Hashimoto's thyroiditis: Difference between revisions
m (Robot: Automated text replacement (-{{SIB}} + & -{{EH}} + & -{{EJ}} + & -{{Editor Help}} + & -{{Editor Join}} +)) |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Infobox_Disease | | {{Infobox_Disease | | ||
Name = Hashimoto's thyroiditis | | Name = Hashimoto's thyroiditis | | ||
| Line 17: | Line 18: | ||
{{SI}} | {{SI}} | ||
''Synonyms and Related Keywords:'' Hashimoto's thyroiditis; | {{CMG}} '''Associate Editor-In-Chief:''' {{CZ}} | ||
''Synonyms and Related Keywords:'' Hashimoto's thyroiditis; chronic lymphocytic thyroiditis; autoimmune thyroiditis | |||
==Overview== | ==Overview== | ||
| Line 27: | Line 27: | ||
'''Hashimoto's thyroiditis''' or '''chronic lymphocytic thyroiditis''' is an [[autoimmune disease]] where the body's own [[antibody|antibodies]] attack the [[cell (biology)|cell]]s of the [[thyroid]]. | '''Hashimoto's thyroiditis''' or '''chronic lymphocytic thyroiditis''' is an [[autoimmune disease]] where the body's own [[antibody|antibodies]] attack the [[cell (biology)|cell]]s of the [[thyroid]]. | ||
==Historical Perspective== | |||
Also known as '''Hashimoto's disease''', Hashimoto's thyroiditis is named after the Japanese physician [[Hashimoto Hakaru]] (1881−1934) of the medical school at Kyushu University,<ref>{{WhoNamedIt|doctor|1974|Hakaru Hashimoto}}</ref> who first described (He described four patients with a chronic disorder of the thyroid, which he termed struma lymphomatosa. | |||
In | The thyroid glands of these patients were characterized by diffuse lymphocytic infiltration, fibrosis, parenchymal atrophy, and an eosinophilic change in some of the acinar cells) the symptoms in 1912 in a German publication <ref>H. Hashimoto: ''Zur Kenntnis der lymphomatösen Veränderung der Schilddrüse (Struma lymphomatosa).'' Archiv für klinische Chirurgie, Berlin, 1912, 97: 219−248.</ref>. | ||
== Pathophysiology== | |||
Hashimoto's thyroiditis is characterized by Iymphocytic infiltration of the thyroid gland and production of antibodies that recognize thyroid-specific antigens. It is currently thought that the disease is caused by abnormal suppressor T-lymphocyte function which results in a localized cell-mediated immune response directed toward the thyroid parenchymal cells. The pathogenesis is not completely understood (In contrast Graves' disease is caused by production of antibodies that mimic the action of thyroid-stimulating hormone, and nutritional goiter is caused by iodine deficiency). | |||
The gland is usually diffusely enlarged, firm, and slightly lobular. The capsule is intact, and the cut surface is light tan and has a slight lobular pattern. Microscopically there is massive infiltration of the thyroid gland by lymphocytes and plasma cells. Germinal centers can often be seen in the gland. Thyroid follicles are usually absent and the few remaining follicles are devoid of colloid. | |||
=== Genetics === | |||
A family history of thyroid disorders is common, with the '''HLA-DR5''' gene most strongly implicated conferring a [[relative risk]] of 3 in the UK.The genes implicated vary in different ethnic groups and the incidence is increased in patients with chromosomal disorders, including [[Turner syndrome|Turner]], [[Down syndrome|Down's]], and [[Klinefelter's syndrome]]s. | |||
=== Associated Conditions=== | |||
Hashimoto's disease may, in rare cases, be associated with other endocrine disorders caused by the immune system. Hashimoto's disease can occur with adrenal insufficiency and type 1 diabetes. In these cases, the condition is called type 2 polyglandular autoimmune syndrome (PGA II). | Hashimoto's disease may, in rare cases, be associated with other endocrine disorders caused by the immune system. Hashimoto's disease can occur with adrenal insufficiency and type 1 diabetes. In these cases, the condition is called type 2 polyglandular autoimmune syndrome (PGA II). | ||
| Line 41: | Line 53: | ||
* [[Hypoparathyroidism]] | * [[Hypoparathyroidism]] | ||
== | ===Gross Pathology=== | ||
[[Image: | At autopsy, significant [[subarachnoid hemorrhage]] from the ruptured [[berry aneurysm]] was documented. In addition, the [[thyroid gland]] was mildly enlarged and firm. On cut section the tissue was slightly pale. | ||
===Microscopic Pathology=== | |||
[http://www.peir.net Images courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | |||
[[Image:Hashimoto's thyroiditis 1.jpg|left|thumb|400px|A gross photograph of thyroid gland taken at autopsy. The gland is only slightly enlarged and has a firm texture.]] | |||
<br clear="left"/> | |||
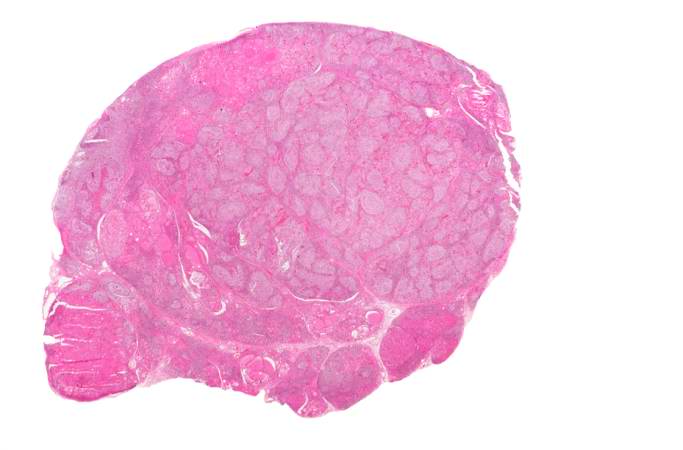
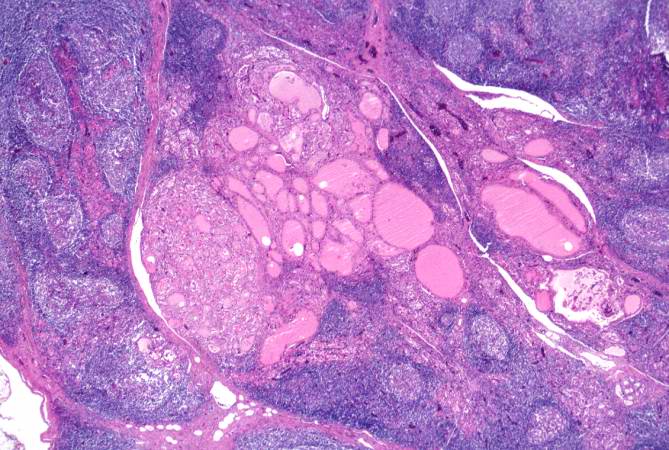
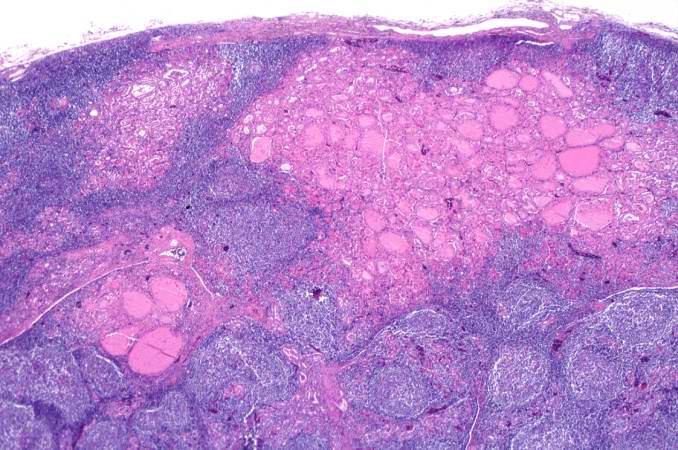
[[Image:Hashimoto's thyroiditis 2.jpg|left|thumb|400px|This is a low-power photomicrograph of thyroid from this case. Note that the tissue is more cellular than one would expect and there does not appear to be normal colloid-filled blue spaces in this gland.]] | |||
<br clear="left"/> | |||
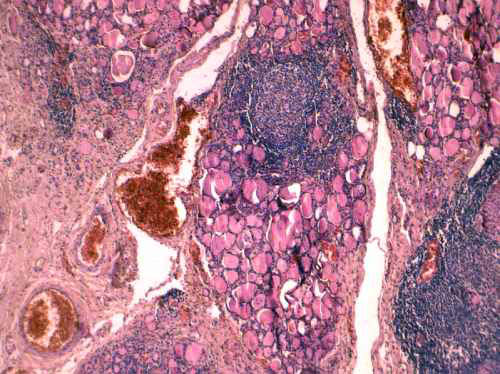
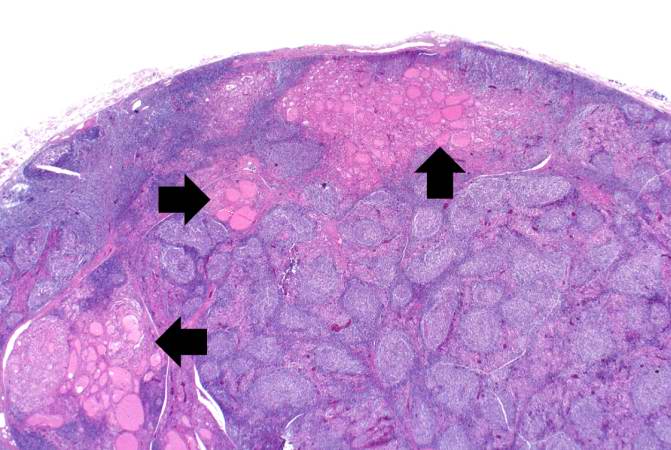
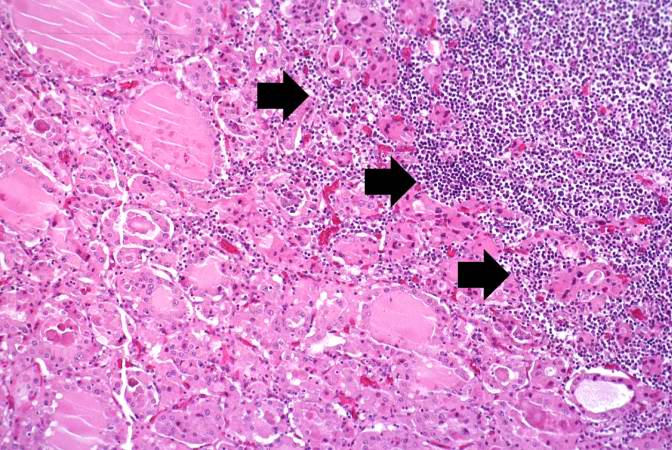
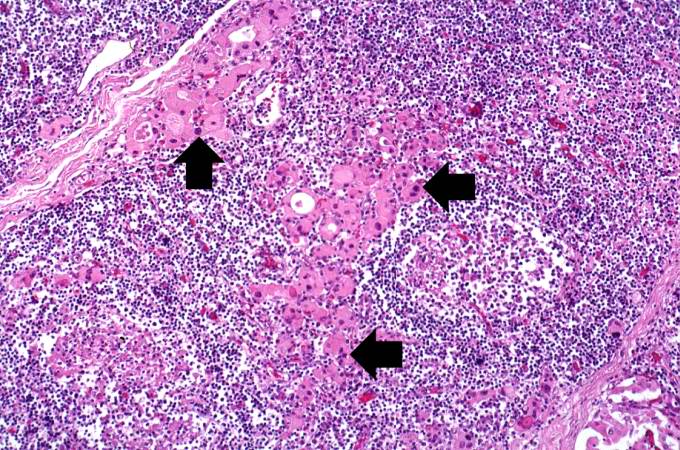
[[Image:Hashimoto's thyroiditis 3.jpg|left|thumb|400px|This is a higher-power photomicrograph of thyroid from this case. Note the large number of blue-staining inflammatory cells in this tissue. These cells appear to be forming germinal centers. Some residual thyroid gland tissue can be seen in this section (arrows).]] | |||
<br clear="left"/> | |||
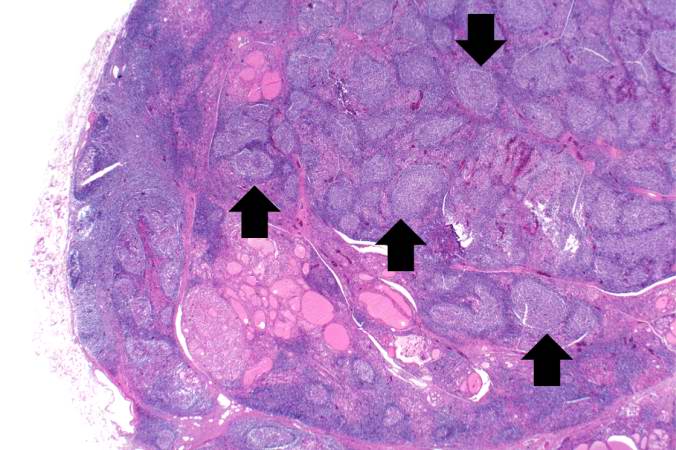
[[Image:Hashimoto's thyroiditis 4.jpg|left|thumb|400px|This is another view of thyroid gland filled with inflammatory cells forming germinal centers (arrows).]] | |||
<br clear="left"/> | |||
[[Image:Hashimoto's thyroiditis 5.jpg|left|thumb|400px|This is a higher-power photomicrograph of thyroid from this case showing the inflammatory cells and the residual thyroid tissue.]] | |||
<br clear="left"/> | |||
[[Image:Hashimoto's thyroiditis 6.jpg|left|thumb|400px|This is another higher-power photomicrograph of thyroid from this case showing the inflammatory cells and the residual thyroid tissue.]] | |||
<br clear="left"/> | |||
[[Image:Hashimoto's thyroiditis 7.jpg||left|thumb|400px|This is a high-power photomicrograph showing the inflammatory cells infiltrating into the residual thyroid tissue (arrows).]] | |||
<br clear="left"/> | |||
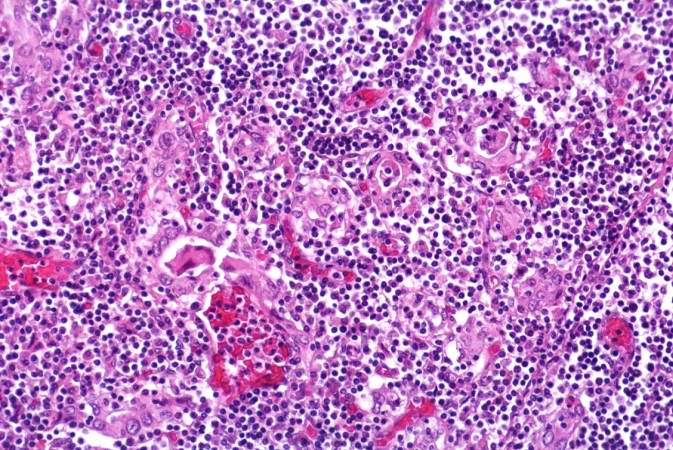
= | [[Image:Hashimoto's thyroiditis 8.jpg||left|thumb|400px|This is a high-power photomicrograph showing the lymphocytes and plasma cells surrounding the thyroid gland epithelium. ]] | ||
<br clear="left"/> | |||
Hashimoto's thyroiditis | [[Image:Hashimoto's thyroiditis 9.jpg||left|thumb|400px|This high-power photomicrograph shows more clearly the lymphocytes and plasma cells surrounding the thyroid gland epithelium. Large, eosinophilic, degenerating thyroid gland cells (Hurthle cells) can be seen in this section (arrows). ]] | ||
<br clear="left"/> | |||
== Epidemiology and Demographics == | |||
This disorder is believed to be the most common cause of primary hypothyroidism in North America. It occurs far more often in women than in men (10:1 to 20:1), and is most prevalent between 45 and 65 years of age. | |||
In European countries an atrophic form of [[autoimmune]] thyroiditis ([[Ord's thyroiditis]]) is more common than Hashimoto's thyroiditis. | |||
The | The disease begins slowly. It may take months or even years for the condition to be detected. Chronic thyroiditis is most common in women and people with a family history of thyroid disease. It affects between 0.1% and 5% of all adults in Western countries. | ||
Various autoantibodies may be present against thyroid peroxidase, thyroglobulin and TSH receptors, although a small percentage of patients may have none of these antibodies present.<!-- This is from eMedicine article, see infobox --> A percentage of the population may also have these antibodies without developing Hashimoto's thyroiditis. | Various autoantibodies may be present against thyroid peroxidase, thyroglobulin and TSH receptors, although a small percentage of patients may have none of these antibodies present.<!-- This is from eMedicine article, see infobox --> A percentage of the population may also have these antibodies without developing Hashimoto's thyroiditis. | ||
== | == Natural History, Complications and Prognosis== | ||
If untreated for an extended period, Hashimoto's thyroiditis may lead to muscle failure, including possible heart failure. | |||
== Diagnosis == | |||
=== Symptoms === | |||
In many cases, Hashimoto's thyroiditis usually results in [[hypothyroidism]], although in its acute phase, it can cause a transient hyperthyroidism [[hyperthyroidism|thyrotoxic]] state known as hashitoxicosis. | |||
* Adolescent goiter | * Adolescent goiter | ||
| Line 77: | Line 114: | ||
* Primary thyroid failure | * Primary thyroid failure | ||
* Subclinical hypothyroidism and goiter | * Subclinical hypothyroidism and goiter | ||
(In alphabetical order) <ref>Ladenson P, Kim M. Thyroid. In: Goldman L and Ausiello D, eds. ''Goldman: Cecil Medicine''. 23rd ed. Philadelphia, Pa:Saunders; 2007:chap 244.</ref> | (In alphabetical order) <ref>Ladenson P, Kim M. Thyroid. In: Goldman L and Ausiello D, eds. ''Goldman: Cecil Medicine''. 23rd ed. Philadelphia, Pa:Saunders; 2007:chap 244.</ref> | ||
| Line 87: | Line 122: | ||
* Difficulty concentrating or thinking | * Difficulty concentrating or thinking | ||
* [[Dry skin]] | * [[Dry skin]] | ||
* Enlarged neck or presence of [[goiter | * Enlarged neck or presence of [[goiter]] | ||
* [[Fatigue]] | * [[Fatigue]] | ||
* [[Hair loss]] | * [[Hair loss]] | ||
* Heavy and irregular periods | * Heavy and irregular periods | ||
* [[Hyperthyroidism]] symptoms | * [[Hyperthyroidism]] symptoms | ||
* [[Hypothyroidism]] symptoms | * [[Hypothyroidism]] symptoms | ||
* [[Infertility]] | * [[Infertility]] | ||
* [[Lethargy]] | * [[Lethargy]] | ||
* [[Mania]] | * [[Mania]] | ||
* [[Memory loss]] | * [[Memory loss]] | ||
| Line 104: | Line 136: | ||
* [[Panic attack]]s | * [[Panic attack]]s | ||
* Puffy face | * Puffy face | ||
* Small or shrunken thyroid gland (late in the disease) | * Small or shrunken thyroid gland (late in the disease) | ||
* [[Weight gain]] | * [[Weight gain]] | ||
| Line 115: | Line 144: | ||
* Joint stiffness | * Joint stiffness | ||
* Swelling of the face | * Swelling of the face | ||
=== Physical Examination === | |||
== | ==== Appearance of the Patient ==== | ||
* [[Myxedema]] | |||
[[ | ====Vital Signs==== | ||
* [[Fast pulse]] | |||
* [[Low pulse]] | |||
== | ====Skin==== | ||
* [[Dry skin]] | |||
====Head==== | |||
* Puffy face | |||
== | ====Throat ==== | ||
* Enlarged neck or presence of [[goiter]] | |||
* Small or shrunken thyroid gland (late in the disease | |||
=== | ==== Neurologic ==== | ||
* Slowed speech | |||
* Slowed reflexes | |||
=== Laboratory Findings === | |||
==== Electrolyte and Biomarker Studies ==== | |||
* [[Thyroid-stimulating hormone]] (TSH) | |||
* Free T3 and Free T4 | |||
* Anti-thyroglobulin antibodies (anti-Tg) | |||
* Anti-thyroid peroxidase antibodies (anti-TPO) | |||
* Anti-microsomal antibodies can help obtain an accurate diagnosis.<ref>{{cite book |last1= Giannini |first1= AJ |authorlink1= |title= The Biological Foundations of Clinical Psychiatry |url= |year= 1986 |publisher= Medical Examination Publishing Company |location= New Hyde Park, NY |language= |isbn= 0-87488-449-7 |oclc= |doi= |id= |page= |pages= 193–198 |quote= |ref= |bibcode= }}</ref> Earlier assessment of the patient may present with elevated levels of thyroglobulin owing to the transient [[thyrotoxicosis]] as inflammation within the thyroid causes damage to the integrity of thyroid follicle storage of thyroglobulin; TSH is concomitantly decreased.<ref>{{cite journal|last=Simmons|first=PJ|coauthors=Dellemarre, FG., Drexhage, HA.|title=Antigen-presenting dendritic cells as regulators of the growth of thyrocytes: a role of interleukin-1beta and interleukin-6|journal=Endocrinology|year=1998|month=July|volume=139|issue=7|pages=3158–3186|pmid=9645688|doi=10.1210/en.139.7.3148}}</ref> | |||
* Diagnosis is made by detecting elevated levels of Anti-TPO antibodies in the serum. | |||
== Treatment == | |||
=== Pharmacotherapy === | |||
==== Chronic Pharmacotherapies ==== | |||
[[Hypothyroidism]] caused by Hashimoto's Thyroiditis is treated with thyroid hormone replacement. A small pill taken once a day should be able to keep the thyroid hormone levels normal. This medicine will, in most cases, need to be taken for the rest of the patient's life. | |||
==Case Studies== | |||
=== | ===Case#1=== | ||
A 49-year-old woman who complained during her yearly [[physical examination]] of [[tiredness]] and difficulty concentrating. She attributed these symptoms to stress at work. She had gained weight over the last year and despite warm weather, she felt chilled without a sweater. | |||
[[Family history]] was significant for [[hypothyroidism]] in her mother and older sister. | |||
[ | On [[physical examination]] she had a pulse of 58 bpm and a blood pressure of 138/88 mm Hg. Examination of her neck disclosed a small thyroid gland with a palpable pyramidal lobe and a firm, bosselated texture. Serum taken at this time demonstrated a total T4 of 7.0 mcg/dL and a TSH of 22.0 mcIU/ml. | ||
[[ | In addition, [[antithyroglobulin antibodies]] were positive at 1:640 and [[antimicrosomal antibodies]] were positive at 1:5120. These results supported the clinical impression of [[hypothyroidism]]; also, the texture of her [[thyroid gland]] and a positive family history suggested an autoimmune etiological factor. | ||
She was referred to an endocrinologist for further evaluation; however, before beginning treatment she died suddenly from a ruptured [[berry aneurysm]] of the [[middle cerebral artery]]. | |||
[[ | |||
[[ | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{Autoimmune diseases}} | {{Autoimmune diseases}} | ||
| Line 187: | Line 205: | ||
[[Category:Thyroid disease]] | [[Category:Thyroid disease]] | ||
[[Category:Endocrinology]] | [[Category:Endocrinology]] | ||
[[Category:Disease]] | |||
[[ | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Revision as of 13:55, 26 August 2012
| Hashimoto's thyroiditis | |
 | |
|---|---|
| Histology | |
| ICD-10 | E06.3 |
| ICD-9 | 245.2 |
| OMIM | 140300 |
| DiseasesDB | 5649 |
| MeSH | D050031 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and Related Keywords: Hashimoto's thyroiditis; chronic lymphocytic thyroiditis; autoimmune thyroiditis
Overview
Hashimoto's thyroiditis or chronic lymphocytic thyroiditis is an autoimmune disease where the body's own antibodies attack the cells of the thyroid.
Historical Perspective
Also known as Hashimoto's disease, Hashimoto's thyroiditis is named after the Japanese physician Hashimoto Hakaru (1881−1934) of the medical school at Kyushu University,[1] who first described (He described four patients with a chronic disorder of the thyroid, which he termed struma lymphomatosa.
The thyroid glands of these patients were characterized by diffuse lymphocytic infiltration, fibrosis, parenchymal atrophy, and an eosinophilic change in some of the acinar cells) the symptoms in 1912 in a German publication [2].
Pathophysiology
Hashimoto's thyroiditis is characterized by Iymphocytic infiltration of the thyroid gland and production of antibodies that recognize thyroid-specific antigens. It is currently thought that the disease is caused by abnormal suppressor T-lymphocyte function which results in a localized cell-mediated immune response directed toward the thyroid parenchymal cells. The pathogenesis is not completely understood (In contrast Graves' disease is caused by production of antibodies that mimic the action of thyroid-stimulating hormone, and nutritional goiter is caused by iodine deficiency).
The gland is usually diffusely enlarged, firm, and slightly lobular. The capsule is intact, and the cut surface is light tan and has a slight lobular pattern. Microscopically there is massive infiltration of the thyroid gland by lymphocytes and plasma cells. Germinal centers can often be seen in the gland. Thyroid follicles are usually absent and the few remaining follicles are devoid of colloid.
Genetics
A family history of thyroid disorders is common, with the HLA-DR5 gene most strongly implicated conferring a relative risk of 3 in the UK.The genes implicated vary in different ethnic groups and the incidence is increased in patients with chromosomal disorders, including Turner, Down's, and Klinefelter's syndromes.
Associated Conditions
Hashimoto's disease may, in rare cases, be associated with other endocrine disorders caused by the immune system. Hashimoto's disease can occur with adrenal insufficiency and type 1 diabetes. In these cases, the condition is called type 2 polyglandular autoimmune syndrome (PGA II).
Less commonly, Hashimoto's disease occurs as part of a condition called type 1 polyglandular autoimmune syndrome (PGA I), along with:
- Adrenal insufficiency
- Fungal infections of the mouth and nails
- Hypoparathyroidism
Gross Pathology
At autopsy, significant subarachnoid hemorrhage from the ruptured berry aneurysm was documented. In addition, the thyroid gland was mildly enlarged and firm. On cut section the tissue was slightly pale.
Microscopic Pathology

Epidemiology and Demographics
This disorder is believed to be the most common cause of primary hypothyroidism in North America. It occurs far more often in women than in men (10:1 to 20:1), and is most prevalent between 45 and 65 years of age.
In European countries an atrophic form of autoimmune thyroiditis (Ord's thyroiditis) is more common than Hashimoto's thyroiditis.
The disease begins slowly. It may take months or even years for the condition to be detected. Chronic thyroiditis is most common in women and people with a family history of thyroid disease. It affects between 0.1% and 5% of all adults in Western countries.
Various autoantibodies may be present against thyroid peroxidase, thyroglobulin and TSH receptors, although a small percentage of patients may have none of these antibodies present. A percentage of the population may also have these antibodies without developing Hashimoto's thyroiditis.
Natural History, Complications and Prognosis
If untreated for an extended period, Hashimoto's thyroiditis may lead to muscle failure, including possible heart failure.
Diagnosis
Symptoms
In many cases, Hashimoto's thyroiditis usually results in hypothyroidism, although in its acute phase, it can cause a transient hyperthyroidism thyrotoxic state known as hashitoxicosis.
- Adolescent goiter
- Alternating hypo- and hyperthyroidism
- Euthyroidism and goiter
- Hypothyroidism
- Painless thyroiditis or silent thyroiditis
- Postpartum painless thyrotoxicosis
- Primary thyroid failure
- Subclinical hypothyroidism and goiter
(In alphabetical order) [3]
- Cold intolerance
- Constipation
- Depression
- Difficulty concentrating or thinking
- Dry skin
- Enlarged neck or presence of goiter
- Fatigue
- Hair loss
- Heavy and irregular periods
- Hyperthyroidism symptoms
- Hypothyroidism symptoms
- Infertility
- Lethargy
- Mania
- Memory loss
- Migraines
- Myxedema
- Panic attacks
- Puffy face
- Small or shrunken thyroid gland (late in the disease)
- Weight gain
- Weight loss
Other symptoms that can occur with this disease:
- Joint stiffness
- Swelling of the face
Physical Examination
Appearance of the Patient
Vital Signs
Skin
Head
- Puffy face
Throat
- Enlarged neck or presence of goiter
- Small or shrunken thyroid gland (late in the disease
Neurologic
- Slowed speech
- Slowed reflexes
Laboratory Findings
Electrolyte and Biomarker Studies
- Thyroid-stimulating hormone (TSH)
- Free T3 and Free T4
- Anti-thyroglobulin antibodies (anti-Tg)
- Anti-thyroid peroxidase antibodies (anti-TPO)
- Anti-microsomal antibodies can help obtain an accurate diagnosis.[4] Earlier assessment of the patient may present with elevated levels of thyroglobulin owing to the transient thyrotoxicosis as inflammation within the thyroid causes damage to the integrity of thyroid follicle storage of thyroglobulin; TSH is concomitantly decreased.[5]
- Diagnosis is made by detecting elevated levels of Anti-TPO antibodies in the serum.
Treatment
Pharmacotherapy
Chronic Pharmacotherapies
Hypothyroidism caused by Hashimoto's Thyroiditis is treated with thyroid hormone replacement. A small pill taken once a day should be able to keep the thyroid hormone levels normal. This medicine will, in most cases, need to be taken for the rest of the patient's life.
Case Studies
Case#1
A 49-year-old woman who complained during her yearly physical examination of tiredness and difficulty concentrating. She attributed these symptoms to stress at work. She had gained weight over the last year and despite warm weather, she felt chilled without a sweater.
Family history was significant for hypothyroidism in her mother and older sister.
On physical examination she had a pulse of 58 bpm and a blood pressure of 138/88 mm Hg. Examination of her neck disclosed a small thyroid gland with a palpable pyramidal lobe and a firm, bosselated texture. Serum taken at this time demonstrated a total T4 of 7.0 mcg/dL and a TSH of 22.0 mcIU/ml.
In addition, antithyroglobulin antibodies were positive at 1:640 and antimicrosomal antibodies were positive at 1:5120. These results supported the clinical impression of hypothyroidism; also, the texture of her thyroid gland and a positive family history suggested an autoimmune etiological factor.
She was referred to an endocrinologist for further evaluation; however, before beginning treatment she died suddenly from a ruptured berry aneurysm of the middle cerebral artery.
References
- ↑ Template:WhoNamedIt
- ↑ H. Hashimoto: Zur Kenntnis der lymphomatösen Veränderung der Schilddrüse (Struma lymphomatosa). Archiv für klinische Chirurgie, Berlin, 1912, 97: 219−248.
- ↑ Ladenson P, Kim M. Thyroid. In: Goldman L and Ausiello D, eds. Goldman: Cecil Medicine. 23rd ed. Philadelphia, Pa:Saunders; 2007:chap 244.
- ↑ Giannini, AJ (1986). The Biological Foundations of Clinical Psychiatry. New Hyde Park, NY: Medical Examination Publishing Company. pp. 193–198. ISBN 0-87488-449-7.
- ↑ Simmons, PJ (1998). "Antigen-presenting dendritic cells as regulators of the growth of thyrocytes: a role of interleukin-1beta and interleukin-6". Endocrinology. 139 (7): 3158–3186. doi:10.1210/en.139.7.3148. PMID 9645688. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help)