Campylobacter
| Campylobacter | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
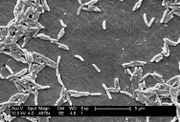 SEM micrograph of C. fetus
| ||||||||||||
| Scientific classification | ||||||||||||
| ||||||||||||
| Species | ||||||||||||
|
C. coli |
The genus Campylobacter are Gram-negative, spiral, microaerophilic bacteria. Motile, with either uni- or bi-polar flagella, the organisms have a somewhat curved, rod-like appearance, and are oxidase-positive.[1] Campylobacter jejuni is now recognised as one of the main causes of bacterial foodborne disease in many developed countries.[2] At least a dozen species of Campylobacter have been implicated in human disease, with C. jejuni and C. coli the most common.[1] C. fetus is a cause of spontaneous abortions in cattle and sheep, as well as an opportunisitic pathogen in humans.[3]
Genome
The genomes of several Campylobacter species have been sequenced, providing insights into their mechanisms of pathogenesis.[4]
Campylobacter species contain two flagellin genes in tandem for motility, flaA and flaB. These genes undergo intergenic recombination, further contributing to their virulence. [5] Non-motile mutants do not colonize.
Pathogenesis
Campylobacteriosis is an infection by campylobacter [6]. The common routes of transmission are fecal-oral, person-to-person sexual contact, ingestion of contaminated food or water. It produces an inflammatory, sometimes bloody, diarrhea, periodontitis [7] or dysentery syndrome, mostly including cramps, fever and pain. The infection is usually self-limiting and in most cases, symptomatic treatment by reposition of liquid and electrolyte replacement is enough in human infections. The use of antibiotics, on the other hand, is controversial.
Cause
This is most commonly caused by C. jejuni, a spiral and comma shaped bacterium normally found in cattle, swine, and birds, where it is non-pathogenic. But the illness can also be caused by C. coli (also found in cattle, swine, and birds) C. upsaliensis (found in cats and dogs) and C. lari (present in seabirds in particular).
One cause of the effects of campylobacteriosis is tissue injury in the gut. The sites of tissue injury include the jejunum, the ileum, and the colon. C jejuni appears to achieve this by invading and destroying epithelial cells.
Some strains of C jejuni produce a cholera-like enterotoxin, which is important in the watery diarrhea observed in infections. The organism produces diffuse, bloody, edematous, and exudative enteritis. In a small number of cases, the infection may be associated with hemolytic uremic syndrome and thrombotic thrombocytopenic purpura through a poorly understood mechanism.
Differential diagnosis
Campylobacter infection must be differentiated from other causes of viral, bacterial, and parasitic gastroentritis.
| Organism | Age predilection | Travel History | Incubation Size (cell) | Incubation Time | History and Symptoms | Diarrhea type8 | Food source | Specific consideration | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fever | N/V | Cramping Abd Pain | Small Bowel | Large Bowel | Inflammatory | Non-inflammatory | |||||||||
| Viral | Rotavirus | <2 y | - | <102 | <48 h | + | + | - | + | + | - | Mostly in day cares, most common in winter. | |||
| Norovirus | Any age | - | 10 -103 | 24-48 h | + | + | + | + | + | - | Most common cause of gastroenteritis, abdominal tenderness, | ||||
| Adenovirus | <2 y | - | 105 -106 | 8-10 d | + | + | + | + | + | - | No seasonality | ||||
| Astrovirus | <5 y | - | 72-96 h | + | + | + | + | + | Seafood | Mostly during winter | |||||
| Bacterial | Escherichia coli | ETEC | Any age | + | 108 -1010 | 24 h | - | + | + | + | + | - | Causes travelers diarrhea, contains heat-labile toxins (LT) and heat-stable toxins (ST) | ||
| EPEC | <1 y | - | 10† | 6-12 h | - | + | + | + | + | Raw beef and chicken | - | ||||
| EIEC | Any ages | - | 10† | 24 h | + | + | + | + | + | Hamburger meat and unpasteurized milk | Similar to shigellosis, can cause bloody diarrhea | ||||
| EHEC | Any ages | - | 10 | 3-4 d | - | + | + | + | + | Undercooked or raw hamburger (ground beef) | Known as E. coli O157:H7, can cause HUS/TTP. | ||||
| EAEC | Any ages | + | 1010 | 8-18 h | - | - | + | + | + | - | May cause prolonged or persistent diarrhea in children | ||||
| Salmonella sp. | Any ages | + | 1 | 6 to 72 h | + | + | + | + | + | Meats, poultry, eggs, milk and dairy products, fish, shrimp, spices, yeast, coconut, sauces, freshly prepared salad. | Can cause salmonellosis or typhoid fever. | ||||
| Shigella sp. | Any ages | - | 10 - 200 | 8-48 h | + | + | + | + | + | Raw foods, for example, lettuce, salads (potato, tuna, shrimp, macaroni, and chicken) | Some strains produce enterotoxin and Shiga toxin similar to those produced by E. coli O157:H7 | ||||
| Campylobacter sp. | <5 y, 15-29 y | - | 104 | 2-5 d | + | + | + | + | + | Undercooked poultry products, unpasteurized milk and cheeses made from unpasteurized milk, vegetables, seafood and contaminated water. | May cause bacteremia, Guillain-Barré syndrome (GBS), hemolytic uremic syndrome (HUS) and recurrent colitis | ||||
| Yersinia enterocolitica | <10 y | - | 104 -106 | 1-11 d | + | + | + | + | + | Meats (pork, beef, lamb, etc.), oysters, fish, crabs, and raw milk. | May cause reactive arthritis; glomerulonephritis; endocarditis; erythema nodosum.
can mimic appendicitis and mesenteric lymphadenitis. | ||||
| Clostridium perfringens | Any ages | > 106 | 16 h | - | - | + | + | + | Meats (especially beef and poultry), meat-containing products (e.g., gravies and stews), and Mexican foods. | Can survive high heat, | |||||
| Vibrio cholerae | Any ages | - | 106-1010 | 24-48 h | - | + | + | + | + | Seafoods, including molluscan shellfish (oysters, mussels, and clams), crab, lobster, shrimp, squid, and finfish. | Hypotension, tachycardia, decreased skin turgor. Rice-water stools | ||||
| Parasites | Protozoa | Giardia lamblia | 2-5 y | + | 1 cyst | 1-2 we | - | - | + | + | + | Contaminated water | May cause malabsorption syndrome and severe weight loss | ||
| Entamoeba histolytica | 4-11 y | + | <10 cysts | 2-4 we | - | + | + | + | + | Contaminated water and raw foods | May cause intestinal amebiasis and amebic liver abscess | ||||
| Cryptosporidium parvum | Any ages | - | 10-100 oocysts | 7-10 d | + | + | + | + | + | Juices and milk | May cause copious diarrhea and dehydration in patients with AIDS especially with 180 > CD4 | ||||
| Cyclospora cayetanensis | Any ages | + | 10-100 oocysts | 7-10 d | - | + | + | + | + | Fresh produce, such as raspberries, basil, and several varieties of lettuce. | More common in rainy areas | ||||
| Helminths | Trichinella spp | Any ages | - | Two viable larvae (male and female) | 1-4 we | - | + | + | + | + | Undercooked meats | More common in hunters or people who eat traditionally uncooked meats | |||
| Taenia spp | Any ages | - | 1 larva or egg | 2-4 m | - | + | + | + | + | Undercooked beef and pork | Neurocysticercosis: Cysts located in the brain may be asymptomatic or seizures, increased intracranial pressure, headache. | ||||
| Diphyllobothrium latum | Any ages | - | 1 larva | 15 d | - | - | - | + | + | Raw or undercooked fish. | May cause vitamin B12 deficiency | ||||
8Small bowel diarrhea: watery, voluminous with less than 5 WBC/high power field
Large bowel diarrhea: Mucousy and/or bloody with less volume and more than 10 WBC/high power field
† It could be as high as 1000 based on patient's immunity system.
The table below summarizes the findings that differentiate inflammatory causes of chronic diarrhea[8][9][10][11][11]
| Cause | History | Laboratory findings | Diagnosis | Treatment |
|---|---|---|---|---|
| Diverticulitis |
|
|
Abdominal CT scan with oral and intravenous (IV) contrast | bowel rest, IV fluid resuscitation, and broad-spectrum antimicrobial therapy which covers anaerobic bacteria and gram-negative rods |
| Ulcerative colitis |
|
|
Endoscopy | Induction of remission with mesalamine and corticosteroids followed by the administration of sulfasalazine and 6-Mercaptopurine depending on the severity of the disease. |
| Entamoeba histolytica |
|
cysts shed with the stool | detects ameba DNA in feces | Amebic dysentery
Luminal amebicides for E. histolytica in the colon:
For amebic liver abscess:
|
Gallery
-
3D computer-generated image of a cluster of drug-resistant Campylobacter bacteria. From Public Health Image Library (PHIL). [12]
References
- ↑ 1.0 1.1 Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. pp. pp. 378&ndash, 80. ISBN 0838585299.
- ↑ Moore JE; et al. (2005). "Campylobacter". Vet Res. 36 (3): 351–82. PMID 15845230.
- ↑ Sauerwein R, Bisseling J, Horrevorts A (1993). "Septic abortion associated with Campylobacter fetus subspecies fetus infection: case report and review of the literature". Infection. 21 (5): 331–3. PMID 8300253.
- ↑ Fouts DE; et al. (2005). "Major structural differences and novel potential virulence mechanisms from the genomes of multiple Campylobacter species". PLoS Biol. 3 (1): e15. doi:10.1371/journal.pbio.0030015. PMID 15660156.
- ↑ Grant C, Konkel M, Cieplak W, Tompkins L (1993). "Role of flagella in adherence, internalization, and translocation of Campylobacter jejuni in nonpolarized and polarized epithelial cell cultures". Infect Immun. 61 (5): 1764–71. PMID 8478066.
- ↑ cdc.gov
- ↑ Humphrey, Tom; et al. (2007). "Campylobacters as zoonotic pathogens: A food production perspective <internet>". International Journal of Food Microbiology. 117 (3). doi:10.1016 Check
|doi=value (help). - ↑ Konvolinka CW (1994). "Acute diverticulitis under age forty". Am J Surg. 167 (6): 562–5. PMID 8209928.
- ↑ Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR; et al. (2005). "Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology". Can J Gastroenterol. 19 Suppl A: 5A–36A. PMID 16151544.
- ↑ Satsangi J, Silverberg MS, Vermeire S, Colombel JF (2006). "The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications". Gut. 55 (6): 749–53. doi:10.1136/gut.2005.082909. PMC 1856208. PMID 16698746.
- ↑ 11.0 11.1 Haque R, Huston CD, Hughes M, Houpt E, Petri WA (2003). "Amebiasis". N Engl J Med. 348 (16): 1565–73. doi:10.1056/NEJMra022710. PMID 12700377.
- ↑ "Public Health Image Library (PHIL)".
See also
External links
ca:Campilobàcter de:Campylobacter hr:Campylobacter nl:Campylobacter no:Campylobacter uk:Campylobacter
![3D computer-generated image of a cluster of drug-resistant Campylobacter bacteria. From Public Health Image Library (PHIL). [12]](/images/c/cb/Campylobacter01.jpeg)