Pericarditis treatment: Difference between revisions
Hardik Patel (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (98 intermediate revisions by 15 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Pericarditis}} | {{Pericarditis}} | ||
{{CMG}}; | {{CMG}}; {{AE}} {{CZ}} {{AZ}}{{Homa}} | ||
==Overview== | ==Overview== | ||
The management of | The management of pericarditis depends on whether the [[patient]] has an uncomplicated vs. complicated [[disease]] course. Uncomplicated pericarditis is generally treated with [[non-steroidal anti-inflammatory drug]]s, such as [[Ibuprofen]] in cases of either [[viral]] or [[idiopathic]] pericarditis, and [[Aspirin]] in cases of post-[[MI]] pericarditis. Pericarditis complicated with either [[pericardial effusion|effusion]] or [[cardiac tamponade]] is generally treated with [[Urgent care|urgent]] [[pericardiocentesis]] in the case of [[cardiac tamponade]], [[antibiotics]] in the case of purulent [[pericardial effusion]], and either [[steroids]] or [[colchicine]] among [[patients]] with [[Recurrent pericarditis|recurrent]] or [[refractory]] [[disease]]. | ||
==Management of Uncomplicated Pericarditis | ==Management of Uncomplicated Pericarditis== | ||
Patients with uncomplicated [[acute pericarditis]] can generally be treated and followed up in an outpatient clinic. The treatment of [[viral]] or idiopathic pericarditis is with [[non-steroidal anti-inflammatory drug]]s. Patients should be observed for side effects since [[NSAID]]s are known to affect the GI mucosa. If the underlying cause of pericarditis is something other than a viral cause, the specific etiology should be treated. | [[Patients]] with uncomplicated [[acute pericarditis]] can generally be treated and followed up in an [[outpatient]] [[clinic]]. The treatment of [[viral]] or [[idiopathic]] pericarditis is with [[non-steroidal anti-inflammatory drug]]s. [[Patients]] should be observed for [[side effects]] since [[NSAID]]s are known to affect the [[Gastrointestinal tract|GI]] [[mucosa]]. If the underlying [[Causes|cause]] of pericarditis is something other than a [[viral]] cause, the specific [[etiology]] should be treated. | ||
===Non-steroidal Anti-inflammatory Drugs (NSAIDs)=== | |||
* [[NSAIDs]] are the mainstay of [[therapy]] for uncomplicated pericarditis ([[viral]] or [[idiopathic]] pericarditis). The goal of [[therapy]] is to [[Reduction|reduce]] [[pain]] and [[inflammation]]. While [[symptoms]] are improved by [[NSAID]]s, the duration of the episode may not be [[reduced]]. The preferred [[NSAID]] is [[ibuprofen]] which has a large [[Range (statistics)|range]] of [[doses]] that can be titrated to the [[Patient|patient's]] [[tolerance]]. Depending on the severity of [[symptoms]], the [[dosing]] is between 300-800 mg every 6-8 hours for days or weeks as needed. In order to minimize a recurrence of [[symptoms]], a [[slow]] tapering of the [[NSAID]] [[dose]] may be required. As with all [[NSAID]] use, [[GI]] [[prophylaxis]] should be strongly recommended. Gastroprotection with [[misoprostol]] (600 to 800 g/day) or [[omeprazole]] (20 mg/day) is highly recommended. The gastroprotection recommendation is based on several studies have evaluated factors that place [[patients]] at increased risk of [[Gastroduodenal ulcer|gastroduodenal]] [[toxicity]] from [[NSAIDs]].<ref name="Gabriel-1991">{{Cite journal | last1 = Gabriel | first1 = SE. | last2 = Jaakkimainen | first2 = L. | last3 = Bombardier | first3 = C. | title = Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. A meta-analysis. | journal = Ann Intern Med | volume = 115 | issue = 10 | pages = 787-96 | month = Nov | year = 1991 | doi = | PMID = 1834002 }}</ref><ref name="maisch2">{{cite journal | author= Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmuller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH | title= Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology | journal= Eur Heart J | year=2004 | pages=587–10 | volume=25 | issue=7 | pmid=15120056 | doi= 10.1016/j.ehj.2004.02.002}}</ref><ref name="Imazio-2004">{{Cite journal | last1 = Imazio | first1 = M. | last2 = Demichelis | first2 = B. | last3 = Parrini | first3 = I. | last4 = Giuggia | first4 = M. | last5 = Cecchi | first5 = E. | last6 = Gaschino | first6 = G. | last7 = Demarie | first7 = D. | last8 = Ghisio | first8 = A. | last9 = Trinchero | first9 = R. | title = Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. | journal = J Am Coll Cardiol | volume = 43 | issue = 6 | pages = 1042-6 | month = Mar | year = 2004 | doi = 10.1016/j.jacc.2003.09.055 | PMID = 15028364 }}</ref> | |||
* The [[American College of Gastroenterology Guidelines|American College of Gastroenterology]] identified the five most important [[risk factors]] for [[Gastroduodenal ulcer|gastroduodenal]] [[toxicity]]:<ref name="Lanza-1998">{{Cite journal | last1 = Lanza | first1 = FL. | title = A guideline for the treatment and prevention of NSAID-induced ulcers. Members of the Ad Hoc Committee on Practice Parameters of the American College of Gastroenterology. | journal = Am J Gastroenterol | volume = 93 | issue = 11 | pages = 2037-46 | month = Nov | year = 1998 | doi = 10.1111/j.1572-0241.1998.00588.x | PMID = 9820370 }}</ref> | |||
:*[[Age]] 60 years ([[relative risk]] [RR] 5.52) | |||
:*History of an adverse [[Gastroduodenal ulcer|gastroduodenal]] event (RR 4.76) | |||
:*High-dosage [[NSAIDs]] (more than twice normal; RR 10.1) | |||
:*[[Concurrent overlap|Concurrent]] use of [[glucocorticoids]] (RR 4.4) | |||
:*[[Concurrent overlap|Concurrent]] use of [[anticoagulants]] (RR 12.7). | |||
'''Note:''' [[Patients]] with several [[risk factors]] are at the highest risk of [[NSAID]]-induced [[Gastroduodenal ulcer|gastroduodenal]] [[toxicity]]. | |||
===Aspirin Therapy=== | ===Aspirin Therapy=== | ||
An alternative therapy is [[aspirin]] 800 mg every 6-8 hours.<ref name="imazio2">{{cite journal | author= Imazio M, Demichelis B, Parrini I, Giuggia M, Cecchi E, Gaschino G, Demarie D, Ghisio A, Trinchero R | title= Day-hospital treatment of acute pericarditis: a management program for outpatient therapy | journal= J Am Coll Cardiol | year=2004 | pages=1042–6 | volume=43 | issue=6 | pmid=15028364 | doi= 10.1016/j.jacc.2003.09.055}}</ref> | An [[alternative therapy]] is [[aspirin]] 800 mg every 6-8 hours.<ref name="imazio2">{{cite journal | author= Imazio M, Demichelis B, Parrini I, Giuggia M, Cecchi E, Gaschino G, Demarie D, Ghisio A, Trinchero R | title= Day-hospital treatment of acute pericarditis: a management program for outpatient therapy | journal= J Am Coll Cardiol | year=2004 | pages=1042–6 | volume=43 | issue=6 | pmid=15028364 | doi= 10.1016/j.jacc.2003.09.055}}</ref> | ||
===Post-MI Pericarditis=== | ===Post-MI Pericarditis=== | ||
In pericarditis following [[acute myocardial infarction]], [[NSAIDs]] other than [[aspirin]] should be avoided since they can impair scar formation. | In pericarditis following [[acute myocardial infarction]], [[NSAIDs]] other than [[aspirin]] should be avoided since they can impair [[scar]] formation. | ||
===Failure to Respond to a Week of Traditional Therapy=== | ===Failure to Respond to a Week of Traditional Therapy=== | ||
Failure to respond to [[NSAIDs]] within one week (as indicated by persistence of [[fever]], a worsening of symptoms such as [[chest pain]], the development of a new [[pericardial effusion]]), likely indicates that the underlying cause may not be viral or idiopathic in nature. These patients may require re-evaluation, observation, and more aggressive therapy as described in the next section. | Failure to respond to [[NSAIDs]] within one week (as indicated by persistence of [[fever]], a worsening of [[symptoms]] such as [[chest pain]], the [[development]] of a new [[pericardial effusion]]), likely indicates that the underlying [[Causes|cause]] may not be [[viral]] or [[idiopathic]] in nature. These [[patients]] may require [[Re-evaluation Counseling|re-evaluation]], [[observation]], and more aggressive [[therapy]] as described in the next section. | ||
===Colchicine=== | ===Colchicine=== | ||
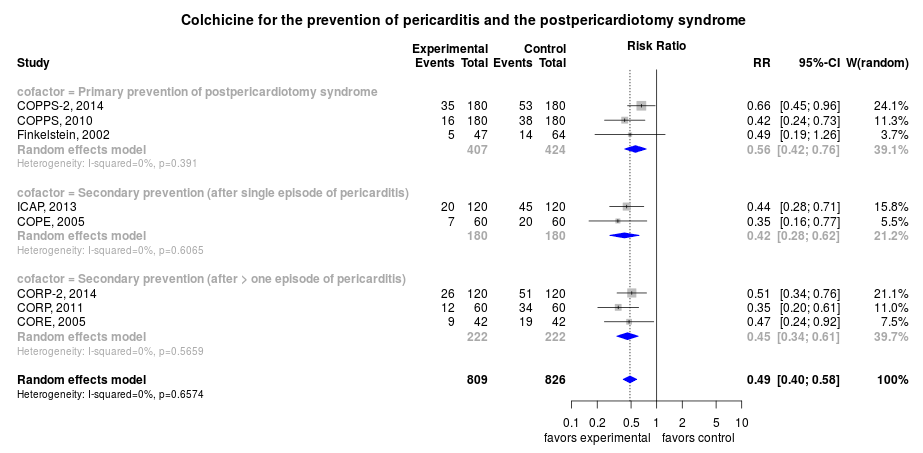
In the European guidelines, [[colchicine]] carries a [[ACC AHA guidelines classification scheme#Classification of Recommendations|class IIa]] recommendation for the treatment of an initial episode of pericarditis along with an [[NSAID]]. The dose is 0.6 mg bid for 3 months. The rate of recurrence is lowered with [[colchicine]] therapy from | In the European guidelines, [[colchicine]] carries a [[ACC AHA guidelines classification scheme#Classification of Recommendations|class IIa]] recommendation for the [[Therapy|treatment]] of an initial episode of pericarditis along with an [[NSAID]]. The [[dose]] is 0.6 mg bid for 3 months. It should be noted that a long term [[Therapy|treatment]] of [[colchicine]] for several weeks or months should be considered, even after disappearance of [[Pericardial Effusion|effusion]].<ref name="Imazio-2012">{{Cite journal | last1 = Imazio | first1 = M. | last2 = Brucato | first2 = A. | last3 = Forno | first3 = D. | last4 = Ferro | first4 = S. | last5 = Belli | first5 = R. | last6 = Trinchero | first6 = R. | last7 = Adler | first7 = Y. | title = Efficacy and safety of colchicine for pericarditis prevention. Systematic review and meta-analysis. | journal = Heart | volume = 98 | issue = 14 | pages = 1078-82 | month = Jul | year = 2012 | doi = 10.1136/heartjnl-2011-301306 | PMID = 22442198 }}</ref> <ref name="Imazio-2005">{{Cite journal | last1 = Imazio | first1 = M. | last2 = Bobbio | first2 = M. | last3 = Cecchi | first3 = E. | last4 = Demarie | first4 = D. | last5 = Demichelis | first5 = B. | last6 = Pomari | first6 = F. | last7 = Moratti | first7 = M. | last8 = Gaschino | first8 = G. | last9 = Giammaria | first9 = M. | title = Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial. | journal = Circulation | volume = 112 | issue = 13 | pages = 2012-6 | month = Sep | year = 2005 | doi = 10.1161/CIRCULATIONAHA.105.542738 | PMID = 16186437 }}</ref> | ||
The rate of recurrence after an initial episode is lowered with [[colchicine]] therapy by approximately 50% - from 26% to 14% (see [http://www.wikidoc.org/index.php/File:Colchicine_for_the_prevention_of_pericarditis_and_the_pospericardiotomy_syndrome.png Forest plot]).<ref>Colchicine for pericarditis: a living systematic review. GitHub. Available at http://openmetaanalysis.github.io/Colchicine-for-Pericarditis/. Accessed November 16, 2014.</ref> | |||
[[Image:Colchicine_for_the_prevention_of_pericarditis_and_the_pospericardiotomy_syndrome.png|400px]] | |||
For example, in a [[Multicenter trial|multicenter]], [[double-blind trial]], the use of [[colchicine]] at a [[dose]] of 0.5 mg twice daily for 3 months for [[patients]] weighing >70 kg or 0.5 mg once daily for [[patients]] weighing ≤70 kg in [[acute pericarditis]], when added to conventional [[antiinflammatory]] [[therapy]] with [[aspirin]] or [[ibuprofen]], significantly reduced the [[rate]] of [[symptom]] persistence at 72 hours (19.2% vs. 40.0%, P=0.001), the [[number]] of recurrences per [[patient]] (0.21 vs. 0.52, P = 0.001), the [[hospitalization]] [[rate]] (5.0% vs. 14.2%, P = 0.02), and the [[Remission (medicine)|remission]] [[Rate (mathematics)|rate]] at 1 week (85.0% vs. 58.3%, P<0.001), as compared with [[placebo]].<ref name="Imazio-2013">{{Cite journal | last1 = Imazio | first1 = M. | last2 = Brucato |first2 = A. | last3 = Cemin | first3 = R. | last4 = Ferrua | first4 = S. | last5 = Maggiolini | first5 = S. | last6 = Beqaraj | first6 = F. | last7 = Demarie | first7 = D.| last8 = Forno | first8 = D. | last9 = Ferro | first9 = S. | title = A Randomized Trial of Colchicine for Acute Pericarditis. | journal = N Engl J Med | volume = | issue = | pages = | month = Aug | year = 2013 | doi = 10.1056/NEJMoa1208536 | PMID = 23992557 }}</ref> | |||
===Steroids=== | ===Steroids=== | ||
| Line 24: | Line 41: | ||
==Identification of High Risk or Complicated Pericarditis== | ==Identification of High Risk or Complicated Pericarditis== | ||
Patients at high risk of developing complications of pericarditis may required admission to an inpatient service for careful observation for hemodynamic compromise. High risk patients include those with:<ref name="imazio2">{{cite journal | author= Imazio M, Demichelis B, Parrini I, Giuggia M, Cecchi E, Gaschino G, Demarie D, Ghisio A, Trinchero R | title= Day-hospital treatment of acute pericarditis: a management program for outpatient therapy | journal= J Am Coll Cardiol | year=2004 | pages=1042–6 | volume=43 | issue=6 | pmid=15028364 | doi= 10.1016/j.jacc.2003.09.055}}</ref> | [[Patients]] at high risk of developing [[complications]] of pericarditis may required admission to an [[inpatient]] service for careful [[observation]] for [[Hemodynamics|hemodynamic]] compromise. High risk [[patients]] include those with:<ref name="imazio2">{{cite journal | author= Imazio M, Demichelis B, Parrini I, Giuggia M, Cecchi E, Gaschino G, Demarie D, Ghisio A, Trinchero R | title= Day-hospital treatment of acute pericarditis: a management program for outpatient therapy | journal= J Am Coll Cardiol | year=2004 | pages=1042–6 | volume=43 | issue=6 | pmid=15028364 | doi= 10.1016/j.jacc.2003.09.055}}</ref> | ||
* Acute onset | *[[Acute]] onset | ||
* High [[fever]] (> 100.4°F) and [[leukocytosis]] | * High [[fever]] (> 100.4°F) and [[leukocytosis]] | ||
* Development of [[cardiac tamponade]] | *[[Development]] of [[cardiac tamponade]] | ||
* Large [[pericardial effusion]] (echo-free space > 20 mm) resistant to [[NSAID]] treatment | * Large [[pericardial effusion]] (echo-free space > 20 mm) resistant to [[NSAID]] [[Therapy|treatment]] | ||
* Immunocompromised status | *[[Immunocompromised]] status | ||
* History of oral [[anticoagulation]] therapy | * History of [[oral]] [[anticoagulation]] [[therapy]] | ||
* Pericarditis secondary to acute [[trauma]] | * Pericarditis [[secondary]] to [[acute]] [[trauma]] | ||
* Failure to respond to seven days of [[NSAID]] treatment | *[[Failure]] to respond to seven days of [[NSAID]] [[Therapy|treatment]] | ||
==Management of Complicated Pericarditis== | ==Management of Complicated Pericarditis== | ||
*[[Pericardiocentesis]] may be required to relieve a large effusion or to treat [[cardiac tamponade]]. | *[[Pericardiocentesis]] may be required to relieve a large [[Pericardial Effusion|effusion]] or to [[Therapy|treat]] [[cardiac tamponade]]. | ||
*[[Antibiotic]]s | |||
*[[Steroid]]s may be required in recurrent refractory cases or in patients with [[autoimmune disease]]. | <div class="mw-collapsible mw-collapsed"> | ||
*[[Colchicine]] may be required in patients with recurrent or refractory disease (see below). | |||
*[[Surgery]] may be required in the presence of recurrent effusion or [[constrictive pericarditis]]. | *[[Antibiotic]]s are required to manage an underlying [[bacterial]] [[infection]] or a [[purulent pericarditis]].<ref name="Parikh-2009">{{Cite journal | last1 = Parikh | first1 = SV. | last2 = Memon | first2 = N. | last3 = Echols | first3 = M. | last4 = Shah | first4 = J. | last5 = McGuire | first5 = DK. | last6 = Keeley | first6 = EC. | title = Purulent pericarditis: report of 2 cases and review of the literature. | journal = Medicine (Baltimore) | volume = 88 | issue = 1 | pages = 52-65 | month = Jan | year = 2009 | doi = 10.1097/MD.0b013e318194432b | PMID = 19352300 }}</ref> | ||
<div class="mw-collapsible-content"> | |||
{| | |||
|- | |||
| valign=top | | |||
{| style="margin: 0 0 0em 0em; border: 1px solid #696969; float: left; width:48em" cellpadding="0" cellspacing="0"; | |||
! style="padding: 0 5px; font-size: 100%; background: #F8F8FF" align=left | ''{{fontcolor|#6C7B8B|Drainage in most of cases for culture and local antibiotics † }}'' | |||
|- | |||
|style="font-size: 95%; padding: 0 5px; background: #DCDCDC" align=left | ''PLUS'' | |||
|- | |||
! style="padding: 0 5px; font-size: 100%; background: #F8F8FF" align=left | ''{{fontcolor|#6C7B8B|Primary Systemic Regimens in Bacterial Pericarditis ‡ }} | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Vancomycin]]: 15-20 mg/kg q8-12h (target troughs of 15-20 μg/mL) x ???? wks''''' | |||
|- | |||
|style="font-size: 95%; padding: 0 5px; background: #DCDCDC" align=left | ''PLUS'' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |▸ '''''[[Ceftriaxone]]: 2 gm IV q24h x ??? wks''''' <br> or <br> ▸ '''''[[Cefepime]]: 2 gm IV q12h x ??? wks ''''' | |||
|- | |||
! style="padding: 0 5px; font-size: 100%; background: #F8F8FF" align=left | ''{{fontcolor|#6C7B8B|Alternative Systemic Regimens in Bacterial Pericarditis}}'' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Vancomycin]]: 15-20 mg/kg q8-12h (target troughs of 15-20 μg/mL) x ??? wks''''' | |||
|- | |||
|style="font-size: 95%; padding: 0 5px; background: #DCDCDC" align=left | ''PLUS'' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Ciprofloxacin]]: 750 mg po bid or 400 mg IV bid''''' | |||
|- | |||
|} | |||
|} | |||
:† Immediate pericardial fluid removal for hemodynamic compromise | |||
:‡ Modify regimen and narrow coverage based on results of [[culture]] and susceptibility tests. | |||
</div></div> | |||
<div class="mw-collapsible mw-collapsed"> | |||
*[[Antifungal]]s are required to manage an underlying [[fungal]] [[infection]], ([[Histoplasmosis]] is the most common [[fungal]] cause pericarditis associated with [[histoplasmosis]] [[mediastinitis]].<ref name="Wheat-2007">{{Cite journal | last1 = Wheat | first1 = LJ. | last2 = Freifeld | first2 = AG. | last3 = Kleiman | first3 = MB. | last4 = Baddley | first4 = JW. | last5 = McKinsey | first5 = DS. | last6 = Loyd | first6 = JE. | last7 = Kauffman | first7 = CA. | title = Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. | journal = Clin Infect Dis | volume = 45 | issue = 7 | pages = 807-25 | month = Oct | year = 2007 | doi = 10.1086/521259 | PMID = 17806045 }}</ref> | |||
<div class="mw-collapsible-content"> | |||
{| | |||
|- | |||
| valign=top | | |||
{| style="margin: 0 0 0em 0em; border: 1px solid #696969; float: left; width:48em" cellpadding="0" cellspacing="0"; | |||
! style="padding: 0 5px; font-size: 100%; background: #F8F8FF" align=left | ''{{fontcolor|#6C7B8B|Mild Histoplasmosis Pericarditis}}'' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Ibuprofen]]: 300-800 mg q 6-8 hrs x 1-2 wks as needed, to be tapered †'''''<br> ''OR'' <br> ▸ '''''[[Indomethacin]]: 50 mg q8 hrs x 1-2 wks as needed, to be tapered ''''' | |||
|- | |||
|style="font-size: 95%; padding: 0 5px; background: #DCDCDC" align=left | ''PLUS'' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |▸ '''''[[Colchicine]]: 0.5 to 0.6 mg two times daily x 3 months''''' | |||
|- | |||
! style="padding: 0 5px; font-size: 100%; background: #F8F8FF" align=left | ''{{fontcolor|#6C7B8B|NSAID Non-Responders or Hemodynamic Compromise Histoplasmosis Pericarditis}}'' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Prednisone]]: 1 mg/kg po daily tapered over 1–2 wks ''''' | |||
|- | |||
|style="font-size: 95%; padding: 0 5px; background: #DCDCDC" align=left | ''PLUS'' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |▸ '''''[[Itraconazole]]: 200 mg po 3 times daily x 3 days, then twice daily x 6–12 wks)''''' | |||
|- | |||
|style="font-size: 95%; padding: 0 5px; background: #DCDCDC" align=left | ''PLUS'' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |▸ '''''Pericardial fluid removal for hemodynamic compromise''''' | |||
|- | |||
|} | |||
|} | |||
</div></div> | |||
*[[Steroid]]s may be required in recurrent [[refractory]] cases or in [[patients]] with [[autoimmune disease]]. | |||
*[[Colchicine]] may be required in [[patients]] with recurrent or [[refractory]] [[disease]] (see below). | |||
*[[Surgery]] may be required in the presence of recurrent [[Pericardial Effusion|effusion]] or [[constrictive pericarditis]]. | |||
===Management of Cardiac Tamponade and Large Pericardial Effusion=== | ===Management of Cardiac Tamponade and Large Pericardial Effusion=== | ||
[[Pericardiocentesis]] is an invasive procedure in which the pericardial fluid is drained through a needle. A [[pericardial window]] is a surgical procedure to drain fluid form the [[pericardium]]. Indications for a [[ | [[Pericardiocentesis]] is an [[invasive]] [[procedure]] in which the [[pericardial fluid]] is [[Drain (surgery)|drained]] through a [[needle]]. A [[pericardial window]] is a [[surgical procedure]] to [[Drain (surgery)|drain]] [[fluid]] form the [[pericardium]]. Indications for a [[pericardiocentesis]] or a [[pericardial window]] include the following:<ref name="maisch2">{{cite journal | author= Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmuller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH | title= Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology | journal= Eur Heart J | year=2004 | pages=587–10 | volume=25 | issue=7 | pmid=15120056 | doi= 10.1016/j.ehj.2004.02.002}}</ref> | ||
*[[Cardiac tamponade]] | *[[Cardiac tamponade]] | ||
*Large, persistent, symptomatic [[pericardial effusion]] | *Large, persistent, [[symptomatic]] [[pericardial effusion]] | ||
*For diagnostic purposes, if there is suspected [[purulent]], [[tuberculosis]], or [[neoplastic]] pericarditis. | *For [[diagnostic]] purposes, if there is suspected [[purulent]], [[tuberculosis]], or [[neoplastic]] pericarditis. | ||
==Management of Recurrent Pericarditis== | ==Management of Recurrent Pericarditis== | ||
*[[Colchicine]] can be used alone or in conjunction with [[NSAID]]s in [[prevention]] and [[Therapy|treatment]] of [[recurrent pericarditis]]. [[Therapy|Treatment]] involves an [[NSAID]] plus [[colchicine]] 2 mg on first day followed by 1 mg daily for three months. A [[Multicenter trial|multicenter]], [[double-blind]], [[randomized trial]], showed [[colchicine]] at a dose of 0.5 mg twice daily for 3 months for [[patients]] weighing >70 kg or 0.5 mg once daily for [[patients]] weighing ≤70 kg, in addition to conventional [[antiinflammatory]] [[therapy]] with [[aspirin]] or [[ibuprofen]], reduced the number of recurrences per [[patient]] (0.21 vs. 0.52, P = 0.001), as compared with [[placebo]].<ref name="Imazio-2013">{{Cite journal | last1 = Imazio | first1 = M. | last2 = Brucato | first2 = A. | last3 = Cemin | first3 = R. | last4 = Ferrua | first4 = S. | last5 = Maggiolini | first5 = S. | last6 = Beqaraj | first6 = F. | last7 = Demarie | first7 = D. | last8 = Forno | first8 = D. | last9 = Ferro | first9 = S. | title = A Randomized Trial of Colchicine for Acute Pericarditis. | journal = N Engl J Med | volume = | issue = | pages = | month = Aug | year = 2013 | doi = 10.1056/NEJMoa1208536 | PMID = 23992557 }}</ref><ref name="adler">{{cite journal | author= Adler Y, Zandman-Goddard G, Ravid M, Avidan B, Zemer D, Ehrenfeld M, Shemesh J, Tomer Y, Shoenfeld Y | title= Usefulness of colchicine in preventing recurrences of pericarditis | journal= Am J of Cardiol | year=1994| pages=916–7 | volume=73 | issue=12 | pmid=8184826 | doi= 10.1016/0002-9149(94)90828-1}}</ref><ref name="imazio3">{{cite journal | author= Imazio M, Bobbio M, Cecchi E, Demarie D, Demichelis B, Pomari F, Moratti M, Gaschino G, Giammaria M, Ghisio A, Belli R, Trinchero R | title= Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial | journal= Circulation | year=2005| pages=2012–6 | volume=112 | issue=13 | pmid=16186437 | doi= 10.1161/CIRCULATIONAHA.105.542738}}</ref><ref name="imazio4">{{cite journal | author= Imazio M, Bobbio M, Cecchi E, Demarie D, Pomari F, Moratti M, Ghisio A, Belli R, Trinchero R | title= Colchicine as first-choice therapy for recurrent pericarditis: results of the CORE (COlchicine for REcurrent pericarditis) trial | journal= Arch Intern Med | year=2005| pages=1987–91 | volume=165 | issue=17 | pmid=16186468 | doi= 10.1001/archinte.165.17.1987}}</ref><ref name="LittleFreeman2006">{{cite journal|last1=Little|first1=William C.|last2=Freeman|first2=Gregory L.|title=Pericardial Disease|journal=Circulation|volume=113|issue=12|year=2006|pages=1622–1632|issn=0009-7322|doi=10.1161/CIRCULATIONAHA.105.561514}}</ref> | |||
[[Colchicine]] can be used alone or in conjunction with | *[[Corticosteroids]] are usually used in those cases that are clearly [[refractory]] to [[NSAID]]s and [[colchicine]] and a specific [[Causes|cause]] has not been found. [[Systemic]] [[corticosteroids]] are usually reserved for those with [[autoimmune disease]]. [[Steroid]]s are sometimes used in post-operative pericarditis as well. | ||
*[[Pericardiectomy]] can be performed if the [[patient]] is [[refractory]] to medical [[therapy]] as a last resort. Most [[patients]] will respond to 2 to 3 months of aggressive [[medical]] [[therapy]]. | |||
==Bacterial Pericarditis== | |||
===Antimicrobial Therapy=== | |||
1. '''Bacterial Pericarditis''' | |||
:* 1.1. '''Empiric antimicrobial therapy'''<ref>{{cite book | last = Gilbert | first = David | title = The Sanford guide to antimicrobial therapy | publisher = Antimicrobial Therapy | location = Sperryville, Va | year = 2015 | isbn = 978-1930808843 }}</ref><ref>{{cite book | last = Bartlett | first = John | title = Johns Hopkins ABX guide : diagnosis and treatment of infectious diseases | publisher = Jones and Bartlett Learning | location = Burlington, MA | year = 2012 | isbn = 978-1449625580 }}</ref> | |||
:::* Preferred regimen: [[Vancomycin]] 1 g [[Intravenous therapy|IV]] q12h targeting trough levels of 15–20 μg/mL for 28 days {{and}} [[Ciprofloxacin]] 400 mg [[Intravenous therapy|IV]] q12h for 28 days | |||
:::* Alternative regimen (1): [[Vancomycin]] 1 g [[Intravenous therapy|IV]] q12h targeting trough [[levels]] of 15–20 μg/mL for 28 days {{and}} [[Cefepime]] 2 g [[Intravenous therapy|IV]] q12h for 28 days | |||
:::* Alternative regimen (2): [[Vancomycin]] 1 g [[Intravenous therapy|IV]] q12h targeting trough levels of 15–20 μg/mL for 14–42 days {{and}} [[Ceftriaxone]] 2 g [[Intravenous therapy|IV]] q24h for 14–42 days | |||
::::'''Note''': [[Pericardiocentesis]] must be promptly performed. [[Pericardial]] [[Drain (surgery)|drainage]] combined with effective [[systemic]] [[antibiotic]] [[therapy]] is mandatory ([[Antistaphylococcal penicillins|antistaphylococcal agent]] plus [[aminoglycoside]], followed by tailored [[antibiotic therapy]] according to [[Growth medium|cultures]]). Frequent [[Irrigation tank|irrigation]] of the [[pericardial cavity]] with [[urokinase]] or [[streptokinase]] may be considered. Open [[surgical]] [[Drain (surgery)|drainage]] through [[subxiphoid]] pericardiotomy is preferable. [[Pericardiectomy]] may be required in [[patients]] with [[dense]] [[adhesions]], loculated and thick [[purulent]] [[Pericardial Effusion|effusion]], recurrence of [[tamponade]], persistent [[infection]], and progression to constriction. | |||
:* 1.2. '''Specific considerations'''<ref>{{Cite journal| doi = 10.1016/j.ehj.2004.02.002| issn = 0195-668X| volume = 25| issue = 7| pages = 587–610| last1 = Maisch| first1 = Bernhard| last2 = Seferović| first2 = Petar M.| last3 = Ristić| first3 = Arsen D.| last4 = Erbel| first4 = Raimund| last5 = Rienmüller| first5 = Reiner| last6 = Adler| first6 = Yehuda| last7 = Tomkowski| first7 = Witold Z.| last8 = Thiene| first8 = Gaetano| last9 = Yacoub| first9 = Magdi H.| last10 = Task Force on the Diagnosis and Management of Pricardial Diseases of the European Society of Cardiology| title = Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology| journal = European Heart Journal| date = 2004-04| pmid = 15120056}}</ref><ref>{{Cite journal| issn = 1175-3277| volume = 5| issue = 2| pages = 103–112| last1 = Pankuweit| first1 = Sabine| last2 = Ristić| first2 = Arsen D.| last3 = Seferović| first3 = Petar M.| last4 = Maisch| first4 = Bernhard| title = Bacterial pericarditis: diagnosis and management| journal = American Journal of Cardiovascular Drugs: Drugs, Devices, and Other Interventions| date = 2005| pmid = 15725041}}</ref><ref>{{Cite journal| issn = 1092-8464| volume = 2| issue = 4| pages = 343–350| last = Goodman| first = null| title = Purulent Pericarditis| journal = Current Treatment Options in Cardiovascular Medicine| date = 2000-08| pmid = 11096539}}</ref><ref>{{cite book | last = Cherry | first = James | title = Feigin and Cherry's textbook of pediatric infectious diseases | publisher = Elsevier/Saunders | location = Philadelphia, PA | year = 2014 | isbn = 978-1455711772 }}</ref> | |||
::* 1.2.1. '''Purulent pericarditis with contiguous pneumonia''' | |||
:::* Preferred regimen: [[Vancomycin]] 1 g [[Intravenous therapy|IV]] q12h targeting trough levels of 15–20 μg/mL {{and}} ([[Ceftriaxone]] 1–2 g [[Intravenous therapy|IV]] q12h {{or}} [[Cefotaxime]] 2 g [[Intravenous therapy|IV]] q6–8h) {{and}} ([[Ciprofloxacin]] 400 mg [[Intravenous therapy|IV]] q12h {{or}} [[Levofloxacin]] 500–750 mg [[Intravenous therapy|IV]] q24h) | |||
::* 1.2.2. '''Purulent pericarditis with contiguous head and neck infection''' | |||
:::* Preferred regimen: [[Imipenem]] 500 mg [[Intravenous therapy|IV]] q6–8h {{or}} [[Ampicillin-Sulbactam]] 3 g [[Intravenous therapy|IV]] q6h | |||
::* 1.2.3. '''Purulent pericarditis secondary to infective endocarditis''' | |||
:::* Preferred regimen: [[Vancomycin]] 15–20 mg/kg [[Intravenous therapy|IV]] q8–12h targeting trough levels of 15–20 μg/mL {{and}} [[Gentamicin]] 3 mg/kg/day [[Intravenous therapy|IV]] q8–12h | |||
::* 1.2.4. '''Purulent pericarditis after cardiac surgery, pediatric''' | |||
:::* Preferred regimen: [[Vancomycin]] 15 mg/kg [[Intravenous therapy|IV]] q6h targeting trough levels of 15–20 μg/mL {{and}} ([[Ceftriaxone]] 100 mg/kg/day [[Intravenous therapy|IV]] q12–24h {{or}} [[Cefotaxime]] 200–300 mg/kg/day [[Intravenous therapy|IV]] q6–8h) {{and}} [[Gentamicin]] 6–7.5 mg/kg/day [[Intravenous therapy|IV]] q8h | |||
::* 1.2.5. '''Purulent pericarditis with genitourinary infection, pediatric''' | |||
:::* Preferred regimen: [[Vancomycin]] 15 mg/kg [[Intravenous therapy|IV]] q6h targeting trough levels of 15–20 μg/mL {{and}} ([[Ceftriaxone]] 100 mg/kg/day [[Intravenous therapy|IV]] q12–24h {{or}} [[Cefotaxime]] 200–300 mg/kg/day [[Intravenous therapy|IV]] q6–8h) {{and}} [[Gentamicin]] 6–7.5 mg/kg/day [[Intravenous therapy|IV]] q8h | |||
::* 1.2.6. '''Purulent pericarditis in immunocompromised host, pediatric''' | |||
:::* Preferred regimen: [[Vancomycin]] 15 mg/kg [[Intravenous therapy|IV]] q6h targeting trough levels of 15–20 μg/mL {{and}} ([[Ceftriaxone]] 100 mg/kg/day [[Intravenous therapy|IV]] q12–24h {{or}} [[Cefotaxime]] 200–300 mg/kg/day [[Intravenous therapy|IV]] q6–8h) {{and}} [[Gentamicin]] 6–7.5 mg/kg/day [[Intravenous therapy|IV]] q8h | |||
:* 1.3. '''Pathogen-directed antimicrobial therapy'''<ref>{{cite book | last = Bartlett | first = John | title = Johns Hopkins ABX guide : diagnosis and treatment of infectious diseases | publisher = Jones and Bartlett Learning | location = Burlington, MA | year = 2012 | isbn = 978-1449625580 }}</ref> | |||
::* 1.3.1. '''Anaerobes''' | |||
:::* Preferred regimen: [[Clindamycin]] 600–900 mg [[Intravenous therapy|IV]] q8h for 14–42 days {{or}} [[Metronidazole]] 7.5 mg/kg [[Intravenous therapy|IV]] q6h for 14–42 days {{or}} [[Ampicillin-Sulbactam]] 3 g [[Intravenous therapy|IV]] q6h for 14–42 days | |||
::* 1.3.2. '''Gram-negative bacilli''' | |||
:::* Preferred regimen: [[Ciprofloxacin]] 400 mg [[Intravenous therapy|IV]] q12h for 14–42 days {{or}} [[Levofloxacin]] 500–750 mg [[Intravenous therapy|IV]] q24h for 14–42 days {{or}} [[Cefepime]] 2 g [[Intravenous therapy|IV]] q12h for 14–42 days | |||
::* 1.3.3. '''Legionella pneumophila''' | |||
:::* Preferred regimen: [[Ciprofloxacin]] 400 mg [[Intravenous therapy|IV]] q12h for 14–42 days {{or}} [[Levofloxacin]] 500–750 mg [[Intravenous therapy|IV]] q24h for 14–42 days {{or}} [[Azithromycin]] 500 mg [[Intravenous therapy|IV]] q24h for 14–42 days | |||
::* 1.3.4. '''Mycoplasma pneumoniae''' | |||
:::* Preferred regimen: [[Doxycycline]] 100 mg [[Intravenous therapy|IV]] q12h for 14–42 days {{or}} [[Azithromycin]] 500 mg [[Intravenous therapy|IV]] q24h for 14–42 days | |||
::* 1.3.5. '''Neisseria meningitidis''' | |||
:::* Preferred regimen: [[Penicillin G]] 5–24 MU/day IM/[[Intravenous therapy|IV]] q4–6h for 14–42 days {{or}} [[Cefotaxime]] 2 g [[Intravenous therapy|IV]] q6–8h for 14–42 days {{or}} [[Ceftriaxone]] 2 g [[Intravenous therapy|IV]] q24h for 14–42 days | |||
::* 1.3.6. '''Staphylococcus aureus, methicillin-susceptible''' | |||
:::* Preferred regimen: [[Nafcillin]] 1–2 g [[Intravenous therapy|IV]] q4h for 14–42 days {{or}} [[Oxacillin]] 1–2 g [[Intravenous therapy|IV]] q4h for 14–42 days {{or}} [[Cefazolin]] 1–2 g [[Intravenous therapy|IV]] q48h for 14–42 days {{or}} [[Vancomycin]] 1 g [[Intravenous therapy|IV]] q12h targeting trough levels of 15–20 μg/mL for 14–42 days {{or}} [[Clindamycin]] 600–900 mg [[Intravenous therapy|IV]] q8h for 14–42 days | |||
::* 1.3.7. '''Staphylococcus aureus, methicillin-resistant''' | |||
:::* Preferred regimen: [[Vancomycin]] 1 g [[Intravenous therapy|IV]] q12h targeting trough levels of 15–20 μg/mL for 14–42 days {{or}} [[Linezolid]] 600 mg [[Intravenous therapy|IV]] q12h for 14–42 days | |||
::* 1.3.8. '''Streptococcus pneumoniae, penicillin-susceptible''' | |||
:::* Preferred regimen: [[Penicillin G]] 5–24 MU/day IM/[[Intravenous therapy|IV]] q4–6h for 14–42 days {{or}} [[Cefotaxime]] 2 g [[Intravenous therapy|IV]] q6–8h for 14–42 days {{or}} [[Ciprofloxacin]] 400 mg [[Intravenous therapy|IV]] q12h for 14–42 days {{or}} [[Levofloxacin]] 500–750 mg [[Intravenous therapy|IV]] q24h for 14–42 days | |||
::* 1.3.9. '''Streptococcus pneumoniae, penicillin-resistant''' | |||
[[ | :::* Preferred regimen: [[Ciprofloxacin]] 400 mg [[Intravenous therapy|IV]] q12h for 14–42 days {{or}} [[Levofloxacin]] 500–750 mg [[Intravenous therapy|IV]] q24h for 14–42 days {{or}} [[Vancomycin]] 1 g [[Intravenous therapy|IV]] q12h targeting trough levels of 15–20 μg/mL for 14–42 days | ||
[[ | |||
2. '''Tuberculous Pericarditis'''<ref name="pmid15120056">{{cite journal| author=Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y et al.| title=Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. | journal=Eur Heart J | year= 2004 | volume= 25 | issue= 7 | pages= 587-610 | pmid=15120056 | doi=10.1016/j.ehj.2004.02.002 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15120056 }} </ref>. | |||
:* Preferred regimen: ([[Isoniazid]] 5 mg/kg (300 mg) PO qd {{and}} [[Rifampicin]] 10 mg/kg (600 mg) PO qd {{and}} [[Pyrazinamide]] 1,500 mg PO qd {{and}} [[Ethambutol]] 1,200 mg PO qd for 2 months) {{then}} ([[Rifampicin]] 10 mg/kg (600 mg) PO qd {{and}} [[Pyrazinamide]] 1,500 mg PO qd for 4 months) {{and}} [[Prednisolone]] 1–2 mg/kg/day for 5–7 days with slow taper over 6–8 weeks<ref name="pmid12588714">{{cite journal| author=Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN et al.| title=American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. | journal=Am J Respir Crit Care Med | year= 2003 | volume= 167 | issue= 4 | pages= 603-62 | pmid=12588714 | doi=10.1164/rccm.167.4.603 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12588714 }} </ref>. | |||
:* Pediatric doses: [[Isoniazid]] 10–15 mg/kg (300 mg); [[Rifampin]] 10–20 mg/kg (600 mg); [[Pyrazinamide]] 15–30 mg/kg (2.0 g); [[Ethambutol]] 15–20 mg/kg daily (1.0 g). | |||
:*'''Note:''' Intrapericardial drainage is done if needed. If constriction develops inspite of medical therapy, [[pericardiectomy]] is indicated. | |||
3. '''Viral pericarditis'''<ref name="pmid15120056">{{cite journal| author=Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y et al.| title=Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. | journal=Eur Heart J | year= 2004 | volume= 25 | issue= 7 | pages= 587-610 | pmid=15120056 | doi=10.1016/j.ehj.2004.02.002 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15120056 }} </ref> | |||
:* 3.1. '''CMV pericarditis''' | |||
::* Preferred regimen: [[Immunoglobulin]] 1 time per day 4 ml/kg on day 0, 4, and 8; 2 ml/kg on day 12 and 16. | |||
:::'''Note:''' [[Symptomatic]] [[Therapy|treatment]] is given to the [[patients]] with [[viral]] [[pericarditis]] while in large [[Pericardial Effusion|effusions]] and [[cardiac tamponade]] [[pericardiocentesis]] is necessary. The use of [[corticosteroid]] [[therapy]] is [[contraindicated]] except in [[patients]] with [[secondary]] [[tuberculous pericarditis]], as an adjunct to [[tuberculosis]] [[Therapy|treatment]]. [[Drain (surgery)|Drainage]], if needed is done. | |||
:* 3.2. '''Coxsackie B pericarditis''' | |||
::* Preferred regimen: [[ Interferon]] alpha or beta 2,5 Mio. IU/m<sup>2</sup> [[surface area]] [[Subcutaneous|SC]] 3 times per week | |||
:::'''Note:''' [[Symptomatic]] [[Therapy|treatment]] is given to the [[patients]] with [[viral]] [[pericarditis]] while in large [[Pericardial effusion|effusions]] and [[cardiac tamponade]] [[pericardiocentesis]] is necessary. The use of [[corticosteroid]] [[therapy]] is [[contraindicated]] except in [[patients]] with [[secondary]] [[tuberculous pericarditis]], as an adjunct to [[tuberculosis]] treatment. [[Drain (surgery)|Drainage]], if needed is done. | |||
:* 3.3. '''Adenovirus and parvovirus B19 perimyocarditis''' | |||
::* Preferred regimen: [[Immunoglobulin]] 10 g [[Intravenous therapy|IV]] at day 1 and 3 for 6–8 hours | |||
:::'''Note:''' [[Symptomatic]] [[Therapy|treatment]] is given to the [[patients]] with [[viral]] [[pericarditis]] while in large [[Pericardial effusion|effusions]] and [[cardiac tamponade]] [[pericardiocentesis]] is necessary. The use of [[corticosteroid]] [[therapy]] is [[contraindicated]] except in [[patients]] with [[secondary]] [[tuberculous pericarditis]], as an adjunct to [[tuberculosis]] treatment. [[Drain (surgery)|Drainage]], if needed is done. | |||
4. '''Fungal Pericarditis'''<ref name="pmid15120056">{{cite journal| author=Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y et al.| title=Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. | journal=Eur Heart J | year= 2004 | volume= 25 | issue= 7 | pages= 587-610 | pmid=15120056 | doi=10.1016/j.ehj.2004.02.002 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15120056 }} </ref> | |||
:* Empiric therapy : [[Fluconazole]], [[Ketoconazole]], [[Itraconazole]], [[Amphotericin B]], Liposomal [[amphotericin B]] or [[Amphotericin B]] lipid complex is indicated. | |||
::* 4.1. '''Histoplasmosis''' | |||
:::* Preferred regimen: [[Nonsteroidal anti-inflammatory drugs]] given during 2–12 weeks. | |||
::::'''Note''': [[Corticosteroids]] and [[NSAIDs]] can support the [[Therapy|treatment]] with [[Antifungal drug|antifungal drugs]]. [[Pericardiocentesis]] or [[Surgery|surgical]] [[Therapy|treatment]] is indicated for [[Hemodynamics|haemodynamic]] [[impairment]]. [[Pericardiectomy]] is indicated in [[fungal]] [[constrictive pericarditis]]. | |||
::* 4.2. '''Nocardiosis''' | |||
:::* Preferred regimen: [[Sulfonamides]] are the [[drugs]] of choice. | |||
::::'''Note:''' [[Corticosteroids]] and [[NSAIDs]] can support the [[Therapy|treatment]] with [[Antifungal drug|antifungal drugs]]. [[Pericardiocentesis]] or [[Surgery|surgical]] [[Therapy|treatment]] is indicated for [[Hemodynamics|haemodynamic]] [[impairment]]. [[Pericardiectomy]] is indicated in [[fungal]] [[constrictive pericarditis]]. | |||
::* 4.3. '''Actinomycosis''' | |||
:::* Preferred regimen: Combination of three [[antibiotics]] including [[Penicillin]]. | |||
::::'''Note:''' [[Corticosteroids]] and [[NSAIDs]] can support the [[Therapy|treatment]] with [[Antifungal drug|antifungal drugs]]. [[Pericardiocentesis]] or [[Surgery|surgical]] [[Therapy|treatment]] is indicated for [[Hemodynamics|haemodynamic]] [[impairment]]. [[Pericardiectomy]] is indicated in [[fungal]] [[constrictive pericarditis]]. | |||
==2006 ACC/AHA/ESC Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death (DO NOT EDIT)<ref name="pmid16935995">{{cite journal| author=Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M et al.| title=ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. | journal=Circulation | year= 2006 | volume= 114 | issue= 10 | pages= e385-484 | pmid=16935995 | doi=10.1161/CIRCULATIONAHA.106.178233 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16935995}}</ref>== | |||
===Pericardial Diseases (DO NOT EDIT)<ref name="pmid16935995">{{cite journal| author=Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M et al.| title=ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. | journal=Circulation | year= 2006 | volume= 114 |issue= 10 | pages= e385-484 | pmid=16935995 | doi=10.1161/CIRCULATIONAHA.106.178233 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16935995}}</ref>=== | |||
{|class="wikitable" | {|class="wikitable" | ||
|- | |- | ||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA Guidelines Classification Scheme#Classification of Recommendations|Class I]] | | colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA Guidelines Classification Scheme#Classification of Recommendations|Class I]] | ||
|- | |- | ||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' [[Ventricular arrhythmias]] that develop in patients with pericardial disease should be treated in the same manner that such [[arrhythmias]] are treated in patients with other diseases including [[ICD]] and [[pacemaker]] implantation as required. Patients receiving ICD implantation should be receiving chronic optimal medical therapy and have reasonable expectation of survival with a good functional status for more than 1 | | bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' [[Ventricular arrhythmias]] that develop in [[Patient|patients]] with [[pericardial disease]] should be [[Therapy|treated]] in the same manner that such [[arrhythmias]] are [[Therapy|treated]] in [[Patient|patients]] with other [[diseases]] including [[ICD]] and [[pacemaker]] [[implantation]] as required. [[Patients]] receiving [[ICD]] [[implantation]] should be receiving [[Chronic (medicine)|chronic]] optimal [[medical]] [[therapy]] and have reasonable [[expectation]] of [[Survival rate|survival]] with a good functional status for more than 1 year. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | ||
|} | |||
==2015 ESC Guidelines on the Diagnosis and Treatment of Pericarditis (DO NOT EDIT)<ref name="AdlerCharron2015">{{cite journal|last1=Adler|first1=Yehuda|last2=Charron|first2=Philippe|last3=Imazio|first3=Massimo|last4=Badano|first4=Luigi|last5=Barón-Esquivias|first5=Gonzalo|last6=Bogaert|first6=Jan|last7=Brucato|first7=Antonio|last8=Gueret|first8=Pascal|last9=Klingel|first9=Karin|last10=Lionis|first10=Christos|last11=Maisch|first11=Bernhard|last12=Mayosi|first12=Bongani|last13=Pavie|first13=Alain|last14=Ristić|first14=Arsen D.|last15=Sabaté Tenas|first15=Manel|last16=Seferovic|first16=Petar|last17=Swedberg|first17=Karl|last18=Tomkowski|first18=Witold|title=2015 ESC Guidelines for the diagnosis and management of pericardial diseases|journal=European Heart Journal|volume=36|issue=42|year=2015|pages=2921–2964|issn=0195-668X|doi=10.1093/eurheartj/ehv318}}</ref>== | |||
=== Recommendations for the management of acute pericarditis === | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ESC Guidelines Classification Scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki></nowiki>'''1.''' [[Hospital]] [[Admission note|admission]] is recommended for high-risk [[patients]] with [[acute pericarditis]] (at least one [[risk factor]]). | |||
'''2.''' [[Outpatient]] management is recommended for low-risk [[patients]] with [[acute pericarditis]]. | |||
'''3.''' Evaluation of response to [[Anti inflammatory medications|anti-inflammatory therapy]] is recommended after 1 week. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: B]])<ref name="ImazioDemichelis2004">{{cite journal|last1=Imazio|first1=Massimo|last2=Demichelis|first2=Brunella|last3=Parrini|first3=Iris|last4=Giuggia|first4=Marco|last5=Cecchi|first5=Enrico|last6=Gaschino|first6=Gianni|last7=Demarie|first7=Daniela|last8=Ghisio|first8=Aldo|last9=Trinchero|first9=Rita|title=Day-hospital treatment of acute pericarditis|journal=Journal of the American College of Cardiology|volume=43|issue=6|year=2004|pages=1042–1046|issn=07351097|doi=10.1016/j.jacc.2003.09.055}}</ref><ref name="ImazioCecchi2007">{{cite journal|last1=Imazio|first1=Massimo|last2=Cecchi|first2=Enrico|last3=Demichelis|first3=Brunella|last4=Ierna|first4=Salvatore|last5=Demarie|first5=Daniela|last6=Ghisio|first6=Aldo|last7=Pomari|first7=Franco|last8=Coda|first8=Luisella|last9=Belli|first9=Riccardo|last10=Trinchero|first10=Rita|title=Indicators of Poor Prognosis of Acute Pericarditis|journal=Circulation|volume=115|issue=21|year=2007|pages=2739–2744|issn=0009-7322|doi=10.1161/CIRCULATIONAHA.106.662114}}</ref>'' | |||
''<nowiki/>'' | |||
|} | |||
=== Recommendations for the treatment of acute pericarditis=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ESC Guidelines Classification Scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki></nowiki>'''1.''' [[Aspirin]] or [[NSAIDs]] are recommended as [[first-line therapy]] for [[acute pericarditis]] with gastroprotection.<ref name="LotrionteBiondi-Zoccai2010">{{cite journal|last1=Lotrionte|first1=Marzia|last2=Biondi-Zoccai|first2=Giuseppe|last3=Imazio|first3=Massimo|last4=Castagno|first4=Davide|last5=Moretti|first5=Claudio|last6=Abbate|first6=Antonio|last7=Agostoni|first7=Pierfrancesco|last8=Brucato|first8=Antonio L.|last9=Di Pasquale|first9=Pietro|last10=Raatikka|first10=Marja|last11=Sangiorgi|first11=Giuseppe|last12=Laudito|first12=Antonio|last13=Sheiban|first13=Imad|last14=Gaita|first14=Fiorenzo|title=International collaborative systematic review of controlled clinical trials on pharmacologic treatments for acute pericarditis and its recurrences|journal=American Heart Journal|volume=160|issue=4|year=2010|pages=662–670|issn=00028703|doi=10.1016/j.ahj.2010.06.015}}</ref> | |||
'''2.''' [[Colchicine]] is recommended as [[first-line therapy]] for [[acute pericarditis]] as an adjunct to [[aspirin]]/[[NSAIDs|NSAID]] [[therapy]]. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: A]])<ref name="ImazioBobbio2005">{{cite journal|last1=Imazio|first1=Massimo|last2=Bobbio|first2=Marco|last3=Cecchi|first3=Enrico|last4=Demarie|first4=Daniela|last5=Demichelis|first5=Brunella|last6=Pomari|first6=Franco|last7=Moratti|first7=Mauro|last8=Gaschino|first8=Gianni|last9=Giammaria|first9=Massimo|last10=Ghisio|first10=Aldo|last11=Belli|first11=Riccardo|last12=Trinchero|first12=Rita|title=Colchicine in Addition to Conventional Therapy for Acute Pericarditis|journal=Circulation|volume=112|issue=13|year=2005|pages=2012–2016|issn=0009-7322|doi=10.1161/CIRCULATIONAHA.105.542738}}</ref><ref name="ImazioBrucato2013">{{cite journal|last1=Imazio|first1=Massimo|last2=Brucato|first2=Antonio|last3=Cemin|first3=Roberto|last4=Ferrua|first4=Stefania|last5=Maggiolini|first5=Stefano|last6=Beqaraj|first6=Federico|last7=Demarie|first7=Daniela|last8=Forno|first8=Davide|last9=Ferro|first9=Silvia|last10=Maestroni|first10=Silvia|last11=Belli|first11=Riccardo|last12=Trinchero|first12=Rita|last13=Spodick|first13=David H.|last14=Adler|first14=Yehuda|title=A Randomized Trial of Colchicine for Acute Pericarditis|journal=New England Journal of Medicine|volume=369|issue=16|year=2013|pages=1522–1528|issn=0028-4793|doi=10.1056/NEJMoa1208536}}</ref><ref name="ImazioBrucato2014">{{cite journal|last1=Imazio|first1=Massimo|last2=Brucato|first2=Antonio|last3=Belli|first3=Riccardo|last4=Forno|first4=Davide|last5=Ferro|first5=Silvia|last6=Trinchero|first6=Rita|last7=Adler|first7=Yehuda|title=Colchicine for the prevention of pericarditis|journal=Journal of Cardiovascular Medicine|volume=15|issue=12|year=2014|pages=840–846|issn=1558-2027|doi=10.2459/JCM.0000000000000103}}</ref><ref name="AlabedCabello2014">{{cite journal|last1=Alabed|first1=Samer|last2=Cabello|first2=Juan B|last3=Irving|first3=Greg J|last4=Qintar|first4=Mohammed|last5=Burls|first5=Amanda|title=Colchicine for pericarditis|journal=Cochrane Database of Systematic Reviews|year=2014|issn=14651858|doi=10.1002/14651858.CD010652.pub2}}</ref>'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki>'''1.''' [[Serum]] [[C-reactive protein|CRP]] should be considered to guide the [[Therapy|treatment]] length and assess the response to [[therapy]]. | |||
'''2.''' Low-[[dose]] [[corticosteroids]] should be considered for [[acute pericarditis]] in cases of [[contraindication]]/[[failure]] of [[aspirin]]/[[NSAIDs]] and [[colchicine]], and when an [[infectious]] [[Causes|cause]] has been excluded, or when there is a specific [[Indication (medicine)|indication]] such as [[autoimmune disease]]. | |||
'''3.''' [[Exercise]] [[restriction]] should be considered for non-[[athletes]] with [[acute pericarditis]] until [[resolution]] of [[symptoms]] and [[Normalization model|normalization]] of [[CRP]], [[The electrocardiogram|ECG]], and [[echocardiogram]]. | |||
'''4.''' For [[athletes]], the duration of [[exercise]] [[restriction]] should be considered until [[resolution]] of [[symptoms]] and normalization of [[CRP]], [[The electrocardiogram|ECG]], and [[echocardiogram]]—at least 3 months is recommended. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightCoral"|[[ESC guidelines classification scheme#Classification of Recommendations|Class III]] | |||
|- | |||
|bgcolor="LightCoral" |<nowiki></nowiki> [[Corticosteroids]] are not recommended as [[first-line therapy]] for [[acute pericarditis]]. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence:]] <nowiki/>[[ACC AHA Guidelines Classification Scheme#Level of Evidence|C]])'' | |||
|} | |||
=== Recommendations for the management of recurrent pericarditis=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ESC Guidelines Classification Scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki></nowiki>'''1.''' [[Aspirin]] and [[NSAIDs]] are mainstays of [[Therapy|treatment]] and are recommended at full [[doses]], if tolerated, until complete [[symptom]] [[resolution]].<ref name="LotrionteBiondi-Zoccai2010">{{cite journal|last1=Lotrionte|first1=Marzia|last2=Biondi-Zoccai|first2=Giuseppe|last3=Imazio|first3=Massimo|last4=Castagno|first4=Davide|last5=Moretti|first5=Claudio|last6=Abbate|first6=Antonio|last7=Agostoni|first7=Pierfrancesco|last8=Brucato|first8=Antonio L.|last9=Di Pasquale|first9=Pietro|last10=Raatikka|first10=Marja|last11=Sangiorgi|first11=Giuseppe|last12=Laudito|first12=Antonio|last13=Sheiban|first13=Imad|last14=Gaita|first14=Fiorenzo|title=International collaborative systematic review of controlled clinical trials on pharmacologic treatments for acute pericarditis and its recurrences|journal=American Heart Journal|volume=160|issue=4|year=2010|pages=662–670|issn=00028703|doi=10.1016/j.ahj.2010.06.015}}</ref><ref name="ImazioBrucato2014">{{cite journal|last1=Imazio|first1=Massimo|last2=Brucato|first2=Antonio|last3=Trinchero|first3=Rita|last4=Spodick|first4=David|last5=Adler|first5=Yehuda|title=Individualized therapy for pericarditis|journal=Expert Review of Cardiovascular Therapy|volume=7|issue=8|year=2014|pages=965–975|issn=1477-9072|doi=10.1586/erc.09.82}}</ref> | |||
'''2.''' [[Colchicine]] (0.5 mg twice daily or 0.5 mg daily for [[patients]], 70 kg or intolerant to higher [[doses]]); use for 6 months is recommended as an adjunct to [[aspirin]]/[[NSAIDs]].''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: A]])<ref name="Imazio2011">{{cite journal|last1=Imazio|first1=Massimo|title=Colchicine for Recurrent Pericarditis (CORP)|journal=Annals of Internal Medicine|volume=155|issue=7|year=2011|pages=409|issn=0003-4819|doi=10.7326/0003-4819-155-7-201110040-00359}}</ref><ref name="ImazioBelli2014">{{cite journal|last1=Imazio|first1=Massimo|last2=Belli|first2=Riccardo|last3=Brucato|first3=Antonio|last4=Cemin|first4=Roberto|last5=Ferrua|first5=Stefania|last6=Beqaraj|first6=Federico|last7=Demarie|first7=Daniela|last8=Ferro|first8=Silvia|last9=Forno|first9=Davide|last10=Maestroni|first10=Silvia|last11=Cumetti|first11=Davide|last12=Varbella|first12=Ferdinando|last13=Trinchero|first13=Rita|last14=Spodick|first14=David H|last15=Adler|first15=Yehuda|title=Efficacy and safety of colchicine for treatment of multiple recurrences of pericarditis (CORP-2): a multicentre, double-blind, placebo-controlled, randomised trial|journal=The Lancet|volume=383|issue=9936|year=2014|pages=2232–2237|issn=01406736|doi=10.1016/S0140-6736(13)62709-9}}</ref><ref name="ImazioBobbio2005">{{cite journal|last1=Imazio|first1=Massimo|last2=Bobbio|first2=Marco|last3=Cecchi|first3=Enrico|last4=Demarie|first4=Daniela|last5=Pomari|first5=Franco|last6=Moratti|first6=Mauro|last7=Ghisio|first7=Aldo|last8=Belli|first8=Riccardo|last9=Trinchero|first9=Rita|title=Colchicine as First-Choice Therapy for Recurrent Pericarditis|journal=Archives of Internal Medicine|volume=165|issue=17|year=2005|pages=1987|issn=0003-9926|doi=10.1001/archinte.165.17.1987}}</ref><ref name="ImazioBrucato2014">{{cite journal|last1=Imazio|first1=Massimo|last2=Brucato|first2=Antonio|last3=Belli|first3=Riccardo|last4=Forno|first4=Davide|last5=Ferro|first5=Silvia|last6=Trinchero|first6=Rita|last7=Adler|first7=Yehuda|title=Colchicine for the prevention of pericarditis|journal=Journal of Cardiovascular Medicine|volume=15|issue=12|year=2014|pages=840–846|issn=1558-2027|doi=10.2459/JCM.0000000000000103}}</ref><ref name="AlabedCabello2014">{{cite journal|last1=Alabed|first1=Samer|last2=Cabello|first2=Juan B|last3=Irving|first3=Greg J|last4=Qintar|first4=Mohammed|last5=Burls|first5=Amanda|title=Colchicine for pericarditis|journal=Cochrane Database of Systematic Reviews|year=2014|issn=14651858|doi=10.1002/14651858.CD010652.pub2}}</ref>'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki><nowiki/>'''1.''' [[Colchicine]] [[therapy]] of longer duration (>6 months) should be considered in some cases, according to [[clinical]] response. | |||
'''2.''' [[CRP]] [[dosage]] should be considered to guide the [[Therapy|treatment]] duration and assess the response to [[therapy]]. | |||
'''3.''' After [[C-reactive protein|CRP]] normalization, a gradual tapering of [[Therapy|therapies]] should be considered, tailored to [[symptoms]] and [[CRP]], stopping a single [[Class (biology)|class]] of [[drugs]] at a time. | |||
'''4.''' [[Drugs]] such as [[IVIG]], [[anakinra]], and [[azathioprine]] may be considered in cases of [[Corticosteroids|corticosteroid]]-dependent [[recurrent pericarditis]] in [[patients]] not responsive to [[Colchicine]]. | |||
'''5.''' [[Exercise]] [[restriction]] should be considered for non-[[athletes]] with [[recurrent pericarditis]] until [[Symptoms|symptom]] [[resolution]] and [[CRP]] normalization, taking into account the previous [[History and Physical examination|history]] and [[clinical]] conditions. | |||
'''6.''' [[Exercise]] [[restriction]] for a [[minimum]] of 3 months should be considered for [[athletes]] with [[recurrent pericarditis]] until [[Symptoms|symptom]] [[resolution]] and normalization of [[CRP]], [[The electrocardiogram|ECG]], and [[echocardiogram]]. | |||
'''7.''' If [[ischaemic heart disease]] is a concern or [[antiplatelet]] [[therapy]] is required, [[Aspirin]] should be considered, at medium-high [[doses]] (1–2.4 g/day). | |||
'''8.''' If [[symptoms]] recur during [[therapy]] tapering, the management should consider not increasing the [[dose]] of [[corticosteroids]] to control [[symptoms]], but increasing to the [[maximum]] [[dose]] of [[Aspirin]] or [[NSAIDs]], well distributed, generally every 8 hours, and [[intravenously]] if necessary, adding [[Colchicine]] and adding [[analgesics]] for [[pain]] control. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightCoral"|[[ESC guidelines classification scheme#Classification of Recommendations|Class III]] | |||
|- | |||
|bgcolor="LightCoral" |<nowiki></nowiki> [[Corticosteroid]] [[therapy]] is not recommended as a [[First-line therapy|first-line approach]].''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: B]])<nowiki/><ref name="Imazio2011">{{cite journal|last1=Imazio|first1=Massimo|title=Colchicine for Recurrent Pericarditis (CORP)|journal=Annals of Internal Medicine|volume=155|issue=7|year=2011|pages=409|issn=0003-4819|doi=10.7326/0003-4819-155-7-201110040-00359}}</ref><ref name="ImazioBelli2014">{{cite journal|last1=Imazio|first1=Massimo|last2=Belli|first2=Riccardo|last3=Brucato|first3=Antonio|last4=Cemin|first4=Roberto|last5=Ferrua|first5=Stefania|last6=Beqaraj|first6=Federico|last7=Demarie|first7=Daniela|last8=Ferro|first8=Silvia|last9=Forno|first9=Davide|last10=Maestroni|first10=Silvia|last11=Cumetti|first11=Davide|last12=Varbella|first12=Ferdinando|last13=Trinchero|first13=Rita|last14=Spodick|first14=David H|last15=Adler|first15=Yehuda|title=Efficacy and safety of colchicine for treatment of multiple recurrences of pericarditis (CORP-2): a multicentre, double-blind, placebo-controlled, randomised trial|journal=The Lancet|volume=383|issue=9936|year=2014|pages=2232–2237|issn=01406736|doi=10.1016/S0140-6736(13)62709-9}}</ref><ref name="ImazioBobbio2005">{{cite journal|last1=Imazio|first1=Massimo|last2=Bobbio|first2=Marco|last3=Cecchi|first3=Enrico|last4=Demarie|first4=Daniela|last5=Pomari|first5=Franco|last6=Moratti|first6=Mauro|last7=Ghisio|first7=Aldo|last8=Belli|first8=Riccardo|last9=Trinchero|first9=Rita|title=Colchicine as First-Choice Therapy for Recurrent Pericarditis|journal=Archives of Internal Medicine|volume=165|issue=17|year=2005|pages=1987|issn=0003-9926|doi=10.1001/archinte.165.17.1987}}</ref><ref name="LotrionteBiondi-Zoccai2010">{{cite journal|last1=Lotrionte|first1=Marzia|last2=Biondi-Zoccai|first2=Giuseppe|last3=Imazio|first3=Massimo|last4=Castagno|first4=Davide|last5=Moretti|first5=Claudio|last6=Abbate|first6=Antonio|last7=Agostoni|first7=Pierfrancesco|last8=Brucato|first8=Antonio L.|last9=Di Pasquale|first9=Pietro|last10=Raatikka|first10=Marja|last11=Sangiorgi|first11=Giuseppe|last12=Laudito|first12=Antonio|last13=Sheiban|first13=Imad|last14=Gaita|first14=Fiorenzo|title=International collaborative systematic review of controlled clinical trials on pharmacologic treatments for acute pericarditis and its recurrences|journal=American Heart Journal|volume=160|issue=4|year=2010|pages=662–670|issn=00028703|doi=10.1016/j.ahj.2010.06.015}}</ref><ref name="ImazioBrucato2008">{{cite journal|last1=Imazio|first1=Massimo|last2=Brucato|first2=Antonio|last3=Cumetti|first3=Davide|last4=Brambilla|first4=Giovanni|last5=Demichelis|first5=Brunella|last6=Ferro|first6=Silvia|last7=Maestroni|first7=Silvia|last8=Cecchi|first8=Enrico|last9=Belli|first9=Riccardo|last10=Palmieri|first10=Giancarlo|last11=Trinchero|first11=Rita|title=Corticosteroids for Recurrent Pericarditis|journal=Circulation|volume=118|issue=6|year=2008|pages=667–671|issn=0009-7322|doi=10.1161/CIRCULATIONAHA.107.761064}}</ref><ref name="ImazioBrucato2007">{{cite journal|last1=Imazio|first1=Massimo|last2=Brucato|first2=Antonio|last3=Adler|first3=Yehuda|last4=Brambilla|first4=Giovanni|last5=Artom|first5=Galit|last6=Cecchi|first6=Enrico|last7=Palmieri|first7=Giancarlo|last8=Trinchero|first8=Rita|title=Prognosis of Idiopathic Recurrent Pericarditis as Determined from Previously Published Reports|journal=The American Journal of Cardiology|volume=100|issue=6|year=2007|pages=1026–1028|issn=00029149|doi=10.1016/j.amjcard.2007.04.047}}</ref>'' | |||
|} | |||
===Recommendations for therapy of constrictive pericarditis=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ESC Guidelines Classification Scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki></nowiki>'''1.''' The mainstay of [[Therapy|treatment]] of [[Chronic (medical)|chronic]] permanent constriction is [[pericardiectomy]]. | |||
'''2.''' [[Medical]] [[therapy]] of specific [[pericarditis]] (i.e.[[tuberculous pericarditis]]) is recommended to [[Prevention|prevent]] the progression of constriction. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIb]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki>[[Empiric therapy|Empiric]] [[Anti inflammatory medications|anti-inflammatory therapy]] may be considered in cases with [[transient]] or [[new]] [[diagnosis]] of constriction with concomitant [[evidence]] of [[pericardial inflammation]] (i.e. [[CRP]] [[elevation]] or [[pericardial]] enhancement on [[Computed tomography|CT]]/[[Cardiovascular magnetic resonance imaging (CMR)|CMR]]). ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]]<nowiki/>)'' | |||
|} | |||
===Recommendations for the diagnosis and therapy of viral pericarditis=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki> For the definited [[diagnosis]] of [[viral pericarditis]], a comprehensive workup of [[histological]], [[cytological]], [[Immunohistochemistry|immunohistological]] and [[molecular]] investigations in [[pericardial fluid]] and peri-/[[epicardial]] [[biopsies]] should be considered. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]]<nowiki/>)'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightCoral"|[[ESC guidelines classification scheme#Classification of Recommendations|Class III]] | |||
|- | |||
|bgcolor="LightCoral" |<nowiki></nowiki> '''1.''' Routine [[viral]] [[serology]] is not recommended, with the possible exception of [[Human Immunodeficiency Virus (HIV)|HIV]] and [[Hepatitis C|HCV]]. | |||
'''2.''' [[Corticosteroid]] [[therapy]] is not recommended in [[viral pericarditis]]. (''[[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
===Recommendations for the therapy of purulent pericarditis=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ESC Guidelines Classification Scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki></nowiki>'''1.''' Effective [[pericardial drainage]] is recommended for [[purulent pericarditis]]. | |||
'''2.''' Administration of [[intravenous]] [[antibiotics]] is [[Indication (medicine)|indicated]] to [[Therapy|treat]] [[purulent pericarditis]].''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki>'''1.''' [[Subxiphoid]] pericardiotomy and rinsing of the [[pericardial cavity]] should be considered. | |||
'''2.''' [[Pericardial|Intrapericardial]] [[thrombolysis]] should be considered. | |||
'''3.''' [[Pericardiectomy]] for [[dense]] [[adhesions]], loculated or thick [[purulent]] [[Pericardial Effusion|effusion]], recurrence of [[tamponade]], persistent [[infection]] and progression to constriction should be considered. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
===Recommendations for the management of pericarditis in renal failure=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki>'''1.''' [[Dialysis]] should be considered in uraemic pericarditis. | |||
'''2.''' When [[patients]] with adequate [[dialysis]] develop [[pericarditis]], intensifying [[dialysis]] should be considered. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIb]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki>'''1.''' [[Pericardial]] [[aspiration]] and/or [[Drain (surgery)|drainage]] may be considered in non-responsive [[patients]] with [[dialysis]]. | |||
'''2.''' [[NSAIDs]] and [[corticosteroids]] ([[systemic]] or intrapericardial) may be considered when intensive [[dialysis]] is ineffective.''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightCoral"|[[ESC guidelines classification scheme#Classification of Recommendations|Class III]] | |||
|- | |||
|bgcolor="LightCoral" |<nowiki></nowiki> [[Colchicine]] is [[contraindicated]] in [[patients]] with [[pericarditis]] and severe [[renal impairment]]. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]]<nowiki/>)'' | |||
|} | |||
===Recommendations for the diagnosis and management of pericarditis associated with myocarditis=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ESC Guidelines Classification Scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki></nowiki>'''1.''' In cases of pericarditis with suspected associated [[myocarditis]], [[coronary angiography]] (according to [[clinical]] presentation and [[risk factor]] assessment) is recommended in order to rule out [[acute coronary syndromes]]. | |||
'''2.''' [[Cardiac magnetic resonance imaging|Cardiac magnetic resonance]] is recommended for the confirmation of [[myocardial]] involvement. | |||
'''3.''' [[Hospitalization]] is recommended for [[diagnosis]] and monitoring in [[patients]] with [[myocardial]] involvement. | |||
'''4.''' Rest and avoidance of [[physical activity]] beyond normal [[Sedentary living|sedentary activities]] is recommended in non-[[athletes]] and [[athletes]] with [[myopericarditis]] for a [[period]] of 6 months. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki> [[Empirical]] [[Anti inflammatory medications|anti-inflammatory therapies]] (lowest [[efficacious]] [[doses]]) should be considered to [[control]] [[Chest pain|chest pain.]] ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence:]]<nowiki/> [[ACC AHA Guidelines Classification Scheme#Level of Evidence|C]])'' | |||
|} | |||
===Recommendations for the prevention and management of radiation pericarditis=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ESC Guidelines Classification Scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki></nowiki>'''1.''' [[Radiation therapy]] methods that reduce both the [[volume]] and the [[dose]] of [[cardiac]] [[irradiation]] are recommended whenever | |||
possible.''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki>'''1.''' [[Pericardiectomy]] should be considered for [[radiation]]-induced [[constrictive pericarditis]], but with a worse [[outcome]] than when performed for [[constrictive pericarditis]] of other [[causes]], because of co-existing [[myopathy]]. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: B]]<nowiki/>)<ref name="BertogThambidorai2004">{{cite journal|last1=Bertog|first1=Stefan C.|last2=Thambidorai|first2=Senthil K.|last3=Parakh|first3=Kapil|last4=Schoenhagen|first4=Paul|last5=Ozduran|first5=Volkan|last6=Houghtaling|first6=Penny L.|last7=Lytle|first7=Bruce W.|last8=Blackstone|first8=Eugene H.|last9=Lauer|first9=Michael S.|last10=Klein|first10=Allan L.|title=Constrictive pericarditis: etiology and cause-specific survival after pericardiectomy|journal=Journal of the American College of Cardiology|volume=43|issue=8|year=2004|pages=1445–1452|issn=07351097|doi=10.1016/j.jacc.2003.11.048}}</ref><ref name="DeValeriaBaumgartner1991">{{cite journal|last1=DeValeria|first1=Patrick A.|last2=Baumgartner|first2=William A.|last3=Casale|first3=Alfred S.|last4=Greene|first4=Peter S.|last5=Cameron|first5=Duke E.|last6=Gardner|first6=Timothy J.|last7=Gott|first7=Vincent L.|last8=Watkins|first8=Levi|last9=Reitz|first9=Bruce A.|title=Current indications, risks, and outcome after pericardiectomy|journal=The Annals of Thoracic Surgery|volume=52|issue=2|year=1991|pages=219–224|issn=00034975|doi=10.1016/0003-4975(91)91339-W}}</ref><ref name="KomodaFrumkin2013">{{cite journal|last1=Komoda|first1=Takeshi|last2=Frumkin|first2=Alexander|last3=Knosalla|first3=Christoph|last4=Hetzer|first4=Roland|title=Child-Pugh Score Predicts Survival After Radical Pericardiectomy for Constrictive Pericarditis|journal=The Annals of Thoracic Surgery|volume=96|issue=5|year=2013|pages=1679–1685|issn=00034975|doi=10.1016/j.athoracsur.2013.06.016}}</ref><ref name="LingOh1999">{{cite journal|last1=Ling|first1=Lieng H.|last2=Oh|first2=Jae K.|last3=Schaff|first3=Hartzell V.|last4=Danielson|first4=Gordon K.|last5=Mahoney|first5=Douglas W.|last6=Seward|first6=James B.|last7=Tajik|first7=A. Jamil|title=Constrictive Pericarditis in the Modern Era|journal=Circulation|volume=100|issue=13|year=1999|pages=1380–1386|issn=0009-7322|doi=10.1161/01.CIR.100.13.1380}}</ref>'' | |||
|} | |||
===Recommendations for therapy of acute and recurrent pericarditis in children=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ESC Guidelines Classification Scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki></nowiki>'''1.''' [[NSAIDs]] at high [[doses]] are recommended as [[first-line therapy]] for [[acute pericarditis]] in [[children]] until complete [[symptom]] | |||
[[resolution]]. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki> [[Colchicine]] should be considered as an adjunct to [[Anti-inflammatory medication|anti-inflammatory therapy]] for [[acute]] [[recurrent pericarditis]] in [[children]]: | |||
<5 years, 0.5 mg/day; >5 years, 1.0–1.5 mg/day in two to three divided [[doses]].''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ESC guidelines classification scheme#Classification of Recommendations|Class IIb]] | |||
|- | |||
|bgcolor="LemonChiffon" |<nowiki></nowiki> [[IL-1|Anti-IL-1]] [[drugs]] may be considered in [[children]] with [[recurrent pericarditis]] and especially when they are [[corticosteroid]] | |||
dependent.''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightCoral"|[[ESC guidelines classification scheme#Classification of Recommendations|Class III]] | |||
|- | |||
|bgcolor="LightCoral" |<nowiki></nowiki> '''1.''' [[Aspirin]] is not recommended in [[children]] due to the associated risk of [[Reye's syndrome|Reye’s syndrome]] and [[hepatotoxicity]]. | |||
'''2.''' [[Corticosteroids]] are not recommended due to the severity of their [[side effects]] in growing [[children]] unless there are specific [[Indications and usage|indications]] such as [[Autoimmune diseases|autoimmune diseases.]]''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C]])'' | |||
''<nowiki/>'' | |||
|} | |} | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Medicine]] | |||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category: | [[Category:Up-To-Date]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Intensive care medicine]] | [[Category:Intensive care medicine]] | ||
Latest revision as of 23:39, 29 July 2020
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Pericarditis treatment On the Web |
|
American Roentgen Ray Society Images of Pericarditis treatment |
|
Risk calculators and risk factors for Pericarditis treatment |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2] Ahmed Zaghw, M.D. [3] Homa Najafi, M.D.[4]
Overview
The management of pericarditis depends on whether the patient has an uncomplicated vs. complicated disease course. Uncomplicated pericarditis is generally treated with non-steroidal anti-inflammatory drugs, such as Ibuprofen in cases of either viral or idiopathic pericarditis, and Aspirin in cases of post-MI pericarditis. Pericarditis complicated with either effusion or cardiac tamponade is generally treated with urgent pericardiocentesis in the case of cardiac tamponade, antibiotics in the case of purulent pericardial effusion, and either steroids or colchicine among patients with recurrent or refractory disease.
Management of Uncomplicated Pericarditis
Patients with uncomplicated acute pericarditis can generally be treated and followed up in an outpatient clinic. The treatment of viral or idiopathic pericarditis is with non-steroidal anti-inflammatory drugs. Patients should be observed for side effects since NSAIDs are known to affect the GI mucosa. If the underlying cause of pericarditis is something other than a viral cause, the specific etiology should be treated.
Non-steroidal Anti-inflammatory Drugs (NSAIDs)
- NSAIDs are the mainstay of therapy for uncomplicated pericarditis (viral or idiopathic pericarditis). The goal of therapy is to reduce pain and inflammation. While symptoms are improved by NSAIDs, the duration of the episode may not be reduced. The preferred NSAID is ibuprofen which has a large range of doses that can be titrated to the patient's tolerance. Depending on the severity of symptoms, the dosing is between 300-800 mg every 6-8 hours for days or weeks as needed. In order to minimize a recurrence of symptoms, a slow tapering of the NSAID dose may be required. As with all NSAID use, GI prophylaxis should be strongly recommended. Gastroprotection with misoprostol (600 to 800 g/day) or omeprazole (20 mg/day) is highly recommended. The gastroprotection recommendation is based on several studies have evaluated factors that place patients at increased risk of gastroduodenal toxicity from NSAIDs.[1][2][3]
- The American College of Gastroenterology identified the five most important risk factors for gastroduodenal toxicity:[4]
- Age 60 years (relative risk [RR] 5.52)
- History of an adverse gastroduodenal event (RR 4.76)
- High-dosage NSAIDs (more than twice normal; RR 10.1)
- Concurrent use of glucocorticoids (RR 4.4)
- Concurrent use of anticoagulants (RR 12.7).
Note: Patients with several risk factors are at the highest risk of NSAID-induced gastroduodenal toxicity.
Aspirin Therapy
An alternative therapy is aspirin 800 mg every 6-8 hours.[5]
Post-MI Pericarditis
In pericarditis following acute myocardial infarction, NSAIDs other than aspirin should be avoided since they can impair scar formation.
Failure to Respond to a Week of Traditional Therapy
Failure to respond to NSAIDs within one week (as indicated by persistence of fever, a worsening of symptoms such as chest pain, the development of a new pericardial effusion), likely indicates that the underlying cause may not be viral or idiopathic in nature. These patients may require re-evaluation, observation, and more aggressive therapy as described in the next section.
Colchicine
In the European guidelines, colchicine carries a class IIa recommendation for the treatment of an initial episode of pericarditis along with an NSAID. The dose is 0.6 mg bid for 3 months. It should be noted that a long term treatment of colchicine for several weeks or months should be considered, even after disappearance of effusion.[6] [7]
The rate of recurrence after an initial episode is lowered with colchicine therapy by approximately 50% - from 26% to 14% (see Forest plot).[8]
For example, in a multicenter, double-blind trial, the use of colchicine at a dose of 0.5 mg twice daily for 3 months for patients weighing >70 kg or 0.5 mg once daily for patients weighing ≤70 kg in acute pericarditis, when added to conventional antiinflammatory therapy with aspirin or ibuprofen, significantly reduced the rate of symptom persistence at 72 hours (19.2% vs. 40.0%, P=0.001), the number of recurrences per patient (0.21 vs. 0.52, P = 0.001), the hospitalization rate (5.0% vs. 14.2%, P = 0.02), and the remission rate at 1 week (85.0% vs. 58.3%, P<0.001), as compared with placebo.[9]
Steroids
Steroids are not used to treat an initial episode of pericarditis. They provide rapid relief in pain, but are associated with a high rate of recurrence.
Identification of High Risk or Complicated Pericarditis
Patients at high risk of developing complications of pericarditis may required admission to an inpatient service for careful observation for hemodynamic compromise. High risk patients include those with:[5]
- Acute onset
- High fever (> 100.4°F) and leukocytosis
- Development of cardiac tamponade
- Large pericardial effusion (echo-free space > 20 mm) resistant to NSAID treatment
- Immunocompromised status
- History of oral anticoagulation therapy
- Pericarditis secondary to acute trauma
- Failure to respond to seven days of NSAID treatment
Management of Complicated Pericarditis
- Pericardiocentesis may be required to relieve a large effusion or to treat cardiac tamponade.
- Antibiotics are required to manage an underlying bacterial infection or a purulent pericarditis.[10]
|
- † Immediate pericardial fluid removal for hemodynamic compromise
- ‡ Modify regimen and narrow coverage based on results of culture and susceptibility tests.
- Antifungals are required to manage an underlying fungal infection, (Histoplasmosis is the most common fungal cause pericarditis associated with histoplasmosis mediastinitis.[11]
|
- Steroids may be required in recurrent refractory cases or in patients with autoimmune disease.
- Colchicine may be required in patients with recurrent or refractory disease (see below).
- Surgery may be required in the presence of recurrent effusion or constrictive pericarditis.
Management of Cardiac Tamponade and Large Pericardial Effusion
Pericardiocentesis is an invasive procedure in which the pericardial fluid is drained through a needle. A pericardial window is a surgical procedure to drain fluid form the pericardium. Indications for a pericardiocentesis or a pericardial window include the following:[2]
- Cardiac tamponade
- Large, persistent, symptomatic pericardial effusion
- For diagnostic purposes, if there is suspected purulent, tuberculosis, or neoplastic pericarditis.
Management of Recurrent Pericarditis
- Colchicine can be used alone or in conjunction with NSAIDs in prevention and treatment of recurrent pericarditis. Treatment involves an NSAID plus colchicine 2 mg on first day followed by 1 mg daily for three months. A multicenter, double-blind, randomized trial, showed colchicine at a dose of 0.5 mg twice daily for 3 months for patients weighing >70 kg or 0.5 mg once daily for patients weighing ≤70 kg, in addition to conventional antiinflammatory therapy with aspirin or ibuprofen, reduced the number of recurrences per patient (0.21 vs. 0.52, P = 0.001), as compared with placebo.[9][12][13][14][15]
- Corticosteroids are usually used in those cases that are clearly refractory to NSAIDs and colchicine and a specific cause has not been found. Systemic corticosteroids are usually reserved for those with autoimmune disease. Steroids are sometimes used in post-operative pericarditis as well.
- Pericardiectomy can be performed if the patient is refractory to medical therapy as a last resort. Most patients will respond to 2 to 3 months of aggressive medical therapy.
Bacterial Pericarditis
Antimicrobial Therapy
1. Bacterial Pericarditis
-
- Preferred regimen: Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 28 days AND Ciprofloxacin 400 mg IV q12h for 28 days
- Alternative regimen (1): Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 28 days AND Cefepime 2 g IV q12h for 28 days
- Alternative regimen (2): Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 14–42 days AND Ceftriaxone 2 g IV q24h for 14–42 days
- Note: Pericardiocentesis must be promptly performed. Pericardial drainage combined with effective systemic antibiotic therapy is mandatory (antistaphylococcal agent plus aminoglycoside, followed by tailored antibiotic therapy according to cultures). Frequent irrigation of the pericardial cavity with urokinase or streptokinase may be considered. Open surgical drainage through subxiphoid pericardiotomy is preferable. Pericardiectomy may be required in patients with dense adhesions, loculated and thick purulent effusion, recurrence of tamponade, persistent infection, and progression to constriction.
-
- 1.2.1. Purulent pericarditis with contiguous pneumonia
- Preferred regimen: Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL AND (Ceftriaxone 1–2 g IV q12h OR Cefotaxime 2 g IV q6–8h) AND (Ciprofloxacin 400 mg IV q12h OR Levofloxacin 500–750 mg IV q24h)
- 1.2.2. Purulent pericarditis with contiguous head and neck infection
- Preferred regimen: Imipenem 500 mg IV q6–8h OR Ampicillin-Sulbactam 3 g IV q6h
- 1.2.3. Purulent pericarditis secondary to infective endocarditis
- Preferred regimen: Vancomycin 15–20 mg/kg IV q8–12h targeting trough levels of 15–20 μg/mL AND Gentamicin 3 mg/kg/day IV q8–12h
- 1.2.4. Purulent pericarditis after cardiac surgery, pediatric
- Preferred regimen: Vancomycin 15 mg/kg IV q6h targeting trough levels of 15–20 μg/mL AND (Ceftriaxone 100 mg/kg/day IV q12–24h OR Cefotaxime 200–300 mg/kg/day IV q6–8h) AND Gentamicin 6–7.5 mg/kg/day IV q8h
- 1.2.5. Purulent pericarditis with genitourinary infection, pediatric
- Preferred regimen: Vancomycin 15 mg/kg IV q6h targeting trough levels of 15–20 μg/mL AND (Ceftriaxone 100 mg/kg/day IV q12–24h OR Cefotaxime 200–300 mg/kg/day IV q6–8h) AND Gentamicin 6–7.5 mg/kg/day IV q8h
- 1.2.6. Purulent pericarditis in immunocompromised host, pediatric
- Preferred regimen: Vancomycin 15 mg/kg IV q6h targeting trough levels of 15–20 μg/mL AND (Ceftriaxone 100 mg/kg/day IV q12–24h OR Cefotaxime 200–300 mg/kg/day IV q6–8h) AND Gentamicin 6–7.5 mg/kg/day IV q8h
- 1.3. Pathogen-directed antimicrobial therapy[22]
- 1.3.1. Anaerobes
- Preferred regimen: Clindamycin 600–900 mg IV q8h for 14–42 days OR Metronidazole 7.5 mg/kg IV q6h for 14–42 days OR Ampicillin-Sulbactam 3 g IV q6h for 14–42 days
- 1.3.2. Gram-negative bacilli
- Preferred regimen: Ciprofloxacin 400 mg IV q12h for 14–42 days OR Levofloxacin 500–750 mg IV q24h for 14–42 days OR Cefepime 2 g IV q12h for 14–42 days
- 1.3.3. Legionella pneumophila
- Preferred regimen: Ciprofloxacin 400 mg IV q12h for 14–42 days OR Levofloxacin 500–750 mg IV q24h for 14–42 days OR Azithromycin 500 mg IV q24h for 14–42 days
- 1.3.4. Mycoplasma pneumoniae
- Preferred regimen: Doxycycline 100 mg IV q12h for 14–42 days OR Azithromycin 500 mg IV q24h for 14–42 days
- 1.3.5. Neisseria meningitidis
- Preferred regimen: Penicillin G 5–24 MU/day IM/IV q4–6h for 14–42 days OR Cefotaxime 2 g IV q6–8h for 14–42 days OR Ceftriaxone 2 g IV q24h for 14–42 days
- 1.3.6. Staphylococcus aureus, methicillin-susceptible
- Preferred regimen: Nafcillin 1–2 g IV q4h for 14–42 days OR Oxacillin 1–2 g IV q4h for 14–42 days OR Cefazolin 1–2 g IV q48h for 14–42 days OR Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 14–42 days OR Clindamycin 600–900 mg IV q8h for 14–42 days
- 1.3.7. Staphylococcus aureus, methicillin-resistant
- Preferred regimen: Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 14–42 days OR Linezolid 600 mg IV q12h for 14–42 days
- 1.3.8. Streptococcus pneumoniae, penicillin-susceptible
- Preferred regimen: Penicillin G 5–24 MU/day IM/IV q4–6h for 14–42 days OR Cefotaxime 2 g IV q6–8h for 14–42 days OR Ciprofloxacin 400 mg IV q12h for 14–42 days OR Levofloxacin 500–750 mg IV q24h for 14–42 days
- 1.3.9. Streptococcus pneumoniae, penicillin-resistant
- Preferred regimen: Ciprofloxacin 400 mg IV q12h for 14–42 days OR Levofloxacin 500–750 mg IV q24h for 14–42 days OR Vancomycin 1 g IV q12h targeting trough levels of 15–20 μg/mL for 14–42 days
2. Tuberculous Pericarditis[23].
- Preferred regimen: (Isoniazid 5 mg/kg (300 mg) PO qd AND Rifampicin 10 mg/kg (600 mg) PO qd AND Pyrazinamide 1,500 mg PO qd AND Ethambutol 1,200 mg PO qd for 2 months) THEN (Rifampicin 10 mg/kg (600 mg) PO qd AND Pyrazinamide 1,500 mg PO qd for 4 months) AND Prednisolone 1–2 mg/kg/day for 5–7 days with slow taper over 6–8 weeks[24].
- Pediatric doses: Isoniazid 10–15 mg/kg (300 mg); Rifampin 10–20 mg/kg (600 mg); Pyrazinamide 15–30 mg/kg (2.0 g); Ethambutol 15–20 mg/kg daily (1.0 g).
- Note: Intrapericardial drainage is done if needed. If constriction develops inspite of medical therapy, pericardiectomy is indicated.
3. Viral pericarditis[23]
- 3.1. CMV pericarditis
- Preferred regimen: Immunoglobulin 1 time per day 4 ml/kg on day 0, 4, and 8; 2 ml/kg on day 12 and 16.
- Note: Symptomatic treatment is given to the patients with viral pericarditis while in large effusions and cardiac tamponade pericardiocentesis is necessary. The use of corticosteroid therapy is contraindicated except in patients with secondary tuberculous pericarditis, as an adjunct to tuberculosis treatment. Drainage, if needed is done.
- 3.2. Coxsackie B pericarditis
- Preferred regimen: Interferon alpha or beta 2,5 Mio. IU/m2 surface area SC 3 times per week
- Note: Symptomatic treatment is given to the patients with viral pericarditis while in large effusions and cardiac tamponade pericardiocentesis is necessary. The use of corticosteroid therapy is contraindicated except in patients with secondary tuberculous pericarditis, as an adjunct to tuberculosis treatment. Drainage, if needed is done.
- 3.3. Adenovirus and parvovirus B19 perimyocarditis
- Preferred regimen: Immunoglobulin 10 g IV at day 1 and 3 for 6–8 hours
- Note: Symptomatic treatment is given to the patients with viral pericarditis while in large effusions and cardiac tamponade pericardiocentesis is necessary. The use of corticosteroid therapy is contraindicated except in patients with secondary tuberculous pericarditis, as an adjunct to tuberculosis treatment. Drainage, if needed is done.
4. Fungal Pericarditis[23]
- Empiric therapy : Fluconazole, Ketoconazole, Itraconazole, Amphotericin B, Liposomal amphotericin B or Amphotericin B lipid complex is indicated.
- 4.1. Histoplasmosis
- Preferred regimen: Nonsteroidal anti-inflammatory drugs given during 2–12 weeks.
- Note: Corticosteroids and NSAIDs can support the treatment with antifungal drugs. Pericardiocentesis or surgical treatment is indicated for haemodynamic impairment. Pericardiectomy is indicated in fungal constrictive pericarditis.
- 4.2. Nocardiosis
- Preferred regimen: Sulfonamides are the drugs of choice.
- Note: Corticosteroids and NSAIDs can support the treatment with antifungal drugs. Pericardiocentesis or surgical treatment is indicated for haemodynamic impairment. Pericardiectomy is indicated in fungal constrictive pericarditis.
- 4.3. Actinomycosis
- Preferred regimen: Combination of three antibiotics including Penicillin.
- Note: Corticosteroids and NSAIDs can support the treatment with antifungal drugs. Pericardiocentesis or surgical treatment is indicated for haemodynamic impairment. Pericardiectomy is indicated in fungal constrictive pericarditis.
2006 ACC/AHA/ESC Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death (DO NOT EDIT)[25]
Pericardial Diseases (DO NOT EDIT)[25]
| Class I |
| "1. Ventricular arrhythmias that develop in patients with pericardial disease should be treated in the same manner that such arrhythmias are treated in patients with other diseases including ICD and pacemaker implantation as required. Patients receiving ICD implantation should be receiving chronic optimal medical therapy and have reasonable expectation of survival with a good functional status for more than 1 year. (Level of Evidence: C)" |
2015 ESC Guidelines on the Diagnosis and Treatment of Pericarditis (DO NOT EDIT)[26]
Recommendations for the management of acute pericarditis
| Class I |
| 1. Hospital admission is recommended for high-risk patients with acute pericarditis (at least one risk factor).
2. Outpatient management is recommended for low-risk patients with acute pericarditis. 3. Evaluation of response to anti-inflammatory therapy is recommended after 1 week. (Level of Evidence: B)[27][28]
|
Recommendations for the treatment of acute pericarditis
| Class I |
| 1. Aspirin or NSAIDs are recommended as first-line therapy for acute pericarditis with gastroprotection.[29]
2. Colchicine is recommended as first-line therapy for acute pericarditis as an adjunct to aspirin/NSAID therapy. (Level of Evidence: A)[30][31][32][33]
|
| Class IIa |
| 1. Serum CRP should be considered to guide the treatment length and assess the response to therapy.
2. Low-dose corticosteroids should be considered for acute pericarditis in cases of contraindication/failure of aspirin/NSAIDs and colchicine, and when an infectious cause has been excluded, or when there is a specific indication such as autoimmune disease. 3. Exercise restriction should be considered for non-athletes with acute pericarditis until resolution of symptoms and normalization of CRP, ECG, and echocardiogram. 4. For athletes, the duration of exercise restriction should be considered until resolution of symptoms and normalization of CRP, ECG, and echocardiogram—at least 3 months is recommended. (Level of Evidence: C)
|
| Class III |
| Corticosteroids are not recommended as first-line therapy for acute pericarditis. (Level of Evidence: C) |
Recommendations for the management of recurrent pericarditis
| Class I |
| 1. Aspirin and NSAIDs are mainstays of treatment and are recommended at full doses, if tolerated, until complete symptom resolution.[29][32]
2. Colchicine (0.5 mg twice daily or 0.5 mg daily for patients, 70 kg or intolerant to higher doses); use for 6 months is recommended as an adjunct to aspirin/NSAIDs.(Level of Evidence: A)[34][35][30][32][33]
|
| Class IIa |
| 1. Colchicine therapy of longer duration (>6 months) should be considered in some cases, according to clinical response.
2. CRP dosage should be considered to guide the treatment duration and assess the response to therapy. 3. After CRP normalization, a gradual tapering of therapies should be considered, tailored to symptoms and CRP, stopping a single class of drugs at a time. 4. Drugs such as IVIG, anakinra, and azathioprine may be considered in cases of corticosteroid-dependent recurrent pericarditis in patients not responsive to Colchicine. 5. Exercise restriction should be considered for non-athletes with recurrent pericarditis until symptom resolution and CRP normalization, taking into account the previous history and clinical conditions. 6. Exercise restriction for a minimum of 3 months should be considered for athletes with recurrent pericarditis until symptom resolution and normalization of CRP, ECG, and echocardiogram. 7. If ischaemic heart disease is a concern or antiplatelet therapy is required, Aspirin should be considered, at medium-high doses (1–2.4 g/day). 8. If symptoms recur during therapy tapering, the management should consider not increasing the dose of corticosteroids to control symptoms, but increasing to the maximum dose of Aspirin or NSAIDs, well distributed, generally every 8 hours, and intravenously if necessary, adding Colchicine and adding analgesics for pain control. (Level of Evidence: C)
|
| Class III |
| Corticosteroid therapy is not recommended as a first-line approach.(Level of Evidence: B)[34][35][30][29][36][37] |
Recommendations for therapy of constrictive pericarditis
| Class I |
| 1. The mainstay of treatment of chronic permanent constriction is pericardiectomy.
2. Medical therapy of specific pericarditis (i.e.tuberculous pericarditis) is recommended to prevent the progression of constriction. (Level of Evidence: C)
|
| Class IIb |
| Empiric anti-inflammatory therapy may be considered in cases with transient or new diagnosis of constriction with concomitant evidence of pericardial inflammation (i.e. CRP elevation or pericardial enhancement on CT/CMR). (Level of Evidence: C) |
Recommendations for the diagnosis and therapy of viral pericarditis
| Class IIa |
| For the definited diagnosis of viral pericarditis, a comprehensive workup of histological, cytological, immunohistological and molecular investigations in pericardial fluid and peri-/epicardial biopsies should be considered. (Level of Evidence: C) |
| Class III |
| 1. Routine viral serology is not recommended, with the possible exception of HIV and HCV.
2. Corticosteroid therapy is not recommended in viral pericarditis. (Level of Evidence: C)
|
Recommendations for the therapy of purulent pericarditis
| Class I |
| 1. Effective pericardial drainage is recommended for purulent pericarditis.
2. Administration of intravenous antibiotics is indicated to treat purulent pericarditis.(Level of Evidence: C) |
| Class IIa |
| 1. Subxiphoid pericardiotomy and rinsing of the pericardial cavity should be considered.
2. Intrapericardial thrombolysis should be considered. 3. Pericardiectomy for dense adhesions, loculated or thick purulent effusion, recurrence of tamponade, persistent infection and progression to constriction should be considered. (Level of Evidence: C)
|
Recommendations for the management of pericarditis in renal failure
| Class IIa |
| 1. Dialysis should be considered in uraemic pericarditis.
2. When patients with adequate dialysis develop pericarditis, intensifying dialysis should be considered. (Level of Evidence: C)
|
| Class IIb |
| 1. Pericardial aspiration and/or drainage may be considered in non-responsive patients with dialysis.
2. NSAIDs and corticosteroids (systemic or intrapericardial) may be considered when intensive dialysis is ineffective.(Level of Evidence: C)
|
| Class III |
| Colchicine is contraindicated in patients with pericarditis and severe renal impairment. (Level of Evidence: C) |
Recommendations for the diagnosis and management of pericarditis associated with myocarditis
| Class I |
| 1. In cases of pericarditis with suspected associated myocarditis, coronary angiography (according to clinical presentation and risk factor assessment) is recommended in order to rule out acute coronary syndromes.
2. Cardiac magnetic resonance is recommended for the confirmation of myocardial involvement. 3. Hospitalization is recommended for diagnosis and monitoring in patients with myocardial involvement. 4. Rest and avoidance of physical activity beyond normal sedentary activities is recommended in non-athletes and athletes with myopericarditis for a period of 6 months. (Level of Evidence: C)
|
| Class IIa |
| Empirical anti-inflammatory therapies (lowest efficacious doses) should be considered to control chest pain. (Level of Evidence: C) |
Recommendations for the prevention and management of radiation pericarditis
| Class I |
| 1. Radiation therapy methods that reduce both the volume and the dose of cardiac irradiation are recommended whenever
possible.(Level of Evidence: C)
|
| Class IIa |
| 1. Pericardiectomy should be considered for radiation-induced constrictive pericarditis, but with a worse outcome than when performed for constrictive pericarditis of other causes, because of co-existing myopathy. (Level of Evidence: B)[38][39][40][41] |
Recommendations for therapy of acute and recurrent pericarditis in children
| Class I |
| 1. NSAIDs at high doses are recommended as first-line therapy for acute pericarditis in children until complete symptom
resolution. (Level of Evidence: C)
|
| Class IIa |
| Colchicine should be considered as an adjunct to anti-inflammatory therapy for acute recurrent pericarditis in children:
<5 years, 0.5 mg/day; >5 years, 1.0–1.5 mg/day in two to three divided doses.(Level of Evidence: C)
|
| Class IIb |
| Anti-IL-1 drugs may be considered in children with recurrent pericarditis and especially when they are corticosteroid
dependent.(Level of Evidence: C)
|
| Class III |
| 1. Aspirin is not recommended in children due to the associated risk of Reye’s syndrome and hepatotoxicity.
2. Corticosteroids are not recommended due to the severity of their side effects in growing children unless there are specific indications such as autoimmune diseases.(Level of Evidence: C)
|
References
- ↑ Gabriel, SE.; Jaakkimainen, L.; Bombardier, C. (1991). "Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. A meta-analysis". Ann Intern Med. 115 (10): 787–96. PMID 1834002. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmuller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH (2004). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology". Eur Heart J. 25 (7): 587–10. doi:10.1016/j.ehj.2004.02.002. PMID 15120056.
- ↑ Imazio, M.; Demichelis, B.; Parrini, I.; Giuggia, M.; Cecchi, E.; Gaschino, G.; Demarie, D.; Ghisio, A.; Trinchero, R. (2004). "Day-hospital treatment of acute pericarditis: a management program for outpatient therapy". J Am Coll Cardiol. 43 (6): 1042–6. doi:10.1016/j.jacc.2003.09.055. PMID 15028364. Unknown parameter
|month=ignored (help) - ↑ Lanza, FL. (1998). "A guideline for the treatment and prevention of NSAID-induced ulcers. Members of the Ad Hoc Committee on Practice Parameters of the American College of Gastroenterology". Am J Gastroenterol. 93 (11): 2037–46. doi:10.1111/j.1572-0241.1998.00588.x. PMID 9820370. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 Imazio M, Demichelis B, Parrini I, Giuggia M, Cecchi E, Gaschino G, Demarie D, Ghisio A, Trinchero R (2004). "Day-hospital treatment of acute pericarditis: a management program for outpatient therapy". J Am Coll Cardiol. 43 (6): 1042–6. doi:10.1016/j.jacc.2003.09.055. PMID 15028364.
- ↑ Imazio, M.; Brucato, A.; Forno, D.; Ferro, S.; Belli, R.; Trinchero, R.; Adler, Y. (2012). "Efficacy and safety of colchicine for pericarditis prevention. Systematic review and meta-analysis". Heart. 98 (14): 1078–82. doi:10.1136/heartjnl-2011-301306. PMID 22442198. Unknown parameter
|month=ignored (help) - ↑ Imazio, M.; Bobbio, M.; Cecchi, E.; Demarie, D.; Demichelis, B.; Pomari, F.; Moratti, M.; Gaschino, G.; Giammaria, M. (2005). "Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial". Circulation. 112 (13): 2012–6. doi:10.1161/CIRCULATIONAHA.105.542738. PMID 16186437. Unknown parameter
|month=ignored (help) - ↑ Colchicine for pericarditis: a living systematic review. GitHub. Available at http://openmetaanalysis.github.io/Colchicine-for-Pericarditis/. Accessed November 16, 2014.
- ↑ 9.0 9.1 Imazio, M.; Brucato, A.; Cemin, R.; Ferrua, S.; Maggiolini, S.; Beqaraj, F.; Demarie, D.; Forno, D.; Ferro, S. (2013). "A Randomized Trial of Colchicine for Acute Pericarditis". N Engl J Med. doi:10.1056/NEJMoa1208536. PMID 23992557. Unknown parameter
|month=ignored (help) - ↑ Parikh, SV.; Memon, N.; Echols, M.; Shah, J.; McGuire, DK.; Keeley, EC. (2009). "Purulent pericarditis: report of 2 cases and review of the literature". Medicine (Baltimore). 88 (1): 52–65. doi:10.1097/MD.0b013e318194432b. PMID 19352300. Unknown parameter
|month=ignored (help) - ↑ Wheat, LJ.; Freifeld, AG.; Kleiman, MB.; Baddley, JW.; McKinsey, DS.; Loyd, JE.; Kauffman, CA. (2007). "Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America". Clin Infect Dis. 45 (7): 807–25. doi:10.1086/521259. PMID 17806045. Unknown parameter
|month=ignored (help) - ↑ Adler Y, Zandman-Goddard G, Ravid M, Avidan B, Zemer D, Ehrenfeld M, Shemesh J, Tomer Y, Shoenfeld Y (1994). "Usefulness of colchicine in preventing recurrences of pericarditis". Am J of Cardiol. 73 (12): 916–7. doi:10.1016/0002-9149(94)90828-1. PMID 8184826.
- ↑ Imazio M, Bobbio M, Cecchi E, Demarie D, Demichelis B, Pomari F, Moratti M, Gaschino G, Giammaria M, Ghisio A, Belli R, Trinchero R (2005). "Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial". Circulation. 112 (13): 2012–6. doi:10.1161/CIRCULATIONAHA.105.542738. PMID 16186437.
- ↑ Imazio M, Bobbio M, Cecchi E, Demarie D, Pomari F, Moratti M, Ghisio A, Belli R, Trinchero R (2005). "Colchicine as first-choice therapy for recurrent pericarditis: results of the CORE (COlchicine for REcurrent pericarditis) trial". Arch Intern Med. 165 (17): 1987–91. doi:10.1001/archinte.165.17.1987. PMID 16186468.
- ↑ Little, William C.; Freeman, Gregory L. (2006). "Pericardial Disease". Circulation. 113 (12): 1622–1632. doi:10.1161/CIRCULATIONAHA.105.561514. ISSN 0009-7322.
- ↑ Gilbert, David (2015). The Sanford guide to antimicrobial therapy. Sperryville, Va: Antimicrobial Therapy. ISBN 978-1930808843.
- ↑ Bartlett, John (2012). Johns Hopkins ABX guide : diagnosis and treatment of infectious diseases. Burlington, MA: Jones and Bartlett Learning. ISBN 978-1449625580.
- ↑ Maisch, Bernhard; Seferović, Petar M.; Ristić, Arsen D.; Erbel, Raimund; Rienmüller, Reiner; Adler, Yehuda; Tomkowski, Witold Z.; Thiene, Gaetano; Yacoub, Magdi H.; Task Force on the Diagnosis and Management of Pricardial Diseases of the European Society of Cardiology (2004-04). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology". European Heart Journal. 25 (7): 587–610. doi:10.1016/j.ehj.2004.02.002. ISSN 0195-668X. PMID 15120056. Check date values in:
|date=(help) - ↑ Pankuweit, Sabine; Ristić, Arsen D.; Seferović, Petar M.; Maisch, Bernhard (2005). "Bacterial pericarditis: diagnosis and management". American Journal of Cardiovascular Drugs: Drugs, Devices, and Other Interventions. 5 (2): 103–112. ISSN 1175-3277. PMID 15725041.
- ↑ Goodman, null (2000-08). "Purulent Pericarditis". Current Treatment Options in Cardiovascular Medicine. 2 (4): 343–350. ISSN 1092-8464. PMID 11096539. Check date values in:
|date=(help) - ↑ Cherry, James (2014). Feigin and Cherry's textbook of pediatric infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455711772.
- ↑ Bartlett, John (2012). Johns Hopkins ABX guide : diagnosis and treatment of infectious diseases. Burlington, MA: Jones and Bartlett Learning. ISBN 978-1449625580.
- ↑ 23.0 23.1 23.2 Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y; et al. (2004). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology". Eur Heart J. 25 (7): 587–610. doi:10.1016/j.ehj.2004.02.002. PMID 15120056.
- ↑ Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN; et al. (2003). "American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis". Am J Respir Crit Care Med. 167 (4): 603–62. doi:10.1164/rccm.167.4.603. PMID 12588714.
- ↑ 25.0 25.1 Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M; et al. (2006). "ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation. 114 (10): e385–484. doi:10.1161/CIRCULATIONAHA.106.178233. PMID 16935995.
- ↑ Adler, Yehuda; Charron, Philippe; Imazio, Massimo; Badano, Luigi; Barón-Esquivias, Gonzalo; Bogaert, Jan; Brucato, Antonio; Gueret, Pascal; Klingel, Karin; Lionis, Christos; Maisch, Bernhard; Mayosi, Bongani; Pavie, Alain; Ristić, Arsen D.; Sabaté Tenas, Manel; Seferovic, Petar; Swedberg, Karl; Tomkowski, Witold (2015). "2015 ESC Guidelines for the diagnosis and management of pericardial diseases". European Heart Journal. 36 (42): 2921–2964. doi:10.1093/eurheartj/ehv318. ISSN 0195-668X.
- ↑ Imazio, Massimo; Demichelis, Brunella; Parrini, Iris; Giuggia, Marco; Cecchi, Enrico; Gaschino, Gianni; Demarie, Daniela; Ghisio, Aldo; Trinchero, Rita (2004). "Day-hospital treatment of acute pericarditis". Journal of the American College of Cardiology. 43 (6): 1042–1046. doi:10.1016/j.jacc.2003.09.055. ISSN 0735-1097.
- ↑ Imazio, Massimo; Cecchi, Enrico; Demichelis, Brunella; Ierna, Salvatore; Demarie, Daniela; Ghisio, Aldo; Pomari, Franco; Coda, Luisella; Belli, Riccardo; Trinchero, Rita (2007). "Indicators of Poor Prognosis of Acute Pericarditis". Circulation. 115 (21): 2739–2744. doi:10.1161/CIRCULATIONAHA.106.662114. ISSN 0009-7322.
- ↑ 29.0 29.1 29.2 Lotrionte, Marzia; Biondi-Zoccai, Giuseppe; Imazio, Massimo; Castagno, Davide; Moretti, Claudio; Abbate, Antonio; Agostoni, Pierfrancesco; Brucato, Antonio L.; Di Pasquale, Pietro; Raatikka, Marja; Sangiorgi, Giuseppe; Laudito, Antonio; Sheiban, Imad; Gaita, Fiorenzo (2010). "International collaborative systematic review of controlled clinical trials on pharmacologic treatments for acute pericarditis and its recurrences". American Heart Journal. 160 (4): 662–670. doi:10.1016/j.ahj.2010.06.015. ISSN 0002-8703.
- ↑ 30.0 30.1 30.2 Imazio, Massimo; Bobbio, Marco; Cecchi, Enrico; Demarie, Daniela; Demichelis, Brunella; Pomari, Franco; Moratti, Mauro; Gaschino, Gianni; Giammaria, Massimo; Ghisio, Aldo; Belli, Riccardo; Trinchero, Rita (2005). "Colchicine in Addition to Conventional Therapy for Acute Pericarditis". Circulation. 112 (13): 2012–2016. doi:10.1161/CIRCULATIONAHA.105.542738. ISSN 0009-7322.
- ↑ Imazio, Massimo; Brucato, Antonio; Cemin, Roberto; Ferrua, Stefania; Maggiolini, Stefano; Beqaraj, Federico; Demarie, Daniela; Forno, Davide; Ferro, Silvia; Maestroni, Silvia; Belli, Riccardo; Trinchero, Rita; Spodick, David H.; Adler, Yehuda (2013). "A Randomized Trial of Colchicine for Acute Pericarditis". New England Journal of Medicine. 369 (16): 1522–1528. doi:10.1056/NEJMoa1208536. ISSN 0028-4793.
- ↑ 32.0 32.1 32.2 Imazio, Massimo; Brucato, Antonio; Belli, Riccardo; Forno, Davide; Ferro, Silvia; Trinchero, Rita; Adler, Yehuda (2014). "Colchicine for the prevention of pericarditis". Journal of Cardiovascular Medicine. 15 (12): 840–846. doi:10.2459/JCM.0000000000000103. ISSN 1558-2027.
- ↑ 33.0 33.1 Alabed, Samer; Cabello, Juan B; Irving, Greg J; Qintar, Mohammed; Burls, Amanda (2014). "Colchicine for pericarditis". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD010652.pub2. ISSN 1465-1858.
- ↑ 34.0 34.1 Imazio, Massimo (2011). "Colchicine for Recurrent Pericarditis (CORP)". Annals of Internal Medicine. 155 (7): 409. doi:10.7326/0003-4819-155-7-201110040-00359. ISSN 0003-4819.
- ↑ 35.0 35.1 Imazio, Massimo; Belli, Riccardo; Brucato, Antonio; Cemin, Roberto; Ferrua, Stefania; Beqaraj, Federico; Demarie, Daniela; Ferro, Silvia; Forno, Davide; Maestroni, Silvia; Cumetti, Davide; Varbella, Ferdinando; Trinchero, Rita; Spodick, David H; Adler, Yehuda (2014). "Efficacy and safety of colchicine for treatment of multiple recurrences of pericarditis (CORP-2): a multicentre, double-blind, placebo-controlled, randomised trial". The Lancet. 383 (9936): 2232–2237. doi:10.1016/S0140-6736(13)62709-9. ISSN 0140-6736.
- ↑ Imazio, Massimo; Brucato, Antonio; Cumetti, Davide; Brambilla, Giovanni; Demichelis, Brunella; Ferro, Silvia; Maestroni, Silvia; Cecchi, Enrico; Belli, Riccardo; Palmieri, Giancarlo; Trinchero, Rita (2008). "Corticosteroids for Recurrent Pericarditis". Circulation. 118 (6): 667–671. doi:10.1161/CIRCULATIONAHA.107.761064. ISSN 0009-7322.
- ↑ Imazio, Massimo; Brucato, Antonio; Adler, Yehuda; Brambilla, Giovanni; Artom, Galit; Cecchi, Enrico; Palmieri, Giancarlo; Trinchero, Rita (2007). "Prognosis of Idiopathic Recurrent Pericarditis as Determined from Previously Published Reports". The American Journal of Cardiology. 100 (6): 1026–1028. doi:10.1016/j.amjcard.2007.04.047. ISSN 0002-9149.
- ↑ Bertog, Stefan C.; Thambidorai, Senthil K.; Parakh, Kapil; Schoenhagen, Paul; Ozduran, Volkan; Houghtaling, Penny L.; Lytle, Bruce W.; Blackstone, Eugene H.; Lauer, Michael S.; Klein, Allan L. (2004). "Constrictive pericarditis: etiology and cause-specific survival after pericardiectomy". Journal of the American College of Cardiology. 43 (8): 1445–1452. doi:10.1016/j.jacc.2003.11.048. ISSN 0735-1097.
- ↑ DeValeria, Patrick A.; Baumgartner, William A.; Casale, Alfred S.; Greene, Peter S.; Cameron, Duke E.; Gardner, Timothy J.; Gott, Vincent L.; Watkins, Levi; Reitz, Bruce A. (1991). "Current indications, risks, and outcome after pericardiectomy". The Annals of Thoracic Surgery. 52 (2): 219–224. doi:10.1016/0003-4975(91)91339-W. ISSN 0003-4975.
- ↑ Komoda, Takeshi; Frumkin, Alexander; Knosalla, Christoph; Hetzer, Roland (2013). "Child-Pugh Score Predicts Survival After Radical Pericardiectomy for Constrictive Pericarditis". The Annals of Thoracic Surgery. 96 (5): 1679–1685. doi:10.1016/j.athoracsur.2013.06.016. ISSN 0003-4975.
- ↑ Ling, Lieng H.; Oh, Jae K.; Schaff, Hartzell V.; Danielson, Gordon K.; Mahoney, Douglas W.; Seward, James B.; Tajik, A. Jamil (1999). "Constrictive Pericarditis in the Modern Era". Circulation. 100 (13): 1380–1386. doi:10.1161/01.CIR.100.13.1380. ISSN 0009-7322.