Defibrillation
|
WikiDoc Resources for Defibrillation |
|
Articles |
|---|
|
Most recent articles on Defibrillation Most cited articles on Defibrillation |
|
Media |
|
Powerpoint slides on Defibrillation |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Defibrillation at Clinical Trials.gov Trial results on Defibrillation Clinical Trials on Defibrillation at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Defibrillation NICE Guidance on Defibrillation
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Defibrillation Discussion groups on Defibrillation Patient Handouts on Defibrillation Directions to Hospitals Treating Defibrillation Risk calculators and risk factors for Defibrillation
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Defibrillation |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Defibrillation is the definitive treatment for the life-threatening cardiac arrhythmias ventricular fibrillation and pulseless ventricular tachycardia. Defibrillation consists of delivering a therapeutic dose of electrical energy to the affected heart with a device called a defibrillator. This depolarizes a critical mass of the heart muscle, terminates the arrhythmia, and allows normal sinus rhythm to be reestablished by the body's natural pacemaker, in the sinoatrial node of the heart.
Defibrillators can be external, transvenous, or implanted, depending on the type of device used. Some external units, known as automated external defibrillators (AEDs), automate the diagnosis of treatable rhythms, meaning that lay responders or bystanders are able to use them successfully with little, or in some cases no, training.
Historical Perspective
Defibrillation was first demonstrated in 1899 by Prevost and Batelli, two physiologists from University of Geneva, Switzerland. They discovered that small electric shocks could induce ventricular fibrillation in dogs, and that larger charges would reverse the condition.
The first use on a human was in 1947 by Claude Beck,[1] professor of surgery at Western Reserve University. Beck's theory was that ventricular fibrillation often occurred in hearts which were fundamentally healthy, in his terms "Heart too good to die", and that there must be a way of saving them. Beck first used the technique successfully on a 14 year old boy who was being operated on for a congenital chest defect. The boy's chest was surgically opened, and manual cardiac massage was undertaken for 45 minutes until the arrival of the defibrillator. Beck used internal paddles either side of the heart, along with procaine amide, a heart drug, and achieved return of normal sinus rhythm.
These early defibrillators used the alternating current from a power socket, transformed from the 110-240 volts available in the line, up to between 300 and 1000 volts, to the exposed heart by way of 'paddle' type electrodes. The technique was often ineffective in reverting VF while morphological studies showed damage to the cells of the heart muscle post mortem. The nature of the AC machine with a large transformer also made these units very hard to transport, and they tended to be large units on wheels.
Closed-Chest Method
Until the early 1950s, defibrillation of the heart was possible only when the chest cavity was open during surgery. The technique used an alternating current from a 300 or greater volts source delivered to the sides of the exposed heart by 'paddle' electrodes where each electrode was a flat or slightly concave metal plate of about 40 mm diameter. The closed-chest defibrillator device which applied an alternating current of greater than 1000 volts, conducted by means of externally applied electrodes through the chest cage to the heart, was pioneered by Dr V. Eskin with assistance by A. Klimov in Frunze, USSR in mid 1950s.[2]
Move to Direct Current
In 1959 Bernard Lown commenced research into an alternative technique which involved charging of a bank of capacitors to approximately 1000 Volts with an energy content of 100-200 Joules then delivering the charge through an inductance such as to produce a heavily damped sinusoidal wave of finite duration (~5 milliseconds) to the heart by way of 'paddle' electrodes. The work of Lown was taken to clinical application by engineer Barouh Berkovits with his "cardioverter".
The Lown waveform, as it was known, was the standard for defibrillation until the late 1980s when numerous studies showed that a biphasic truncated waveform (BTE) was equally efficacious while requiring the delivery of lower levels of energy to produce defibrillation. A side effect was a significant reduction in weight of the machine. The BTE waveform, combined with automatic measurement of transthoracic impedance is the basis for modern defibrillators.
Portable Units Become Available
A major breakthrough was the introduction of portable defibrillators in ambulances. This was pioneered in the early 1960s by Prof. Frank Pantridge in Belfast. Today portable defibrillators are one of the most important tools carried by ambulances. They are the only proven way to resuscitate a person who has had a cardiac arrest unwitnessed by EMS who is still in persistent ventricular fibrillation or ventricular tachycardia at the arrival of pre-hospital providers.
Gradual improvements in the design of defibrillators, and partly based on the work developing implanted versions (see below) have lead to the availability of Automated External Defibrillators, which can analyze the heart rhythm by themselves, diagnosing the shockable rhythms, and then charging to treat. This means that no clinical skill is required in their use, allowing lay people to respond to emergencies effectively.
Change to a Biphasic Waveform
Until the late 1980s, external defibrillators delivered a Lown type waveform (see Bernard Lown) which was a heavily damped sinusoidal impulse having a mainly uniphasic characteristic. Biphasic defibrillation, however, alternates the direction of the pulses, completing one cycle in approximately 10 milliseconds. Biphasic defibrillation was originally developed and used for implantable cardioverter-defibrillators. When applied to external defibrillators, biphasic defibrillation significantly decreases the energy level necessary for successful defibrillation. This, in turn, decreases risk of burns and myocardial damage.
Ventricular fibrillation (VF) could be returned to normal sinus rhythm in 60% of cardiac arrest patients treated with a single shock from a monophasic defibrillator. Most biphasic defibrillators have a first shock success rate of greater than 90%.[3]
Implantable Devices
A further development in defibrillation came with the invention of the implantable device, known as an implantable cardioverter-defibrillator (or ICD). This was pioneered at Sinai Hospital in Baltimore by a team including Stephen Heilman, Alois Langer, Morton Mower, Michel Mirowski, and Mir Imran, with the help of industrial collaborator Intec Systems of Pittsburgh. Mirowski teamed up with Mower and Staewen, and together they commenced their research in 1969 but it was 11 years before they treated their first patient. Similar developmental work was carried out by Schuder and colleagues at the University of Missouri.
The work was commenced, despite doubts amongst leading experts in the field of arrhythmias and sudden death. There was doubt that their ideas would ever become a clinical reality. In 1972 Bernard Lown, the inventor of the external defibrillator, stated in the journal Circulation - "The very rare patient who has frequent bouts of ventricular fibrillation is best treated in a coronary care unit and is better served by an effective antiarrhythmic program or surgical correction of inadequate coronary blood flow or ventricular malfunction. In fact, the implanted defibrillator system represents an imperfect solution in search of a plausible and practical application."
The problems to be overcome were the design of a system which would allow detection of ventricular fibrillation or ventricular tachycardia. Despite the lack of financial backing and grants, they persisted and the first device was implanted in February 1980 at Johns Hopkins Hospital by Dr. Levi Watkins, Jr. Modern ICDs do not require a thoracotomy and possess pacing, cardioversion, and defibrillation capabilities.
The invention of implantable units is invaluable to some regular sufferers of heart problems, although they are generally only given to those people who have already had a cardiac episode.
Types
Manual External Defibrillator
The units are used in conjunction with (or more often have inbuilt) electrocardiogram readers, which the clinician uses to diagnose a cardiac condition (most often fibrillation or tachycardia although there are some other rhythms which can be treated by different shocks). The clinician will then decide what charge (voltage) to use, based on their prior knowledge and experience, and will deliver the shock through paddles or pads on the patient's chest. As they require detailed medical knowledge, these units are generally only found in hospitals and on some ambulances. For instance, every NHS ambulance in the United Kingdom is equipped with a manual defibrillator for use by the attending Paramedics and Technicians.
Manual Internal Defibrillator
These are the direct descendants of the work of Beck and Lown. They are virtually identical to the external version, except that the charge is delivered through internal paddles in direct contact with the heart. These are almost exclusively found in operating theatres, where the chest is likely to be open, or can be opened quickly by a surgeon.
Automated External Defibrillator (AED)
These simple to use units are based on computer technology which is designed to analyze the heart rhythm itself, and then advise whether a shock is required. They are designed to be used by lay persons, who require little training. They are usually limited in their interventions to delivering high joule shocks for VF and VT rhythms, making them generally limiting for use by health professionals, who could diagnose and treat a wider range of problems with a manual or semi-automatic unit.
The automatic units also take time (generally 10-20 seconds) to diagnose the rhythm, where a professional could diagnose and treat the condition far quicker with a manual unit. These time intervals for analysis, which require stopping chest compressions, have been shown in a number of studies to have a significant negative effect on shock success. This effect led to the recent change in the AHA defibrillation guideline (calling for two minutes of CPR after each shock without analyzing the cardiac rhythm) and a statement in the ACLS Provider Manual that AEDs should not be used when manual defibrillators and trained operators are available.
Automated external defibrillators are generally either held by trained personnel who will attend incidents, or are public access units which can be found in places including corporate and government offices, shopping centers, airports, restaurants, casinos, hotels, sports stadiums, schools and universities, community centers, fitness centers and health clubs.
The locating of a public access AED should take in to account where large groups of people gather, and the risk category associated with these people, to ascertain whether the risk of a sudden cardiac arrest incident is high. For example, a center for teenage children is a particularly low risk category (as children very rarely enter heart rhythms such as VF or VT, being generally young and fit, and the most common cause of pediatric cardiac arrest is trauma - where the heart is more likely to enter asystole or PEA, where an AED is no use), whereas a large office building with a high ratio of males over 50 is a very high risk environment.
In many areas, emergency services vehicles are likely to carry AEDs, with some ambulances carrying an AED in addition to a manual unit. In addition, some police or fire service vehicles carry an AED for first responder use. Some areas have dedicated community first responders, who are volunteers tasking with keeping an AED and taking it to any victims in their area. It is also increasingly common to find AEDs on transport such as commercial airlines and cruise ships.
In order to make them highly visible, public access AEDs often are brightly colored, and are mounted in protective cases near the entrance of a building. When these protective cases are opened, and the defibrillator removed, some will sound a buzzer to alert nearby staff to their removal but do not necessarily summon emergency services. All trained AED operators should also know to phone for an ambulance when sending for or using an AED, as the patient will be unconscious, which always requires ambulance attendance.
Semi-Automated External Defibrillators
These units are a compromise between a full manual unit and an automated unit. They are mostly used by pre-hospital care professionals such as paramedics and emergency medical technicians. These units have the automated capabilities of the AED but also feature an ECG display, and a manual override, where the clinician can make their own decision, either before or instead of the computer. Some of these units are also able to act as a pacemaker if the heart rate is too slow (bradycardia) and perform other functions which require a skilled operator.
Implantable Cardioverter-Defibrillator (ICD)
Also known as Automatic Internal Cardiac Defibrillator (AICD). These devices are implants, similar to pacemakers (and many can also perform the pacemaking function). They constantly monitor the patient's heart rhythm, and automatically administer shocks for various life threatening arrhythmias, according to the device's programming. Many modern devices can distinguish between ventricular fibrillation, ventricular tachycardia, and more benign arrhythmias like supraventricular tachycardia and atrial fibrillation. Some devices may attempt overdrive pacing prior to synchronized cardioversion. When the life threatening arrhythmia is ventricular fibrillation, the device is programmed to proceed immediately to an unsynchronized shock.
There are cases where the patient's ICD may fire constantly or inappropriately This is considered a medical emergency, as it depletes the device's battery life, causes significant discomfort and anxiety to the patient, and in some cases may actually trigger life threatening arrhythmias. Some emergency medical services personnel are now equipped with a ring magnet to place over the device, which effectively disables the shock function of the device while still allowing the pacemaker to function (if the device is so equipped). If the device is shocking frequently, but appropriately, EMS personnel may administer sedation.
-
A circuit diagram showing the simplest (non-electronically controlled) defibrillator design, depending on the inductor ( damping ), producing a Lown, Edmark or Gurvich Waveform
-
An automated external defibrillator, open and ready for pads to be attached
-
An AED at a railway station in Japan. The AED box has information on how to use it in Japanese, English, Chinese and Korean, and station staff are trained to use it.
-
External defibrillator / monitor
Interface With The Patient
The most well-known type of electrode is the traditional metal paddle with an insulated handle. This type must be held in place on the patient's skin while a shock or a series of shocks is delivered. Before the paddle is used, a gel must be applied to the patient's skin, in order to ensure a good connection and to minimize electrical resistance, also called chest impedance (despite the DC discharge). These are generally only found on the manual external units.
Another type of resuscitation electrode is designed as an adhesive pad. When a patient has been admitted due to heart problems, and the physician or nurse has determined that he or she is at risk of arrhythmia, they may apply adhesive electrodes to the patient in anticipation of any problems that may arise. These electrodes are left connected to a defibrillator. If defibrillation is required, the machine is charged, and the shock is delivered, without any need to apply any gel or to retrieve and place any paddles. These adhesive pads are found on most automated and semi-automated units.
Both solid- and wet-gel adhesive electrodes are available. Solid-gel electrodes are more convenient, because there is no need to clean the patient's skin after removing the electrodes. However, the use of solid-gel electrodes presents a higher risk of burns during defibrillation, since wet-gel electrodes more evenly conduct electricity into the body.
Adhesive electrodes are designed to be used not only for defibrillation, but also for non-invasive pacing and electrical cardioversion.
While the paddles on a Monitor/Defibrillator may be quicker than using the patches, adhesive patches are superior due to their ability to provide appropriate EKG tracing without the artifact visible from human interference with the paddles. Adhesive electrodes are also inherently safer than the paddles for the operator of the defibrillator to use, as they minimize the risk of the operator coming into physical (and thus electrical) contact with the patient as the shock is delivered, by allowing the operator to stand several feet away. Another inconvenience of the paddles is the requirement of around 25lbs of pressure to be applied while defibrillating.
Placement
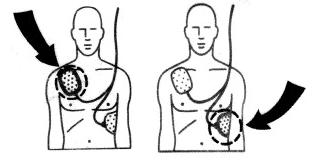
Resuscitation electrodes are placed according to one of two schemes. The anterior-posterior scheme (conf. image) is the preferred scheme for long-term electrode placement. One electrode is placed over the left precordium (the lower part of the chest, in front of the heart). The other electrode is placed on the back, behind the heart in the region between the scapula. This placement is preferred because it is best for non-invasive pacing.
The anterior-apex scheme can be used when the anterior-posterior scheme is inconvenient or unnecessary. In this scheme, the anterior electrode is placed on the right, below the clavicle. The apex electrode is applied to the left side of the patient, just below and to the left of the pectoral muscle. This scheme works well for defibrillation and cardioversion, as well as for monitoring an ECG.
Related Chapters
- Advanced cardiac life support (ACLS)
- Ambulance
- Automated external defibrillator
- Cardiopulmonary resuscitation (CPR)
- Cardioversion
- Heart Attack
- Implantable cardioverter-defibrillator
References
- ↑ "Claude Beck, defibrillation and CPR". Case Western Reserve University.
- ↑ Sov Zdravookhr Kirg. "Some results with the use of the DPA-3 defibrillator (developed by V. Ia. Eskin and A. M. Klimov) in the treatment of terminal states" (in Russian).
- ↑ Heart Smarter: EMS Implications of the 2005 AHA Guidelines for ECC & CPR pp 15-16
External Links
- American Red Cross: Saving a Life is as Easy as A-E-D
- FDA Heart Health Online: Automated External Defibrillator (AED)
cs:Defibrilátor
de:Defibrillation
de:Defibrillator
it:Defibrillazione
he:דפיברילטור
lb:Defibrillator
nl:Defibrillator
no:Defibrillering
no:Defibrillator
simple:Defibrillation
sr:Дефибрилатор
sr:Дефибрилација
fi:Defibrillaattori
sv:Defibrillator
sv:Defibrillering



