Diabetic foot pathophysiology: Difference between revisions
| (40 intermediate revisions by 3 users not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
[[Diabetic foot]] is an umbrella term for [[foot]] problems in [[patients]] with [[diabetes mellitus]]. [[Neuropathy]], [[ischemia]] and [[trauma]] are three main [[pathogenesis]] of [[diabetic foot]]. [[Neuropathy]] is the most common and is responsible in more than 60% of [[diabetic foot]] cases. Factors such as high [[Blood sugar|blood glucose]], [[reactive oxygen species]], insufficient [[oxygenation]] of the [[nerves]] and [[inflammation]] leads to [[neuropathy]] development | [[Diabetic foot]] is an umbrella term for [[foot]] problems in [[patients]] with [[diabetes mellitus]]. [[Neuropathy]], [[ischemia]] and [[trauma]] are three main [[pathogenesis]] of [[diabetic foot]]. [[Neuropathy]] is the most common and is the responsible element in more than 60% of [[diabetic foot]] cases. Factors such as high [[Blood sugar|blood glucose]], [[reactive oxygen species]], insufficient [[oxygenation]] of the [[nerves]], and [[inflammation]] leads to [[neuropathy]] development in [[diabetes|diabetic]] [[patient|patients]] and it gets worse with [[alcohol]] use and [[smoking]]. [[Neuropathy]] can involve [[nerve|motor]], [[Autonomic nervous system|autonomic]], or [[Sensory system|sensory]] [[nerve|nerves]] and is able to involve both large and small fibers. [[nerve|Motor nerve]] involvement can lead to some mechanical changes in the [[foot]] of a [[diabetes|diabetic]] [[patient]], which causes more [[Anatomical terms of location|plantar]] pressure and higher risk of [[callus]] formation. Each and every factor leads to a higher rate of [[skin]] breakdown and [[ulcer|ulceration]]. [[Autonomic nervous system|Autonomic]] [[neuropathy]] leads to [[anhidrosis]] and impaired function of oil [[glands]], subsequent [[skin]] [[Xeroderma|dryness]], higher chance of [[skin]] breakdown, and [[ulcer]] formation. [[Diabetes|Diabetic]] [[patients]] with [[sensory system|sensory]] [[neuropathy]] are more prone to [[ulcer]] formation and related [[Complication (medicine)|complications]], since they don't feel [[pain]] with ever-deepening [[ulcers]]. [[Ischemia]] is the second best known [[pathogenesis]] of [[diabetic foot]] that could occur due to a higher rate of [[Limb (anatomy)|lower limb]] [[atherosclerosis]] in [[diabetes|diabetic]] [[patients]], compared to the normal population. [[Diabetes]] related [[Complication (medicine)|complications]] such as [[Microvascular disease|micro]] and [[Macrovascular disease|macrovascular]] [[Complication (medicine)|complications]] further intensify [[ischemia]]. [[Ischemia|Ischemic]] changes can be discovered by an impaired [[ABI|ankle brachial index]] ([[ABI]]). [[Physical trauma|Trauma]] to the [[foot]] usually acts as a trigger for [[diabetic foot]]. A defective hypoxic response has been explained in [[diabetic foot]], which is related to a [[transcription factor]] named [[HIF1A|hypoxia‐inducible factor‐1]] ([[HIF1A|HIF‐1]]). Lower levels of [[HIF1A|HIF‐1]] in [[biopsy|biopsies]] of [[diabetic foot]] could be related to its role in [[wound healing]]. Some genetic associations (such as [[MAPK14]] gene located on [[chromosome 6]], decreased expression of certain [[cytokines]] and [[growth factors]], and the HSPA1B genotype) have been explained in [[diabetic foot]] development. [[Charcot joint|Charcot arthropathy]], some [[Psychiatry|psychosocial conditions]], [[necrotizing fasciitis]] ([[necrotizing fasciitis|NF]]), [[vitamin D deficiency]], [[Athlete's foot|tinea pedis]], [[onychomycosis]], and [[diabetic retinopathy]] are associated conditions in [[diabetic foot]]. On [[gross pathology]], the most common site of [[ulcer|ulceration]] is on the [[Sole (foot)|soles of the feet]], under the [[Metatarsus|metatarsal head]] with various depths and possible [[anatomy|anatomical]] deformities of the [[foot]]. In microscopic evaluations of the [[ulcers]], evidence of [[necrosis]], [[hyperkeratosis]], [[fibrosis]], [[inflammation]], [[cell|cellular]] debris, [[granulation tissue]], and [[angiogenesis]] have been found. | ||
== Pathophysiology== | ==Pathophysiology== | ||
*[[Diabetic foot]] is an umbrella term for [[foot]] problems in [[patients]] with [[diabetes mellitus]]. There are numerous responsible [[pathogenesis]], such as [[artery|arterial]] abnormalities, [[diabetic neuropathy]], delayed [[wound healing]] and being more vulnerable to [[infection]] or [[gangrene]] of the [[foot]]. The key components of [[diabetic foot]] are [[neuropathy]], [[ischemia]] and [[trauma]]. <ref name="pmid12039404">{{cite journal| author=Assal JP, Mehnert H, Tritschler HJ, Sidorenko A, Keen H, Hellmut Mehnert Award Workshop Participants| title=On your feet! Workshop on the diabetic foot. | journal=J Diabetes Complications | year= 2002 | volume= 16 | issue= 2 | pages= 183-94 | pmid=12039404 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12039404 }} </ref> | |||
*Only 10% of [[diabetic foot]] | *[[Diabetic foot]] is an umbrella term for [[foot]] problems in [[patients]] with [[diabetes mellitus]]. There are numerous responsible [[pathogenesis]], such as [[artery|arterial]] abnormalities, [[diabetic neuropathy]], delayed [[wound healing]], and being more vulnerable to [[infection]] or [[gangrene]] of the [[foot]]. The key components of [[diabetic foot]] are [[neuropathy]], [[ischemia]], and [[trauma]]. <ref name="pmid12039404">{{cite journal| author=Assal JP, Mehnert H, Tritschler HJ, Sidorenko A, Keen H, Hellmut Mehnert Award Workshop Participants| title=On your feet! Workshop on the diabetic foot. | journal=J Diabetes Complications | year= 2002 | volume= 16 | issue= 2 | pages= 183-94 | pmid=12039404 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12039404 }} </ref> | ||
*Only 10% of [[diabetic foot]] cases are exclusively due to [[ischemia]], nevertheless, 90% of them are related to [[neuropathy]] (alone or in combination to [[ischemia]]).<ref name="pmid25685277">{{cite journal| author=Yazdanpanah L, Nasiri M, Adarvishi S| title=Literature review on the management of diabetic foot ulcer. | journal=World J Diabetes | year= 2015 | volume= 6 | issue= 1 | pages= 37-53 | pmid=25685277 | doi=10.4239/wjd.v6.i1.37 | pmc=4317316 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25685277 }} </ref> | |||
*Components such as [[neuropathy]] and [[peripheral arterial disease]] can mask [[Medical sign|signs]] and [[symptoms]] of the local [[infection]].<ref name="LepäntaloApelqvist2011">{{cite journal|last1=Lepäntalo|first1=M.|last2=Apelqvist|first2=J.|last3=Setacci|first3=C.|last4=Ricco|first4=J.-B.|last5=de Donato|first5=G.|last6=Becker|first6=F.|last7=Robert-Ebadi|first7=H.|last8=Cao|first8=P.|last9=Eckstein|first9=H.H.|last10=De Rango|first10=P.|last11=Diehm|first11=N.|last12=Schmidli|first12=J.|last13=Teraa|first13=M.|last14=Moll|first14=F.L.|last15=Dick|first15=F.|last16=Davies|first16=A.H.|title=Chapter V: Diabetic Foot|journal=European Journal of Vascular and Endovascular Surgery|volume=42|year=2011|pages=S60–S74|issn=10785884|doi=10.1016/S1078-5884(11)60012-9}}</ref> | *Components such as [[neuropathy]] and [[peripheral arterial disease]] can mask [[Medical sign|signs]] and [[symptoms]] of the local [[infection]].<ref name="LepäntaloApelqvist2011">{{cite journal|last1=Lepäntalo|first1=M.|last2=Apelqvist|first2=J.|last3=Setacci|first3=C.|last4=Ricco|first4=J.-B.|last5=de Donato|first5=G.|last6=Becker|first6=F.|last7=Robert-Ebadi|first7=H.|last8=Cao|first8=P.|last9=Eckstein|first9=H.H.|last10=De Rango|first10=P.|last11=Diehm|first11=N.|last12=Schmidli|first12=J.|last13=Teraa|first13=M.|last14=Moll|first14=F.L.|last15=Dick|first15=F.|last16=Davies|first16=A.H.|title=Chapter V: Diabetic Foot|journal=European Journal of Vascular and Endovascular Surgery|volume=42|year=2011|pages=S60–S74|issn=10785884|doi=10.1016/S1078-5884(11)60012-9}}</ref> | ||
*Based on a study done on [[diabetes|diabetic]] [[patients]] with [[foot]] [[ulcer]]s, three components such as [[neuropathy|peripheral neuropathy]], deformity and [[trauma]] were responsible for [[pathogenesis]] of [[diabetic foot]] in 63% of cases.<ref name="pmid10333919">{{cite journal| author=Reiber GE, Vileikyte L, Boyko EJ, del Aguila M, Smith DG, Lavery LA | display-authors=etal| title=Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. | journal=Diabetes Care | year= 1999 | volume= 22 | issue= 1 | pages= 157-62 | pmid=10333919 | doi=10.2337/diacare.22.1.157 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10333919 }} </ref> | *Based on a study done on [[diabetes|diabetic]] [[patients]] with [[foot]] [[ulcer]]s, three components such as [[neuropathy|peripheral neuropathy]], deformity, and [[trauma]] were responsible for [[pathogenesis]] of [[diabetic foot]] in 63% of cases.<ref name="pmid10333919">{{cite journal| author=Reiber GE, Vileikyte L, Boyko EJ, del Aguila M, Smith DG, Lavery LA | display-authors=etal| title=Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. | journal=Diabetes Care | year= 1999 | volume= 22 | issue= 1 | pages= 157-62 | pmid=10333919 | doi=10.2337/diacare.22.1.157 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10333919 }} </ref> | ||
===Neuropathy=== | ===Neuropathy=== | ||
*The most important cause of [[diabetic foot]] is [[neuropathy]]. Based on a study, more than 60% of cases of [[diabetic foot]] are due to [[neuropathy]].<ref name="pmid1557993">{{cite journal| author=Grunfeld C| title=Diabetic foot ulcers: etiology, treatment, and prevention. | journal=Adv Intern Med | year= 1992 | volume= 37 | issue= | pages= 103-32 | pmid=1557993 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1557993 }} </ref> | *The most important cause of [[diabetic foot]] is [[neuropathy]]. Based on a study, more than 60% of cases of [[diabetic foot]] are due to [[neuropathy]].<ref name="pmid1557993">{{cite journal| author=Grunfeld C| title=Diabetic foot ulcers: etiology, treatment, and prevention. | journal=Adv Intern Med | year= 1992 | volume= 37 | issue= | pages= 103-32 | pmid=1557993 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1557993 }} </ref> | ||
*It involves roughly more than half of the [[patients]] with [[diabetes]] who are older than 60 years old. | *It involves roughly more than half of the [[patients]] with [[diabetes]] who are older than 60 years old. | ||
*[[Peripheral neuropathy]] is usually profound at the point where it leads to formation of a [[foot]] [[ulcer]]. | *[[Peripheral neuropathy]] is usually profound at the point where it leads to the formation of a [[foot]] [[ulcer]]. | ||
*Some [[Metabolic disorder|metabolic abnormalities]] due to [[hyperglycemia]] leads to [[ischemia]] of endoneurial [[Blood vessel|microvessels]]. In a nutshell, these changes are most likely caused by a combination of factors listed below: | *Some [[Metabolic disorder|metabolic abnormalities]] are due to [[hyperglycemia]] which leads to [[ischemia]] of endoneurial [[Blood vessel|microvessels]]. In a nutshell, these changes are most likely caused by a combination of the factors listed below: | ||
**High [[Blood sugar|blood glucose]] | **High [[Blood sugar|blood glucose]] | ||
**[[Reactive oxygen species]] | **[[Reactive oxygen species]] | ||
| Line 24: | Line 27: | ||
**Mechanical [[injury]] | **Mechanical [[injury]] | ||
**[[Smoking]] | **[[Smoking]] | ||
**[[Alcohol abuse]] | **[[Alcohol abuse]] | ||
*Generalized [[Symmetry|symmetric]] distal [[neuropathy|polyneuropathy]] is the most common and widely recognized form of [[diabetic neuropathy]] that leads to [[diabetic foot]]. It may be either motor, autonomic or [[Sensory system|sensory]], and can involve small fibers, large fibers or both. | *Generalized [[Symmetry|symmetric]] distal [[neuropathy|polyneuropathy]] is the most common and widely recognized form of [[diabetic neuropathy]] that leads to [[diabetic foot]]. It may be either motor, autonomic, or [[Sensory system|sensory]], and can involve small fibers, large fibers, or both. | ||
**[[nerve|Motor nerve]] involvement:<ref name="pmid9562671">{{cite journal| author=Younger DS, Rosoklija G, Hays AP| title=Diabetic peripheral neuropathy. | journal=Semin Neurol | year= 1998 | volume= 18 | issue= 1 | pages= 95-104 | pmid=9562671 | doi=10.1055/s-2008-1040865 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9562671 }} </ref><ref name="pmid2142042">{{cite journal| author=Borssén B, Bergenheim T, Lithner F| title=The epidemiology of foot lesions in diabetic patients aged 15-50 years. | journal=Diabet Med | year= 1990 | volume= 7 | issue= 5 | pages= 438-44 | pmid=2142042 | doi=10.1111/j.1464-5491.1990.tb01420.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2142042 }} </ref> | **[[nerve|Motor nerve]] involvement:<ref name="pmid9562671">{{cite journal| author=Younger DS, Rosoklija G, Hays AP| title=Diabetic peripheral neuropathy. | journal=Semin Neurol | year= 1998 | volume= 18 | issue= 1 | pages= 95-104 | pmid=9562671 | doi=10.1055/s-2008-1040865 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9562671 }} </ref><ref name="pmid2142042">{{cite journal| author=Borssén B, Bergenheim T, Lithner F| title=The epidemiology of foot lesions in diabetic patients aged 15-50 years. | journal=Diabet Med | year= 1990 | volume= 7 | issue= 5 | pages= 438-44 | pmid=2142042 | doi=10.1111/j.1464-5491.1990.tb01420.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2142042 }} </ref> | ||
***[[nerve|Motor nerve]] involvement can lead to some mechanical changes in the [[foot]] of a [[diabetes|diabetic]] [[patient]] due to loss of sufficient [[nerve|neural supply]] and alteration in natural [[anatomy]] of the [[foot]]. These mechanical changes cause more [[Anatomical terms of location|plantar]] pressure and higher risk of [[callus]] formation, which subsequently | ***[[nerve|Motor nerve]] involvement can lead to some mechanical changes in the [[foot]] of a [[diabetes|diabetic]] [[patient]] due to loss of sufficient [[nerve|neural supply]] and alteration in the natural [[anatomy]] of the [[foot]]. These mechanical changes cause more [[Anatomical terms of location|plantar]] pressure and a higher risk of [[callus]] formation, which subsequently leads to a higher rate of [[skin]] breakdown. | ||
***Moreover, these [[anatomy|anatomical changes]] usually result in wider and thicker [[foot| | ***Moreover, these [[anatomy|anatomical changes]] usually result in wider and thicker [[foot|feet]], which no longer fit in the [[patient]]'s regular shoes and cause more [[physical trauma|trauma]]. | ||
***[[Pathogenesis]] of some of these mechanical changes are listed below: | ***[[Pathogenesis]] of some of these mechanical changes are listed below: | ||
****Deprivation of [[nerve|neural supply]] to the [[muscle|intrinsic muscles]] of the [[foot]] → [[flexion| | ****Deprivation of [[nerve|neural supply]] to the [[muscle|intrinsic muscles]] of the [[foot]] → [[flexion|Long flexor]] and [[Extension (kinesiology)|extensor]] [[tendons]] imbalanced → [[Flexion]] of the [[foot]] → [[Pes cavus|High-arched]] [[foot]] and [[Hammer toe|claw-toe deformity]] | ||
****[[Toes]] [[Extension (kinesiology)|hyperextension]] → | ****[[Toes]] [[Extension (kinesiology)|hyperextension]] → Overriding of the [[foot|metatarsal-phalangeal]] [[joints]] and downward displacement of [[foot|metatarsal heads]] → Increased prominence of both | ||
****[[Toes]] [[Extension (kinesiology)|hyperextension]] → | ****[[Toes]] [[Extension (kinesiology)|hyperextension]] → Distal displacement of [[foot|metatarsal]] [[fat]] pads → Altering the natural cushioning of these [[fat]] pads | ||
**[[Autonomic nervous system|Autonomic]] [[neuropathy]]:<ref name="pmid21616974">{{cite journal| author=Ebenezer GJ, O'Donnell R, Hauer P, Cimino NP, McArthur JC, Polydefkis M| title=Impaired neurovascular repair in subjects with diabetes following experimental intracutaneous axotomy. | journal=Brain | year= 2011 | volume= 134 | issue= Pt 6 | pages= 1853-63 | pmid=21616974 | doi=10.1093/brain/awr086 | pmc=3140859 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21616974 }} </ref> | **[[Autonomic nervous system|Autonomic]] [[neuropathy]]:<ref name="pmid21616974">{{cite journal| author=Ebenezer GJ, O'Donnell R, Hauer P, Cimino NP, McArthur JC, Polydefkis M| title=Impaired neurovascular repair in subjects with diabetes following experimental intracutaneous axotomy. | journal=Brain | year= 2011 | volume= 134 | issue= Pt 6 | pages= 1853-63 | pmid=21616974 | doi=10.1093/brain/awr086 | pmc=3140859 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21616974 }} </ref> | ||
***[[Autonomic nervous system|Autonomic]] [[neuropathy]] leads to [[anhidrosis]] and impaired function of oil [[glands]]. The subsequent [[Xeroderma|dryness]] of the [[skin]] results in higher chance of [[skin]] breakdown, [[ulcer]] formation and [[bacteria|bacterial]] invasion. | ***[[Autonomic nervous system|Autonomic]] [[neuropathy]] leads to [[anhidrosis]] and impaired function of oil [[glands]]. The subsequent [[Xeroderma|dryness]] of the [[skin]] results in a higher chance of [[skin]] breakdown, [[ulcer]] formation, and [[bacteria|bacterial]] invasion. | ||
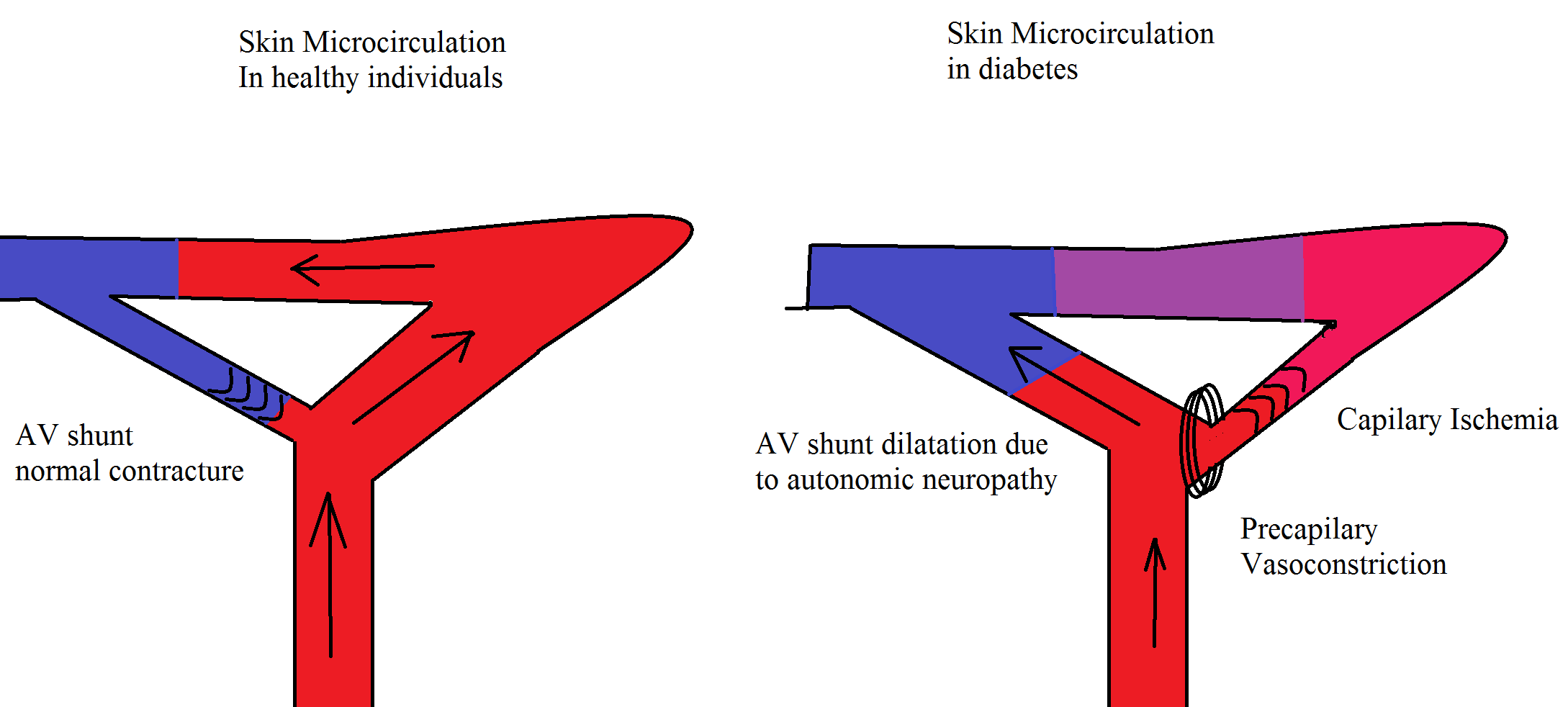
***[[Autonomic nervous system|Autonomic]] [[neuropathy]] also decreases the proper peripheral [[Sympathetic nervous system|sympathetic]] [[blood vessel|vascular]] tone which can | ***[[Autonomic nervous system|Autonomic]] [[neuropathy]] also decreases the proper peripheral [[Sympathetic nervous system|sympathetic]] [[blood vessel|vascular]] tone which can lead to higher [[blood]] flow and [[blood pressure|pressure]] in [[Anatomical terms of location|distal]] [[artery|arteries]]. The aforementioned changes plus [[capillary]] [[basement membrane]] destruction leads to [[edema]]. [[Edema]] itself increases the risk of [[ulcer]] formation. | ||
**[[Sensory system|Sensory]] [[neuropathy]]: | **[[Sensory system|Sensory]] [[neuropathy]]: | ||
***Appropriate [[sensory system]] helps [[patients]] to notice the tiniest [[fissures]] or [[blisters]] on their [[skin]]. This early sensation | ***Appropriate [[sensory system]] helps [[patients]] to notice the tiniest [[fissures]] or [[blisters]] on their [[skin]]. This early sensation makes it possible for [[patients]] to take care of these [[skin]] defects and prevent further [[Complication (medicine)|complications]]. | ||
***Conversely, [[diabetes|diabetic]] [[patients]] with [[sensory system| | ***Conversely, [[diabetes|diabetic]] [[patients]] with [[sensory system|sensory]] [[neuropathy]] are more prone to [[ulcer]] formation and related [[Complication (medicine)|complications]], since they don't feel [[pain]] with their ever-deepening [[ulcers]]. | ||
===Ischemia=== | ===Ischemia=== | ||
*[[Atherosclerosis]]:<ref name="pmid9839111">{{cite journal| author=Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM| title=Preventive foot care in people with diabetes. | journal=Diabetes Care | year= 1998 | volume= 21 | issue= 12 | pages= 2161-77 | pmid=9839111 | doi=10.2337/diacare.21.12.2161 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9839111 }} </ref><ref name="pmid6390204">{{cite journal| author=LoGerfo FW, Coffman JD| title=Current concepts. Vascular and microvascular disease of the foot in diabetes. Implications for foot care. | journal=N Engl J Med | year= 1984 | volume= 311 | issue= 25 | pages= 1615-9 | pmid=6390204 | doi=10.1056/NEJM198412203112506 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6390204 }} </ref> | *[[Atherosclerosis]]:<ref name="pmid9839111">{{cite journal| author=Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM| title=Preventive foot care in people with diabetes. | journal=Diabetes Care | year= 1998 | volume= 21 | issue= 12 | pages= 2161-77 | pmid=9839111 | doi=10.2337/diacare.21.12.2161 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9839111 }} </ref><ref name="pmid6390204">{{cite journal| author=LoGerfo FW, Coffman JD| title=Current concepts. Vascular and microvascular disease of the foot in diabetes. Implications for foot care. | journal=N Engl J Med | year= 1984 | volume= 311 | issue= 25 | pages= 1615-9 | pmid=6390204 | doi=10.1056/NEJM198412203112506 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6390204 }} </ref> | ||
**[[Atherosclerosis]] of the [[Limb (anatomy)|lower limb]] is 2 to 3 times more common in [[diabetes|diabetic]] [[patients]], compared to the normal population. | **[[Atherosclerosis]] of the [[Limb (anatomy)|lower limb]] is 2 to 3 times more common in [[diabetes|diabetic]] [[patients]], compared to the normal population. | ||
** | **Investigators reported that [[atherosclerosis]] in [[diabetes|diabetic]] [[patients]] is more prominent in [[Anterior tibial artery|tibial]] and [[fibular artery|fibular arteries]] of the calf, and [[artery|arteries]] of the [[foot]] are relatively spared. | ||
**It usually occurs due to [[inflammation]] and consequently leads to accumulation of the [[foam cells]]. | **It usually occurs due to [[inflammation]] and consequently leads to accumulation of the [[foam cells]]. | ||
*[[Microvascular disease|Micro]] and [[Macrovascular disease|macrovascular]] [[Complication (medicine)|complications]] are one of the leading causes of [[diabetes|diabetic]] [[Complication (medicine)|complications]]. [[Microvascular disease|Microvascular]] [[Complication (medicine)|complications]] cause [[skin]] damage, [[infection]] and impaired [[wound healing]].<ref name="pmid22623440">{{cite journal| author=Venermo M, Vikatmaa P, Terasaki H, Sugano N| title=Vascular laboratory for critical limb ischaemia. | journal=Scand J Surg | year= 2012 | volume= 101 | issue= 2 | pages= 86-93 | pmid=22623440 | doi=10.1177/145749691210100203 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22623440 }} </ref> | *[[Microvascular disease|Micro]] and [[Macrovascular disease|macrovascular]] [[Complication (medicine)|complications]] are one of the leading causes of [[diabetes|diabetic]] [[Complication (medicine)|complications]]. [[Microvascular disease|Microvascular]] [[Complication (medicine)|complications]] cause [[skin]] damage, [[infection]], and impaired [[wound healing]].<ref name="pmid22623440">{{cite journal| author=Venermo M, Vikatmaa P, Terasaki H, Sugano N| title=Vascular laboratory for critical limb ischaemia. | journal=Scand J Surg | year= 2012 | volume= 101 | issue= 2 | pages= 86-93 | pmid=22623440 | doi=10.1177/145749691210100203 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22623440 }} </ref> | ||
*The vascular changes which are responsible for [[foot]] problems include stiff [[artery|arteries]] due to [[calcification]] of the [[Smooth muscle|smooth muscle cells]] in the [[artery|arterial wall]] (mediasclerosis). Consequently the stiff [[artery|arteries]] are unable to expand in response to | *The vascular changes which are responsible for [[foot]] problems include stiff [[artery|arteries]] due to [[calcification]] of the [[Smooth muscle|smooth muscle cells]] in the [[artery|arterial wall]] (mediasclerosis). Consequently, the stiff [[artery|arteries]] are unable to expand in response to [[blood pressure|systolic pressure]], which can lead to the movement of [[plaque|plaques]] in calf [[artery|arteries]].<ref name="pmid2411027">{{cite journal| author=McMillan DE| title=Blood flow and the localization of atherosclerotic plaques. | journal=Stroke | year= 1985 | volume= 16 | issue= 4 | pages= 582-7 | pmid=2411027 | doi=10.1161/01.str.16.4.582 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2411027 }} </ref> | ||
*Most of these changes are discovered by an impaired [[ABI|ankle brachial index]] ([[ABI]]). | *Most of these changes are discovered by an impaired [[ABI|ankle brachial index]] ([[ABI]]). | ||
**The resting [[ABI]] is the ratio of the [[blood pressure]] in the [[Limb (anatomy)|lower limb]] to the [[blood pressure]] of the [[arms]]. It is calculated by dividing the [[systolic blood pressure]] of the [[ankle]] by the [[systolic blood pressure]] of the [[arm]]. | **The resting [[ABI]] is the ratio of the [[blood pressure]] in the [[Limb (anatomy)|lower limb]] to the [[blood pressure]] of the [[arms]]. It is calculated by dividing the [[systolic blood pressure]] of the [[ankle]] by the [[systolic blood pressure]] of the [[arm]]. | ||
**It is a non-invasive method to assess the [[Limb (anatomy)|lower extremty]] [[artery|arterial system]] and to detect the presence of [[artery|arterial]] occlusion [[disease]]. | **It is a non-invasive method to assess the [[Limb (anatomy)|lower extremty]] [[artery|arterial system]] and to detect the presence of [[artery|arterial]] occlusion [[disease]]. | ||
*Even in the presence of [[neuropathy|neuropathic]] [[diabetic foot|foot ulcers]], the reason of non healing [[wounds]] could be due to impaired [[blood]] supply to the [[Tissue (biology)|tissue]], which could be further augmented by [[antihypertensive]] [[medications]].<ref name="pmid22529027">{{cite journal| author=Alexiadou K, Doupis J| title=Management of diabetic foot ulcers. | journal=Diabetes Ther | year= 2012 | volume= 3 | issue= 1 | pages= 4 | pmid=22529027 | doi=10.1007/s13300-012-0004-9 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22529027 }} </ref>. | *Even in the presence of [[neuropathy|neuropathic]] [[diabetic foot|foot ulcers]], the reason of non healing [[wounds]] could be due to impaired [[blood]] supply to the [[Tissue (biology)|tissue]], which could be further augmented by [[antihypertensive]] [[medications]].<ref name="pmid22529027">{{cite journal| author=Alexiadou K, Doupis J| title=Management of diabetic foot ulcers. | journal=Diabetes Ther | year= 2012 | volume= 3 | issue= 1 | pages= 4 | pmid=22529027 | doi=10.1007/s13300-012-0004-9 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22529027 }} </ref>. | ||
[[Image:Microcirculation image.png|500px|Neuropathy and angiopathy in the foot have a positive feedback on each other]] | [[Image:Microcirculation image.png|500px|Neuropathy and angiopathy in the foot have a positive feedback on each other]] | ||
===Trauma=== | ===Trauma=== | ||
*[[Physical trauma|Trauma]] to the [[foot]] is frequently the trigger of [[diabetes|diabetic]] [[foot]] [[ulcer]] development and repetitive [[Physical trauma|trauma]] and pressure to the area prevent [[Wound healing|healing]].<ref name="pmid25982677">{{cite journal| author=Noor S, Zubair M, Ahmad J| title=Diabetic foot ulcer--A review on pathophysiology, classification and microbial etiology. | journal=Diabetes Metab Syndr | year= 2015 | volume= 9 | issue= 3 | pages= 192-9 | pmid=25982677 | doi=10.1016/j.dsx.2015.04.007 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25982677 }} </ref> | |||
*[[Physical trauma|Trauma]] to the [[foot]] is frequently the trigger of [[diabetes|diabetic]] [[foot]] [[ulcer]] development, and repetitive [[Physical trauma|trauma]] and pressure to the area prevent [[Wound healing|healing]].<ref name="pmid25982677">{{cite journal| author=Noor S, Zubair M, Ahmad J| title=Diabetic foot ulcer--A review on pathophysiology, classification and microbial etiology. | journal=Diabetes Metab Syndr | year= 2015 | volume= 9 | issue= 3 | pages= 192-9 | pmid=25982677 | doi=10.1016/j.dsx.2015.04.007 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25982677 }} </ref> | |||
*Excessive [[Anatomical terms of location|plantar]] pressure is related to limited [[joint]] mobility and [[foot]] deformities (such as [[Charcot joint|charcot foot]] and [[hammer toe]]). Limited [[joint]] mobility and abnormal [[foot]] biomechanisms have been associated to an increased risk of [[ulcer|ulceration]].<ref name="pmid22529027">{{cite journal| author=Alexiadou K, Doupis J| title=Management of diabetic foot ulcers. | journal=Diabetes Ther | year= 2012 | volume= 3 | issue= 1 | pages= 4 | pmid=22529027 | doi=10.1007/s13300-012-0004-9 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22529027 }} </ref> | *Excessive [[Anatomical terms of location|plantar]] pressure is related to limited [[joint]] mobility and [[foot]] deformities (such as [[Charcot joint|charcot foot]] and [[hammer toe]]). Limited [[joint]] mobility and abnormal [[foot]] biomechanisms have been associated to an increased risk of [[ulcer|ulceration]].<ref name="pmid22529027">{{cite journal| author=Alexiadou K, Doupis J| title=Management of diabetic foot ulcers. | journal=Diabetes Ther | year= 2012 | volume= 3 | issue= 1 | pages= 4 | pmid=22529027 | doi=10.1007/s13300-012-0004-9 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22529027 }} </ref> | ||
*Poor [[Visual system|vision]] and [[Sensory system|sensory]] [[neuropathy]] further put [[diabetes|diabetic]] [[patients]] at risk of [[foot]] [[ulcer|ulceration]], as they not feel the [[pain]], nor do they see the [[ulcer]]. Loss of balance can also make [[patients]] more susceptible to falls.<ref name="pmid22529027">{{cite journal| author=Alexiadou K, Doupis J| title=Management of diabetic foot ulcers. | journal=Diabetes Ther | year= 2012 | volume= 3 | issue= 1 | pages= 4 | pmid=22529027 | doi=10.1007/s13300-012-0004-9 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22529027 }} </ref> | *Poor [[Visual system|vision]] and [[Sensory system|sensory]] [[neuropathy]] further put [[diabetes|diabetic]] [[patients]] at risk of [[foot]] [[ulcer|ulceration]], as they do not feel the [[pain]], nor do they see the [[ulcer]]. Loss of balance can also make [[patients]] more susceptible to falls.<ref name="pmid22529027">{{cite journal| author=Alexiadou K, Doupis J| title=Management of diabetic foot ulcers. | journal=Diabetes Ther | year= 2012 | volume= 3 | issue= 1 | pages= 4 | pmid=22529027 | doi=10.1007/s13300-012-0004-9 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22529027 }} </ref> | ||
===Defective hypoxic response=== | ===Defective hypoxic response=== | ||
*A [[transcription factor]] named [[HIF1A|hypoxia‐inducible factor‐1]] ([[HIF1A|HIF‐1]]), which | |||
*Since [[HIF1A|HIF‐1]] helps cells to | *A [[transcription factor]] named [[HIF1A|hypoxia‐inducible factor‐1]] ([[HIF1A|HIF‐1]]), which becomes stable in [[hypoxemia|hypoxia]], functions as a [[oxygen]] [[homeostasis]] regulator.<ref name="pmid22304911">{{cite journal| author=Semenza GL| title=Hypoxia-inducible factors in physiology and medicine. | journal=Cell | year= 2012 | volume= 148 | issue= 3 | pages= 399-408 | pmid=22304911 | doi=10.1016/j.cell.2012.01.021 | pmc=3437543 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22304911 }} </ref> | ||
*In addition, [[HIF1A|hypoxia‐inducible factor‐1]] is responsible for expression of [[gene|genes]] that are critical to facilitate [[wound healing]], such as the [[GLUT1]] and [[GLUT3]], [[lactate dehydrogenase]], [[gene|genes]] responsible for proper [[Mitochondrion|mitochondrial]] function (such as [[Phosphoinositide-dependent kinase-1|phosphoinositide‐dependent kinase‐1]]), [[type I collagen]] and [[fibronectin]]. <ref name="pmid26453314">{{cite journal| author=Catrina SB, Zheng X| title=Disturbed hypoxic responses as a pathogenic mechanism of diabetic foot ulcers. | journal=Diabetes Metab Res Rev | year= 2016 | volume= 32 Suppl 1 | issue= | pages= 179-85 | pmid=26453314 | doi=10.1002/dmrr.2742 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26453314 }} </ref> | *Since [[HIF1A|HIF‐1]] helps cells to respond adequately to [[hypoxemia|hypoxia]] (by regulating [[erythropoiesis]], [[metabolism|metabolic changes]], [[angiogenesis]], [[Cell growth|proliferation]], migration, and [[cell]] survival), it plays a critical role in [[wound healing]].<ref name="pmid23937437">{{cite journal| author=Semenza GL| title=Oxygen sensing, hypoxia-inducible factors, and disease pathophysiology. | journal=Annu Rev Pathol | year= 2014 | volume= 9 | issue= | pages= 47-71 | pmid=23937437 | doi=10.1146/annurev-pathol-012513-104720 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23937437 }} </ref> | ||
*There are numerous studies that detected lower | *In addition, [[HIF1A|hypoxia‐inducible factor‐1]] is responsible for the expression of [[gene|genes]] that are critical to facilitate [[wound healing]], such as the [[GLUT1]] and [[GLUT3]], [[lactate dehydrogenase]], [[gene|genes]] responsible for proper [[Mitochondrion|mitochondrial]] function (such as [[Phosphoinositide-dependent kinase-1|phosphoinositide‐dependent kinase‐1]]), [[type I collagen]], and [[fibronectin]]. <ref name="pmid26453314">{{cite journal| author=Catrina SB, Zheng X| title=Disturbed hypoxic responses as a pathogenic mechanism of diabetic foot ulcers. | journal=Diabetes Metab Res Rev | year= 2016 | volume= 32 Suppl 1 | issue= | pages= 179-85 | pmid=26453314 | doi=10.1002/dmrr.2742 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26453314 }} </ref> | ||
*One of the known [[pathogenesis]] of destabilized [[HIF1A|hypoxia‐inducible factor‐1]] is [[hyperglycemia]]. This destabilization in [[hyperglycemia|hyperglycaemic conditions]] has been explained by an increase in tendency of [[HIF1A|HIF‐1]] towards [[Von Hippel–Lindau tumor suppressor|VHL]]‐dependent degradation. <ref name="pmid21124777">{{cite journal| author=Bento CF, Fernandes R, Ramalho J, Marques C, Shang F, Taylor A | display-authors=etal| title=The chaperone-dependent ubiquitin ligase CHIP targets HIF-1α for degradation in the presence of methylglyoxal. | journal=PLoS One | year= 2010 | volume= 5 | issue= 11 | pages= e15062 | pmid=21124777 | doi=10.1371/journal.pone.0015062 | pmc=2993942 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21124777 }} </ref> | *There are numerous studies that detected lower levels of [[HIF1A|HIF‐1]] in [[biopsy|biopsies]] of [[diabetic foot]]. <ref name="pmid19057015">{{cite journal| author=Botusan IR, Sunkari VG, Savu O, Catrina AI, Grünler J, Lindberg S | display-authors=etal| title=Stabilization of HIF-1alpha is critical to improve wound healing in diabetic mice. | journal=Proc Natl Acad Sci U S A | year= 2008 | volume= 105 | issue= 49 | pages= 19426-31 | pmid=19057015 | doi=10.1073/pnas.0805230105 | pmc=2614777 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19057015 }} </ref><ref name="pmid17971009">{{cite journal| author=Mace KA, Yu DH, Paydar KZ, Boudreau N, Young DM| title=Sustained expression of Hif-1alpha in the diabetic environment promotes angiogenesis and cutaneous wound repair. | journal=Wound Repair Regen | year= 2007 | volume= 15 | issue= 5 | pages= 636-45 | pmid=17971009 | doi=10.1111/j.1524-475X.2007.00278.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17971009 }} </ref><ref name="pmid15561954">{{cite journal| author=Catrina SB, Okamoto K, Pereira T, Brismar K, Poellinger L| title=Hyperglycemia regulates hypoxia-inducible factor-1alpha protein stability and function. | journal=Diabetes | year= 2004 | volume= 53 | issue= 12 | pages= 3226-32 | pmid=15561954 | doi=10.2337/diabetes.53.12.3226 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15561954 }} </ref> | ||
*One of the known [[pathogenesis]] of destabilized [[HIF1A|hypoxia‐inducible factor‐1]] is [[hyperglycemia]]. This destabilization in [[hyperglycemia|hyperglycaemic conditions]] has been explained by an increase in the tendency of [[HIF1A|HIF‐1]] towards [[Von Hippel–Lindau tumor suppressor|VHL]]‐dependent degradation. <ref name="pmid21124777">{{cite journal| author=Bento CF, Fernandes R, Ramalho J, Marques C, Shang F, Taylor A | display-authors=etal| title=The chaperone-dependent ubiquitin ligase CHIP targets HIF-1α for degradation in the presence of methylglyoxal. | journal=PLoS One | year= 2010 | volume= 5 | issue= 11 | pages= e15062 | pmid=21124777 | doi=10.1371/journal.pone.0015062 | pmc=2993942 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21124777 }} </ref> | |||
==Genetics== | ==Genetics== | ||
*Naturally [[growth factors]] and [[cytokines]] are two mediators involved in [[wound healing]]. It is crystal clear that any [[Genetics|genetical]] changes that affect the aforementioned mediators can result in defective [[wound healing]] and higher chance of [[diabetic foot]]. The following are some known [[Genetics|genetical]] changes:<ref name="pmid27372176">{{cite journal| author=Jhamb S, Vangaveti VN, Malabu UH| title=Genetic and molecular basis of diabetic foot ulcers: Clinical review. | journal=J Tissue Viability | year= 2016 | volume= 25 | issue= 4 | pages= 229-236 | pmid=27372176 | doi=10.1016/j.jtv.2016.06.005 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27372176 }} </ref><ref name="pmid21159125">{{cite journal| author=Rafehi H, El-Osta A, Karagiannis TC| title=Genetic and epigenetic events in diabetic wound healing. | journal=Int Wound J | year= 2011 | volume= 8 | issue= 1 | pages= 12-21 | pmid=21159125 | doi=10.1111/j.1742-481X.2010.00745.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21159125 }} </ref><ref name="pmid3501286">{{cite journal| author=Laato M, Kähäri VM, Niinikoski J, Vuorio E| title=Epidermal growth factor increases collagen production in granulation tissue by stimulation of fibroblast proliferation and not by activation of procollagen genes. | journal=Biochem J | year= 1987 | volume= 247 | issue= 2 | pages= 385-8 | pmid=3501286 | doi=10.1042/bj2470385 | pmc=1148420 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3501286 }} </ref><ref name="pmid23936790">{{cite journal| author=Singh K, Singh VK, Agrawal NK, Gupta SK, Singh K| title=Association of Toll-like receptor 4 polymorphisms with diabetic foot ulcers and application of artificial neural network in DFU risk assessment in type 2 diabetes patients. | journal=Biomed Res Int | year= 2013 | volume= 2013 | issue= | pages= 318686 | pmid=23936790 | doi=10.1155/2013/318686 | pmc=3725976 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23936790 }} </ref> | *Naturally [[growth factors]] and [[cytokines]] are two mediators involved in [[wound healing]]. It is crystal clear that any [[Genetics|genetical]] changes that affect the aforementioned mediators can result in defective [[wound healing]] and higher chance of [[diabetic foot]]. The following are some known [[Genetics|genetical]] changes:<ref name="pmid27372176">{{cite journal| author=Jhamb S, Vangaveti VN, Malabu UH| title=Genetic and molecular basis of diabetic foot ulcers: Clinical review. | journal=J Tissue Viability | year= 2016 | volume= 25 | issue= 4 | pages= 229-236 | pmid=27372176 | doi=10.1016/j.jtv.2016.06.005 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27372176 }} </ref><ref name="pmid21159125">{{cite journal| author=Rafehi H, El-Osta A, Karagiannis TC| title=Genetic and epigenetic events in diabetic wound healing. | journal=Int Wound J | year= 2011 | volume= 8 | issue= 1 | pages= 12-21 | pmid=21159125 | doi=10.1111/j.1742-481X.2010.00745.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21159125 }} </ref><ref name="pmid3501286">{{cite journal| author=Laato M, Kähäri VM, Niinikoski J, Vuorio E| title=Epidermal growth factor increases collagen production in granulation tissue by stimulation of fibroblast proliferation and not by activation of procollagen genes. | journal=Biochem J | year= 1987 | volume= 247 | issue= 2 | pages= 385-8 | pmid=3501286 | doi=10.1042/bj2470385 | pmc=1148420 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3501286 }} </ref><ref name="pmid23936790">{{cite journal| author=Singh K, Singh VK, Agrawal NK, Gupta SK, Singh K| title=Association of Toll-like receptor 4 polymorphisms with diabetic foot ulcers and application of artificial neural network in DFU risk assessment in type 2 diabetes patients. | journal=Biomed Res Int | year= 2013 | volume= 2013 | issue= | pages= 318686 | pmid=23936790 | doi=10.1155/2013/318686 | pmc=3725976 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23936790 }} </ref> | ||
**A [[single nucleotide polymorphism]] ([[single nucleotide polymorphism|SNPs]]) is responsible in the variation of these [[growth factors]] and [[cytokines]]. The best known [[gene]] is [[MAPK14]] located on [[chromosome 6]]. | **A [[single nucleotide polymorphism]] ([[single nucleotide polymorphism|SNPs]]) is responsible in the variation of these [[growth factors]] and [[cytokines]]. The best known [[gene]] is [[MAPK14]] located on [[chromosome 6]]. | ||
**Decreased expression of certain [[cytokines]] and [[growth factors]] (such as [[Insulin-like growth factor-I|IGF-1]], [[TGF beta|TGF‐β1]], [[Platelet-derived growth factor|PDGF]], [[Epidermal growth factor|EGF]], [[Interleukin 8]] and [[Angiopoietin receptor|Angiopoietin‐2]]) | **Decreased expression of certain [[cytokines]] and [[growth factors]] (such as [[Insulin-like growth factor-I|IGF-1]], [[TGF beta|TGF‐β1]], [[Platelet-derived growth factor|PDGF]], [[Epidermal growth factor|EGF]], [[Interleukin 8]], and [[Angiopoietin receptor|Angiopoietin‐2]]) | ||
*The HSPA1B genotype, a member of the [[heat shock protein|heat shock protein 70]] ([[heat shock protein|Hsp70]]) family, has been related to higher chance of diabetic foot development, amputation and elongated hospital stay.<ref name="pmid19731315">{{cite journal| author=Mir KA, Pugazhendhi S, Paul MJ, Nair A, Ramakrishna BS| title=Heat-shock protein 70 gene polymorphism is associated with the severity of diabetic foot ulcer and the outcome of surgical treatment. | journal=Br J Surg | year= 2009 | volume= 96 | issue= 10 | pages= 1205-9 | pmid=19731315 | doi=10.1002/bjs.6689 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19731315 }} </ref> | *The HSPA1B genotype, a member of the [[heat shock protein|heat shock protein 70]] ([[heat shock protein|Hsp70]]) family, has been related to a higher chance of diabetic foot development, amputation, and elongated hospital stay.<ref name="pmid19731315">{{cite journal| author=Mir KA, Pugazhendhi S, Paul MJ, Nair A, Ramakrishna BS| title=Heat-shock protein 70 gene polymorphism is associated with the severity of diabetic foot ulcer and the outcome of surgical treatment. | journal=Br J Surg | year= 2009 | volume= 96 | issue= 10 | pages= 1205-9 | pmid=19731315 | doi=10.1002/bjs.6689 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19731315 }} </ref> | ||
==Associated Conditions== | ==Associated Conditions== | ||
Conditions associated with [[diabetic foot]] include:<ref name="pmid31850665">{{cite journal| author=Vileikyte L, Pouwer F, Gonzalez JS| title=Psychosocial research in the diabetic foot: Are we making progress? | journal=Diabetes Metab Res Rev | year= 2020 | volume= 36 Suppl 1 | issue= | pages= e3257 | pmid=31850665 | doi=10.1002/dmrr.3257 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31850665 }} </ref><ref name="pmid20670730">{{cite journal| author=Williams LH, Rutter CM, Katon WJ, Reiber GE, Ciechanowski P, Heckbert SR | display-authors=etal| title=Depression and incident diabetic foot ulcers: a prospective cohort study. | journal=Am J Med | year= 2010 | volume= 123 | issue= 8 | pages= 748-754.e3 | pmid=20670730 | doi=10.1016/j.amjmed.2010.01.023 | pmc=2913143 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20670730 }} </ref><ref name="pmid26415868">{{cite journal| author=Iacopi E, Coppelli A, Goretti C, Piaggesi A| title=Necrotizing Fasciitis and The Diabetic Foot. | journal=Int J Low Extrem Wounds | year= 2015 | volume= 14 | issue= 4 | pages= 316-27 | pmid=26415868 | doi=10.1177/1534734615606534 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26415868 }} </ref><ref name="pmid25331710">{{cite journal| author=Tiwari S, Pratyush DD, Gupta SK, Singh SK| title=Vitamin D deficiency is associated with inflammatory cytokine concentrations in patients with diabetic foot infection. | journal=Br J Nutr | year= 2014 | volume= 112 | issue= 12 | pages= 1938-43 | pmid=25331710 | doi=10.1017/S0007114514003018 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25331710 }} </ref><ref name="pmid29791040">{{cite journal| author=Sellman A, Katzman P, Andreasson S, Löndahl M| title=Presence of chronic diabetic foot ulcers is associated with more frequent and more advanced retinopathy. | journal=Diabet Med | year= 2018 | volume= 35 | issue= 10 | pages= 1364-1370 | pmid=29791040 | doi=10.1111/dme.13682 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29791040 }} </ref><ref name="pmid27648034">{{cite journal| author=Akkus G, Evran M, Gungor D, Karakas M, Sert M, Tetiker T| title=Tinea pedis and onychomycosis frequency in diabetes mellitus patients and diabetic foot ulcers. A cross sectional - observational study. | journal=Pak J Med Sci | year= 2016 | volume= 32 | issue= 4 | pages= 891-5 | pmid=27648034 | doi=10.12669/pjms.324.10027 | pmc=5017097 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27648034 }} </ref> | Conditions associated with [[diabetic foot]] include:<ref name="pmid31850665">{{cite journal| author=Vileikyte L, Pouwer F, Gonzalez JS| title=Psychosocial research in the diabetic foot: Are we making progress? | journal=Diabetes Metab Res Rev | year= 2020 | volume= 36 Suppl 1 | issue= | pages= e3257 | pmid=31850665 | doi=10.1002/dmrr.3257 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31850665 }} </ref><ref name="pmid20670730">{{cite journal| author=Williams LH, Rutter CM, Katon WJ, Reiber GE, Ciechanowski P, Heckbert SR | display-authors=etal| title=Depression and incident diabetic foot ulcers: a prospective cohort study. | journal=Am J Med | year= 2010 | volume= 123 | issue= 8 | pages= 748-754.e3 | pmid=20670730 | doi=10.1016/j.amjmed.2010.01.023 | pmc=2913143 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20670730 }} </ref><ref name="pmid26415868">{{cite journal| author=Iacopi E, Coppelli A, Goretti C, Piaggesi A| title=Necrotizing Fasciitis and The Diabetic Foot. | journal=Int J Low Extrem Wounds | year= 2015 | volume= 14 | issue= 4 | pages= 316-27 | pmid=26415868 | doi=10.1177/1534734615606534 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26415868 }} </ref><ref name="pmid25331710">{{cite journal| author=Tiwari S, Pratyush DD, Gupta SK, Singh SK| title=Vitamin D deficiency is associated with inflammatory cytokine concentrations in patients with diabetic foot infection. | journal=Br J Nutr | year= 2014 | volume= 112 | issue= 12 | pages= 1938-43 | pmid=25331710 | doi=10.1017/S0007114514003018 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25331710 }} </ref><ref name="pmid29791040">{{cite journal| author=Sellman A, Katzman P, Andreasson S, Löndahl M| title=Presence of chronic diabetic foot ulcers is associated with more frequent and more advanced retinopathy. | journal=Diabet Med | year= 2018 | volume= 35 | issue= 10 | pages= 1364-1370 | pmid=29791040 | doi=10.1111/dme.13682 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29791040 }} </ref><ref name="pmid27648034">{{cite journal| author=Akkus G, Evran M, Gungor D, Karakas M, Sert M, Tetiker T| title=Tinea pedis and onychomycosis frequency in diabetes mellitus patients and diabetic foot ulcers. A cross sectional - observational study. | journal=Pak J Med Sci | year= 2016 | volume= 32 | issue= 4 | pages= 891-5 | pmid=27648034 | doi=10.12669/pjms.324.10027 | pmc=5017097 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27648034 }} </ref> | ||
*[[Charcot joint|Charcot arthropathy]] | *[[Charcot joint|Charcot arthropathy]] | ||
*[[Peripheral arterial disease]] | |||
*[[Psychiatry|Psychosocial conditions]], such as [[depression]] | *[[Psychiatry|Psychosocial conditions]], such as [[depression]] | ||
*[[Necrotizing fasciitis]] ([[Necrotizing fasciitis|NF]]) | *[[Necrotizing fasciitis]] ([[Necrotizing fasciitis|NF]]) | ||
*[[Vitamin D deficiency]] | *[[Vitamin D deficiency]] | ||
*[[Fungus|Fungal infections]], such as [[Athlete's foot|tinea pedis]] and [[onychomycosis]] | *[[Fungus|Fungal infections]], such as [[Athlete's foot|tinea pedis]] and [[onychomycosis]] | ||
*Other [[Complication (medicine)|complications]] of [[diabetes mellitus]], | *Other [[Complication (medicine)|complications]] of [[diabetes mellitus]], such as [[diabetic retinopathy]] and [[nephropathy]] | ||
*[[Hypertension]] | |||
==Gross Pathology== | ==Gross Pathology== | ||
*On [[gross pathology]], the most common site of [[ulcer|ulceration]] is on the [[Sole (foot)| | [[File:Dijabetesno stopalo 2011 1.jpg|200px|left|thumb|Diabetic foot ulcer, source:wikimedia commons<ref>Diabetic foot ulcer. Author: Milorad Dimic MD, Nis, Serbia, decembar 2011</ref>]] | ||
*Depth of [[ulcers]] could be different, ranging from superficial [[ulcer|wounds]] to involvement of [[ligament|ligaments]] and [[tendon|tendons]], [[joint]] capsule, or deep [[fascia]] | [[File:Diabetic Charcot Foot Deformity.jpg|200px|right|thumb|Charcot joint, source:wikimedia commons]] | ||
*On [[gross pathology]], the most common site of [[ulcer|ulceration]] is on the [[Sole (foot)|soles of the feet]], under the [[Metatarsus|metatarsal head]] (particularly at the second [[Metatarsus|metatarsal head]]). | |||
*Depth of [[ulcers]] could be different, ranging from superficial [[ulcer|wounds]] to the involvement of [[ligament|ligaments]] and [[tendon|tendons]], [[joint]] capsule, or deep [[fascia]] | |||
*There is a high chance of concurrent [[anatomy|anatomical]] [[foot]] deformities, such as [[Hammer toe|claw toe]] or [[charcot joint]]. | *There is a high chance of concurrent [[anatomy|anatomical]] [[foot]] deformities, such as [[Hammer toe|claw toe]] or [[charcot joint]]. | ||
*Presence of [[infection|infective features]] of a [[ulcer]], such as [[erythema]], [[edema|swelling]] and [[pus|purulent]] and malodor discharge. | *Presence of [[infection|infective features]] of a [[ulcer]], such as [[erythema]], [[edema|swelling]], and [[pus|purulent]] and malodor discharge. | ||
*[[Abscess]] | *[[Abscess]] | ||
*[[Gangrene]] | *[[Gangrene]] | ||
<br> | |||
<br> | |||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
The following list is a summary of the possible [[Microscope|microscopic]] [[histopathological|histopathological changes]] of [[diabetic foot]]:<ref name="pmid21561305">{{cite journal| author=Neut D, Tijdens-Creusen EJ, Bulstra SK, van der Mei HC, Busscher HJ| title=Biofilms in chronic diabetic foot ulcers--a study of 2 cases. | journal=Acta Orthop | year= 2011 | volume= 82 | issue= 3 | pages= 383-5 | pmid=21561305 | doi=10.3109/17453674.2011.581265 | pmc=3235322 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21561305 }} </ref><ref name="pmid18719880">{{cite journal| author=Aragón-Sánchez FJ, Cabrera-Galván JJ, Quintana-Marrero Y, Hernández-Herrero MJ, Lázaro-Martínez JL, García-Morales E | display-authors=etal| title=Outcomes of surgical treatment of diabetic foot osteomyelitis: a series of 185 patients with histopathological confirmation of bone involvement. | journal=Diabetologia | year= 2008 | volume= 51 | issue= 11 | pages= 1962-70 | pmid=18719880 | doi=10.1007/s00125-008-1131-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18719880 }} </ref><ref name="pmid14578249">{{cite journal| author=Piaggesi A, Viacava P, Rizzo L, Naccarato G, Baccetti F, Romanelli M | display-authors=etal| title=Semiquantitative analysis of the histopathological features of the neuropathic foot ulcer: effects of pressure relief. | journal=Diabetes Care | year= 2003 | volume= 26 | issue= 11 | pages= 3123-8 | pmid=14578249 | doi=10.2337/diacare.26.11.3123 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14578249 }} </ref> | The following list is a summary of the possible [[Microscope|microscopic]] [[histopathological|histopathological changes]] of [[diabetic foot]]:<ref name="pmid21561305">{{cite journal| author=Neut D, Tijdens-Creusen EJ, Bulstra SK, van der Mei HC, Busscher HJ| title=Biofilms in chronic diabetic foot ulcers--a study of 2 cases. | journal=Acta Orthop | year= 2011 | volume= 82 | issue= 3 | pages= 383-5 | pmid=21561305 | doi=10.3109/17453674.2011.581265 | pmc=3235322 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21561305 }} </ref><ref name="pmid18719880">{{cite journal| author=Aragón-Sánchez FJ, Cabrera-Galván JJ, Quintana-Marrero Y, Hernández-Herrero MJ, Lázaro-Martínez JL, García-Morales E | display-authors=etal| title=Outcomes of surgical treatment of diabetic foot osteomyelitis: a series of 185 patients with histopathological confirmation of bone involvement. | journal=Diabetologia | year= 2008 | volume= 51 | issue= 11 | pages= 1962-70 | pmid=18719880 | doi=10.1007/s00125-008-1131-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18719880 }} </ref><ref name="pmid14578249">{{cite journal| author=Piaggesi A, Viacava P, Rizzo L, Naccarato G, Baccetti F, Romanelli M | display-authors=etal| title=Semiquantitative analysis of the histopathological features of the neuropathic foot ulcer: effects of pressure relief. | journal=Diabetes Care | year= 2003 | volume= 26 | issue= 11 | pages= 3123-8 | pmid=14578249 | doi=10.2337/diacare.26.11.3123 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14578249 }} </ref> | ||
*[[Skin]] [[necrosis]] | *[[Skin]] [[necrosis]] | ||
*[[Hyperkeratosis]] | *[[Hyperkeratosis]] | ||
| Line 98: | Line 115: | ||
*[[Granulation tissue]] | *[[Granulation tissue]] | ||
*[[biofilm|Biofilms]] formation, which resembles infection | *[[biofilm|Biofilms]] formation, which resembles infection | ||
*[[Angiogenesis]], which | *[[Angiogenesis]], which represents proper [[wound healing]] | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Endocrinology]] | [[Category:Endocrinology]] | ||
[[Category: | [[Category:Up to Date]] | ||
Latest revision as of 14:08, 28 September 2021
|
Diabetic foot Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Diabetic foot pathophysiology On the Web |
|
American Roentgen Ray Society Images of Diabetic foot pathophysiology |
|
Risk calculators and risk factors for Diabetic foot pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Anahita Deylamsalehi, M.D.[2]Vishnu Vardhan Serla M.B.B.S. [3]
Overview
Diabetic foot is an umbrella term for foot problems in patients with diabetes mellitus. Neuropathy, ischemia and trauma are three main pathogenesis of diabetic foot. Neuropathy is the most common and is the responsible element in more than 60% of diabetic foot cases. Factors such as high blood glucose, reactive oxygen species, insufficient oxygenation of the nerves, and inflammation leads to neuropathy development in diabetic patients and it gets worse with alcohol use and smoking. Neuropathy can involve motor, autonomic, or sensory nerves and is able to involve both large and small fibers. Motor nerve involvement can lead to some mechanical changes in the foot of a diabetic patient, which causes more plantar pressure and higher risk of callus formation. Each and every factor leads to a higher rate of skin breakdown and ulceration. Autonomic neuropathy leads to anhidrosis and impaired function of oil glands, subsequent skin dryness, higher chance of skin breakdown, and ulcer formation. Diabetic patients with sensory neuropathy are more prone to ulcer formation and related complications, since they don't feel pain with ever-deepening ulcers. Ischemia is the second best known pathogenesis of diabetic foot that could occur due to a higher rate of lower limb atherosclerosis in diabetic patients, compared to the normal population. Diabetes related complications such as micro and macrovascular complications further intensify ischemia. Ischemic changes can be discovered by an impaired ankle brachial index (ABI). Trauma to the foot usually acts as a trigger for diabetic foot. A defective hypoxic response has been explained in diabetic foot, which is related to a transcription factor named hypoxia‐inducible factor‐1 (HIF‐1). Lower levels of HIF‐1 in biopsies of diabetic foot could be related to its role in wound healing. Some genetic associations (such as MAPK14 gene located on chromosome 6, decreased expression of certain cytokines and growth factors, and the HSPA1B genotype) have been explained in diabetic foot development. Charcot arthropathy, some psychosocial conditions, necrotizing fasciitis (NF), vitamin D deficiency, tinea pedis, onychomycosis, and diabetic retinopathy are associated conditions in diabetic foot. On gross pathology, the most common site of ulceration is on the soles of the feet, under the metatarsal head with various depths and possible anatomical deformities of the foot. In microscopic evaluations of the ulcers, evidence of necrosis, hyperkeratosis, fibrosis, inflammation, cellular debris, granulation tissue, and angiogenesis have been found.
Pathophysiology
- Diabetic foot is an umbrella term for foot problems in patients with diabetes mellitus. There are numerous responsible pathogenesis, such as arterial abnormalities, diabetic neuropathy, delayed wound healing, and being more vulnerable to infection or gangrene of the foot. The key components of diabetic foot are neuropathy, ischemia, and trauma. [1]
- Only 10% of diabetic foot cases are exclusively due to ischemia, nevertheless, 90% of them are related to neuropathy (alone or in combination to ischemia).[2]
- Components such as neuropathy and peripheral arterial disease can mask signs and symptoms of the local infection.[3]
- Based on a study done on diabetic patients with foot ulcers, three components such as peripheral neuropathy, deformity, and trauma were responsible for pathogenesis of diabetic foot in 63% of cases.[4]
Neuropathy
- The most important cause of diabetic foot is neuropathy. Based on a study, more than 60% of cases of diabetic foot are due to neuropathy.[5]
- It involves roughly more than half of the patients with diabetes who are older than 60 years old.
- Peripheral neuropathy is usually profound at the point where it leads to the formation of a foot ulcer.
- Some metabolic abnormalities are due to hyperglycemia which leads to ischemia of endoneurial microvessels. In a nutshell, these changes are most likely caused by a combination of the factors listed below:
- High blood glucose
- Reactive oxygen species
- Vasculopathy
- Insufficient oxygenation of the nerves
- Presence of inflammation and autoimmunity due to diabetes
- Genetic factors
- Mechanical injury
- Smoking
- Alcohol abuse
- Generalized symmetric distal polyneuropathy is the most common and widely recognized form of diabetic neuropathy that leads to diabetic foot. It may be either motor, autonomic, or sensory, and can involve small fibers, large fibers, or both.
- Motor nerve involvement:[6][7]
- Motor nerve involvement can lead to some mechanical changes in the foot of a diabetic patient due to loss of sufficient neural supply and alteration in the natural anatomy of the foot. These mechanical changes cause more plantar pressure and a higher risk of callus formation, which subsequently leads to a higher rate of skin breakdown.
- Moreover, these anatomical changes usually result in wider and thicker feet, which no longer fit in the patient's regular shoes and cause more trauma.
- Pathogenesis of some of these mechanical changes are listed below:
- Deprivation of neural supply to the intrinsic muscles of the foot → Long flexor and extensor tendons imbalanced → Flexion of the foot → High-arched foot and claw-toe deformity
- Toes hyperextension → Overriding of the metatarsal-phalangeal joints and downward displacement of metatarsal heads → Increased prominence of both
- Toes hyperextension → Distal displacement of metatarsal fat pads → Altering the natural cushioning of these fat pads
- Autonomic neuropathy:[8]
- Autonomic neuropathy leads to anhidrosis and impaired function of oil glands. The subsequent dryness of the skin results in a higher chance of skin breakdown, ulcer formation, and bacterial invasion.
- Autonomic neuropathy also decreases the proper peripheral sympathetic vascular tone which can lead to higher blood flow and pressure in distal arteries. The aforementioned changes plus capillary basement membrane destruction leads to edema. Edema itself increases the risk of ulcer formation.
- Sensory neuropathy:
- Appropriate sensory system helps patients to notice the tiniest fissures or blisters on their skin. This early sensation makes it possible for patients to take care of these skin defects and prevent further complications.
- Conversely, diabetic patients with sensory neuropathy are more prone to ulcer formation and related complications, since they don't feel pain with their ever-deepening ulcers.
- Motor nerve involvement:[6][7]
Ischemia
- Atherosclerosis:[9][10]
- Atherosclerosis of the lower limb is 2 to 3 times more common in diabetic patients, compared to the normal population.
- Investigators reported that atherosclerosis in diabetic patients is more prominent in tibial and fibular arteries of the calf, and arteries of the foot are relatively spared.
- It usually occurs due to inflammation and consequently leads to accumulation of the foam cells.
- Micro and macrovascular complications are one of the leading causes of diabetic complications. Microvascular complications cause skin damage, infection, and impaired wound healing.[11]
- The vascular changes which are responsible for foot problems include stiff arteries due to calcification of the smooth muscle cells in the arterial wall (mediasclerosis). Consequently, the stiff arteries are unable to expand in response to systolic pressure, which can lead to the movement of plaques in calf arteries.[12]
- Most of these changes are discovered by an impaired ankle brachial index (ABI).
- The resting ABI is the ratio of the blood pressure in the lower limb to the blood pressure of the arms. It is calculated by dividing the systolic blood pressure of the ankle by the systolic blood pressure of the arm.
- It is a non-invasive method to assess the lower extremty arterial system and to detect the presence of arterial occlusion disease.
- Even in the presence of neuropathic foot ulcers, the reason of non healing wounds could be due to impaired blood supply to the tissue, which could be further augmented by antihypertensive medications.[13].
Trauma
- Trauma to the foot is frequently the trigger of diabetic foot ulcer development, and repetitive trauma and pressure to the area prevent healing.[14]
- Excessive plantar pressure is related to limited joint mobility and foot deformities (such as charcot foot and hammer toe). Limited joint mobility and abnormal foot biomechanisms have been associated to an increased risk of ulceration.[13]
- Poor vision and sensory neuropathy further put diabetic patients at risk of foot ulceration, as they do not feel the pain, nor do they see the ulcer. Loss of balance can also make patients more susceptible to falls.[13]
Defective hypoxic response
- A transcription factor named hypoxia‐inducible factor‐1 (HIF‐1), which becomes stable in hypoxia, functions as a oxygen homeostasis regulator.[15]
- Since HIF‐1 helps cells to respond adequately to hypoxia (by regulating erythropoiesis, metabolic changes, angiogenesis, proliferation, migration, and cell survival), it plays a critical role in wound healing.[16]
- In addition, hypoxia‐inducible factor‐1 is responsible for the expression of genes that are critical to facilitate wound healing, such as the GLUT1 and GLUT3, lactate dehydrogenase, genes responsible for proper mitochondrial function (such as phosphoinositide‐dependent kinase‐1), type I collagen, and fibronectin. [17]
- There are numerous studies that detected lower levels of HIF‐1 in biopsies of diabetic foot. [18][19][20]
- One of the known pathogenesis of destabilized hypoxia‐inducible factor‐1 is hyperglycemia. This destabilization in hyperglycaemic conditions has been explained by an increase in the tendency of HIF‐1 towards VHL‐dependent degradation. [21]
Genetics
- Naturally growth factors and cytokines are two mediators involved in wound healing. It is crystal clear that any genetical changes that affect the aforementioned mediators can result in defective wound healing and higher chance of diabetic foot. The following are some known genetical changes:[22][23][24][25]
- A single nucleotide polymorphism (SNPs) is responsible in the variation of these growth factors and cytokines. The best known gene is MAPK14 located on chromosome 6.
- Decreased expression of certain cytokines and growth factors (such as IGF-1, TGF‐β1, PDGF, EGF, Interleukin 8, and Angiopoietin‐2)
- The HSPA1B genotype, a member of the heat shock protein 70 (Hsp70) family, has been related to a higher chance of diabetic foot development, amputation, and elongated hospital stay.[26]
Associated Conditions
Conditions associated with diabetic foot include:[27][28][29][30][31][32]
- Charcot arthropathy
- Peripheral arterial disease
- Psychosocial conditions, such as depression
- Necrotizing fasciitis (NF)
- Vitamin D deficiency
- Fungal infections, such as tinea pedis and onychomycosis
- Other complications of diabetes mellitus, such as diabetic retinopathy and nephropathy
- Hypertension
Gross Pathology


- On gross pathology, the most common site of ulceration is on the soles of the feet, under the metatarsal head (particularly at the second metatarsal head).
- Depth of ulcers could be different, ranging from superficial wounds to the involvement of ligaments and tendons, joint capsule, or deep fascia
- There is a high chance of concurrent anatomical foot deformities, such as claw toe or charcot joint.
- Presence of infective features of a ulcer, such as erythema, swelling, and purulent and malodor discharge.
- Abscess
- Gangrene
Microscopic Pathology
The following list is a summary of the possible microscopic histopathological changes of diabetic foot:[34][35][36]
- Skin necrosis
- Hyperkeratosis
- Fibrosis
- Inflammation
- Cellular debris
- Granulation tissue
- Biofilms formation, which resembles infection
- Angiogenesis, which represents proper wound healing
References
- ↑ Assal JP, Mehnert H, Tritschler HJ, Sidorenko A, Keen H, Hellmut Mehnert Award Workshop Participants (2002). "On your feet! Workshop on the diabetic foot". J Diabetes Complications. 16 (2): 183–94. PMID 12039404.
- ↑ Yazdanpanah L, Nasiri M, Adarvishi S (2015). "Literature review on the management of diabetic foot ulcer". World J Diabetes. 6 (1): 37–53. doi:10.4239/wjd.v6.i1.37. PMC 4317316. PMID 25685277.
- ↑ Lepäntalo, M.; Apelqvist, J.; Setacci, C.; Ricco, J.-B.; de Donato, G.; Becker, F.; Robert-Ebadi, H.; Cao, P.; Eckstein, H.H.; De Rango, P.; Diehm, N.; Schmidli, J.; Teraa, M.; Moll, F.L.; Dick, F.; Davies, A.H. (2011). "Chapter V: Diabetic Foot". European Journal of Vascular and Endovascular Surgery. 42: S60–S74. doi:10.1016/S1078-5884(11)60012-9. ISSN 1078-5884.
- ↑ Reiber GE, Vileikyte L, Boyko EJ, del Aguila M, Smith DG, Lavery LA; et al. (1999). "Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings". Diabetes Care. 22 (1): 157–62. doi:10.2337/diacare.22.1.157. PMID 10333919.
- ↑ Grunfeld C (1992). "Diabetic foot ulcers: etiology, treatment, and prevention". Adv Intern Med. 37: 103–32. PMID 1557993.
- ↑ Younger DS, Rosoklija G, Hays AP (1998). "Diabetic peripheral neuropathy". Semin Neurol. 18 (1): 95–104. doi:10.1055/s-2008-1040865. PMID 9562671.
- ↑ Borssén B, Bergenheim T, Lithner F (1990). "The epidemiology of foot lesions in diabetic patients aged 15-50 years". Diabet Med. 7 (5): 438–44. doi:10.1111/j.1464-5491.1990.tb01420.x. PMID 2142042.
- ↑ Ebenezer GJ, O'Donnell R, Hauer P, Cimino NP, McArthur JC, Polydefkis M (2011). "Impaired neurovascular repair in subjects with diabetes following experimental intracutaneous axotomy". Brain. 134 (Pt 6): 1853–63. doi:10.1093/brain/awr086. PMC 3140859. PMID 21616974.
- ↑ Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM (1998). "Preventive foot care in people with diabetes". Diabetes Care. 21 (12): 2161–77. doi:10.2337/diacare.21.12.2161. PMID 9839111.
- ↑ LoGerfo FW, Coffman JD (1984). "Current concepts. Vascular and microvascular disease of the foot in diabetes. Implications for foot care". N Engl J Med. 311 (25): 1615–9. doi:10.1056/NEJM198412203112506. PMID 6390204.
- ↑ Venermo M, Vikatmaa P, Terasaki H, Sugano N (2012). "Vascular laboratory for critical limb ischaemia". Scand J Surg. 101 (2): 86–93. doi:10.1177/145749691210100203. PMID 22623440.
- ↑ McMillan DE (1985). "Blood flow and the localization of atherosclerotic plaques". Stroke. 16 (4): 582–7. doi:10.1161/01.str.16.4.582. PMID 2411027.
- ↑ 13.0 13.1 13.2 Alexiadou K, Doupis J (2012). "Management of diabetic foot ulcers". Diabetes Ther. 3 (1): 4. doi:10.1007/s13300-012-0004-9. PMID 22529027.
- ↑ Noor S, Zubair M, Ahmad J (2015). "Diabetic foot ulcer--A review on pathophysiology, classification and microbial etiology". Diabetes Metab Syndr. 9 (3): 192–9. doi:10.1016/j.dsx.2015.04.007. PMID 25982677.
- ↑ Semenza GL (2012). "Hypoxia-inducible factors in physiology and medicine". Cell. 148 (3): 399–408. doi:10.1016/j.cell.2012.01.021. PMC 3437543. PMID 22304911.
- ↑ Semenza GL (2014). "Oxygen sensing, hypoxia-inducible factors, and disease pathophysiology". Annu Rev Pathol. 9: 47–71. doi:10.1146/annurev-pathol-012513-104720. PMID 23937437.
- ↑ Catrina SB, Zheng X (2016). "Disturbed hypoxic responses as a pathogenic mechanism of diabetic foot ulcers". Diabetes Metab Res Rev. 32 Suppl 1: 179–85. doi:10.1002/dmrr.2742. PMID 26453314.
- ↑ Botusan IR, Sunkari VG, Savu O, Catrina AI, Grünler J, Lindberg S; et al. (2008). "Stabilization of HIF-1alpha is critical to improve wound healing in diabetic mice". Proc Natl Acad Sci U S A. 105 (49): 19426–31. doi:10.1073/pnas.0805230105. PMC 2614777. PMID 19057015.
- ↑ Mace KA, Yu DH, Paydar KZ, Boudreau N, Young DM (2007). "Sustained expression of Hif-1alpha in the diabetic environment promotes angiogenesis and cutaneous wound repair". Wound Repair Regen. 15 (5): 636–45. doi:10.1111/j.1524-475X.2007.00278.x. PMID 17971009.
- ↑ Catrina SB, Okamoto K, Pereira T, Brismar K, Poellinger L (2004). "Hyperglycemia regulates hypoxia-inducible factor-1alpha protein stability and function". Diabetes. 53 (12): 3226–32. doi:10.2337/diabetes.53.12.3226. PMID 15561954.
- ↑ Bento CF, Fernandes R, Ramalho J, Marques C, Shang F, Taylor A; et al. (2010). "The chaperone-dependent ubiquitin ligase CHIP targets HIF-1α for degradation in the presence of methylglyoxal". PLoS One. 5 (11): e15062. doi:10.1371/journal.pone.0015062. PMC 2993942. PMID 21124777.
- ↑ Jhamb S, Vangaveti VN, Malabu UH (2016). "Genetic and molecular basis of diabetic foot ulcers: Clinical review". J Tissue Viability. 25 (4): 229–236. doi:10.1016/j.jtv.2016.06.005. PMID 27372176.
- ↑ Rafehi H, El-Osta A, Karagiannis TC (2011). "Genetic and epigenetic events in diabetic wound healing". Int Wound J. 8 (1): 12–21. doi:10.1111/j.1742-481X.2010.00745.x. PMID 21159125.
- ↑ Laato M, Kähäri VM, Niinikoski J, Vuorio E (1987). "Epidermal growth factor increases collagen production in granulation tissue by stimulation of fibroblast proliferation and not by activation of procollagen genes". Biochem J. 247 (2): 385–8. doi:10.1042/bj2470385. PMC 1148420. PMID 3501286.
- ↑ Singh K, Singh VK, Agrawal NK, Gupta SK, Singh K (2013). "Association of Toll-like receptor 4 polymorphisms with diabetic foot ulcers and application of artificial neural network in DFU risk assessment in type 2 diabetes patients". Biomed Res Int. 2013: 318686. doi:10.1155/2013/318686. PMC 3725976. PMID 23936790.
- ↑ Mir KA, Pugazhendhi S, Paul MJ, Nair A, Ramakrishna BS (2009). "Heat-shock protein 70 gene polymorphism is associated with the severity of diabetic foot ulcer and the outcome of surgical treatment". Br J Surg. 96 (10): 1205–9. doi:10.1002/bjs.6689. PMID 19731315.
- ↑ Vileikyte L, Pouwer F, Gonzalez JS (2020). "Psychosocial research in the diabetic foot: Are we making progress?". Diabetes Metab Res Rev. 36 Suppl 1: e3257. doi:10.1002/dmrr.3257. PMID 31850665.
- ↑ Williams LH, Rutter CM, Katon WJ, Reiber GE, Ciechanowski P, Heckbert SR; et al. (2010). "Depression and incident diabetic foot ulcers: a prospective cohort study". Am J Med. 123 (8): 748–754.e3. doi:10.1016/j.amjmed.2010.01.023. PMC 2913143. PMID 20670730.
- ↑ Iacopi E, Coppelli A, Goretti C, Piaggesi A (2015). "Necrotizing Fasciitis and The Diabetic Foot". Int J Low Extrem Wounds. 14 (4): 316–27. doi:10.1177/1534734615606534. PMID 26415868.
- ↑ Tiwari S, Pratyush DD, Gupta SK, Singh SK (2014). "Vitamin D deficiency is associated with inflammatory cytokine concentrations in patients with diabetic foot infection". Br J Nutr. 112 (12): 1938–43. doi:10.1017/S0007114514003018. PMID 25331710.
- ↑ Sellman A, Katzman P, Andreasson S, Löndahl M (2018). "Presence of chronic diabetic foot ulcers is associated with more frequent and more advanced retinopathy". Diabet Med. 35 (10): 1364–1370. doi:10.1111/dme.13682. PMID 29791040.
- ↑ Akkus G, Evran M, Gungor D, Karakas M, Sert M, Tetiker T (2016). "Tinea pedis and onychomycosis frequency in diabetes mellitus patients and diabetic foot ulcers. A cross sectional - observational study". Pak J Med Sci. 32 (4): 891–5. doi:10.12669/pjms.324.10027. PMC 5017097. PMID 27648034.
- ↑ Diabetic foot ulcer. Author: Milorad Dimic MD, Nis, Serbia, decembar 2011
- ↑ Neut D, Tijdens-Creusen EJ, Bulstra SK, van der Mei HC, Busscher HJ (2011). "Biofilms in chronic diabetic foot ulcers--a study of 2 cases". Acta Orthop. 82 (3): 383–5. doi:10.3109/17453674.2011.581265. PMC 3235322. PMID 21561305.
- ↑ Aragón-Sánchez FJ, Cabrera-Galván JJ, Quintana-Marrero Y, Hernández-Herrero MJ, Lázaro-Martínez JL, García-Morales E; et al. (2008). "Outcomes of surgical treatment of diabetic foot osteomyelitis: a series of 185 patients with histopathological confirmation of bone involvement". Diabetologia. 51 (11): 1962–70. doi:10.1007/s00125-008-1131-8. PMID 18719880.
- ↑ Piaggesi A, Viacava P, Rizzo L, Naccarato G, Baccetti F, Romanelli M; et al. (2003). "Semiquantitative analysis of the histopathological features of the neuropathic foot ulcer: effects of pressure relief". Diabetes Care. 26 (11): 3123–8. doi:10.2337/diacare.26.11.3123. PMID 14578249.