Parathyroid gland
|
WikiDoc Resources for Parathyroid gland |
|
Articles |
|---|
|
Most recent articles on Parathyroid gland Most cited articles on Parathyroid gland |
|
Media |
|
Powerpoint slides on Parathyroid gland |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Parathyroid gland |
|
Clinical Trials |
|
Ongoing Trials on Parathyroid gland at Clinical Trials.gov Trial results on Parathyroid gland Clinical Trials on Parathyroid gland at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Parathyroid gland NICE Guidance on Parathyroid gland
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Parathyroid gland Discussion groups on Parathyroid gland Patient Handouts on Parathyroid gland Directions to Hospitals Treating Parathyroid gland Risk calculators and risk factors for Parathyroid gland
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Parathyroid gland |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-in-Chief: Larry Gordon, M.D.
Overview
The parathyroid glands are small endocrine glands in the neck, usually located behind the thyroid gland, which produce parathyroid hormone. In rare cases the parathyroid glands are located within the thyroid glands. Most often there are four parathyroid glands, but some people have six or even eight.
Anatomy
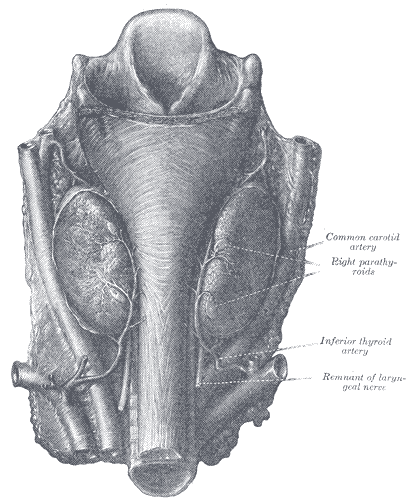
The parathyroid glands are four or more small glands located on the posterior surface of the thyroid gland. Histologically they are quite easily recognizable from the thyroid as they have densely packed cells in contrast with the follicle structure of the thyroid. [1] However at surgery they are harder to differentiate from the thyroid or fat.
They distinguish themselves from the thyroid gland histologically as they contain two types of cells:[2]
| Name | Staining | Quantity | Size | Function |
| parathyroid chief cells | darker | many[3] | smaller | manufacture PTH (see below). |
| oxyphil cells | lighter | few | larger | function unknown.[4][5] |
History
- The parathyroid glands were first discovered in the Indian Rhinoceros by Richard Owen in 1852.[6] In his description of the neck anatomy, Owen referred to the glands as "a small compact yellow glandular body attached to the thyroid at the point where the veins emerged".
- The glands were first discovered in humans by Ivar Viktor Sandström (1852–1889), a Swedish medical student, in 1880 at Uppsala University.[7] Unaware of Owen's description, he described the glands in his monograph "On a New Gland in Man and Fellow Animals" as the "glandulae parathyroidae", noting its existence in dogs, cats, rabbits, oxen, horses and humans.[8][9] For several years, Sandström's description received little attention.[10]
- Physiologist Eugene Gley first documented the putative function of the glands in 1891, noting the connection between their removal and the development of muscular tetani. William G. MacCallum in 1908, investigating tumours of the parathyroid, proposed their role in calcium metabolism.[9] He noted that "Tetany occurs spontaneously in many forms and may also be produced by the destruction of the parathyroid glands".[11]
- Parathyroid hormone was isolated in 1923 by Adolph M. Hanson and 1925 by James B. Collip. Studies of parathyroid hormone levels by Roger Guillemin, Andrew Schally and Rosalyn Sussman Yalow led to the development of immunoassays capable of measuring body substances and a Nobel Prize in 1977.[12]
Physiology
The sole function of the parathyroid glands is to maintain the body's calcium level within a very narrow range, so that the nervous and muscular systems can function properly.
When blood calcium levels drop below a certain point, calcium-sensing receptors in the parathyroid gland are activated to release hormone into the blood.
Parathyroid hormone (PTH, also known as parathormone) is a small protein that takes part in the control of calcium and phosphate homeostasis, as well as bone physiology. Parathyroid hormone has effects antagonistic to those of calcitonin. It increases blood calcium levels by stimulating osteoclasts to break down bone and release calcium. It also increases gastrointestinal calcium absorption by activating vitamin D, and promotes calcium uptake by the kidneys.
Role in disease
The single major disease of parathyroid glands is overactivity of one or more of the parathyroid lobes, which make too much parathyroid hormone causing a potentially serious calcium imbalance. This is called hyperparathyroidism; it leads to hypercalcemia and osteitis fibrosa cystica. Since hyperparathyroidism was first described in 1925, the symptoms have become known as "moans, groans, stones, and bones." The primary treatment for this disease is the surgical removal of the faulty gland.
Modern high frequency ultrasound can see parathyroid masses, even before they cause high calcium. They are called parathyroid incidentalomas. If a patient has elevated calcium, the ultrasound can be used to locate the abnormal glands. The use of ultrasound guided FNA, and parathyroid hormone washings can confirm the abnormal glands. A blood calcium 15-30 minutes after the biopsy can help determine if the disease is caused by a single abnormal gland or multiple glands.
A drop in serum calcium suggests a single source, and no drop suggests multiple glands. This, with a non-localizing Sestamibi scan would point toward a neck exploration, rather than a minimally invasive method aimed a single gland disease.
A Sestamibi scan is often used to determine which parathyroid gland(s) are responsible for overproduction of parathyroid hormone.
Another related condition is called secondary hyperparathyroidism (high-per-parr-uh-THIGH-royd-izm), or secondary HPT - common in patients with chronic kidney disease on dialysis. In secondary HPT, the parathyroid glands make too much parathyroid hormone (PTH), and the kidneys do not produce enough vitamin D, and calcium and phosphorus are out of balance. Even though one may not have any symptoms, treating secondary HPT is important. Cinacalcet (Sensipar®) is a medicine that can help treat such dialysis patients and is available by prescription only.
- Hypoparathyroidism
- Pseudohypoparathyroidism
- Pseudopseudohypoparathyroidism
- Disorders of the parathyroid hormone receptor have been associated with Jansen's metaphyseal chondroplasia and Blomstrand's chondroplasia.
Embryology and Evolution
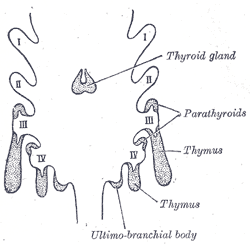
The parathyroid glands originate from the interaction of neural crest mesenchyme and third and fourth pharyngeal pouch endoderm.
Genetically, Eya-1 (transcripitonal co-activator), Six-1 (a homeobox transcription factor), and Gcm-2 (a transcription factor) have been associated with the development of the parathyroid gland, and alterations in these genes alters parathyroid gland development.
The conserved homology of genes and calcium sensing receptors in fish gills with those in the parathryroid glands of birds and mammals is recognized by evolutionary developmental biology as evolution using genes and gene networks in novel ways to generate new structures with some similar functions and novel functions.
Additional images
-
Scheme showing development of branchial epithelial bodies. I, II, III, IV. Branchial pouches.
-
Human parathyroid glands
References
- ↑ Histology image: 15001ooa – Histology Learning System at Boston University
- ↑ Histology image: 15002loa – Histology Learning System at Boston University
- ↑ Histology at University of Southern California end/c_28
- ↑ Template:OklahomaHistology
- ↑ Histology at University of Southern California end/c_34
- ↑ Cave, A.J.E. (1953). "Richard Owen and the discovery of the parathyroid glands" (PDF). In E. Ashworth Underwood. Science, Medicine and History. Essays on the Evolution of Scientific Thought and Medical Practice. 2. Oxford University Press. pp. 217–222. Retrieved 2009-07-20.
- ↑ Eknoyan G (November 1995). "A history of the parathyroid glands". American Journal of Kidney Disease. 26 (5): 801–7. doi:10.1016/0272-6386(95)90447-6. PMID 7485136.
- ↑ "On a New Gland in Man and Several Mammals (Glandulæ Parathyreoideæ)". Journal of the American Medical Association. 111 (2): 197. 9 July 1938. doi:10.1001/jama.1938.02790280087037.
- ↑ Jump up to: 9.0 9.1 DuBose, Joseph; Ragsdale, Timothy; Morvant, Jason (January 2005). ""Bodies so tiny": The history of parathyroid surgery". Current Surgery. 62 (1): 91–95. doi:10.1016/j.cursur.2004.07.012.
- ↑ Carney, JA (Sep 1996). "The glandulae parathyroideae of Ivar Sandström. Contributions from two continents". The American journal of surgical pathology. 20 (9): 1123–44. doi:10.1097/00000478-199609000-00010. PMID 8764749.
- ↑ Maccallum, W. G; Voegtlin, C. (Jan 9, 1909). "On the Relation of Tetant to the Parathyroid Glands and to Calcium Metabolism". The Journal of experimental medicine. 11 (1): 118–51. doi:10.1084/jem.11.1.118. PMC 2124703. PMID 19867238.
- ↑ Parathyroid gland. Wikipedia (2015). https://en.wikipedia.org/wiki/Parathyroid_gland Accessed on December 28, 2015
External links
- Parathyroid disease and treatments discussed in layman's terms at Parathyroid.com
- Endocrine Web at endocrineweb.com
- Parathyroid disease resources and treatment options at AdvancedParathyroid.com
- The origin of the parathyroid gland at pnas.org
- Human Gland Probably Evolved From Gills at pandasthumb.org
- The role of the endoderm in the development and evolution of the pharyngeal arches at blackwell-synergy.com
- Deep homologies in the pharyngeal arches at scienceblogs.com
- Template:EMedicineDictionary
- Histology at University of Southern California end/c_29
- Template:IowaHistologyInteractive
ar:غدة جار درقية bn:প্যারাথাইরয়েড গ্রন্থি de:Nebenschilddrüse dv:ޕަރަތައިރޮއިޑް ގްލޭންޑް it:Paratiroide he:פאראתירואיד la:Glandulae parathyroidae lt:Prieskydinė liauka mk:Параштитна жлезда nl:Bijschildklier sk:Príštitne teliesko sl:Obščitnica fi:Lisäkilpirauhanen sv:Paratyroidea