Small intestinal bacterial overgrowth syndrome
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Mazia Fatima, MBBS [2]
| Small intestinal bacterial overgrowth syndrome | |
| ICD-10 | K63 |
|---|---|
| ICD-9 | 579.9 |
| DiseasesDB | 29209 |
| MedlinePlus | 000222 |
| eMedicine | med/198 |
Overview
Small intestinal bacterial overgrowth (SIBO) was first discovered by Barber and Hummel in 1939. There is no established system for the classification of small intestinal bacterial overgrowth(SIBO).The pathogenesis of small intestinal bacterial overgrowth (SIBO) is characterized by an increased microbial load in the small intestine. Disruption of protective homeostatic mechanisms can increase the risk of SIBO. Bacterial colonization causes an inflammatory response in the intestinal mucosa. Damage to the intestinal mucosa leads to malabsorption of bile acids, carbohydrates, proteins and vitamins resulting in symptoms of diarrhea and weight loss. On gross pathology, mucosal edema, loss of normal vascular pattern, patchy erythema, friability and ulceration of the small intestinal wall is associated with small intestinal bacterial overgrowth (SIBO). On microscopic histopathological analysis small intestine and colon are normal in most patients with SIBO. Findings include blunting of the intestinal villi, thinning of the mucosa and crypts, increased intraepithelial lymphocytes. Small intestinal bacterial overgrowth (SIBO) must be differentiated from other diseases that cause chronic diarrhea. Small intestinal bacterial overgrowth is more commonly observed among elderly patients. Small intestinal bacterial overgrowth (SIBO) affects men and women equally.There is no racial predilection for small intestinal bacterial overgrowth (SIBO). Early clinical features include bloating, flatulence, abdominal pain. If left untreated, patients with small intestinal bacterial overgrowth (SIBO) may progress to develop diarrhea, dyspepsia and weight loss. Prognosis is generally good and associated with frequent relapses and symptom-free periods. The diagnosis of small intestinal bacterial overgrowth (SIBO) is made when at least one of the following diagnostic criteria are met : a positive carbohydrate breath test, bacterial concentration of >103 units/mL in a jejunal aspirate culture. Physical examination may be remarkable for distended abdomen with positive succussion splash as a result of distended bowel loops, peripheral edema due to malabsorption. Small intestinal bacterial obstruction(SIBO) may also be diagnosed using breath tests. The mainstay of therapy for small intestinal bacterial overgrowth(SIBO) is antibiotic therapy. Surgical approach can only be performed for patients with strictures, fistulae, and diverticula or any other structural abnormality resulting in obstruction and resultant bacterial overgrowth. Effective measures for the prevention of small bowel bacterial overgrowth syndrome include avoiding medications like narcotics and benzodiazepines that decrease intestinal motility, avoid achlorhydria in high-risk patients. Consider antibiotic prophylaxis for patients with four or more episodes of recurrent small bowel bacterial overgrowth syndrome within one year.
Historical Perspective
- Small intestinal bacterial overgrowth (SIBO) was first discovered by Barber and Hummel in 1939.
- In 2000, Pimentel et all at Cedars-Sinai Medical Center first identified that SIBO was present in 78% of patients with irritable bowel syndrome (IBS), and that treatment with antibiotics improved symptoms.
- In May 2015, U.S. Food and Drug Administration (FDA) approved rifaximin to treat SIBO.
Classification
- There is no established system for the classification of small intestinal bacterial overgrowth(SIBO).
Pathophysiology
- The pathogenesis of small intestinal bacterial overgrowth (SIBO) is characterized by an increased microbial load in the small intestine.
- A healthy individual has less than 103 organisms/mL in the upper small intestine, and the majority of these organisms are gram-positive bacteria.
- Human body's homeostatic mechanisms protect against excessive small intestinal colonization by bacteria include :
- Gastric acid and bile eradicate micro-organisms before they leave the stomach
- Migrating motor complex clears the excess bacteria of upper intestine
- Intestinal mucosa serves as a protective layer for the gut wall.
- Normal intestinal flora (eg, Lactobacillus) maintains a low pH that prevents bacterial overgrowth.
- Physical barrier of the ileocecal valve that prevents retrograde translocation of bacteria from colon to the small intestine.
- Disruption of these protective homeostatic mechanisms can increase the risk of SIBO.
- Bacterial colonization causes an inflammatory response in the intestinal mucosa.
- Damage to the intestinal mucosa leads to malabsorption of bile acids, carbohydrates, proteins and vitamins resulting in symptoms of diarrhea and weight loss.
- On gross pathology, mucosal edema, loss of normal vascular pattern, patchy erythema, friability and ulceration of the small intestinal wall is associated with small intestinal bacterial overgrowth (SIBO).
- On microscopic histopathological analysis small intestine and colon is normal in most patients with SIBO. Findings include:
- Blunting of the intestinal villi
- Thinning of the mucosa and crypts
- Increased intraepithelial lymphocytes
Causes
- Small intestinal bacterial overgrowth (SIBO) may be caused by disruption of the protective homeostatic mechanisms that control enteric bacteria population.
- Causes of small intestinal bacterial overgrowth (SIBO) include:
- Irregular small intestinal motility
- Blind pouches in the gastrointestinal tract
- Side-to-side or end-to-side anastomoses
- Duodenal or jejunal diverticula
- Segmental dilatation of the ileum
- Blind loop syndrome
- Biliopancreatic diversion
- Chagasic megacolon
- Fistula
- Partial Obstruction
- Decreased gastric acid secretion
- Achlorhydria
- Vagotomy
- Long-term proton pump inhibitor therapy
Differentiating [disease name] from other Diseases
- Small intestinal bacterial overgrowth (SIBO) must be differentiated from other diseases that cause chronic diarrhea.
The following table outlines the major differential diagnoses of chronic diarrhea.[1][2][3][4][5][6][7][8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24][25][26][27][28][29][30]
Abbreviations: GI: Gastrointestinal, CBC: Complete blood count, WBC: White blood cell, RBC: Red blood cell, Plt: Platelet, Hgb: Hemoglobin, ESR: Erythrocyte sedimentation rate, CRP: C–reactive protein, IgE: Immunoglobulin E, IgA: Immunoglobulin A, ETEC: Escherichia coli enteritis, EPEC: Enteropathogenic Escherichia coli, EIEC: Enteroinvasive Escherichia coli, EHEC: Enterohemorrhagic Escherichia coli, EAEC: Enteroaggregative Escherichia coli, Nl: Normal, ASCA: Anti saccharomyces cerevisiae antibodies, ANCA: Anti–neutrophil cytoplasmic antibody, DNA: Deoxyribonucleic acid, CFTR: Cystic fibrosis transmembrane conductance regulator, SLC10A2: Solute carrier family 10 member 2, SeHCAT: Selenium homocholic acid taurine or tauroselcholic acid, IEL: Intraepithelial lymphocytes, MRCP: Magnetic resonance cholangiopancreatography, ANA: Antinuclear antibodies, AMA: Anti-mitochondrial antibody, LDH: Lactate dehydrogenase, CPK: Creatine phosphokinase, PCR: Polymerase chain reaction, ELISA: Enzyme–linked immunosorbent assay, LT: Heat–labile enterotoxin, ST: Heat–stable enterotoxin, RT-PCR: Reverse–transcriptase polymerase chain reaction, CD4: Cluster of differentiation 4, HIV: Human immunodeficiency virus, RUQ: Right-upper quadrant, VIP: Vasoactive intestinal peptide, GI: Gastrointestinal, FAP: Familial adenomatous polyposis, HNPCC: Hereditary nonpolyposis colorectal cancer, MTP: Microsomal triglyceride transfer protein, Scl‑70: Anti–topoisomerase I, TSH: Thyroid-stimulating hormone, T4: Thyroxine, T3: Triiodothyronine, DTR: Deep tendon reflex, RNA: Ribonucleic acid
| Cause | Clinical manifestation | Lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | GI signs | |||||||||||||||||||||
| Duration | Diarrhea | Fever | Abdominal pain | Weight loss | ||||||||||||||||||
| Stool exam | CBC | Other lab findings | ||||||||||||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Crohn's disease | – | + | + | + | + | ± | + | + |
|
+ | + | – | Nl | – | ↑ | ↓ | ↑ |
|
|
|
| |
| Ulcerative colitis | – | + | + | + | + | ± | + | + | + | + | – | Nl | – | ↑ | ↓ | ↑ |
|
|
| |||
| Celiac disease | – | + | ± | – | ± | – | + | + |
|
– | – | – | Nl |
|
Nl | ↓ | Nl |
|
| |||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Cystic fibrosis | – | + | – | – | + | ± | + | + | – | – | – | Nl |
|
Nl | ↓ | Nl |
|
|
| |||
| Chronic pancreatitis | – | + | + | – | + | – | + | + | – | – | – | Nl |
|
Nl | Nl | Nl |
|
|||||
| Bile acid malabsorption | – | + | + | – | + | – | – | + | – | – | – | Nl |
|
Nl | Nl | Nl |
|
|
| |||
| Microscopic colitis | – | + | + | – | – | – | + | + | – | – | – | Nl | – | Nl | ↓ | Nl |
|
|
| |||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Infective colitis | – | + | + | + | – | + | + | + |
|
+ | + | + | Nl |
|
↑ | ↓ | ↑ | |||||
| Ischemic colitis | + | + | + | + | – | + | + | + |
|
+ | + | – | Nl | – | ↑ | ↓ | ↑ |
|
|
| ||
| Lactose intolerance | + | + | + | – | – | – | + | – | – | – | – | ↑ | – | Nl | Nl | Nl |
|
|
| |||
| Irritable bowel syndrome | – | + | ± | – | ± | – | ± | – | – | – | – | Nl | – | Nl | Nl | Nl | Nl |
|
| |||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Whipple's disease | – | + | + | – | + | ± | + | + | – | – | – | Nl |
|
↓ | ↓ | ↓/↑ |
|
| ||||
| Tropical sprue | + | + | + | – | + | + | + | + |
|
+ | – | – | Nl |
|
Nl | ↓ | Nl |
| ||||
| Small bowel bacterial overgrowth | – | + | + | – | + | – | + | + | + | – | – | Nl |
|
Nl | ↓ | Nl |
|
| ||||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Salmonellosis | + | + | + | + | – | + | + | – | + | + | – | Nl |
|
↑ | Nl | ↑ | ||||||
| Escherichia coli enteritis | EPEC | + | + | + | + | – | + | + | + |
|
+ | + | – | Nl |
|
↑ | Nl | Nl | – | – |
| |
| EAEC | + | + | + | + | – | – | + | – |
|
+ | + | – | Nl |
|
↑ | ↓ | ↓ | – |
|
|||
| Aeromonas | + | + | + | + | – | + | + | – |
|
+ | + | – | Nl |
|
↑ | Nl | Nl | – |
|
| ||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Mycobacterium avium complex | + | + | + | + | – | + | + | – | + | + | – | Nl | – | ↓ | ↓ | Nl |
|
|||||
| CMV colitis | + | + | – | + | – | ± | + | – |
|
+ | + | – | Nl |
|
↓ | Nl | Nl |
|
| |||
| HIV | – | + | + | – | – | + | + | + | + | – | – | Nl | – | ↓ | ↓ | Nl |
|
|
| |||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Entamoeba histolytica | + | + | + | + | – | + | + | – | + | + | + | Nl | – | ↑ | Nl | Nl | – |
|
| |||
| Giardia | – | + | + | – | + | – | + | + | – | – | + | Nl | – | Nl | Nl | Nl | – |
| ||||
| Cryptosporidium | – | + | + | – | – | – | + | + | – | – | + | Nl |
|
Nl | Nl | Nl |
|
|
| |||
| Microsporidia | + | + | + | – | – | + | + | – | – | – | + | Nl |
|
Nl | Nl | Nl |
|
| ||||
| Isospora | + | + | + | – | + | + | + | + | + | + | + | Nl |
|
↑ | Nl | Nl |
|
|
| |||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Carcinoid tumor | – | + | + | + | – | – | + | + | – | + | – | ↓ | – | Nl | Nl | Nl |
|
|
| |||
| VIPoma | + | + | + | – | + | – | + | + |
|
– | – | – | ↓ | – | Nl | Nl | Nl |
|
|
| ||
| Zollinger–Ellison syndrome | – | + | + | + | + | – | + | + | – | – | – | ↓ | – | Nl | ↓ | Nl |
|
| ||||
| Somatostatinoma | – | + | + | – | – | – | + | + | – | – | – | ↓ | – | Nl | Nl | Nl |
|
|
| |||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Lymphoma | – | + | + | + | – | + | + | + | – | + | – | Nl | – | Nl | ↓ | Nl |
|
| ||||
| Colorectal cancer | – | + | + | + | + | – | + | + |
|
– | + | – | Nl | – | Nl | ↓ | Nl |
|
| |||
| Medications | + | + | + | – | ± | ± | + | + | – | – | – | ↑/↓ | – | ↑ | Nl | Nl |
|
– |
| |||
| Factitious diarrhea | + | + | + | – | – | – | + | + | – | – | – | ↑/↓ | – | Nl | Nl | Nl |
| |||||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Heavy metal ingestion | – | + | + | – | – | – | + | + | – | – | – | Nl | – | Nl | Nl | Nl |
|
| ||||
| Organophosphate poisoning | + | + | + | – | – | – | + | – | – | – | – | Nl | – | Nl | Nl | Nl |
|
|
|
| ||
| Opium withdrawal | + | + | + | – | – | – | + | – |
|
– | – | – | Nl | – | Nl | Nl | Nl |
| ||||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Short bowel syndrome | + | + | + | – | + | – | – | + | – | – | – | Nl |
|
Nl | ↓ | ↑ |
|
|
|
| ||
| Radiation enteritis | + | + | + | + | + | – | + | + | + | + | – | Nl |
|
Nl | ↓ | Nl |
|
|
| |||
| Dumping syndrome | – | + | + | – | + | – | – | + |
|
– | – | – | Nl | – | Nl | Nl | Nl |
|
| |||
| Cause | Duration | Diarrhea | Fever | Abdominal pain | Weight loss | GI signs | Stool exam | CBC | Other lab findings | Extra intestinal findings | Cause/Pathogenesis | Gold standard diagnosis | ||||||||||
| Acute | Chronic | Watery | Bloody | Fatty | WBC | RBC | Ova/Parasite | Osmotic gap | Other | WBC | Hgb | Plt | ||||||||||
| Abetalipoproteinemia | – | + | + | – | + | – | + | + | – | – | – | Nl | – | Nl | Nl | Nl |
|
|
| |||
| Hyperthyroidism | – | + | + | – | – | ± | + | + | – | – | – | – | Nl |
|
Nl | Nl | Nl |
|
|
|||
| Diabetic neuropathy | – | + | + | – | + | – | + | + | – | – | – | Nl |
|
Nl | ↓ | Nl |
|
| ||||
| Systemic sclerosis | – | + | + | ± | + | – | + | + | – | + | – | Nl |
|
Nl | ↓ | Nl |
|
| ||||
Epidemiology and Demographics
- The prevalence of SIBO is unknown.
Age
Gender
Race
- There is no racial predilection for small intestinal bacterial overgrowth (SIBO).
Risk Factors
- Common risk factors in the development of small intestinal bacterial overgrowth (SIBO) are :
- Intestinal tract surgery
- Irritable bowel syndrome
- Liver cirrhosis
- Celiac disease
- Immune deficiency (eg, AIDS, IgA deficiency, severe malnutrition)
- Short bowel syndrome
- End-stage renal disease
- Gastrojejunal anastomosis
- Antral resection
- Pancreatic exocrine insufficiency
Natural History, Complications and Prognosis
- Early clinical features include bloating, flatulence, abdominal pain.
- If left untreated, patients with small intestinal bacterial overgrowth (SIBO) may progress to develop diarrhea, dyspepsia and weight loss.
- Common complications of small intestinal bacterial overgrowth (SIBO) include:
- Iron deficiency resulting in microcytic anemia
- Vitamin B-12/ folate deficiency resulting in macrocytic anemia
- Vitamin B-12 deficiency associated polyneuropathy
- Steatorrhea
- Hypocalcemia
- Vitamin A deficiency resulting in night blindness
- Selenium deficiency causing dermatitis
- Rosacea
- Cachexia as a result of protein-energy malnutrition
- Prognosis is generally good and associated with frequent relapses and symptom-free periods.
Diagnosis
Diagnostic Criteria
- The diagnosis of small intestinal bacterial overgrowth (SIBO) is made when at least one of the following diagnostic criteria are met:
- A positive carbohydrate breath test
- Bacterial concentration of >103 units/mL in a jejunal aspirate culture
Symptoms
- Symptoms of small intestinal bacterial overdose (SIBO) may include the following:
Physical Examination
- Patients with small intestinal bacterial overgrowth (SIBO) usually appear normal.
- Physical examination may be remarkable for:
- Distended abdomen with positive succussion splash as a result of distended bowel loops
- Peripheral edema due to malabsorption
Laboratory Findings
- A positive carbohydrate breath test is diagnostic of small intestinal bacterial overgrowth (SIBO).
- An elevated concentration of bacterial colony forming units >103/mL in jejunal aspirate culture is diagnostic of small intestinal bacterial overgrowth (SIBO).
- Other laboratory findings consistent with the diagnosis of small intestinal bacterial overgrowth (SIBO) include
- Macrocytic anemia
- B12 deficiency
- Presence of fecal fat on stool examination.
- Low levels of thiamine and niacin
- Elevated serum folate and vitamin K levels
Imaging Findings
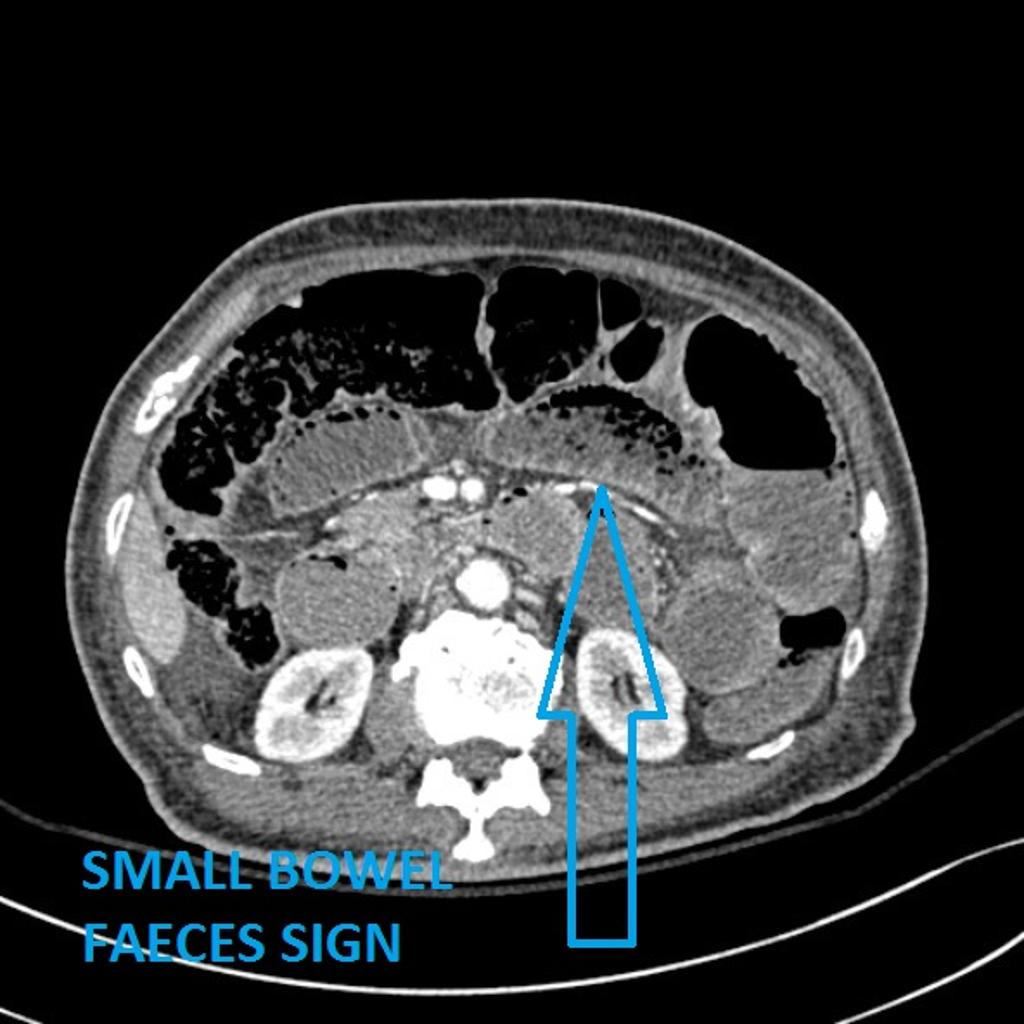
- In CT abdomen/MRI may demonstrate associated strictures, malrotation, fistulae.
- Small intestinal bacterial overgrowth can result in small bowel obstruction that presents as small bowel feaces sign on abdominal CT.
- Small bowel faeces sign is the presence of particulate faeculent material mingled with gas bubbles in the lumen of the small intestine , it is believed to be the result of delayed intestinal transit.
Other Diagnostic Studies
Breath Tests
- Small intestinal bacterial obstruction(SIBO) may also be diagnosed using breath tests.
- Breath tests have the advantage of being easy to perform, noninvasive and inexpensive. Breath tests are based on the principle that carbohydrates are metabolized by bacteria in the gut to produce hydrogen or methane that is absorbed and excreted in breath.
- The findings on carbohydrate breath test diagnostic of small intestinal bacterial obstruction(SIBO) include:
Treatment
Medical Therapy
- The mainstay of therapy for small intestinal bacterial overgrowth(SIBO) is antibiotic therapy.
- Antibiotics acts by eliminating the bacterial overgrowth.
- Rifaximin is the antibiotic of choice for the treatment of small intestinal bacterial overgrowth(SIBO).
- Preferred regimen: Rifaximin 550 mg PO 8h for 14 days.
- Response to antibiotics can be assessed by the symptomatic improvement. In case of recurrent symptoms, the antibiotic dose is repeated.
Surgery
- Surgical approach can only be performed for patients with strictures, fistulae, and diverticula or any other structural abnormality resulting in obstruction and resultant bacterial overgrowth.
Prevention
- Effective measures for the prevention of small bowel bacterial overgrowth syndrome include :
- Avoiding medications like narcotics and benzodiazepines that decrease intestinal motility.
- Avoid achlorhydria in high-risk patients.
- Consider antibiotic prophylaxis for patients with four or more episodes of recurrent small bowel bacterial overgrowth syndrome within one year.
References
- ↑ Casburn-Jones, Anna C; Farthing, Michael Jg (2004). "Traveler's diarrhea". Journal of Gastroenterology and Hepatology. 19 (6): 610–618. doi:10.1111/j.1440-1746.2003.03287.x. ISSN 0815-9319.
- ↑ Kamat, Deepak; Mathur, Ambika (2006). "Prevention and Management of Travelers' Diarrhea". Disease-a-Month. 52 (7): 289–302. doi:10.1016/j.disamonth.2006.08.003. ISSN 0011-5029.
- ↑ Pfeiffer, Margaret L.; DuPont, Herbert L.; Ochoa, Theresa J. (2012). "The patient presenting with acute dysentery – A systematic review". Journal of Infection. 64 (4): 374–386. doi:10.1016/j.jinf.2012.01.006. ISSN 0163-4453.
- ↑ Barr W, Smith A (2014). "Acute diarrhea". Am Fam Physician. 89 (3): 180–9. PMID 24506120.
- ↑ Amil Dias J (2017). "Celiac Disease: What Do We Know in 2017?". GE Port J Gastroenterol. 24 (6): 275–278. doi:10.1159/000479881. PMID 29255768.
- ↑ Kotloff KL, Riddle MS, Platts-Mills JA, Pavlinac P, Zaidi A (2017). "Shigellosis". Lancet. doi:10.1016/S0140-6736(17)33296-8. PMID 29254859. Vancouver style error: initials (help)
- ↑ Yamamoto-Furusho, J.K.; Bosques-Padilla, F.; de-Paula, J.; Galiano, M.T.; Ibañez, P.; Juliao, F.; Kotze, P.G.; Rocha, J.L.; Steinwurz, F.; Veitia, G.; Zaltman, C. (2017). "Diagnóstico y tratamiento de la enfermedad inflamatoria intestinal: Primer Consenso Latinoamericano de la Pan American Crohn's and Colitis Organisation". Revista de Gastroenterología de México. 82 (1): 46–84. doi:10.1016/j.rgmx.2016.07.003. ISSN 0375-0906.
- ↑ Borbély, Yves M; Osterwalder, Alice; Kröll, Dino; Nett, Philipp C; Inglin, Roman A (2017). "Diarrhea after bariatric procedures: Diagnosis and therapy". World Journal of Gastroenterology. 23 (26): 4689. doi:10.3748/wjg.v23.i26.4689. ISSN 1007-9327.
- ↑ Crawford, Sue E.; Ramani, Sasirekha; Tate, Jacqueline E.; Parashar, Umesh D.; Svensson, Lennart; Hagbom, Marie; Franco, Manuel A.; Greenberg, Harry B.; O'Ryan, Miguel; Kang, Gagandeep; Desselberger, Ulrich; Estes, Mary K. (2017). "Rotavirus infection". Nature Reviews Disease Primers. 3: 17083. doi:10.1038/nrdp.2017.83. ISSN 2056-676X.
- ↑ Kist M (2000). "[Chronic diarrhea: value of microbiology in diagnosis]". Praxis (Bern 1994) (in German). 89 (39): 1559–65. PMID 11068510.
- ↑ Guerrant RL, Shields DS, Thorson SM, Schorling JB, Gröschel DH (1985). "Evaluation and diagnosis of acute infectious diarrhea". Am. J. Med. 78 (6B): 91–8. PMID 4014291.
- ↑ López-Vélez R, Turrientes MC, Garrón C, Montilla P, Navajas R, Fenoy S, del Aguila C (1999). "Microsporidiosis in travelers with diarrhea from the tropics". J Travel Med. 6 (4): 223–7. PMID 10575169.
- ↑ Wahnschaffe, Ulrich; Ignatius, Ralf; Loddenkemper, Christoph; Liesenfeld, Oliver; Muehlen, Marion; Jelinek, Thomas; Burchard, Gerd Dieter; Weinke, Thomas; Harms, Gundel; Stein, Harald; Zeitz, Martin; Ullrich, Reiner; Schneider, Thomas (2009). "Diagnostic value of endoscopy for the diagnosis of giardiasis and other intestinal diseases in patients with persistent diarrhea from tropical or subtropical areas". Scandinavian Journal of Gastroenterology. 42 (3): 391–396. doi:10.1080/00365520600881193. ISSN 0036-5521.
- ↑ Mena Bares LM, Carmona Asenjo E, García Sánchez MV, Moreno Ortega E, Maza Muret FR, Guiote Moreno MV, Santos Bueno AM, Iglesias Flores E, Benítez Cantero JM, Vallejo Casas JA (2017). "75SeHCAT scan in bile acid malabsorption in chronic diarrhoea". Rev Esp Med Nucl Imagen Mol. 36 (1): 37–47. doi:10.1016/j.remn.2016.08.005. PMID 27765536.
- ↑ Gibson RJ, Stringer AM (2009). "Chemotherapy-induced diarrhoea". Curr Opin Support Palliat Care. 3 (1): 31–5. doi:10.1097/SPC.0b013e32832531bb. PMID 19365159.
- ↑ Abraham BP, Sellin JH (2012). "Drug-induced, factitious, & idiopathic diarrhoea". Best Pract Res Clin Gastroenterol. 26 (5): 633–48. doi:10.1016/j.bpg.2012.11.007. PMID 23384808.
- ↑ Reintam Blaser A, Deane AM, Fruhwald S (2015). "Diarrhoea in the critically ill". Curr Opin Crit Care. 21 (2): 142–53. doi:10.1097/MCC.0000000000000188. PMID 25692805.
- ↑ McMahan ZH, DuPont HL (2007). "Review article: the history of acute infectious diarrhoea management--from poorly focused empiricism to fluid therapy and modern pharmacotherapy". Aliment. Pharmacol. Ther. 25 (7): 759–69. doi:10.1111/j.1365-2036.2007.03261.x. PMID 17373914.
- ↑ Schiller LR (2012). "Definitions, pathophysiology, and evaluation of chronic diarrhoea". Best Pract Res Clin Gastroenterol. 26 (5): 551–62. doi:10.1016/j.bpg.2012.11.011. PMID 23384801.
- ↑ Giannella RA (1986). "Chronic diarrhea in travelers: diagnostic and therapeutic considerations". Rev. Infect. Dis. 8 Suppl 2: S223–6. PMID 3523719.
- ↑ Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR; et al. (2005). "Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology". Can J Gastroenterol. 19 Suppl A: 5A–36A. PMID 16151544.
- ↑ Sauter GH, Moussavian AC, Meyer G, Steitz HO, Parhofer KG, Jüngst D (2002). "Bowel habits and bile acid malabsorption in the months after cholecystectomy". Am J Gastroenterol. 97 (7): 1732–5. doi:10.1111/j.1572-0241.2002.05779.x. PMID 12135027.
- ↑ Maiuri L, Raia V, Potter J, Swallow D, Ho MW, Fiocca R; et al. (1991). "Mosaic pattern of lactase expression by villous enterocytes in human adult-type hypolactasia". Gastroenterology. 100 (2): 359–69. PMID 1702075.
- ↑ RUBIN CE, BRANDBORG LL, PHELPS PC, TAYLOR HC (1960). "Studies of celiac disease. I. The apparent identical and specific nature of the duodenal and proximal jejunal lesion in celiac disease and idiopathic sprue". Gastroenterology. 38: 28–49. PMID 14439871.
- ↑ Konvolinka CW (1994). "Acute diverticulitis under age forty". Am J Surg. 167 (6): 562–5. PMID 8209928.
- ↑ Satsangi J, Silverberg MS, Vermeire S, Colombel JF (2006). "The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications". Gut. 55 (6): 749–53. doi:10.1136/gut.2005.082909. PMC 1856208. PMID 16698746.
- ↑ Haque R, Huston CD, Hughes M, Houpt E, Petri WA (2003). "Amebiasis". N Engl J Med. 348 (16): 1565–73. doi:10.1056/NEJMra022710. PMID 12700377.
- ↑ Hertzler SR, Savaiano DA (1996). "Colonic adaptation to daily lactose feeding in lactose maldigesters reduces lactose intolerance". Am J Clin Nutr. 64 (2): 232–6. PMID 8694025.
- ↑ Briet F, Pochart P, Marteau P, Flourie B, Arrigoni E, Rambaud JC (1997). "Improved clinical tolerance to chronic lactose ingestion in subjects with lactose intolerance: a placebo effect?". Gut. 41 (5): 632–5. PMC 1891556. PMID 9414969.
- ↑ BLACK-SCHAFFER B (1949). "The tinctoral demonstration of a glycoprotein in Whipple's disease". Proc Soc Exp Biol Med. 72 (1): 225–7. PMID 15391722.