaging (DWI) throughout the bilateral frontal, parietal, and occipital lobes. Images on the bottom show a corresponding decreased signal intensity on apparent diffusion coefficient that is consistent with acute abnormal restricted diffusion. These findings suggest new/ongoing acute infarcts.[https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
| | |||
|} | |||
|- | |||
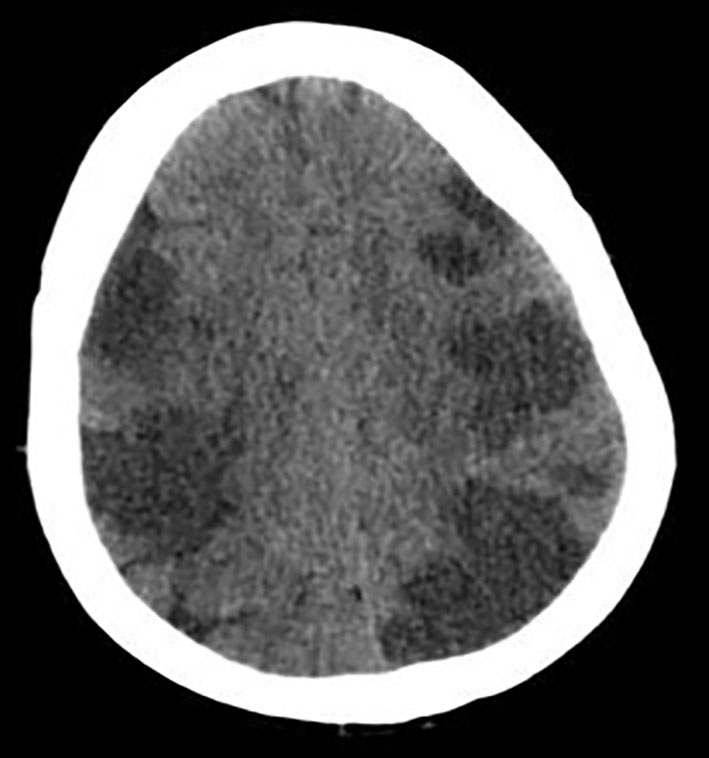
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[CT scan]] ([[Head]]) | |||
| | |||
* In [[patients]] with [[Cerebrovascular disease|cerebrovascular]] [[emboli]], [[CT scan]] of the [[head]] without [[contrast]] may show extensive multifocal hypoattenuating [[Area|areas]] in the involved [[Region of interest|region]] as shown in the [[image]] below: | |||
{| | |||
| | |||
[[File:Cr534e-g001.jpg|thumb|250px|none|CT of head without contrast showing extensive multifocal areas of hypoattentuation throughout the bilateral frontal, parietal, occipital, and right > left temporal lobes. No mass effect or midline shift or hemorrhage was seen.[https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
| | |||
|} | |||
|} | |||
==Other Diagnostic Studies== | |||
===Cardiac Catheterization=== | ===Cardiac Catheterization=== | ||
* | *In case of severe [[valvular disease]], [[cardiac catheterization]] may be required with a view to [[valve replacement]]. | ||
==Treatment== | ==Treatment== | ||
*There is no specific treatment for Libman-Sacks endocarditis. | *There is no [[Specific activity|specific]] [[Treatment Planning|treatment]] for Libman-Sacks [[endocarditis]]. | ||
*Steroids and immunosuppressive agents are useful in the treatment of | *[[Treatment Planning|Treatment]] of LSE is quite difficult with the [[Main effect|main]] [[Focusing|focus]] being on the [[Correction (newspaper)|correction]] of the [[Underlying representation|underlying]] [[Causes|cause]]. | ||
* | |||
* | {| class="wikitable" | ||
|+Common treatment options for Libman-Sacks endocarditis depending on the underlying cause | |||
* | !style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Treatment option}} | ||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Details}} | |||
* | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Steroids]] and [[immunosuppressive agents]] | |||
|They are [[Usage analysis|useful]] in the [[Treatment Planning|treatment]] of [[Underlying representation|underlying]] [[disease]] but they have a controversial role in the [[pathogenesis]] of [[Vegetation (pathology)|vegetations]]: | |||
*[[Patients]] [[Treatment Planning|treated]] with [[steroids]] have smaller and fewer [[lesions]] (mostly on one [[valve]] and usually confined to the left side) as [[Comparability|compared]] to the [[Postmortem studies|postmortem reports]] of [[patients]] before the advent of [[steroids]]. | |||
*The [[Usage analysis|use]] of [[corticosteroids]] has also [[lead]] to the 5 [[Timespan|times]] decline in [[hypertension]] and 8 [[Timespan|times]] decline in [[congestive heart failure]] [[rates]] in the [[patients]] of Libman-Sacks [[endocarditis]]. | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Anticoagulants]] | |||
| | |||
*In the case of [[Systemic embolization|systemic emboli]], [[Anticoagulation therapy|anticoagulation]] with [[warfarin]] is beneficial. | |||
*[[Anticoagulation therapy|Anticoagulation]] is advised if there is [[evidence]] of one [[cerebrovascular event]]. | |||
*[[Patients]] with a [[Potential|potentially]] [[Cure|curable]] [[cancer]], [[coagulopathy]] should be [[Correction (newspaper)|corrected]] with [[heparin]] (if there is no [[contraindication]]). | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Other [[medications]] | |||
| | |||
*[[Vasodilators]] | |||
*[[Beta-blockers]] | |||
*[[Diuretics]] | |||
*[[Digoxin]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Valve replacement surgery|Valve replacement]]<ref name="pmid20331896">{{cite journal| author=Bouma W, Klinkenberg TJ, van der Horst IC, Wijdh-den Hamer IJ, Erasmus ME, Bijl M | display-authors=etal| title=Mitral valve surgery for mitral regurgitation caused by Libman-Sacks endocarditis: a report of four cases and a systematic review of the literature. | journal=J Cardiothorac Surg | year= 2010 | volume= 5 | issue= | pages= 13 | pmid=20331896 | doi=10.1186/1749-8090-5-13 | pmc=2859362 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20331896 }} </ref><ref name="pmid28734427">{{cite journal| author=Samura T, Toda K, Yoshioka D, Nakamura T, Miyagawa S, Yoshikawa Y | display-authors=etal| title=Libman-Sacks Endocarditis Due to Systemic Lupus Erythematosus Activation After Mitral Valve Plasty. | journal=Ann Thorac Surg | year= 2017 | volume= 104 | issue= 2 | pages= e109-e111 | pmid=28734427 | doi=10.1016/j.athoracsur.2017.01.073 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28734427 }} </ref><ref name="pmid21404907">{{cite journal| author=Perier P, Jeserich M, Vieth M, Pohle K, Hohenberger W, Diegeler A| title=Mitral valve reconstruction in a patient with Libman-Sacks endocarditis: a case report. | journal=J Heart Valve Dis | year= 2011 | volume= 20 | issue= 1 | pages= 103-6 | pmid=21404907 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21404907 }} </ref> | |||
| | |||
*[[Valve replacement surgery]] is [[done]] in case of severe [[valvular disease]]. | |||
*[[Mechanical valve|Mechanical valves]] may be more [[Susceptible individual|susceptible]] to [[Thromboembolism|thromboemboli]] as [[Comparability|compared]] to [[bioprosthetic valves]]. | |||
*[[Mitral valve replacement]] [[surgery]] has an [[Operation (mathematics)|operative]] [[mortality]] of as high as 25% in [[patients]] with Libman-Sacks [[endocarditis]]. | |||
|} | |||
== | ==Differentiating Libman-Sacks Endocarditis from other Diseases== | ||
Libman-Sacks [[endocarditis]] should be [[Differentiate|differentiated]] from other [[diseases]] [[Presenting symptom|presenting]] with [[fever]], [[chest pain]] and [[anorexia]]. The [[Difference (philosophy)|differentials]] include the following:<ref name="pmid24550636">{{cite journal |vauthors=Brenes-Salazar JA |title=Westermark's and Palla's signs in acute and chronic pulmonary embolism: Still valid in the current computed tomography era |journal=J Emerg Trauma Shock |volume=7 |issue=1 |pages=57–8 |year=2014 |pmid=24550636 |pmc=3912657 |doi=10.4103/0974-2700.125645 |url=}}</ref><ref name="urlCT Angiography of Pulmonary Embolism: Diagnostic Criteria and Causes of Misdiagnosis | RadioGraphics">{{cite web |url=http://pubs.rsna.org/doi/full/10.1148/rg.245045008 |title=CT Angiography of Pulmonary Embolism: Diagnostic Criteria and Causes of Misdiagnosis | RadioGraphics |format= |work= |accessdate=}}</ref><ref name="pmid23940438">{{cite journal |vauthors=Bĕlohlávek J, Dytrych V, Linhart A |title=Pulmonary embolism, part I: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism |journal=Exp Clin Cardiol |volume=18 |issue=2 |pages=129–38 |year=2013 |pmid=23940438 |pmc=3718593 |doi= |url=}}</ref><ref name="urlPulmonary Embolism: Symptoms - National Library of Medicine - PubMed Health">{{cite web |url=https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0022657/ |title=Pulmonary Embolism: Symptoms - National Library of Medicine - PubMed Health |format= |work= |accessdate=}}</ref><ref name="pmid20118395">{{cite journal |vauthors=Ramani GV, Uber PA, Mehra MR |title=Chronic heart failure: contemporary diagnosis and management |journal=Mayo Clin. Proc. |volume=85 |issue=2 |pages=180–95 |year=2010 |pmid=20118395 |pmc=2813829 |doi=10.4065/mcp.2009.0494 |url=}}</ref><ref name="pmid18215495">{{cite journal |vauthors=Blinderman CD, Homel P, Billings JA, Portenoy RK, Tennstedt SL |title=Symptom distress and quality of life in patients with advanced congestive heart failure |journal=J Pain Symptom Manage |volume=35 |issue=6 |pages=594–603 |year=2008 |pmid=18215495 |pmc=2662445 |doi=10.1016/j.jpainsymman.2007.06.007 |url=}}</ref><ref name="pmid19168510">{{cite journal |vauthors=Hawkins NM, Petrie MC, Jhund PS, Chalmers GW, Dunn FG, McMurray JJ |title=Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology |journal=Eur. J. Heart Fail. |volume=11 |issue=2 |pages=130–9 |year=2009 |pmid=19168510 |pmc=2639415 |doi=10.1093/eurjhf/hfn013 |url=}}</ref><ref name="pmid9465867">{{cite journal |vauthors=Takasugi JE, Godwin JD |title=Radiology of chronic obstructive pulmonary disease |journal=Radiol. Clin. North Am. |volume=36 |issue=1 |pages=29–55 |year=1998 |pmid=9465867 |doi= |url=}}</ref><ref name="pmid14651761">{{cite journal |vauthors=Wedzicha JA, Donaldson GC |title=Exacerbations of chronic obstructive pulmonary disease |journal=Respir Care |volume=48 |issue=12 |pages=1204–13; discussion 1213–5 |year=2003 |pmid=14651761 |doi= |url=}}</ref><ref name="pmid23833163">{{cite journal |vauthors=Nakawah MO, Hawkins C, Barbandi F |title=Asthma, chronic obstructive pulmonary disease (COPD), and the overlap syndrome |journal=J Am Board Fam Med |volume=26 |issue=4 |pages=470–7 |year=2013 |pmid=23833163 |doi=10.3122/jabfm.2013.04.120256 |url=}}</ref><ref name="pmid20511488">{{cite journal |vauthors=Khandaker MH, Espinosa RE, Nishimura RA, Sinak LJ, Hayes SN, Melduni RM, Oh JK |title=Pericardial disease: diagnosis and management |journal=Mayo Clin. Proc. |volume=85 |issue=6 |pages=572–93 |year=2010 |pmid=20511488 |pmc=2878263 |doi=10.4065/mcp.2010.0046 |url=}}</ref><ref name="pmid23610095">{{cite journal |vauthors=Bogaert J, Francone M |title=Pericardial disease: value of CT and MR imaging |journal=Radiology |volume=267 |issue=2 |pages=340–56 |year=2013 |pmid=23610095 |doi=10.1148/radiol.13121059 |url=}}</ref><ref name="pmid11680112">{{cite journal |vauthors=Gharib AM, Stern EJ |title=Radiology of pneumonia |journal=Med. Clin. North Am. |volume=85 |issue=6 |pages=1461–91, x |year=2001 |pmid=11680112 |doi= |url=}}</ref><ref name="pmid23507061">{{cite journal |vauthors=Schmidt WA |title=Imaging in vasculitis |journal=Best Pract Res Clin Rheumatol |volume=27 |issue=1 |pages=107–18 |year=2013 |pmid=23507061 |doi=10.1016/j.berh.2013.01.001 |url=}}</ref><ref name="pmid16891436">{{cite journal |vauthors=Suresh E |title=Diagnostic approach to patients with suspected vasculitis |journal=Postgrad Med J |volume=82 |issue=970 |pages=483–8 |year=2006 |pmid=16891436 |pmc=2585712 |doi=10.1136/pgmj.2005.042648 |url=}}</ref><ref name="pmid123074">{{cite journal |vauthors=Stein PD, Dalen JE, McIntyre KM, Sasahara AA, Wenger NK, Willis PW |title=The electrocardiogram in acute pulmonary embolism |journal=Prog Cardiovasc Dis |volume=17 |issue=4 |pages=247–57 |year=1975 |pmid=123074 |doi= |url=}}</ref><ref name="pmid23413894">{{cite journal |vauthors=Warnier MJ, Rutten FH, Numans ME, Kors JA, Tan HL, de Boer A, Hoes AW, De Bruin ML |title=Electrocardiographic characteristics of patients with chronic obstructive pulmonary disease |journal=COPD |volume=10 |issue=1 |pages=62–71 |year=2013 |pmid=23413894 |doi=10.3109/15412555.2012.727918 |url=}}</ref><ref name="pmid23000104">{{cite journal |vauthors=Stein PD, Matta F, Ekkah M, Saleh T, Janjua M, Patel YR, Khadra H |title=Electrocardiogram in pneumonia |journal=Am. J. Cardiol. |volume=110 |issue=12 |pages=1836–40 |year=2012 |pmid=23000104 |doi=10.1016/j.amjcard.2012.08.019 |url=}}</ref><ref name="pmid26209947">{{cite journal |vauthors=Hazebroek MR, Kemna MJ, Schalla S, Sanders-van Wijk S, Gerretsen SC, Dennert R, Merken J, Kuznetsova T, Staessen JA, Brunner-La Rocca HP, van Paassen P, Cohen Tervaert JW, Heymans S |title=Prevalence and prognostic relevance of cardiac involvement in ANCA-associated vasculitis: eosinophilic granulomatosis with polyangiitis and granulomatosis with polyangiitis |journal=Int. J. Cardiol. |volume=199 |issue= |pages=170–9 |year=2015 |pmid=26209947 |doi=10.1016/j.ijcard.2015.06.087 |url=}}</ref><ref name="pmid20112390">{{cite journal |vauthors=Dennert RM, van Paassen P, Schalla S, Kuznetsova T, Alzand BS, Staessen JA, Velthuis S, Crijns HJ, Tervaert JW, Heymans S |title=Cardiac involvement in Churg-Strauss syndrome |journal=Arthritis Rheum. |volume=62 |issue=2 |pages=627–34 |year=2010 |pmid=20112390 |doi=10.1002/art.27263 |url=}}</ref> | Libman-Sacks [[endocarditis]] should be [[Differentiate|differentiated]] from other [[diseases]] [[Presenting symptom|presenting]] with [[fever]], [[chest pain]] and [[anorexia]]. The [[Difference (philosophy)|differentials]] include the following:<ref name="pmid24550636">{{cite journal |vauthors=Brenes-Salazar JA |title=Westermark's and Palla's signs in acute and chronic pulmonary embolism: Still valid in the current computed tomography era |journal=J Emerg Trauma Shock |volume=7 |issue=1 |pages=57–8 |year=2014 |pmid=24550636 |pmc=3912657 |doi=10.4103/0974-2700.125645 |url=}}</ref><ref name="urlCT Angiography of Pulmonary Embolism: Diagnostic Criteria and Causes of Misdiagnosis | RadioGraphics">{{cite web |url=http://pubs.rsna.org/doi/full/10.1148/rg.245045008 |title=CT Angiography of Pulmonary Embolism: Diagnostic Criteria and Causes of Misdiagnosis | RadioGraphics |format= |work= |accessdate=}}</ref><ref name="pmid23940438">{{cite journal |vauthors=Bĕlohlávek J, Dytrych V, Linhart A |title=Pulmonary embolism, part I: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism |journal=Exp Clin Cardiol |volume=18 |issue=2 |pages=129–38 |year=2013 |pmid=23940438 |pmc=3718593 |doi= |url=}}</ref><ref name="urlPulmonary Embolism: Symptoms - National Library of Medicine - PubMed Health">{{cite web |url=https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0022657/ |title=Pulmonary Embolism: Symptoms - National Library of Medicine - PubMed Health |format= |work= |accessdate=}}</ref><ref name="pmid20118395">{{cite journal |vauthors=Ramani GV, Uber PA, Mehra MR |title=Chronic heart failure: contemporary diagnosis and management |journal=Mayo Clin. Proc. |volume=85 |issue=2 |pages=180–95 |year=2010 |pmid=20118395 |pmc=2813829 |doi=10.4065/mcp.2009.0494 |url=}}</ref><ref name="pmid18215495">{{cite journal |vauthors=Blinderman CD, Homel P, Billings JA, Portenoy RK, Tennstedt SL |title=Symptom distress and quality of life in patients with advanced congestive heart failure |journal=J Pain Symptom Manage |volume=35 |issue=6 |pages=594–603 |year=2008 |pmid=18215495 |pmc=2662445 |doi=10.1016/j.jpainsymman.2007.06.007 |url=}}</ref><ref name="pmid19168510">{{cite journal |vauthors=Hawkins NM, Petrie MC, Jhund PS, Chalmers GW, Dunn FG, McMurray JJ |title=Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology |journal=Eur. J. Heart Fail. |volume=11 |issue=2 |pages=130–9 |year=2009 |pmid=19168510 |pmc=2639415 |doi=10.1093/eurjhf/hfn013 |url=}}</ref><ref name="pmid9465867">{{cite journal |vauthors=Takasugi JE, Godwin JD |title=Radiology of chronic obstructive pulmonary disease |journal=Radiol. Clin. North Am. |volume=36 |issue=1 |pages=29–55 |year=1998 |pmid=9465867 |doi= |url=}}</ref><ref name="pmid14651761">{{cite journal |vauthors=Wedzicha JA, Donaldson GC |title=Exacerbations of chronic obstructive pulmonary disease |journal=Respir Care |volume=48 |issue=12 |pages=1204–13; discussion 1213–5 |year=2003 |pmid=14651761 |doi= |url=}}</ref><ref name="pmid23833163">{{cite journal |vauthors=Nakawah MO, Hawkins C, Barbandi F |title=Asthma, chronic obstructive pulmonary disease (COPD), and the overlap syndrome |journal=J Am Board Fam Med |volume=26 |issue=4 |pages=470–7 |year=2013 |pmid=23833163 |doi=10.3122/jabfm.2013.04.120256 |url=}}</ref><ref name="pmid20511488">{{cite journal |vauthors=Khandaker MH, Espinosa RE, Nishimura RA, Sinak LJ, Hayes SN, Melduni RM, Oh JK |title=Pericardial disease: diagnosis and management |journal=Mayo Clin. Proc. |volume=85 |issue=6 |pages=572–93 |year=2010 |pmid=20511488 |pmc=2878263 |doi=10.4065/mcp.2010.0046 |url=}}</ref><ref name="pmid23610095">{{cite journal |vauthors=Bogaert J, Francone M |title=Pericardial disease: value of CT and MR imaging |journal=Radiology |volume=267 |issue=2 |pages=340–56 |year=2013 |pmid=23610095 |doi=10.1148/radiol.13121059 |url=}}</ref><ref name="pmid11680112">{{cite journal |vauthors=Gharib AM, Stern EJ |title=Radiology of pneumonia |journal=Med. Clin. North Am. |volume=85 |issue=6 |pages=1461–91, x |year=2001 |pmid=11680112 |doi= |url=}}</ref><ref name="pmid23507061">{{cite journal |vauthors=Schmidt WA |title=Imaging in vasculitis |journal=Best Pract Res Clin Rheumatol |volume=27 |issue=1 |pages=107–18 |year=2013 |pmid=23507061 |doi=10.1016/j.berh.2013.01.001 |url=}}</ref><ref name="pmid16891436">{{cite journal |vauthors=Suresh E |title=Diagnostic approach to patients with suspected vasculitis |journal=Postgrad Med J |volume=82 |issue=970 |pages=483–8 |year=2006 |pmid=16891436 |pmc=2585712 |doi=10.1136/pgmj.2005.042648 |url=}}</ref><ref name="pmid123074">{{cite journal |vauthors=Stein PD, Dalen JE, McIntyre KM, Sasahara AA, Wenger NK, Willis PW |title=The electrocardiogram in acute pulmonary embolism |journal=Prog Cardiovasc Dis |volume=17 |issue=4 |pages=247–57 |year=1975 |pmid=123074 |doi= |url=}}</ref><ref name="pmid23413894">{{cite journal |vauthors=Warnier MJ, Rutten FH, Numans ME, Kors JA, Tan HL, de Boer A, Hoes AW, De Bruin ML |title=Electrocardiographic characteristics of patients with chronic obstructive pulmonary disease |journal=COPD |volume=10 |issue=1 |pages=62–71 |year=2013 |pmid=23413894 |doi=10.3109/15412555.2012.727918 |url=}}</ref><ref name="pmid23000104">{{cite journal |vauthors=Stein PD, Matta F, Ekkah M, Saleh T, Janjua M, Patel YR, Khadra H |title=Electrocardiogram in pneumonia |journal=Am. J. Cardiol. |volume=110 |issue=12 |pages=1836–40 |year=2012 |pmid=23000104 |doi=10.1016/j.amjcard.2012.08.019 |url=}}</ref><ref name="pmid26209947">{{cite journal |vauthors=Hazebroek MR, Kemna MJ, Schalla S, Sanders-van Wijk S, Gerretsen SC, Dennert R, Merken J, Kuznetsova T, Staessen JA, Brunner-La Rocca HP, van Paassen P, Cohen Tervaert JW, Heymans S |title=Prevalence and prognostic relevance of cardiac involvement in ANCA-associated vasculitis: eosinophilic granulomatosis with polyangiitis and granulomatosis with polyangiitis |journal=Int. J. Cardiol. |volume=199 |issue= |pages=170–9 |year=2015 |pmid=26209947 |doi=10.1016/j.ijcard.2015.06.087 |url=}}</ref><ref name="pmid20112390">{{cite journal |vauthors=Dennert RM, van Paassen P, Schalla S, Kuznetsova T, Alzand BS, Staessen JA, Velthuis S, Crijns HJ, Tervaert JW, Heymans S |title=Cardiac involvement in Churg-Strauss syndrome |journal=Arthritis Rheum. |volume=62 |issue=2 |pages=627–34 |year=2010 |pmid=20112390 |doi=10.1002/art.27263 |url=}}</ref> | ||
:*[[ | :*[[Nonbacterial thrombotic endocarditis]] ([[Marantic endocarditis]]) | ||
:*[[Vasculitis]] | :*[[Vasculitis]] | ||
:*[[Temporal arteritis]] | :*[[Temporal arteritis]] | ||
| Line 215: | Line 619: | ||
**Eventual [[right heart failure]] | **Eventual [[right heart failure]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Non- | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Non-bacterial thrombotic endocarditis|Non-bacterial thrombotic endocarditis]] | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" | | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" | | ||
Latest revision as of 20:57, 19 August 2020
|
Libman-Sacks endocarditis Microchapters |
|
Differentiating Libman-Sacks Endocarditis from other Diseases |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sara Mohsin, M.D.[2]
Synonyms and keywords:: Nonbacterial thrombotic endocarditis (NBTE), Marantic endocarditis, Verrucous endocarditis
Overview
Libman-Sacks endocarditis (LSE) is a form of nonbacterial thrombotic endocarditis (NBTE) that is considered to be the most common cardiac manifestation seen in patients with systemic lupus erythematosus. LSE is a term used for sterile and verrucous vegetations around the heart valves mostly affecting the mitral and aortic heart valves but other valves may also be involved. Valvular involvement in LSE may lead to valvular regurgitation, aortic insufficiency, thromboembolic cerebrovascular events, and increased risk of infective endocarditis. It is also usually associated with the other autoimmune diseases such as antiphospholipid syndrome (APS) and some malignancies. Secondary APS has a higher rate of cardiac involvement as compared to primary APS, mostly due to the autoimmune causes related to the SLE. LSE can be complicated by embolic cerebrovascular disease, superimposed infective endocarditis, and peripheral arterial embolism. It is also associated with increased mortality, hence, early recognition of LSE and appropriate treatment are of significant importance in preventing any further complications.
Historical Perspective
- In 1888, Zeigler was the first one to describe NBTE, and called it "thromboendocarditis" at that time.
- In 1924, the two American physicians Emanuel Libman, and Benjamin Sacks, working at Mount Sinai Hospital, New York, described the Libman-Sacks endocarditis for the first time, hence, it's named after them. They first presented the complete clinical picture of it with or without skin lesions and described it as unusual non-bacterial endocarditis with verrucous vegetations adherent to the endocardium.[1][2]
- In 1936, Gross and Friedberg finally coined the term "nonbacterial thrombotic endocarditis" (NBTE) for marantic/verrucous endocarditis.
- In 1983, Graham Hughes described the antiphospholipid antibody syndrome for the first time while working as a rheumatologist at St Thomas Hospital. He named it anticardiolipin syndrome (also known as Hughes syndrome named after him) and described it has the following three characteristics:[3]
- In 1985, the association between Libman-Sacks endocarditis and antiphospholipid antibody syndrome was noted for the first time.
- In 1989, four groups highlighted a probable role of antiphospholipid antibodies in the pathogenesis of valvular heart disease in SLE patients.
Pathophysiology
Pathology
- The pathology of Libman-Sacks endocarditis is the same as nonbacterial thrombotic endocarditis except that focal necrosis (seen in the form of hematoxylin bodies) is only found in Libman-Sacks endocarditis.
- Just like NBTE, Libman-Sacks endocarditis develops due to the endothelial damage and subsequent exposure of the sub-endothelial connective tissue to the circulating platelets.
- The factors involved in the pathogenesis can be divided into the ones initiating the Libman-Sacks endocarditis and the subsequent development of vegetations.[4]
| Initiation factor | Description |
|---|---|
| Immune complexes |
|
| Hypoxia | |
| Hypercoagulability |
|
| Carcinomatosis | Following carcinomas are commonly associated with NBTE and Libman-Sacks endocarditis: |
- The vegetations in Libman-Sacks endocarditis are formed from the strands consisting of the following four components:
- Most commonly affected valve is the mitral valve with the vegetations involving the ventricular and atrial surface of the valve.
- The lesions of Libman-Sacks endocarditis rarely lead to any significant valvular dysfunction and they only rarely embolize.[5][6][7][8][9][10][11][12]
Gross pathology
- Vegetations in Libman-Sacks endocarditis have the following typical features:
| Type of NBTE | Features |
|---|---|
| Type 1 |
|
| Type 2 | |
| Type 3 |
|
 |
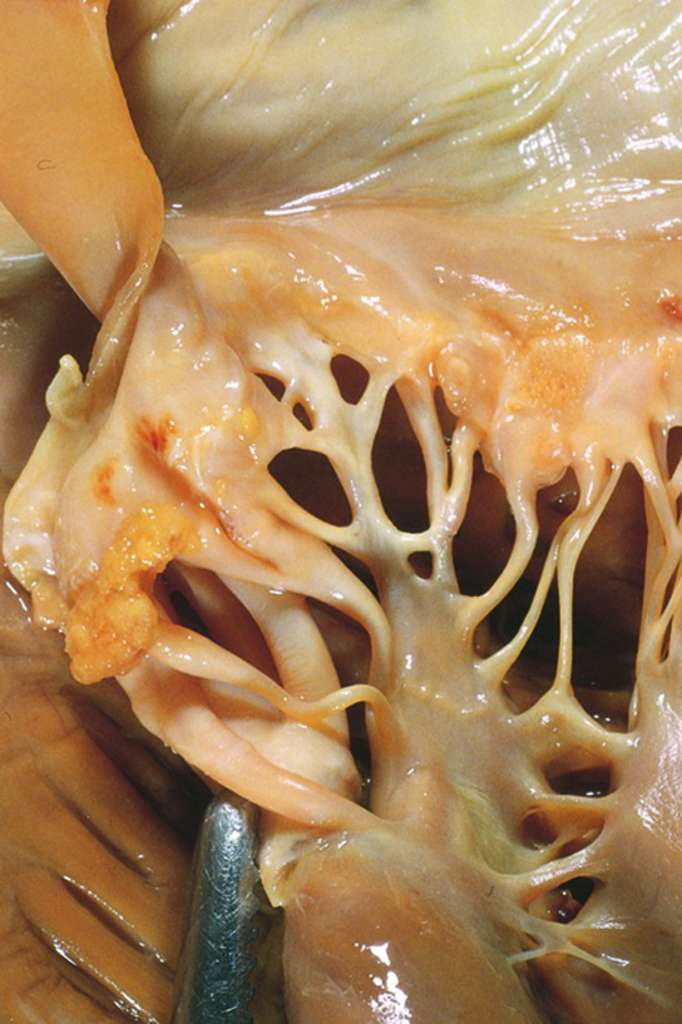 |
Microscopic Pathology
- Vegetations in Libman-Sacks endocarditis consist of degenerating platelets interwoven with the fibrin strands and form a bland, featureless eosinophilic mass except for a few trapped leukocytes.
- Following three stages have been described in the evolution of vegetations in Libman-Sacks endocarditis:[13]
| Stage | Description |
|---|---|
| Stage 1 (active verrucae) |
|
| Stage 2 (Combined active and healed lesions) | |
| Stage 3 (Healed lesions) |
|
Epidemiology and Demographics
- Approximately 1 out of 10 SLE patients have vegetations associated with Libman-Sacks endocarditis. Presence of these vegetations is indicative of the association with the following:[14][15]
- Lupus duration
- Disease activity
- Anticardiolipin antibodies
- APS manifestations
- There's a variable incidence of positive findings on transthoracic echocardiography.
- Higher incidence of detection of positive findings is shown with transesophageal echocardiography and especially with higher frequency with positive antiphospholipid antibodies.
- Thickening of the leaflets is more common as compared to finding vegetations.
- Positive findings on echocardiography are found in approximately one-third of the patients with antiphospholipid antibody syndrome.
- These positive findings are five to nine times more frequently found in women than men.
- Libman-sacks endocarditis typically occurs in young women, however, children can be rarely involved.
- Nonbacterial thrombotic endocarditis (NBTE) is a rare condition which is most often found during 0.9% to 1.6% of the postmortem studies.[16][17][18][19][20][21]
- NBTE affects every age group but most commonly involves patients between the fourth and eighth decades of life with no sex predilection.[22]
- NBTE most commonly affects patients with systemic lupus erythematosus and advanced malignancy.
- According to one autopsy study, patients with underlying malignancy have a higher rate (1.25%) of NBTE as compared to general population (0.2%).[23]
- NBTE is found at higher rates in patients with adenocarcinoma (e.g., lung, colon, ovary, biliary and prostate) (2.7%) as compared to other malignancies (0.47%), with the highest rates observed in patients with mucin-secreting and pancreatic adenocarcinoma (10%).[23][24]
- Observational studies in patients with systemic lupus erythematosus have reported 6% to 11% prevalence rates with transthoracic echocardiography, with higher rates (43%) observed with more sensitive transesophageal echocardiography.[25][26]
Risk Factors
- Following table shows important risk factors for the development of Libman-Sacks endocarditis:
| Risk factor | Details |
|---|---|
| Advanced stage malignancy | Advanced stage malignancies such as: |
| Chronic diseases | Chronic diseases such as: |
| Connective tissue disorders with hypercoagulable state |
|
| Trauma | Trauma due to: |
Natural History, Complications and Prognosis
Complications
- Systemic emboli may occur in Libman-Sacks endocarditis but not very commonly with the risk being much higher with mitral stenosis and subsequent atrial fibrillation.
- It is difficult to predict the underlying etiology in case of a stroke occurrence in LSE, whether it is due to systemic emboli or the underlying pathology of SLE or APS.
- Valvular disease in LSE can lead to the heart failure.
- Double-valve Libman-Sacks endocarditis involving both mitral and aortic valves can lead to ventricular fibrillation and cardiac arrest.[27]
- There's 1% to 2% chance of congenital heart block (usually complete,or 1st or 2nd degree) in a baby of mother with SLE associated with anti-Ro/SS-A (Sjögren's syndrome antigen A) autoantibodies with a 16% recurrence rate. Fluorinated steroids that do not cross the placenta may be beneficial in preventing the congenital heart block.
Prognosis
- All of the SLE patients have got a shorter life span.
- The occurrence of cardiovascular events is the major cause of mortality in SLE patients as SLE is a risk factor for premature & accelerated coronary atherosclerosis and CAD (coronary artery disease) due to the following associated factors:
Diagnosis
- Diagnosis of Libman-Sacks endocarditis requires a high degree of clinical suspicion especially in patients who don't improve clinically after being treated for infective endocarditis.[28]
- Mckay and Wahler proposed the following triad for the diagnosis of NBTE:
| Mckay and Wahler triad for diagnosis of NBTE | |
| 1: |
|
| 2: | |
| 3: |
|
History and Symptoms
- Mostly patients with Libman-Sacks endocarditis are asymptomatic.
- There may be the features of valvular disease if valves are severely affected with the mitral valve disease being more common than the aortic valve disease.
- Valvular regurgitation is more frequent than the valvular stenosis.
- Unusually, the tricuspid or pulmonary valves are involved.
- Systemic embolism may also occur with the effects depending upon the destination of the emboli with the brain and kidneys being more likely involved.
- Emboli can also lead to the blockage of peripheral circulation.
- The vegetations in Libman-Sacks endocarditis are mostly sterile but secondary infective endocarditis can also occur.
- There may or may not be the typical SLE features with the characteristic butterfly rash, fever, and arthritis or the APS features, including recurrent miscarriages.
| Manifestation | Description |
|---|---|
| Heart failure | Heart failure can occur secondary to the valvular dysfunction (most commonly mitral regurgitation), leading to the following signs and symptoms: |
| Cerebrovascular embolism[29] | Cerebrovascular embolism can present as any of the following:
|
| Systemic thromboembolism | Systemic thromboembolism can cause any of the following: |
| Secondary infective endocarditis | Secondary infective endocarditis can present as: |
Physical Examination
- A patient of Libman-Sacks endocarditis can present with any of the signs and symptoms shown in the following table:
Laboratory Findings
| Laboratory Investigations in Libman-Sacks Endocarditis | Laboratory test findings |
|---|---|
| Blood culture |
|
| SLE investigations
(Immunological assays) |
|
| CBC |
|
| Studies to rule out DIC | |
| Polymerase chain reaction (PCR) |
Imaging Findings
| Imaging tests in Libman-Sacks Endocarditis | Imagining Findings | ||
|---|---|---|---|
| Echocardiography[41][26][42] |
| ||
| Chest X-Ray |
| ||
| MRI[43] |
| ||
| CT scan (Head) |
|
Other Diagnostic Studies
Cardiac Catheterization
- In case of severe valvular disease, cardiac catheterization may be required with a view to valve replacement.
Treatment
- There is no specific treatment for Libman-Sacks endocarditis.
- Treatment of LSE is quite difficult with the main focus being on the correction of the underlying cause.
Differentiating Libman-Sacks Endocarditis from other Diseases
Libman-Sacks endocarditis should be differentiated from other diseases presenting with fever, chest pain and anorexia. The differentials include the following:[45][46][47][48][49][50][51][52][53][54][55][56][57][58][59][60][61][62][63][64]
| Diseases | Diagnostic tests | Physical Examination | Symptoms | Past medical history | Other Findings | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CT scan and MRI | EKG | Chest X-ray | Tachypnea | Tachycardia | Fever | Chest Pain | Hemoptysis | Dyspnea on Exertion | Wheezing | Chest Tenderness | Nasalopharyngeal Ulceration | Carotid Bruit | |||
| Pulmonary embolism |
|
|
|
✔ | ✔ | ✔ (Low grade) | ✔ | ✔ (In case of massive PE) | ✔ | - | - | - | - |
|
|
| Infective Endocarditis | ✔ | ✔ | ✔ | - | - | ✔ | - | - | - | - |
|
| |||
| Non-bacterial thrombotic endocarditis |
|
✔ | ✔ | ✔ (Low grade) | ✔ (Relieved by sitting up and leaning forward) | - | ✔ | - | - | - | - |
|
| ||
| Libman Sack Endocarditis |
|
✔ | ✔ | ✔ | ✔ | - | ✔ | ✔ | - | - | - |
|
| ||
| Vasculitis |
|
|
✔ | ✔ | ✔ | ✔ | ✔ | ✔ | - | ✔ | ✔ | ✔ |
|
||
| Fever of unknown origin (FUO) |
|
✔ | ✔ | - | - | - | ✔ | ✔ | - | - | - |
|
| ||
References
- ↑ Libman E, Sacks B: A hitherto undescribed form of valvular and mural endocarditis. Arch Intern Med 1924; 33: 701-37.
- ↑ Libman, Emanuel (1924). "A HITHERTO UNDESCRIBED FORM OF VALVULAR AND MURAL ENDOCARDITIS". Archives of Internal Medicine. 33 (6): 701. doi:10.1001/archinte.1924.00110300044002. ISSN 0003-9926.
- ↑ https://patient.info/doctor/libman-sacks-endocarditis#ref-14
- ↑ https://www.pathologyoutlines.com/topic/heartnontumornoninfecendo.html
- ↑ Mohammadi Kebar Y, Avesta L, Habibzadeh A, Hemmati M (2019). "Libman-Sacks endocarditis in patients with systemic lupus erythematosus with secondary antiphospholipid syndrome". Caspian J Intern Med. 10 (3): 339–342. doi:10.22088/cjim.10.3.339. PMC 6729157 Check
|pmc=value (help). PMID 31558998. - ↑ Murtaza G, Iskandar J, Humphrey T, Adhikari S, Kuruvilla A (2017). "Lupus-Negative Libman-Sacks Endocarditis Complicated by Catastrophic Antiphospholipid Syndrome". Cardiol Res. 8 (2): 57–62. doi:10.14740/cr534e. PMC 5421487. PMID 28515823.
- ↑ 7.0 7.1 Bouma W, Klinkenberg TJ, van der Horst IC, Wijdh-den Hamer IJ, Erasmus ME, Bijl M; et al. (2010). "Mitral valve surgery for mitral regurgitation caused by Libman-Sacks endocarditis: a report of four cases and a systematic review of the literature". J Cardiothorac Surg. 5: 13. doi:10.1186/1749-8090-5-13. PMC 2859362. PMID 20331896.
- ↑ Bai Z, Hou J, Ren W, Guo Y (2015). "Diagnosis and surgical treatment for isolated tricuspid Libman-Sacks endocarditis: a rare case report and literatures review". J Cardiothorac Surg. 10: 93. doi:10.1186/s13019-015-0302-1. PMC 4494164. PMID 26152222.
- ↑ "StatPearls". 2019. PMID 30422459.
- ↑ Wang Y, Ma C, Yang J, Liu S, Zhang Y, Zhao L; et al. (2015). "Libman-sacks endocarditis exclusively involving the tricuspid valve in a patient with systemic lupus erythematosus". J Clin Ultrasound. 43 (4): 265–267. doi:10.1002/jcu.22180. PMID 24925796.
- ↑ 11.0 11.1 Perier P, Jeserich M, Vieth M, Pohle K, Hohenberger W, Diegeler A (2011). "Mitral valve reconstruction in a patient with Libman-Sacks endocarditis: a case report". J Heart Valve Dis. 20 (1): 103–6. PMID 21404907.
- ↑ Bani Hani A, Abu-Abeeleh M, Al Kharabsheh MM, Qabba'ah L (2016). "Libman-Sacks Endocarditis with Unusual Large Size Vegetation Involving the Mitral Valve". Heart Surg Forum. 19 (6): E294–E296. doi:10.1532/hsf.1612. PMID 28054901.
- ↑ https://emedicine.medscape.com/article/155230-workup#showall
- ↑ https://patient.info/doctor/libman-sacks-endocarditis#ref-14
- ↑ Moyssakis I, Tektonidou MG, Vasilliou VA, Samarkos M, Votteas V, Moutsopoulos HM (2007). "Libman-Sacks endocarditis in systemic lupus erythematosus: prevalence, associations, and evolution". Am J Med. 120 (7): 636–42. doi:10.1016/j.amjmed.2007.01.024. PMID 17602939.
- ↑ Deppisch LM, Fayemi AO (1976). "Non-bacterial thrombotic endocarditis: clinicopathologic correlations". Am Heart J. 92 (6): 723–9. doi:10.1016/s0002-8703(76)80008-7. PMID 998478.
- ↑ Rosen P, Armstrong D (1973). "Nonbacterial thrombotic endocarditis in patients with malignant neoplastic diseases". Am J Med. 54 (1): 23–9. doi:10.1016/0002-9343(73)90079-x. PMID 4682494.
- ↑ Llenas-García J, Guerra-Vales JM, Montes-Moreno S, López-Ríos F, Castelbón-Fernández FJ, Chimeno-García J (2007). "[Nonbacterial thrombotic endocarditis: clinicopathologic study of a necropsy series]". Rev Esp Cardiol. 60 (5): 493–500. PMID 17535760.
- ↑ Eiken PW, Edwards WD, Tazelaar HD, McBane RD, Zehr KJ (2001). "Surgical pathology of nonbacterial thrombotic endocarditis in 30 patients, 1985-2000". Mayo Clin Proc. 76 (12): 1204–12. doi:10.4065/76.12.1204. PMID 11761501.
- ↑ Mazokopakis EE, Syros PK, Starakis IK (2010). "Nonbacterial thrombotic endocarditis (marantic endocarditis) in cancer patients". Cardiovasc Hematol Disord Drug Targets. 10 (2): 84–6. doi:10.2174/187152910791292484. PMID 20397972.
- ↑ Lopez JA, Ross RS, Fishbein MC, Siegel RJ (1987). "Nonbacterial thrombotic endocarditis: a review". Am Heart J. 113 (3): 773–84. doi:10.1016/0002-8703(87)90719-8. PMID 3548296.
- ↑ el-Shami K, Griffiths E, Streiff M (2007). "Nonbacterial thrombotic endocarditis in cancer patients: pathogenesis, diagnosis, and treatment". Oncologist. 12 (5): 518–23. doi:10.1634/theoncologist.12-5-518. PMID 17522239.
- ↑ 23.0 23.1 González Quintela A, Candela MJ, Vidal C, Román J, Aramburo P (1991). "Non-bacterial thrombotic endocarditis in cancer patients". Acta Cardiol. 46 (1): 1–9. PMID 1851590.
- ↑ Borowski A, Ghodsizad A, Cohnen M, Gams E (2005). "Recurrent embolism in the course of marantic endocarditis". Ann Thorac Surg. 79 (6): 2145–7. doi:10.1016/j.athoracsur.2003.12.024. PMID 15919332.
- ↑ Roldan CA, Shively BK, Crawford MH (1996). "An echocardiographic study of valvular heart disease associated with systemic lupus erythematosus". N Engl J Med. 335 (19): 1424–30. doi:10.1056/NEJM199611073351903. PMID 8875919.
- ↑ 26.0 26.1 Roldan CA, Qualls CR, Sopko KS, Sibbitt WL (2008). "Transthoracic versus transesophageal echocardiography for detection of Libman-Sacks endocarditis: a randomized controlled study". J Rheumatol. 35 (2): 224–9. PMID 18085739.
- ↑ Tanawuttiwat T, Dia M, Hanif T, Mihailescu M (2011). "Double-valve Libman-Sacks endocarditis causing ventricular fibrillation cardiac arrest". Tex Heart Inst J. 38 (3): 295–7. PMC 3113142. PMID 21720477.
- ↑ Ménard GE (2008). "Establishing the diagnosis of Libman-Sacks endocarditis in systemic lupus erythematosus". J Gen Intern Med. 23 (6): 883–6. doi:10.1007/s11606-008-0627-8. PMC 2517866. PMID 18421506.
- ↑ Roldan CA, Sibbitt WL, Qualls CR, Jung RE, Greene ER, Gasparovic CM; et al. (2013). "Libman-Sacks endocarditis and embolic cerebrovascular disease". JACC Cardiovasc Imaging. 6 (9): 973–83. doi:10.1016/j.jcmg.2013.04.012. PMC 3941465. PMID 24029368.
- ↑ https://www.medscape.com/answers/241381-7641/what-are-signs-of-left-ventricular-hypertrophy-lvh-in-cardiac-exam-of-hypertension-high-blood-pressure
- ↑ Okin PM, Devereux RB, Nieminen MS, Jern S, Oikarinen L, Viitasalo M; et al. (2001). "Relationship of the electrocardiographic strain pattern to left ventricular structure and function in hypertensive patients: the LIFE study. Losartan Intervention For End point". J Am Coll Cardiol. 38 (2): 514–20. doi:10.1016/s0735-1097(01)01378-x. PMID 11499746.
- ↑ Pinto IJ, Nanda NC, Biswas AK, Parulkar VG (1967). "Tall upright T waves in the precordial leads". Circulation. 36 (5): 708–16. doi:10.1161/01.cir.36.5.708. PMID 4227953.
- ↑ Okin PM, Devereux RB, Fabsitz RR, Lee ET, Galloway JM, Howard BV; et al. (2002). "Quantitative assessment of electrocardiographic strain predicts increased left ventricular mass: the Strong Heart Study". J Am Coll Cardiol. 40 (8): 1395–400. doi:10.1016/s0735-1097(02)02171-x. PMID 12392827.
- ↑ Shah AS, Chin CW, Vassiliou V, Cowell SJ, Doris M, Kwok TC; et al. (2014). "Left ventricular hypertrophy with strain and aortic stenosis". Circulation. 130 (18): 1607–16. doi:10.1161/CIRCULATIONAHA.114.011085. PMID 25170097.
- ↑ Mehta A, Jain AC, Mehta MC, Billie M (2000). "Usefulness of left atrial abnormality for predicting left ventricular hypertrophy in the presence of left bundle branch block". Am J Cardiol. 85 (3): 354–9. doi:10.1016/s0002-9149(99)00746-8. PMID 11078306.
- ↑ https://emedicine.medscape.com/article/216650-clinical
- ↑ Jingushi N, Iwata M, Terasawa T (2017). "Clinical features of patients with infective endocarditis presenting to the emergency department: a retrospective case series". Nagoya J Med Sci. 79 (4): 467–476. doi:10.18999/nagjms.79.4.467. PMC 5719206. PMID 29238103.
- ↑ Hoen B, Duval X (2013). "Clinical practice. Infective endocarditis". N Engl J Med. 368 (15): 1425–33. doi:10.1056/NEJMcp1206782. PMID 23574121.
- ↑ Cahill TJ, Prendergast BD (2016). "Infective endocarditis". Lancet. 387 (10021): 882–93. doi:10.1016/S0140-6736(15)00067-7. PMID 26341945.
- ↑ Hojnik, Maja; George, Jacob; Ziporen, Lea; Shoenfeld, Yehuda (1996). "Heart Valve Involvement (Libman-Sacks Endocarditis) in the Antiphospholipid Syndrome". Circulation. 93 (8): 1579–1587. doi:10.1161/01.CIR.93.8.1579. ISSN 0009-7322.
- ↑ Roldan CA, Tolstrup K, Macias L, Qualls CR, Maynard D, Charlton G; et al. (2015). "Libman-Sacks Endocarditis: Detection, Characterization, and Clinical Correlates by Three-Dimensional Transesophageal Echocardiography". J Am Soc Echocardiogr. 28 (7): 770–9. doi:10.1016/j.echo.2015.02.011. PMC 4592775. PMID 25807885.
- ↑ Roldan CA (2009). "Diagnostic value of transesophageal echocardiography in Libman-Sacks endocarditis". Minerva Cardioangiol. 57 (4): 467–81. PMID 19763069.
- ↑ https://radiopaedia.org/articles/libman-sacks-endocarditis-1?lang=us
- ↑ Samura T, Toda K, Yoshioka D, Nakamura T, Miyagawa S, Yoshikawa Y; et al. (2017). "Libman-Sacks Endocarditis Due to Systemic Lupus Erythematosus Activation After Mitral Valve Plasty". Ann Thorac Surg. 104 (2): e109–e111. doi:10.1016/j.athoracsur.2017.01.073. PMID 28734427.
- ↑ Brenes-Salazar JA (2014). "Westermark's and Palla's signs in acute and chronic pulmonary embolism: Still valid in the current computed tomography era". J Emerg Trauma Shock. 7 (1): 57–8. doi:10.4103/0974-2700.125645. PMC 3912657. PMID 24550636.
- ↑ "CT Angiography of Pulmonary Embolism: Diagnostic Criteria and Causes of Misdiagnosis | RadioGraphics".
- ↑ Bĕlohlávek J, Dytrych V, Linhart A (2013). "Pulmonary embolism, part I: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism". Exp Clin Cardiol. 18 (2): 129–38. PMC 3718593. PMID 23940438.
- ↑ "Pulmonary Embolism: Symptoms - National Library of Medicine - PubMed Health".
- ↑ Ramani GV, Uber PA, Mehra MR (2010). "Chronic heart failure: contemporary diagnosis and management". Mayo Clin. Proc. 85 (2): 180–95. doi:10.4065/mcp.2009.0494. PMC 2813829. PMID 20118395.
- ↑ Blinderman CD, Homel P, Billings JA, Portenoy RK, Tennstedt SL (2008). "Symptom distress and quality of life in patients with advanced congestive heart failure". J Pain Symptom Manage. 35 (6): 594–603. doi:10.1016/j.jpainsymman.2007.06.007. PMC 2662445. PMID 18215495.
- ↑ Hawkins NM, Petrie MC, Jhund PS, Chalmers GW, Dunn FG, McMurray JJ (2009). "Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology". Eur. J. Heart Fail. 11 (2): 130–9. doi:10.1093/eurjhf/hfn013. PMC 2639415. PMID 19168510.
- ↑ Takasugi JE, Godwin JD (1998). "Radiology of chronic obstructive pulmonary disease". Radiol. Clin. North Am. 36 (1): 29–55. PMID 9465867.
- ↑ Wedzicha JA, Donaldson GC (2003). "Exacerbations of chronic obstructive pulmonary disease". Respir Care. 48 (12): 1204–13, discussion 1213–5. PMID 14651761.
- ↑ Nakawah MO, Hawkins C, Barbandi F (2013). "Asthma, chronic obstructive pulmonary disease (COPD), and the overlap syndrome". J Am Board Fam Med. 26 (4): 470–7. doi:10.3122/jabfm.2013.04.120256. PMID 23833163.
- ↑ Khandaker MH, Espinosa RE, Nishimura RA, Sinak LJ, Hayes SN, Melduni RM, Oh JK (2010). "Pericardial disease: diagnosis and management". Mayo Clin. Proc. 85 (6): 572–93. doi:10.4065/mcp.2010.0046. PMC 2878263. PMID 20511488.
- ↑ Bogaert J, Francone M (2013). "Pericardial disease: value of CT and MR imaging". Radiology. 267 (2): 340–56. doi:10.1148/radiol.13121059. PMID 23610095.
- ↑ Gharib AM, Stern EJ (2001). "Radiology of pneumonia". Med. Clin. North Am. 85 (6): 1461–91, x. PMID 11680112.
- ↑ Schmidt WA (2013). "Imaging in vasculitis". Best Pract Res Clin Rheumatol. 27 (1): 107–18. doi:10.1016/j.berh.2013.01.001. PMID 23507061.
- ↑ Suresh E (2006). "Diagnostic approach to patients with suspected vasculitis". Postgrad Med J. 82 (970): 483–8. doi:10.1136/pgmj.2005.042648. PMC 2585712. PMID 16891436.
- ↑ Stein PD, Dalen JE, McIntyre KM, Sasahara AA, Wenger NK, Willis PW (1975). "The electrocardiogram in acute pulmonary embolism". Prog Cardiovasc Dis. 17 (4): 247–57. PMID 123074.
- ↑ Warnier MJ, Rutten FH, Numans ME, Kors JA, Tan HL, de Boer A, Hoes AW, De Bruin ML (2013). "Electrocardiographic characteristics of patients with chronic obstructive pulmonary disease". COPD. 10 (1): 62–71. doi:10.3109/15412555.2012.727918. PMID 23413894.
- ↑ Stein PD, Matta F, Ekkah M, Saleh T, Janjua M, Patel YR, Khadra H (2012). "Electrocardiogram in pneumonia". Am. J. Cardiol. 110 (12): 1836–40. doi:10.1016/j.amjcard.2012.08.019. PMID 23000104.
- ↑ Hazebroek MR, Kemna MJ, Schalla S, Sanders-van Wijk S, Gerretsen SC, Dennert R, Merken J, Kuznetsova T, Staessen JA, Brunner-La Rocca HP, van Paassen P, Cohen Tervaert JW, Heymans S (2015). "Prevalence and prognostic relevance of cardiac involvement in ANCA-associated vasculitis: eosinophilic granulomatosis with polyangiitis and granulomatosis with polyangiitis". Int. J. Cardiol. 199: 170–9. doi:10.1016/j.ijcard.2015.06.087. PMID 26209947.
- ↑ Dennert RM, van Paassen P, Schalla S, Kuznetsova T, Alzand BS, Staessen JA, Velthuis S, Crijns HJ, Tervaert JW, Heymans S (2010). "Cardiac involvement in Churg-Strauss syndrome". Arthritis Rheum. 62 (2): 627–34. doi:10.1002/art.27263. PMID 20112390.
Template:Diseases of the musculoskeletal system and connective tissue