COVID-19-associated seizure
|
COVID-19 Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
COVID-19-associated seizure On the Web |
|
American Roentgen Ray Society Images of COVID-19-associated seizure |
|
Risk calculators and risk factors for COVID-19-associated seizure |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mandana Safakhah, MD[2] Tayebah Chaudhry[3] Syed Musadiq Ali M.B.B.S.[4]
Synonyms and keywords:
Overview
Seizure refers to an episode of symptoms due to abnormally excessive or synchronous neuronal activity in the brain followed by return to normal state. Seizures manifest as abnormal uncontrolled shaking movements that involve much of the body with loss of consciousness, shaking movements of part of the body with variable level of consciousness or a subtle momentary loss of consciousness. As COVID-19 (caused by SARS-Cov2) is now known to have several neurological complications, seizure is one of the complications seen in a few cases so far. Brain waive activity can be seen on EEG to confirm diagnosis since structural changes are very rarely seen on brain imaging. Anti-seizure medications are used for symptomatic treatment of seizure along with treatment of COVID-19.
Historical Perspective
- First case of seizure in COVID-19 patient was a result of meningitis/encephalitis caused by SARS-CoV2 and documented by Moriguchi et al in late February 2020 [1].
- After that, more cases were reported with acute seizures as a complication of COVID-19.[2][3]
- In early February 2020, seizurelike activity was reported in two COVID-19 patients but the cause was acute anxiety disorder and electrolyte imbalance instead of viral damage by SARS-Cov-2[4]
- To view the historical perspective of COVID-19, click here.
Classification
Pathophysiology
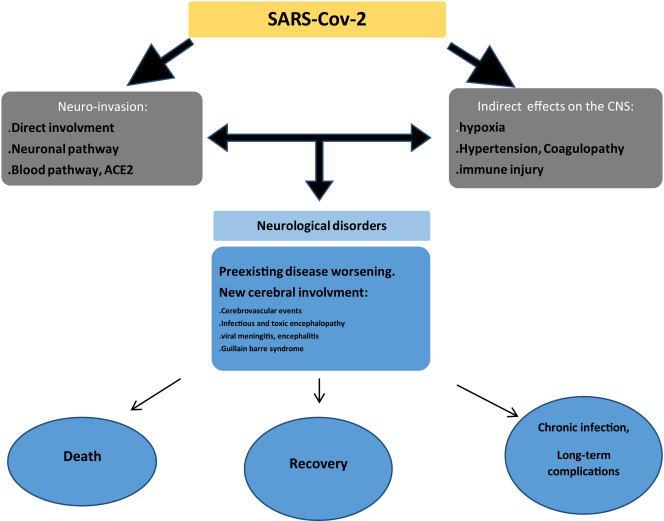
- Neurological complications caused by COVID-19 are through direct or indirect pathways.
- This includes hematogenous pathway, neuronal retrograde dissemination through olfactory bulb, entry into to glial cells and neurons via ACE2 receptor and impairment of gas exchange in lungs leading to anemia, hence increasing anaerobic metabolites in brain resulting in cellular and interstitial edema [5]
- Seizures in a patient with COVID-19 may be due to primary virus infection or due to reactivation of the latent virus.
- Infiltration of the brain tissue by the virus and subsequent production of toxins by the virus is one of the several mechanisms that can cause seizures in a COVID-19 patient. [6]
- Production of inflammatory mediators by the brain may also trigger seizures.
- Inflammatory cytokines that are released as a result of inflammatory cascade provoked by COVID-19 include interleukin 2,6,7, and 10, TNF-α and granulocyte colony-stimulating factor. Consequently, activation of glutamate receptors by the cytokines causes neuronal hyperexcitability and development of seizures. [6]
Causes
- Cause of COVID-19-associated seizure is viral infection by SARS-CoV-2 and its consequences which include:[7]
- Hypoxia
- Metabolic derangement
- Organ failure
- Cerebral damage.[8]
- To view causes of COVID-19, click here.
Differentiating COVID-19-associated seizure from other Diseases
- COVID-19-associated seizure must be differentiated from other diseases that cause collapse, abnormal movements or other seizure manifestations such as encephalitis, meningitis, stroke, tumor, brain hemorrhage, neurosyphilis, migraine, hypertensive encephalopathy, wernicke’s encephalopathy, abscess, and drug toxicity.[9][10][11]
| Diseases | Symptoms | Physical Examination | Past medical history | Diagnostic tests | Other Findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Headache | ↓LOC | Motor weakness | Abnormal sensory | Motor Deficit | Sensory deficit | Speech difficulty | Gait abnormality | Cranial nerves | CT /MRI | CSF Findings | Gold standard test | |||
| Meningitis | + | - | - | - | - | + | + | - | - | History of fever and malaise | - | ↑ Leukocytes,
↑ Protein ↓ Glucose |
CSF analysis[12] | Fever, neck |
| Encephalitis | + | + | +/- | +/- | - | - | + | +/- | + | History of fever and malaise | + | ↑ Leukocytes, ↓ Glucose | CSF PCR | Fever, seizures, focal neurologic abnormalities |
| Brain tumor[13] | + | - | - | - | + | + | + | - | + | Weight loss, fatigue | + | Cancer cells[14] | MRI | Cachexia, gradual progression of symptoms |
| Hemorrhagic stroke | + | + | + | + | + | + | + | + | - | Hypertension | + | - | CT scan without contrast[15][16] | Neck stiffness |
| Subdural hemorrhage | + | + | + | + | + | - | - | - | + | Trauma, fall | + | Xanthochromia[17] | CT scan without contrast[15][16] | Confusion, dizziness, nausea, vomiting |
| Neurosyphilis[18][19] | + | - | + | + | + | + | - | + | - | STIs | + | ↑ Leukocytes and protein | CSF VDRL-specifc
CSF FTA-Ab -sensitive[20] |
Blindness, confusion, depression,
Abnormal gait |
| Complex or atypical migraine | + | - | + | + | - | - | + | - | - | Family history of migraine | - | - | Clinical assesment | Presence of aura, nausea, vomiting |
| Hypertensive encephalopathy | + | + | - | - | - | - | + | + | - | Hypertension | + | - | Clinical assesment | Delirium, cortical blindness, cerebral edema, seizure |
| Wernicke’s encephalopathy | - | + | - | - | - | + | + | + | + | History of alcohal abuse | - | - | Clinical assesment and lab findings | Ophthalmoplegia, confusion |
| CNS abscess | + | + | - | - | + | + | + | - | - | History of drug abuse, endocarditis, immunosupression | + | ↑ leukocytes, ↓ glucose and ↑ protien | MRI is more sensitive and specific | High grade fever, fatigue,nausea, vomiting |
| Drug toxicity | - | + | - | + | + | + | - | + | - | - | - | - | Drug screen test | Lithium, Sedatives, phenytoin, carbamazepine |
| Conversion disorder | + | + | + | + | + | + | + | + | History of emotional stress | - | - | Diagnosis of exclusion | Tremors, blindness, difficulty swallowing | |
| Metabolic disturbances (electrolyte imbalance, hypoglycemia) | - | + | + | + | + | + | - | - | + | - | - | Hypoglycemia, hypo and hypernatremia, hypo and hyperkalemia | Depends on the cause | Confusion, seizure, palpitations, sweating, dizziness, hypoglycemia |
| Multiple sclerosis exacerbation | - | - | + | + | - | + | + | + | + | History of relapses and remissions | + | ↑ CSF IgG levels
(monoclonal bands) |
Clinical assesment and MRI [21] | Blurry vision, urinary incontinence, fatigue |
| Seizure | + | + | - | - | + | + | - | - | + | Previous history of seizures | - | Mass lesion | Clinical assesment and EEG [22] | Confusion, apathy, irritability, |
To view the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
- More data is required to comment on epidemiology and demographics of COVID-19-associated seizure.
- One study, specifically investigated the neurological manifestations of COVID-19 and documented CNS manifestations in 25% of the patients (headache (13%), dizziness (17%), impaired consciousness (8%), acute cerebrovascular problems (3%), ataxia (0.5), and seizures (0.5%)][23]
Risk Factors
- Several risk factors of seizure in COVID-19 patients were considered in a multicenter restrospective study from Jan 18th to FEb 18th, 2020 in China.[24]
- Risk factors that were studied include acute cerebrovascular disease, traumatic brain injury (TBI), central nervous system (CNS) infection, shock, hypoxia, severe metabolic disturbance, multiple‐organ dysfunction syndrome, sepsis, and exposure to drugs or toxic substances.
- According to the study, hypoxia and imipenem were shown to be important risk factors, among several others, for seizure in a COVID-19 patient.
- To view the risk factors of COVID-19, click here.
Screening
Natural History, Complications, and Prognosis
Natural History
- Seizure activity in a patient with or without COVID-19 usually lasts for a few seconds to less than 5 minutes with return to normal after the seizure episode.
- If seizure episode lasts for more than 5 minutes it is called status epilepticus.
- This is followed by a period of confusion, called postictal period that can last 3-15 minutes and sometimes hours.
Complications
- Complications of COVID-19-associated seizure include:
Prognosis
- In general, after the first seizure, subsequent seizure episodes can be predicted using EEG and brain imaging.[25]
- Prognosis of seizure in a COVID-19 patient is not known.
- However, if left untreated, seizure caused by acute brain event is known to have low risk of recurrence but higher risk of death compared to those with epilepsy. [26]
Diagnosis
Diagnostic Study of Choice
- The diagnosis of COVID-19-associated seizure is made through electroencephalogram (EEG, brain waive activity).[27]
- Other diagnostic tests include:
- CT scan brain
- MRI brain
- Blood test
- Lumbar puncture
- Toxicology screening
Symptoms
- Symptoms of COVID-19-associated seizure in a patient include:
- Staring
- Jerking movements of the arms and legs
- Stiffening of the body
- Loss of consciousness
- Breathing problems
- Loss of bowel or bladder control
- Falling suddenly for no apparent reason, especially when associated with loss of consciousness
- Not responding to noise or words for brief periods
- Appearing confused or in a haze
- Nodding of head rhythmically, associated with lack of awareness
- Periods of rapid eye blinking
Physical Examination
- physical examination of a patient with COVID-19-associated seizure include:
- Vital signs: Tachycardia may be present.
- Postictal drowsiness or confusion.
- Finding a bite to the side of the tongue (when present, is helpful in making the diagnosis).
Laboratory Findings
- Postictal levels of the following may be elevated in a patient with seizures:
- Prolactin (within 20 minutes after a convulsive event)
- Lactate (within 1 to 2 hours)
- Ammonia (within several hours)
- Creatine kinase (especially 24 to 48 hours postictally)
- To view the laboratory findings on COVID-19, click here.
Electrocardiogram
- There are no typical ECG findings associated with seizures in a COVID-19 patient.
- To view the electrocardiogram findings on COVID-19, click here.
X-ray
- There are no x-ray findings associated with COVID-19 associated seizure.
- To view the x-ray finidings on COVID-19, click here.
Echocardiography or Ultrasound
- There are no typical echocardiographic findings for seizure related to COVID-19.
- To view the echocardiographic findings on COVID-19, click here.
CT scan
- CT brain may show structural lesions but majority of patients will show nothing.
- To view the CT scan findings on COVID-19, click here.
MRI
- MRI brain may show structural lesions but majority of patients will show nothing.
- To view the MRI findings on COVID-19, click here.
Other Imaging Findings
- There are no other imaging findings associated with seizure related to COVID-19.
- To view other imaging findings on COVID-19, click here.
Other Diagnostic Studies
- To view other diagnostic studies for COVID-19, click here.
Treatment
Medical Therapy
- Development of seizures in a COVID-19 patient requires urgent treatment.
- After the cause of seizure is determined, medical therapy should be aimed at treating the cause immediately (for example, hypoxia, fever, metabolic imbalance).
- Anti-seizure medication (ASM) is often necessary.
- Anti-epileptics therapy with mannitol has been documented in decreasing cerebral edema[28].
- For a single seizure less than 5 min rescue treatment with benzodiazepine is not needed.
- Intravenous ASM are used with caution in COVID-19 patients due to the adverse effects (e.g., Phenytoin, Phenobarbital and Lacosamide in respiratory and cardiac problems) and drug interactions (e.g., Carbamazepine, Phenytoin, Phenobarbital and Valproic acid). [7]
- Brivaracetam and Levetiracetam have less adverse effects and drug interactions. [7]
- In patients with more than one seizure (either shorter or longer than 5 min) and in status epilepticus rescue treatment with benzodiazepines in addition to ASM is needed. [7]
Surgery
Surgical intervention is not recommended for the management of COVID-19 associated seizure.
Primary Prevention
There are no established measures for the primary prevention of seizures associated with COVID-19.
Secondary Prevention
There are no established measures for the secondary prevention of seizures associated with COVID-19.
References
- ↑ Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Ueno M, Sakata H, Kondo K, Myose N, Nakao A, Takeda M, Haro H, Inoue O, Suzuki-Inoue K, Kubokawa K, Ogihara S, Sasaki T, Kinouchi H, Kojin H, Ito M, Onishi H, Shimizu T, Sasaki Y, Enomoto N, Ishihara H, Furuya S, Yamamoto T, Shimada S (May 2020). "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2". Int. J. Infect. Dis. 94: 55–58. doi:10.1016/j.ijid.2020.03.062. PMC 7195378 Check
|pmc=value (help). PMID 32251791 Check|pmid=value (help). - ↑ Template:Citejournal
- ↑ {{https://www.sciencedirect.com/science/article/pii/S1059131120301151}}
- ↑ {{https://onlinelibrary.wiley.com/doi/full/10.1111/epi.16524}}
- ↑ {{https://pubmed.ncbi.nlm.nih.gov/32458193/}}
- ↑ 6.0 6.1 Karimi, Narges; Sharifi Razavi, Athena; Rouhani, Nima (2020). "Frequent Convulsive Seizures in an Adult Patient with COVID-19: A Case Report". Iranian Red Crescent Medical Journal. 22 (3). doi:10.5812/ircmj.102828. ISSN 2074-1804.
- ↑ 7.0 7.1 7.2 7.3 Asadi-Pooya AA (July 2020). "Seizures associated with coronavirus infections". Seizure. 79: 49–52. doi:10.1016/j.seizure.2020.05.005. PMC 7212943 Check
|pmc=value (help). PMID 32416567 Check|pmid=value (help). - ↑ {{https://www.ncbi.nlm.nih.gov/books/NBK430765/}}
- ↑ Sohal S, Mossammat M (May 2020). "COVID-19 Presenting with Seizures". IDCases: e00782. doi:10.1016/j.idcr.2020.e00782. PMC 7194035 Check
|pmc=value (help). PMID 32363146 Check|pmid=value (help). - ↑ Bohmwald K, Gálvez N, Ríos M, Kalergis AM (2018). "Neurologic Alterations Due to Respiratory Virus Infections". Front Cell Neurosci. 12: 386. doi:10.3389/fncel.2018.00386. PMC 6212673. PMID 30416428. Vancouver style error: initials (help)
- ↑ Tsivgoulis G, Palaiodimou L, Katsanos AH, Caso V, Köhrmann M, Molina C, Cordonnier C, Fischer U, Kelly P, Sharma VK, Chan AC, Zand R, Sarraj A, Schellinger PD, Voumvourakis KI, Grigoriadis N, Alexandrov AV, Tsiodras S (2020). "Neurological manifestations and implications of COVID-19 pandemic". Ther Adv Neurol Disord. 13: 1756286420932036. doi:10.1177/1756286420932036. PMC 7284455 Check
|pmc=value (help). PMID 32565914 Check|pmid=value (help). - ↑ Carbonnelle E (2009). "[Laboratory diagnosis of bacterial meningitis: usefulness of various tests for the determination of the etiological agent]". Med Mal Infect. 39 (7–8): 581–605. doi:10.1016/j.medmal.2009.02.017. PMID 19398286.
- ↑ Morgenstern LB, Frankowski RF (1999). "Brain tumor masquerading as stroke". J Neurooncol. 44 (1): 47–52. PMID 10582668.
- ↑ Weston CL, Glantz MJ, Connor JR (2011). "Detection of cancer cells in the cerebrospinal fluid: current methods and future directions". Fluids Barriers CNS. 8 (1): 14. doi:10.1186/2045-8118-8-14. PMC 3059292. PMID 21371327.
- ↑ 15.0 15.1 Birenbaum D, Bancroft LW, Felsberg GJ (2011). "Imaging in acute stroke". West J Emerg Med. 12 (1): 67–76. PMC 3088377. PMID 21694755.
- ↑ 16.0 16.1 DeLaPaz RL, Wippold FJ, Cornelius RS, Amin-Hanjani S, Angtuaco EJ, Broderick DF; et al. (2011). "ACR Appropriateness Criteria® on cerebrovascular disease". J Am Coll Radiol. 8 (8): 532–8. doi:10.1016/j.jacr.2011.05.010. PMID 21807345.
- ↑ Lee MC, Heaney LM, Jacobson RL, Klassen AC (1975). "Cerebrospinal fluid in cerebral hemorrhage and infarction". Stroke. 6 (6): 638–41. PMID 1198628.
- ↑ Liu LL, Zheng WH, Tong ML, Liu GL, Zhang HL, Fu ZG; et al. (2012). "Ischemic stroke as a primary symptom of neurosyphilis among HIV-negative emergency patients". J Neurol Sci. 317 (1–2): 35–9. doi:10.1016/j.jns.2012.03.003. PMID 22482824.
- ↑ Berger JR, Dean D (2014). "Neurosyphilis". Handb Clin Neurol. 121: 1461–72. doi:10.1016/B978-0-7020-4088-7.00098-5. PMID 24365430.
- ↑ Ho EL, Marra CM (2012). "Treponemal tests for neurosyphilis--less accurate than what we thought?". Sex Transm Dis. 39 (4): 298–9. doi:10.1097/OLQ.0b013e31824ee574. PMC 3746559. PMID 22421697.
- ↑ Giang DW, Grow VM, Mooney C, Mushlin AI, Goodman AD, Mattson DH; et al. (1994). "Clinical diagnosis of multiple sclerosis. The impact of magnetic resonance imaging and ancillary testing. Rochester-Toronto Magnetic Resonance Study Group". Arch Neurol. 51 (1): 61–6. PMID 8274111.
- ↑ Manford M (2001). "Assessment and investigation of possible epileptic seizures". J Neurol Neurosurg Psychiatry. 70 Suppl 2: II3–8. PMC 1765557. PMID 11385043.
- ↑ Mao, Ling; Jin, Huijuan; Wang, Mengdie; Hu, Yu; Chen, Shengcai; He, Quanwei; Chang, Jiang; Hong, Candong; Zhou, Yifan; Wang, David; Miao, Xiaoping; Li, Yanan; Hu, Bo (2020). "Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China". JAMA Neurology. 77 (6): 683. doi:10.1001/jamaneurol.2020.1127. ISSN 2168-6149.
- ↑ {{https://onlinelibrary.wiley.com/doi/full/10.1111/epi.16524}}
- ↑ Wilden JA, Cohen-Gadol AA (August 2012). "Evaluation of first nonfebrile seizures". Am Fam Physician. 86 (4): 334–40. PMID 22963022.
- ↑ Sander JW, Shorvon SD (November 1996). "Epidemiology of the epilepsies". J. Neurol. Neurosurg. Psychiatry. 61 (5): 433–43. doi:10.1136/jnnp.61.5.433. PMC 1074036. PMID 8965090.
- ↑ Haines S, Caccamo A, Chan F, Galaso G, Catinchi A, Gupta PK (2020). "Practical Considerations When Performing Neurodiagnostic Studies on Patients with COVID-19 and Other Highly Virulent Diseases". Neurodiagn J. 60 (2): 78–95. doi:10.1080/21646821.2020.1756132. PMC 7212538 Check
|pmc=value (help). PMID 32374647 Check|pmid=value (help). - ↑ Ye M, Ren Y, Lv T (April 2020). "Encephalitis as a clinical manifestation of COVID-19". Brain Behav. Immun. doi:10.1016/j.bbi.2020.04.017. PMC 7146652 Check
|pmc=value (help). PMID 32283294 Check|pmid=value (help).