Asystole
| Resident Survival Guide |
|
WikiDoc Resources for Asystole |
|
Articles |
|---|
|
Most recent articles on Asystole |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Asystole at Clinical Trials.gov Clinical Trials on Asystole at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Asystole
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Asystole Risk calculators and risk factors for Asystole
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Asystole |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Asystole is a state of no cardiac electrical activity, hence no contractions of the myocardium and no cardiac output or blood flow. Asystole is one of the conditions required for a medical practitioner to certify death.
In asystole, the heart will not respond to defibrillation because it is already depolarized, however some emergency physicians advocate a trial of defibrillation in case the rhythm is actually fine ventricular fibrillation, although little evidence exists to support the practice. Asystole is usually a confirmation of death as opposed to a heart rhythm to be treated, although a small minority of patients are successfully resuscitated, if the underlying cause is identified and treated immediately.
Causes
Common Causes
Possible underlying causes include the Hs and Ts.[1][2][3]
- Hypovolemia
- Hypoxia
- Acidosis
- Hypothermia
- Hyperkalemia or Hypokalemia
- Hypoglycemia
- Cardiac Tamponade
- Tension pneumothorax
- Thrombosis
- Myocardial infarction
- Thrombosis
- Pulmonary embolism
- Cardiogenic shock
- Degeneration of the sinoatrial or atrioventricular nodes
- Ischemic stroke
Causes by Organ System
| Cardiovascular | Cardiogenic shock, Degeneration of the sinoatrial or atrioventricular nodes, Ischemic stroke, Myocardial infarction, Pacemaker failure, Pulmonary embolism, Thrombosis |
| Chemical/Poisoning | No underlying causes |
| Dental | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | No underlying causes |
| Ear Nose Throat | No underlying causes |
| Endocrine | Hypoglycemia |
| Environmental | Hypothermia, Lightning strike |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | Hypovolemia, Hypoxia |
| Iatrogenic | No underlying causes |
| Infectious Disease | No underlying causes |
| Musculoskeletal/Orthopedic | No underlying causes |
| Neurologic | No underlying causes |
| Nutritional/Metabolic | No underlying causes |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | No underlying causes |
| Ophthalmologic | No underlying causes |
| Overdose/Toxicity | Drug overdose |
| Psychiatric | No underlying causes |
| Pulmonary | Drowning, Pulmonary embolism, Tension pneumothorax |
| Renal/Electrolyte | Hyperkalemia, hypokalemia |
| Rheumatology/Immunology/Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | Trauma |
| Urologic | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
- Acidosis
- Beta blockers
- Cardiac tamponade
- Cardiogenic shock
- Degeneration of the sinoatrial or atrioventricular nodes
- Drowning
- Drug overdose
- Hyperkalemia
- Hypokalemia
- Hypoglycemia
- Hypothermia
- Hypovolemia
- Hypoxia
- Ischemic stroke
- Lightning strike
- Myocardial infarction
- Pacemaker failure
- Pulmonary embolism
- Tension pneumothorax
- Thrombosis
- Trauma
Diagnosis
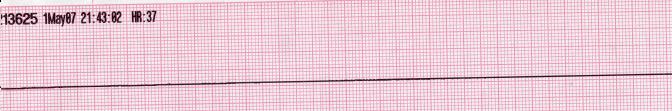
Electrocardigram
Shown below are EKGs depicting asystole.

Treatment
Medical Therapy
It is important to exclude fine ventricular fibrillation in the patient presumed to have asystole. If VF is present, then cardioversion should be performed.
While the heart is asystolic, there is no blood flow to the brain unless CPR or internal cardiac massage (when the chest is opened and the heart is manually compressed) is performed, and even then, it is still a small amount. After many emergency treatments have been applied but the heart is still unresponsive, it is time to consider pronouncing the patient dead. Even in the rare case that a rhythm should reappear, if asystole has persisted for fifteen minutes or more the brain will have been deprived of oxygen long enough to cause brain death.
Related Chapters
References
- ↑ ACLS: Principles and Practice. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.
- ↑ ACLS for Experienced Providers. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.
- ↑ "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." Circulation 2005; 112: IV-58 - IV-66.
da:Asystoli
de:Asystolie
nl:Asystolie
sv:Asystoli
ur:لا انقباض