Pericarditis treatment
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Pericarditis treatment On the Web |
|
American Roentgen Ray Society Images of Pericarditis treatment |
|
Risk calculators and risk factors for Pericarditis treatment |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2] Ahmed Zaghw, M.D. [3] Homa Najafi, M.D.[4]
Overview
The management of pericarditis depends on whether the patient has an uncomplicated vs. complicated disease course. Uncomplicated pericarditis is generally treated with non-steroidal anti-inflammatory drugs, such as Ibuprofen in cases of either viral or idiopathic pericarditis, and Aspirin in cases of post-MI pericarditis. Pericarditis complicated with either effusion or cardiac tamponade is generally treated with urgent pericardiocentesis in the case of cardiac tamponade, antibiotics in the case of purulent pericardial effusion, and either steroids or colchicine among patients with recurrent or refractory disease.
Management of Uncomplicated Pericarditis
Patients with uncomplicated acute pericarditis can generally be treated and followed up in an outpatient clinic. The treatment of viral or idiopathic pericarditis is with non-steroidal anti-inflammatory drugs. Patients should be observed for side effects since NSAIDs are known to affect the GI mucosa. If the underlying cause of pericarditis is something other than a viral cause, the specific etiology should be treated.
Non-steroidal Anti-inflammatory Drugs (NSAIDs)
NSAIDs are the mainstay of therapy for uncomplicated pericarditis (viral or idiopathic pericarditis). The goal of therapy is to reduce pain and inflammation. While symptoms are improved by NSAIDs, the duration of the episode may not be reduced. The preferred NSAID is ibuprofen which has a large range of doses that can be titrated to the patient's tolerance.[1] Depending on the severity of symptoms, the dosing is between 300-800 mg every 6-8 hours for days or weeks as needed. In order to minimize a recurrence of symptoms, a slow tapering of the NSAID dose may be required. As with all NSAID use, GI prophylaxis should be strongly recommended. Gastroprotection with misoprostol (600 to 800 g/day) or omeprazole (20 mg/day) is highly recommended.[2] The gastroprotection recommendation is based on several studies have evaluated factors that place patients at increased risk of gastroduodenal toxicity from NSAIDs.[3]
The American College of Gastroenterology identified the five most important risk factors for gastroduodenal toxicity:
- Age 60 years (relative risk [RR] 5.52)
- History of an adverse gastroduodenal event (RR 4.76)
- High-dosage NSAIDs (more than twice normal; RR 10.1)
- Concurrent use of glucocorticoids (RR 4.4)
- Concurrent use of anticoagulants (RR 12.7).[4]
Patients with several risk factors are at highest risk of NSAID-induced gastroduodenal toxicity.
Aspirin Therapy
An alternative therapy is aspirin 800 mg every 6-8 hours.[5]
Post-MI Pericarditis
In pericarditis following acute myocardial infarction, NSAIDs other than aspirin should be avoided since they can impair scar formation.
Failure to Respond to a Week of Traditional Therapy
Failure to respond to NSAIDs within one week (as indicated by persistence of fever, a worsening of symptoms such as chest pain, the development of a new pericardial effusion), likely indicates that the underlying cause may not be viral or idiopathic in nature. These patients may require re-evaluation, observation, and more aggressive therapy as described in the next section.
Colchicine
In the European guidelines, colchicine carries a class IIa recommendation for the treatment of an initial episode of pericarditis along with an NSAID. The dose is 0.6 mg bid for 3 months. It should be noted that a long term treatment of colchicine for several weeks or months should be considered, even after disappearance of effusion.[6] [7]
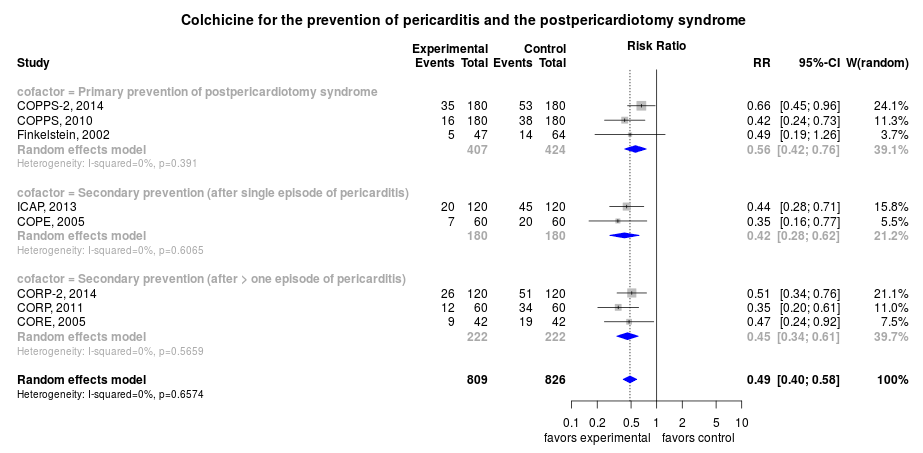
The rate of recurrence after an initial episode is lowered with colchicine therapy by approximately 50% - from 26% to 14% (see Forest plot).[8]
For example, in a multicenter, double-blind trial, the use of colchicine at a dose of 0.5 mg twice daily for 3 months for patients weighing >70 kg or 0.5 mg once daily for patients weighing ≤70 kg in acute pericarditis, when added to conventional antiinflammatory therapy with aspirin or ibuprofen, significantly reduced the rate of symptom persistence at 72 hours (19.2% vs. 40.0%, P=0.001), the number of recurrences per patient (0.21 vs. 0.52, P = 0.001), the hospitalization rate (5.0% vs. 14.2%, P = 0.02), and the remission rate at 1 week (85.0% vs. 58.3%, P<0.001), as compared with placebo.[9]
Steroids
Steroids are not used to treat an initial episode of pericarditis. They provide rapid relief in pain, but are associated with a high rate of recurrence.
Identification of High Risk or Complicated Pericarditis
Patients at high risk of developing complications of pericarditis may required admission to an inpatient service for careful observation for hemodynamic compromise. High risk patients include those with:[5]
- Acute onset
- High fever (> 100.4°F) and leukocytosis
- Development of cardiac tamponade
- Large pericardial effusion (echo-free space > 20 mm) resistant to NSAID treatment
- Immunocompromised status
- History of oral anticoagulation therapy
- Pericarditis secondary to acute trauma
- Failure to respond to seven days of NSAID treatment
Management of Complicated Pericarditis
- Pericardiocentesis may be required to relieve a large effusion or to treat cardiac tamponade.
- Antibiotics are required to manage an underlying bacterial infection or a purulent pericarditis.[10]
|
- † Immediate pericardial fluid removal for hemodynamic compromise
- ‡ Modify regimen and narrow coverage based on results of culture and susceptibility tests.
- Antifungals are required to manage an underlying fungal infection, (Histoplasmosis is the most common fungal cause pericarditis associated with histoplasmosis mediastinitis.[11]
|
- Steroids may be required in recurrent refractory cases or in patients with autoimmune disease.
- Colchicine may be required in patients with recurrent or refractory disease (see below).
- Surgery may be required in the presence of recurrent effusion or constrictive pericarditis.
Management of Cardiac Tamponade and Large Pericardial Effusion
Pericardiocentesis is an invasive procedure in which the pericardial fluid is drained through a needle. A pericardial window is a surgical procedure to drain fluid form the pericardium. Indications for a pericardiocentesis or a pericardial window include the following:[1]
- Cardiac tamponade
- Large, persistent, symptomatic pericardial effusion
- For diagnostic purposes, if there is suspected purulent, tuberculosis, or neoplastic pericarditis.
Management of Recurrent Pericarditis
- Colchicine can be used alone or in conjunction with NSAIDs in prevention and treatment of recurrent pericarditis. Treatment involves an NSAID plus colchicine 2 mg on first day followed by 1 mg daily[5] for three months.[12][13][14] A multicenter, double-blind, randomized trial, showed colchicine at a dose of 0.5 mg twice daily for 3 months for patients weighing >70 kg or 0.5 mg once daily for patients weighing ≤70 kg, in addition to conventional antiinflammatory therapy with aspirin or ibuprofen, reduced the number of recurrences per patient (0.21 vs. 0.52, P = 0.001), as compared with placebo.[9]
- Corticosteroids are usually used in those cases that are clearly refractory to NSAIDs and colchicine and a specific cause has not been found. Systemic corticosteroids are usually reserved for those with autoimmune disease. Steroids are sometimes used in post-operative pericarditis as well.
- Pericardiectomy can be performed if the patient is refractory to medical therapy as a last resort. Most patients will respond to 2 to 3 months of aggressive medical therapy.
Bacterial Pericarditis
Antimicrobial Therapy
1. Bacterial Pericarditis
-
- Preferred regimen: Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 28 days AND Ciprofloxacin 400 mg IV q12h for 28 days
- Alternative regimen (1): Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 28 days AND Cefepime 2 g IV q12h for 28 days
- Alternative regimen (2): Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 14–42 days AND Ceftriaxone 2 g IV q24h for 14–42 days
- Note: Pericardiocentesis must be promptly performed. Pericardial drainage combined with effective systemic antibiotic therapy is mandatory (antistaphylococcal agent plus aminoglycoside, followed by tailored antibiotic therapy according to cultures). Frequent irrigation of the pericardial cavity with urokinase or streptokinase may be considered. Open surgical drainage through subxiphoid pericardiotomy is preferable. Pericardiectomy may be required in patients with dense adhesions, loculated and thick purulent effusion, recurrence of tamponade, persistent infection, and progression to constriction.
-
- 1.2.1. Purulent pericarditis with contiguous pneumonia
- Preferred regimen: Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL AND (Ceftriaxone 1–2 g IV q12h OR Cefotaxime 2 g IV q6–8h) AND (Ciprofloxacin 400 mg IV q12h OR Levofloxacin 500–750 mg IV q24h)
- 1.2.2. Purulent pericarditis with contiguous head and neck infection
- Preferred regimen: Imipenem 500 mg IV q6–8h OR Ampicillin-Sulbactam 3 g IV q6h
- 1.2.3. Purulent pericarditis secondary to infective endocarditis
- Preferred regimen: Vancomycin 15–20 mg/kg IV q8–12h targeting trough levels of 15–20 μg/mL AND Gentamicin 3 mg/kg/day IV q8–12h
- 1.2.4. Purulent pericarditis after cardiac surgery, pediatric
- Preferred regimen: Vancomycin 15 mg/kg IV q6h targeting trough levels of 15–20 μg/mL AND (Ceftriaxone 100 mg/kg/day IV q12–24h OR Cefotaxime 200–300 mg/kg/day IV q6–8h) AND Gentamicin 6–7.5 mg/kg/day IV q8h
- 1.2.5. Purulent pericarditis with genitourinary infection, pediatric
- Preferred regimen: Vancomycin 15 mg/kg IV q6h targeting trough levels of 15–20 μg/mL AND (Ceftriaxone 100 mg/kg/day IV q12–24h OR Cefotaxime 200–300 mg/kg/day IV q6–8h) AND Gentamicin 6–7.5 mg/kg/day IV q8h
- 1.2.6. Purulent pericarditis in immunocompromised host, pediatric
- Preferred regimen: Vancomycin 15 mg/kg IV q6h targeting trough levels of 15–20 μg/mL AND (Ceftriaxone 100 mg/kg/day IV q12–24h OR Cefotaxime 200–300 mg/kg/day IV q6–8h) AND Gentamicin 6–7.5 mg/kg/day IV q8h
- 1.3. Pathogen-directed antimicrobial therapy[21]
- 1.3.1. Anaerobes
- Preferred regimen: Clindamycin 600–900 mg IV q8h for 14–42 days OR Metronidazole 7.5 mg/kg IV q6h for 14–42 days OR Ampicillin-Sulbactam 3 g IV q6h for 14–42 days
- 1.3.2. Gram-negative bacilli
- Preferred regimen: Ciprofloxacin 400 mg IV q12h for 14–42 days OR Levofloxacin 500–750 mg IV q24h for 14–42 days OR Cefepime 2 g IV q12h for 14–42 days
- 1.3.3. Legionella pneumophila
- Preferred regimen: Ciprofloxacin 400 mg IV q12h for 14–42 days OR Levofloxacin 500–750 mg IV q24h for 14–42 days OR Azithromycin 500 mg IV q24h for 14–42 days
- 1.3.4. Mycoplasma pneumoniae
- Preferred regimen: Doxycycline 100 mg IV q12h for 14–42 days OR Azithromycin 500 mg IV q24h for 14–42 days
- 1.3.5. Neisseria meningitidis
- Preferred regimen: Penicillin G 5–24 MU/day IM/IV q4–6h for 14–42 days OR Cefotaxime 2 g IV q6–8h for 14–42 days OR Ceftriaxone 2 g IV q24h for 14–42 days
- 1.3.6. Staphylococcus aureus, methicillin-susceptible
- Preferred regimen: Nafcillin 1–2 g IV q4h for 14–42 days OR Oxacillin 1–2 g IV q4h for 14–42 days OR Cefazolin 1–2 g IV q48h for 14–42 days OR Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 14–42 days OR Clindamycin 600–900 mg IV q8h for 14–42 days
- 1.3.7. Staphylococcus aureus, methicillin-resistant
- Preferred regimen: Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 14–42 days OR Linezolid 600 mg IV q12h for 14–42 days
- 1.3.8. Streptococcus pneumoniae, penicillin-susceptible
- Preferred regimen: Penicillin G 5–24 MU/day IM/IV q4–6h for 14–42 days OR Cefotaxime 2 g IV q6–8h for 14–42 days OR Ciprofloxacin 400 mg IV q12h for 14–42 days OR Levofloxacin 500–750 mg IV q24h for 14–42 days
- 1.3.9. Streptococcus pneumoniae, penicillin-resistant
- Preferred regimen: Ciprofloxacin 400 mg IV q12h for 14–42 days OR Levofloxacin 500–750 mg IV q24h for 14–42 days OR Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 14–42 days
2. Tuberculous Pericarditis
- Preferred regimen: (Isoniazid 5 mg/kg (300 mg) PO qd AND Rifampicin 10 mg/kg (600 mg) PO qd AND Pyrazinamide 1,500 mg PO qd AND Ethambutol 1,200 mg PO qd for 2 months) THEN (Rifampicin 10 mg/kg (600 mg) PO qd AND Pyrazinamide 1,500 mg PO qd for 4 months) AND Prednisolone 1–2 mg/kg/day for 5–7 days with slow taper over 6–8 weeks[22].
- Pediatric doses: Isoniazid 10–15 mg/kg (300 mg); Rifampin 10–20 mg/kg (600 mg); Pyrazinamide 15–30 mg/kg (2.0 g); Ethambutol 15–20 mg/kg daily (1.0 g).
- Note: Intrapericardial drainage is done if needed. If constriction develops inspite of medical therapy, pericardiectomy is indicated.[23].
3. Viral pericarditis[23]
- 3.1. CMV pericarditis
- Preferred regimen: Immunoglobulin 1 time per day 4 ml/kg on day 0, 4, and 8; 2 ml/kg on day 12 and 16.
- Note: Symptomatic treatment is given to the patients with viral pericarditis while in large effusions and cardiac tamponade pericardiocentesis is necessary. The use of corticosteroid therapy is contraindicated except in patients with secondary tuberculous pericarditis, as an adjunct to tuberculosis treatment. Drainage, if needed is done.
- 3.2. Coxsackie B pericarditis
- Preferred regimen: Interferon alpha or beta 2,5 Mio. IU/m2 surface area s.c. 3 times per week
- Note: Symptomatic treatment is given to the patients with viral pericarditis while in large effusions and cardiac tamponade pericardiocentesis is necessary. The use of corticosteroid therapy is contraindicated except in patients with secondary tuberculous pericarditis, as an adjunct to tuberculosis treatment. Drainage, if needed is done.
- 3.3. Adenovirus and parvovirus B19 perimyocarditis
- Preferred regimen: Immunoglobulin 10 g IV at day 1 and 3 for 6–8 hours
- Note: Symptomatic treatment is given to the patients with viral pericarditis while in large effusions and cardiac tamponade pericardiocentesis is necessary. The use of corticosteroid therapy is contraindicated except in patients with secondary tuberculous pericarditis, as an adjunct to tuberculosis treatment. Drainage, if needed is done.
4. Fungal Pericarditis[23]
- Empiric therapy : Fluconazole, Ketoconazole, Itraconazole, Amphotericin B, Liposomal amphotericin B or Amphotericin B lipid complex is indicated.
- 4.1. Histoplasmosis
- Preferred regimen: Nonsteroidal anti-inflammatory drugs given during 2–12 weeks.
- Note: Corticosteroids and NSAIDs can support the treatment with antifungal drugs. Pericardiocentesis or surgical treatment is indicated for haemodynamic impairment. Pericardiectomy is indicated in fungal constrictive pericarditis.
- 4.2. Nocardiosis
- Preferred regimen: Sulfonamides are the drugs of choice.
- Note: Corticosteroids and NSAIDs can support the treatment with antifungal drugs. Pericardiocentesis or surgical treatment is indicated for haemodynamic impairment. Pericardiectomy is indicated in fungal constrictive pericarditis.
- 4.3. Actinomycosis
- Preferred regimen: Combination of three antibiotics including Penicillin.
- Note: Corticosteroids and NSAIDs can support the treatment with antifungal drugs. Pericardiocentesis or surgical treatment is indicated for haemodynamic impairment. Pericardiectomy is indicated in fungal constrictive pericarditis.
2006 ACC/AHA/ESC Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death (DO NOT EDIT)[24]
Pericardial Diseases (DO NOT EDIT)[24]
| Class I |
| "1. Ventricular arrhythmias that develop in patients with pericardial disease should be treated in the same manner that such arrhythmias are treated in patients with other diseases including ICD and pacemaker implantation as required. Patients receiving ICD implantation should be receiving chronic optimal medical therapy and have reasonable expectation of survival with a good functional status for more than 1 year. (Level of Evidence: C)" |
References
- ↑ 1.0 1.1 Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmuller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH (2004). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology". Eur Heart J. 25 (7): 587–10. doi:10.1016/j.ehj.2004.02.002. PMID 15120056.
- ↑ Imazio, M.; Demichelis, B.; Parrini, I.; Giuggia, M.; Cecchi, E.; Gaschino, G.; Demarie, D.; Ghisio, A.; Trinchero, R. (2004). "Day-hospital treatment of acute pericarditis: a management program for outpatient therapy". J Am Coll Cardiol. 43 (6): 1042–6. doi:10.1016/j.jacc.2003.09.055. PMID 15028364. Unknown parameter
|month=ignored (help) - ↑ Gabriel, SE.; Jaakkimainen, L.; Bombardier, C. (1991). "Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. A meta-analysis". Ann Intern Med. 115 (10): 787–96. PMID 1834002. Unknown parameter
|month=ignored (help) - ↑ Lanza, FL. (1998). "A guideline for the treatment and prevention of NSAID-induced ulcers. Members of the Ad Hoc Committee on Practice Parameters of the American College of Gastroenterology". Am J Gastroenterol. 93 (11): 2037–46. doi:10.1111/j.1572-0241.1998.00588.x. PMID 9820370. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 Imazio M, Demichelis B, Parrini I, Giuggia M, Cecchi E, Gaschino G, Demarie D, Ghisio A, Trinchero R (2004). "Day-hospital treatment of acute pericarditis: a management program for outpatient therapy". J Am Coll Cardiol. 43 (6): 1042–6. doi:10.1016/j.jacc.2003.09.055. PMID 15028364.
- ↑ Imazio, M.; Brucato, A.; Forno, D.; Ferro, S.; Belli, R.; Trinchero, R.; Adler, Y. (2012). "Efficacy and safety of colchicine for pericarditis prevention. Systematic review and meta-analysis". Heart. 98 (14): 1078–82. doi:10.1136/heartjnl-2011-301306. PMID 22442198. Unknown parameter
|month=ignored (help) - ↑ Imazio, M.; Bobbio, M.; Cecchi, E.; Demarie, D.; Demichelis, B.; Pomari, F.; Moratti, M.; Gaschino, G.; Giammaria, M. (2005). "Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial". Circulation. 112 (13): 2012–6. doi:10.1161/CIRCULATIONAHA.105.542738. PMID 16186437. Unknown parameter
|month=ignored (help) - ↑ Colchicine for pericarditis: a living systematic review. GitHub. Available at http://openmetaanalysis.github.io/Colchicine-for-Pericarditis/. Accessed November 16, 2014.
- ↑ 9.0 9.1 Imazio, M.; Brucato, A.; Cemin, R.; Ferrua, S.; Maggiolini, S.; Beqaraj, F.; Demarie, D.; Forno, D.; Ferro, S. (2013). "A Randomized Trial of Colchicine for Acute Pericarditis". N Engl J Med. doi:10.1056/NEJMoa1208536. PMID 23992557. Unknown parameter
|month=ignored (help) - ↑ Parikh, SV.; Memon, N.; Echols, M.; Shah, J.; McGuire, DK.; Keeley, EC. (2009). "Purulent pericarditis: report of 2 cases and review of the literature". Medicine (Baltimore). 88 (1): 52–65. doi:10.1097/MD.0b013e318194432b. PMID 19352300. Unknown parameter
|month=ignored (help) - ↑ Wheat, LJ.; Freifeld, AG.; Kleiman, MB.; Baddley, JW.; McKinsey, DS.; Loyd, JE.; Kauffman, CA. (2007). "Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America". Clin Infect Dis. 45 (7): 807–25. doi:10.1086/521259. PMID 17806045. Unknown parameter
|month=ignored (help) - ↑ Adler Y, Zandman-Goddard G, Ravid M, Avidan B, Zemer D, Ehrenfeld M, Shemesh J, Tomer Y, Shoenfeld Y (1994). "Usefulness of colchicine in preventing recurrences of pericarditis". Am J of Cardiol. 73 (12): 916–7. doi:10.1016/0002-9149(94)90828-1. PMID 8184826.
- ↑ Imazio M, Bobbio M, Cecchi E, Demarie D, Demichelis B, Pomari F, Moratti M, Gaschino G, Giammaria M, Ghisio A, Belli R, Trinchero R (2005). "Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial". Circulation. 112 (13): 2012–6. doi:10.1161/CIRCULATIONAHA.105.542738. PMID 16186437.
- ↑ Imazio M, Bobbio M, Cecchi E, Demarie D, Pomari F, Moratti M, Ghisio A, Belli R, Trinchero R (2005). "Colchicine as first-choice therapy for recurrent pericarditis: results of the CORE (COlchicine for REcurrent pericarditis) trial". Arch Intern Med. 165 (17): 1987–91. doi:10.1001/archinte.165.17.1987. PMID 16186468.
- ↑ Gilbert, David (2015). The Sanford guide to antimicrobial therapy. Sperryville, Va: Antimicrobial Therapy. ISBN 978-1930808843.
- ↑ Bartlett, John (2012). Johns Hopkins ABX guide : diagnosis and treatment of infectious diseases. Burlington, MA: Jones and Bartlett Learning. ISBN 978-1449625580.
- ↑ Maisch, Bernhard; Seferović, Petar M.; Ristić, Arsen D.; Erbel, Raimund; Rienmüller, Reiner; Adler, Yehuda; Tomkowski, Witold Z.; Thiene, Gaetano; Yacoub, Magdi H.; Task Force on the Diagnosis and Management of Pricardial Diseases of the European Society of Cardiology (2004-04). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology". European Heart Journal. 25 (7): 587–610. doi:10.1016/j.ehj.2004.02.002. ISSN 0195-668X. PMID 15120056. Check date values in:
|date=(help) - ↑ Pankuweit, Sabine; Ristić, Arsen D.; Seferović, Petar M.; Maisch, Bernhard (2005). "Bacterial pericarditis: diagnosis and management". American Journal of Cardiovascular Drugs: Drugs, Devices, and Other Interventions. 5 (2): 103–112. ISSN 1175-3277. PMID 15725041.
- ↑ Goodman, null (2000-08). "Purulent Pericarditis". Current Treatment Options in Cardiovascular Medicine. 2 (4): 343–350. ISSN 1092-8464. PMID 11096539. Check date values in:
|date=(help) - ↑ Cherry, James (2014). Feigin and Cherry's textbook of pediatric infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455711772.
- ↑ Bartlett, John (2012). Johns Hopkins ABX guide : diagnosis and treatment of infectious diseases. Burlington, MA: Jones and Bartlett Learning. ISBN 978-1449625580.
- ↑ Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN; et al. (2003). "American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis". Am J Respir Crit Care Med. 167 (4): 603–62. doi:10.1164/rccm.167.4.603. PMID 12588714.
- ↑ 23.0 23.1 23.2 Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y; et al. (2004). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology". Eur Heart J. 25 (7): 587–610. doi:10.1016/j.ehj.2004.02.002. PMID 15120056.
- ↑ 24.0 24.1 Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M; et al. (2006). "ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation. 114 (10): e385–484. doi:10.1161/CIRCULATIONAHA.106.178233. PMID 16935995.