Wide complex tachycardia differential diagnosis
| Resident Survival Guide |
| File:Physician Extender Algorithms.gif |
|
Wide complex tachycardia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Wide complex tachycardia differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Wide complex tachycardia differential diagnosis |
|
Risk calculators and risk factors for Wide complex tachycardia differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby, M.D. [2] Syed Hassan A. Kazmi BSc, MD [3]
Overview
When wide QRS tachycardia is present on the electrocardiogram ECG, it is necessary to rapidly differentiate whether it is caused by ventricular tachycardia (VT) or a supraventricular tachycardia (SVT) with aberrant conduction. While the EKG provides the most reliable data to distinguish VT from SVT with aberrant conduction, the clinical history and the age of the patient may also provide additional discriminatory information regarding the cause of the wide QRS tachycardia. While older patients with a prior history of myocardial infarction are more likely to have VT, young hemodynamically stable patients presenting with paroxysmal tachycardia are more likely to have SVT with aberrant conduction. Nevertheless, the primary tool to differentiate VT from SVT with aberrant conduction is the ECG. There are several findings that are more common in ventricular tachycardia, and there are also more sophisticated electrophysiologic algorithms such as the Brugada and Vereckei algorithms that can be used to distinguish VT from SVT with aberrant conduction. The diagnosis of VT is more likely if: There is a history of myocardial infarction or structural heart disease, the electrical axis is -90 to -180 degrees (a “northwest” or “superior” axis), the QRS is > 140 msec, there is AV dissociation, there are positive or negative QRS complexes in all the precordial leads, and the morphology of the QRS complexes resembles that of a previous premature ventricular contraction (PVC).
History of Ischemic Heart Disease
Risk factors for the ventricular tachycardia as a cause of wide complex tachycardia include a history of prior myocardial infarction, a history of congestive heart failure, and a history of recent angina pectoris. These three historical features have positive predictive values for VT of > 95% in a small study, but sensitivities of 66%, 24%, and 24%, respectively.[1] Wide complex tachycardia will be due to VT in 98% of cases if there's a history of structural heart disease. Only 7% of patients with SVT with aberrancy will have had a prior myocardial infarction (MI).[2]
Hemodynamic Stability
Hemodynamic stability does not reliably differentiate VT from SVT. Patients with ventricular tachycardia can often be hemodynamically stable, and stable vital signs do not rule out ventricular tachycardia. This is often a major mistake on the part of clinicians and can lead to inappropriate treatment of VT as SVT with poor outcomes. [3]
EKG Findings Suggestive of VT
The Presence of AV Dissociation
Although AV dissociation is highly suggestive of VT, it may also be seen in junctional tachycardias with retrograde block.
Example: Shown below is a wide complex tachycardia. AV dissociation is present as shown by the varying morphology highlighted by the red arrows. LBBB configuration. Absence of RS in the chest leads. The diagnosis is VT.
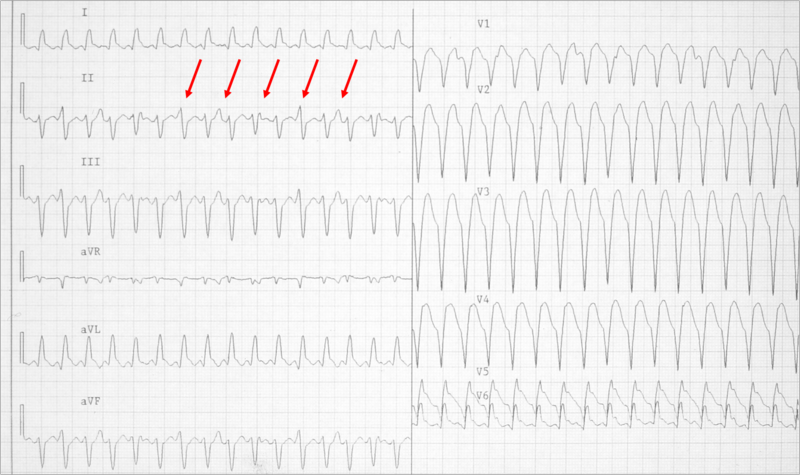
Example: Shown below is a wide complex tachycardia. AV dissociation is present as shown by the varying morphology highlighted by the red arrows. LBBB configuration. Absence of RS in the chest leads. The diagnosis is VT.

Duration of the QRS Complex
- A wide complex tachycardia with a RBBB morphology and a QRS > 0.14, or a LBBB morphology with a QRS > 0.16 suggests VT.
Morphology of the QRS Complexes
- The finding of a positive or negative QRS complex in all precordial leads is in favor of ventricular tachycardia.
- A monophasic or biphasic RBBB QRS complex in V1. But none of their patients with SVT had a preexisting RBBB. Therefore, this finding is of limited importance (A Wellens criterion).
- 80 to 85% of aberrant beats have a RBBB pattern, but ectopic beats that arise from the LV have a similar morphology.
- LBBB with a rightward axis
- LBBB with the following QRS morphology:
- R wave in V1 or V2 > 0.03 second
- Any Q wave in V6
- Onset of the QRS to nadir of the S wave in V1 > 0.06 seconds
- Notching of the S wave in V1 or V2
| Morphological criteria | ||
|---|---|---|
| LBBB pattern | ||
| Initial R more than 40 ms? | Yes ≥ VT |  |
| Slurred or notched downwards leg of S wave in leads V1 or V2? | Yes ≥ VT | |
| Beginning of Q to nadir QS > 60 ms in V1 or V2? | Yes ≥ VT | LR > 50:1 |
| Q or QS in V6? | Yes ≥ VT | LR > 50:1 |
 | ||
| RBBB pattern | ||
| Monophasic R or qR in V1? | Yes ≥ VT | |
| R taller than R' (rabbit-ear sign)? | Yes ≥ VT | LR > 50:1 |
| rS in V6? | Yes ≥ VT | LR > 50:1 |
Morphology of Premature Beats During Sinus Rhythm
- If premature ventricular contractions (PVCs) are present on a prior tracing, and if the morphology of the wide complex tachycardia is the same, then it is likely to be ventricular tachycardia.
- Previous EKG may show a preexisting intraventricular conduction delay (IVCD) which would favor SVT with abberancy.
- If there are premature atrial contractions (PAC)s with aberrant conduction, then the origin of the wide complex tachycardia may be supraventricular.
- Example: Shown below is a wide complex tachycardia. There is no AV dissociation. A RBBB morphology is present. The wide complex tachycardia resembles sinus rhythm from the same patient. The diagnosis in this patient is SVT with RBBB:

- Shown below is the ECG from the same patient as above in sinus rhythm. The QRS complex is very similiar to that during the wide complex tachycardia:

The QRS Axis
- A "northwest axis" with a QRS axis in the RUQ between -90 and +180 degrees favors ventricular tachycardia.
- The image below illustrates the "Northwest axis"also known as "Extreme Right Axis" or "No Man's Land":

Capture Beats
- Rare, but one of the strongest pieces of evidence in favor of VT.
- SVT with aberrancy rarely follows a beat with a short cycle length.
Fusion Beats
- Fusion beats are rare, but strongly suggests VT.

Vagal Manuevers
- VT is generally not affected by vagal stimulation.
- May terminate reentrant arrhythmias
Atrial Pacing
- A pacing wire is placed in the RA and the atrium is stimulated at a rate faster than the tachycardia.
- If ventricular capture occurs and the QRS is normal in duration, then one can exclude the possibility of aberrant conduction.
Onset of the Tachycardia
- Diagnosis of SVT made if the episode is initiated by a premature P wave.
- If the paroxysm begins with a QRS then the tachycardia may be either ventricular or junctional in origin.
- If the first QRS of the tachycardia is preceded by a sinus p wave with a PR interval shorter than that of the conducted sinus beats, the tachycardia is ventricular.
His Bundle Recording
- In SVT, each QRS is preceded by a His bundle potential.
- In VT there is no preceding His deflection.
- The retrograde His deflection is usually obscured by the much larger QRS complex.
Regularity of the Rhythm
Regular
- VT (slight irregularity of RR)
- SVT with aberrancy: Sinus, atrial tachycardia (AT), or flutter
- Antidromic atrioventricular reentrant tachycardia (AVRT)
Irregular
- The first 50 beats of VT can be irregular
- SVT with aberrancy: Atrial fibrillation, multifocal atrial tachycardia (MAT)
- Atrial fibrillation with bypass tract usch as WPW is a dangerous cause of a very rapid irregular rhythm as the atrial rate is conducted rapidly over the bypass tract. Shown below is the tracing of a patient with atrial fibrillation conducting down the bypass tract in WPW. Note that the rate is extremely rapid, and the rhythm is irregularly irregular. It is critical that this rhythm be recognized to avoid the administration of agents that would further accelerate conduction down the accessory pathway in this patient with WPW which could cause degeneration into ventricular fibrillation. The best treatment for this patient is Pronestyl 15 mg/kg load over 30 minutes then 2-6 mg/min gtt or DC cardioversion:

- The mechanism of SVT with aberrancy is usually concealed retrograde conduction. The ventricular beat penetrates the right branch (RB) or left branch (LB). When the next supraventricular activation front occurs that bundle is refractory and if conduction can occur, it will proceed down the other bundle. Since the RB has a longer refractory period than the LB, a right bundle branch block (RBBB) morphology is more common.
- Other mechanisms of “rate related aberrancy” are preexisting bundle branch block (BBB), physiologic (phase 3) aberration and use dependent aberration secondary to medication. In physiologic aberration, the stimulus comes to the His-Purkinje system before it has fully recovered from the previous stimulus. The ensuing activation is either blocked or conducts slowly. Again, the RB is the one more at risk. Most commonly seen at the onset of paroxysmal supraventricular tachycardia (PSVT), but can become sustained.
- In use-dependent aberration, a patient on and anti-arrhythmic (especially class Ic agents) will have a progressive decrement in ventricular conduction rate the more it is stimulated. During faster heart rates, less time is available for the drug to dissociate from the receptor and an increased number of receptors are blocked.
Sophisticated Electrophysiologic Criteria
Several ECG criteria and algorithms have been used to differentiate VT and SVT, the common one of which is Brugada algorithm. Below is a list of all algorithms:
- Brugada algorithm: sensitivity 89%, specificity 59.2%[4]
- The lead II R-wave-peak-time: sensitivity 60%, specificity 82.7%[5]
- The aVR algorithm: sensitivity 87.1%, specificity 48%[6]
- The Bayesian algorithm: sensitivity 89%, specificity 52%[7]
- The Griffith algorithm: sensitivity 94.2%, specificity 39.8%[8]
The R Wave Peak Time
In 2010 Joseph Brugada et al. published a new criterion to differentiate VT from SVT in wide complex tachycardias: the R wave peak time (RWPT) in Lead II.[5] To aplly the criteria, the duration of onset of the QRS to the first change in polarity (either nadir Q or peak R) is measured in lead II as shown below. If the RWPT is ≥ 50ms the likelihood of a VT very high (positive likelihood ratio 34.8). This criterion was successful in their own population of 163 selected patients and is awaiting prospective testing in a larger trial.
Example: As shown below, an R-wave to Peak Time (RWPT) of ≥ 50ms in lead II strongly suggests VT:

Brugada Criteria[9]
| Absence of an RS complex in all precordial leads? | Yes? VT (SN=0.21 SP=1.0) | ||||||||||||||||||||||||||||||||||||||||
| No? | |||||||||||||||||||||||||||||||||||||||||
| R to S interval>100 ms in one precordial lead? | Yes? VT (SN=0.66 SP=0.98) | ||||||||||||||||||||||||||||||||||||||||
| No? | |||||||||||||||||||||||||||||||||||||||||
| AV dissociation? | Yes? VT (SN=0.82 SP=0.98) | ||||||||||||||||||||||||||||||||||||||||
| No? | |||||||||||||||||||||||||||||||||||||||||
| Morphology criteria for VT present both in precordial leads V1, V2 and V6? | Yes? VT (SN=0.987 SP=0.965) | ||||||||||||||||||||||||||||||||||||||||
| No? | |||||||||||||||||||||||||||||||||||||||||
| SVT (SN=0.965 SP=0.987) | |||||||||||||||||||||||||||||||||||||||||
Based on the 2011 Nature Reviews Cardiology algorithm of broad complex tachycardia.[10]
Vereckei Criteria[11]
- An algorithm has been proposed by Vereckei and colleagues, wherein in addition to do the traditional criteria, the voltage change on the EKG is used as a final discriminatory criteria.
- In this method, the voltage change during the initial 40 ms (Vi) and the terminal 40 ms (Vt) of the same QRS complex is used to estimate the (Vi) and terminal (Vt) ventricular activation velocity ratio (Vi/Vt).
- A Vi/Vt > 1 suggests SVT and a Vi/Vt ≤ 1 suggests VT.[6]
| AV dissociation present? | Yes? VT | ||||||||||||||||||||||||||||||||||||||||
| No? | |||||||||||||||||||||||||||||||||||||||||
| Initial R wave in aVR present? | Yes? VT | ||||||||||||||||||||||||||||||||||||||||
| No? | |||||||||||||||||||||||||||||||||||||||||
| QRS morphology unlike BBB or FB? | Yes? VT | ||||||||||||||||||||||||||||||||||||||||
| No? | |||||||||||||||||||||||||||||||||||||||||
| Vi/Vt≤1? | Yes? VT | ||||||||||||||||||||||||||||||||||||||||
| No? | |||||||||||||||||||||||||||||||||||||||||
| SVT | |||||||||||||||||||||||||||||||||||||||||
Based on the 2011 Nature Reviews Cardiology algorithm of broad complex tachycardia.[12]
Calculation of Vi/Vt
Shown below is an image demonstrating the method used to calculate Vi/Vt. In this tracing, Vi/Vt is < 1 is suggestive of ventricular tachycardia according to Vereckei criteria.

Pacemaker Mediated Tachycardia
Pacer spikes are present. There is a ventricular-paced rhythm at or near the upper rate limit at approximately 120-130 beats per minute. Given the mechanical nature of the trigger, the EKG is absolutely regular.
Shown below is a rhythm strip demonstrating pacemaker mediated tachycardia:

Putting It All Together: The ACC Algorithm
| Wide QRS complex tachycardia (QRS duration greater than 120 ms) | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Regular or irregular? | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Regular | Irregular | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Is QRS identical to that during SR? If yes, consider: - SVT and BBB - Antidromic AVRT | Atrial fibrillation Atrial flutter / AT with variable conduction and: a) BBB or b) Antegrade conduction via AP | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Vagal maneuvers or adenosine | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Previous myocardial infarction or structural heart disease? If yes, VT is likely. | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 to 1 AV relationship? | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes or unknown | No | ||||||||||||||||||||||||||||||||||||||||||||||||||
| V rate faster than A rate | A rate faster than V rate | ||||||||||||||||||||||||||||||||||||||||||||||||||
| QRS morphology in precordial leads | VT | Atrial tachycardia Atrial flutter | |||||||||||||||||||||||||||||||||||||||||||||||||
| Typical RBBB or LBBB | Precordial leads: - Concordant - No R/S pattern - Onset of R to nadir longer than 100ms | RBBB pattern: - qR, Rs or Rr' in V1 - Frontal plane axis range from +90 degrees to -90 degrees | LBBB pattern: - R in V1 longer than 30 ms - R to nadir of S in V1 greater than 60 ms - qR or qS in V6 | ||||||||||||||||||||||||||||||||||||||||||||||||
| SVT | VT | VT | VT | ||||||||||||||||||||||||||||||||||||||||||||||||
The above algorithm is adapted from the 2003 American College of Cardiology.[13]
Response to Pharmacotherapy As a Diagnostic Tool to Differentiate the VT from SVT
Although termination of a wide complex tachycardia by either adenosine, a calcium channel blocker, a beta blocker or digoxin is suggestive of supraventricular tachycardia with aberrant conduction, VT can also be terminated by these pharmacotherapies.[14][15] Verapamil should be avoided in patients with wide complex tachycardia as it can result in hemodynamic deterioration in patients with ventricular tachycardia.[16]
Differentiating Ventricular Tachycardia From Other Diseases
| Arrhythmia | Rhythm | Rate | P wave | PR Interval | QRS Complex | Response to Maneuvers | Epidemiology | Co-existing Conditions |
|---|---|---|---|---|---|---|---|---|
| Atrial Fibrillation (AFib)[17][18] |
|
|
|
|
|
|
|
|
| Atrial Flutter[19] |
|
|
|
|
|
|
|
|
| Atrioventricular nodal reentry tachycardia (AVNRT)[20][21][22][23] |
|
|
|
|
|
|
|
|
| Multifocal Atrial Tachycardia[24][25] |
|
|
|
|
|
|
|
|
| Paroxysmal Supraventricular Tachycardia |
|
|
|
|
|
|
|
|
| Premature Atrial Contractrions (PAC)[26][27] |
|
|
|
|
|
|
||
| Wolff-Parkinson-White Syndrome[28][29] |
|
|
|
|
|
|
|
|
| Ventricular Fibrillation (VF)[30][31][32] |
|
|
|
|
|
|
|
|
| Ventricular Tachycardia[33][34] |
|
|
|
|
|
|
|
|
References
- ↑ Baerman JM, Morady F, DiCarlo LA, de Buitleir M (1987). "Differentiation of ventricular tachycardia from supraventricular tachycardia with aberration: value of the clinical history". Annals of Emergency Medicine. 16 (1): 40–3. PMID 3800075. Retrieved 2013-08-04. Unknown parameter
|month=ignored (help) - ↑ http://en.ecgpedia.org/wiki/Approach_to_the_Wide_Complex_Tachycardia
- ↑ Morady F, Baerman JM, DiCarlo LA, DeBuitleir M, Krol RB, Wahr DW (1985). "A prevalent misconception regarding wide-complex tachycardias". JAMA : the Journal of the American Medical Association. 254 (19): 2790–2. PMID 4057488. Retrieved 2013-08-04. Unknown parameter
|month=ignored (help) - ↑ Brugada P, Brugada J, Mont L, Smeets J, Andries EW (1991). "A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex". Circulation. 83 (5): 1649–59. PMID 2022022.
- ↑ 5.0 5.1 Pava LF, Perafán P, Badiel M, Arango JJ, Mont L, Morillo CA; et al. (2010). "R-wave peak time at DII: a new criterion for differentiating between wide complex QRS tachycardias". Heart Rhythm. 7 (7): 922–6. doi:10.1016/j.hrthm.2010.03.001. PMID 20215043.
- ↑ 6.0 6.1 Vereckei A, Duray G, Szénási G, Altemose GT, Miller JM (2007). "Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia". Eur Heart J. 28 (5): 589–600. doi:10.1093/eurheartj/ehl473. PMID 17272358.
- ↑ Lau EW, Pathamanathan RK, Ng GA, Cooper J, Skehan JD, Griffith MJ (2000). "The Bayesian approach improves the electrocardiographic diagnosis of broad complex tachycardia". Pacing Clin Electrophysiol. 23 (10 Pt 1): 1519–26. PMID 11060873.
- ↑ Griffith MJ, Garratt CJ, Mounsey P, Camm AJ (1994). "Ventricular tachycardia as default diagnosis in broad complex tachycardia". Lancet. 343 (8894): 386–8. PMID 7905552.
- ↑ Brugada, P.; Brugada, J.; Mont, L.; Smeets, J.; Andries, EW. (1991). "A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex". Circulation. 83 (5): 1649–59. PMID 2022022. Unknown parameter
|month=ignored (help) - ↑ Kurt C. Roberts-Thomson, Dennis H. Lau & Prashanthan Sanders. The diagnosis and management of ventricular arrhythmias. Nature Reviews Cardiology 8, 311-321.
- ↑ Vereckei, A.; Duray, G.; Szénási, G.; Altemose, GT.; Miller, JM. (2008). "New algorithm using only lead aVR for differential diagnosis of wide QRS complex tachycardia". Heart Rhythm. 5 (1): 89–98. doi:10.1016/j.hrthm.2007.09.020. PMID 18180024. Unknown parameter
|month=ignored (help) - ↑ Kurt C. Roberts-Thomson, Dennis H. Lau & Prashanthan Sanders. The diagnosis and management of ventricular arrhythmias. Nature Reviews Cardiology 8, 311-321.
- ↑ Blomström-Lundqvist C, Scheinman MM, Aliot EM, Alpert JS, Calkins H, Camm AJ; et al. (2003). "ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias--executive summary. a report of the American college of cardiology/American heart association task force on practice guidelines and the European society of cardiology committee for practice guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society". J Am Coll Cardiol. 42 (8): 1493–531. PMID 14563598.
- ↑ Lerman BB, Belardinelli L, West GA, Berne RM, DiMarco JP (1986). "Adenosine-sensitive ventricular tachycardia: evidence suggesting cyclic AMP-mediated triggered activity". Circulation. 74 (2): 270–80. PMID 3015453. Retrieved 2013-08-04. Unknown parameter
|month=ignored (help) - ↑ Belhassen B, Rotmensch HH, Laniado S (1981). "Response of recurrent sustained ventricular tachycardia to verapamil". British Heart Journal. 46 (6): 679–82. PMC 482717. PMID 7317238. Retrieved 2013-08-04. Unknown parameter
|month=ignored (help) - ↑ Buxton AE, Marchlinski FE, Doherty JU, Flores B, Josephson ME (1987). "Hazards of intravenous verapamil for sustained ventricular tachycardia". The American Journal of Cardiology. 59 (12): 1107–10. PMID 3578051. Retrieved 2013-08-04. Unknown parameter
|month=ignored (help) - ↑ Lankveld TA, Zeemering S, Crijns HJ, Schotten U (July 2014). "The ECG as a tool to determine atrial fibrillation complexity". Heart. 100 (14): 1077–84. doi:10.1136/heartjnl-2013-305149. PMID 24837984.
- ↑ Harris K, Edwards D, Mant J (2012). "How can we best detect atrial fibrillation?". J R Coll Physicians Edinb. 42 Suppl 18: 5–22. doi:10.4997/JRCPE.2012.S02. PMID 22518390.
- ↑ Cosío FG (June 2017). "Atrial Flutter, Typical and Atypical: A Review". Arrhythm Electrophysiol Rev. 6 (2): 55–62. doi:10.15420/aer.2017.5.2. PMC 5522718. PMID 28835836.
- ↑ Katritsis DG, Josephson ME (August 2016). "Classification, Electrophysiological Features and Therapy of Atrioventricular Nodal Reentrant Tachycardia". Arrhythm Electrophysiol Rev. 5 (2): 130–5. doi:10.15420/AER.2016.18.2. PMC 5013176. PMID 27617092.
- ↑ Letsas KP, Weber R, Siklody CH, Mihas CC, Stockinger J, Blum T, Kalusche D, Arentz T (April 2010). "Electrocardiographic differentiation of common type atrioventricular nodal reentrant tachycardia from atrioventricular reciprocating tachycardia via a concealed accessory pathway". Acta Cardiol. 65 (2): 171–6. doi:10.2143/AC.65.2.2047050. PMID 20458824.
- ↑ "Atrioventricular Nodal Reentry Tachycardia (AVNRT) - StatPearls - NCBI Bookshelf".
- ↑ Schernthaner C, Danmayr F, Strohmer B (2014). "Coexistence of atrioventricular nodal reentrant tachycardia with other forms of arrhythmias". Med Princ Pract. 23 (6): 543–50. doi:10.1159/000365418. PMC 5586929. PMID 25196716.
- ↑ Scher DL, Arsura EL (September 1989). "Multifocal atrial tachycardia: mechanisms, clinical correlates, and treatment". Am. Heart J. 118 (3): 574–80. doi:10.1016/0002-8703(89)90275-5. PMID 2570520.
- ↑ Goodacre S, Irons R (March 2002). "ABC of clinical electrocardiography: Atrial arrhythmias". BMJ. 324 (7337): 594–7. doi:10.1136/bmj.324.7337.594. PMC 1122515. PMID 11884328.
- ↑ Lin CY, Lin YJ, Chen YY, Chang SL, Lo LW, Chao TF, Chung FP, Hu YF, Chong E, Cheng HM, Tuan TC, Liao JN, Chiou CW, Huang JL, Chen SA (August 2015). "Prognostic Significance of Premature Atrial Complexes Burden in Prediction of Long-Term Outcome". J Am Heart Assoc. 4 (9): e002192. doi:10.1161/JAHA.115.002192. PMC 4599506. PMID 26316525.
- ↑ Strasburger JF, Cheulkar B, Wichman HJ (December 2007). "Perinatal arrhythmias: diagnosis and management". Clin Perinatol. 34 (4): 627–52, vii–viii. doi:10.1016/j.clp.2007.10.002. PMC 3310372. PMID 18063110.
- ↑ Rao AL, Salerno JC, Asif IM, Drezner JA (July 2014). "Evaluation and management of wolff-Parkinson-white in athletes". Sports Health. 6 (4): 326–32. doi:10.1177/1941738113509059. PMC 4065555. PMID 24982705.
- ↑ Rosner MH, Brady WJ, Kefer MP, Martin ML (November 1999). "Electrocardiography in the patient with the Wolff-Parkinson-White syndrome: diagnostic and initial therapeutic issues". Am J Emerg Med. 17 (7): 705–14. doi:10.1016/s0735-6757(99)90167-5. PMID 10597097.
- ↑ Glinge C, Sattler S, Jabbari R, Tfelt-Hansen J (September 2016). "Epidemiology and genetics of ventricular fibrillation during acute myocardial infarction". J Geriatr Cardiol. 13 (9): 789–797. doi:10.11909/j.issn.1671-5411.2016.09.006. PMC 5122505. PMID 27899944.
- ↑ Samie FH, Jalife J (May 2001). "Mechanisms underlying ventricular tachycardia and its transition to ventricular fibrillation in the structurally normal heart". Cardiovasc. Res. 50 (2): 242–50. doi:10.1016/s0008-6363(00)00289-3. PMID 11334828.
- ↑ Adabag AS, Luepker RV, Roger VL, Gersh BJ (April 2010). "Sudden cardiac death: epidemiology and risk factors". Nat Rev Cardiol. 7 (4): 216–25. doi:10.1038/nrcardio.2010.3. PMC 5014372. PMID 20142817.
- ↑ Koplan BA, Stevenson WG (March 2009). "Ventricular tachycardia and sudden cardiac death". Mayo Clin. Proc. 84 (3): 289–97. doi:10.1016/S0025-6196(11)61149-X. PMC 2664600. PMID 19252119.
- ↑ Levis JT (2011). "ECG Diagnosis: Monomorphic Ventricular Tachycardia". Perm J. 15 (1): 65. doi:10.7812/tpp/10-130. PMC 3048638. PMID 21505622.