Dexlansoprazole
{{DrugProjectFormSinglePage |authorTag=
Vignesh Ponnusamy, M.B.B.S. [1]
|genericName=
Dexlansoprazole
|aOrAn=
a
|drugClass=
proton pump inhibitor (PPI)
|indication=
all grades of erosive esophagitis (EE), heartburn associated with symptomatic non-erosive gastroesophageal reflux disease (GERD)
|hasBlackBoxWarning=
|adverseReactions=
diarrhea, abdominal pain, nausea, upper respiratory tract infection, vomiting, and flatulence
|blackBoxWarningTitle=
Title
|blackBoxWarningBody= ConditionName:
- Content
|fdaLIADAdult=
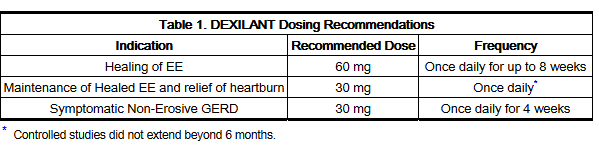
Healing of Erosive Esophagitis
- Dosing Information
- 60 mg once daily for up to 8 weeks.
Maintenance of Healed Erosive Esophagitis
- Dosing Information
- 30 mg once daily.
Symptomatic Non-Erosive Gastroesophageal Reflux Disease
- Dosing Information
- 30 mg once daily for 4 weeks.
|offLabelAdultGuideSupport=
There is limited information regarding Off-Label Guideline-Supported Use of Dexlansoprazole in adult patients.
|offLabelAdultNoGuideSupport=
There is limited information regarding Off-Label Non–Guideline-Supported Use of Dexlansoprazole in adult patients.
|fdaLIADPed=
There is limited information regarding FDA-Labeled Use of Dexlansoprazole in pediatric patients.
|offLabelPedGuideSupport=
There is limited information regarding Off-Label Guideline-Supported Use of Dexlansoprazole in pediatric patients.
|offLabelPedNoGuideSupport=
There is limited information regarding Off-Label Non–Guideline-Supported Use of Dexlansoprazole in pediatric patients.
|contraindications=
- DEXILANT is contraindicated in patients with known hypersensitivity to any component of the formulation. Hypersensitivity and anaphylaxis have been reported with DEXILANT use.
|warnings=
Precautions
- Gastric Malignancy
- Symptomatic response with DEXILANT does not preclude the presence of gastric malignancy.
- Clostridium Difficile Associated Diarrhea
- Published observational studies suggest that PPI therapy like DEXILANT may be associated with an increased risk of Clostridium difficile associated diarrhea, especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve.
- Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated.
- Bone Fracture
- Several published observational studies suggest that PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the conditions being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines.
- Hypomagnesemia
- Hypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.
- For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically.
- Concomitant Use of DEXILANT with Methotrexate
- Literature suggests that concomitant use of PPIs with methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration, a temporary withdrawal of the PPI may be considered in some patients.
|clinicalTrials=
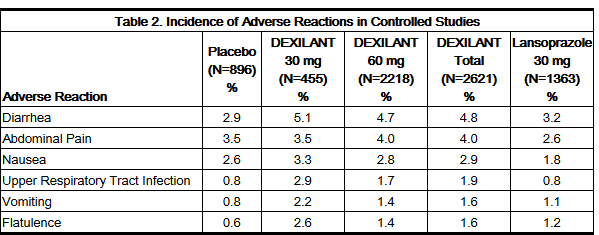
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The safety of DEXILANT was evaluated in 4548 patients in controlled and uncontrolled clinical studies, including 863 patients treated for at least six months and 203 patients treated for one year. Patients ranged in age from 18 to 90 years (median age 48 years), with 54% female, 85% Caucasian, 8% Black, 4% Asian, and 3% other races. Six randomized controlled clinical trials were conducted for the treatment of EE, maintenance of healed EE, and symptomatic GERD, which included 896 patients on placebo, 455 patients on DEXILANT 30 mg, 2218 patients on DEXILANT 60 mg, and 1363 patients on lansoprazole 30 mg once daily.
- Most Commonly Reported Adverse Reactions
- The most common adverse reactions (≥2%) that occurred at a higher incidence for DEXILANT than placebo in the controlled studies are presented in Table 2.
- Adverse Reactions Resulting in Discontinuation
- In controlled clinical studies, the most common adverse reaction leading to discontinuation from DEXILANT therapy was diarrhea (0.7%).
- Other adverse reactions that were reported in controlled studies at an incidence of less than 2% are listed below by body system:
- Blood and Lymphatic System Disorders: anemia,lymphadenopathy
- Cardiac Disorders: angina, arrhythmia, bradycardia, chest pain, edema, myocardial infarction, palpitation, tachycardia
- Ear and Labyrinth Disorders: ear pain, tinnitus, vertigo
- Endocrine Disorders: goiter
- Eye Disorders: eye irritation, eye swelling
- Gastrointestinal Disorders: abdominal discomfort, abdominal tenderness, abnormal feces, anal discomfort, Barrett's esophagus, bezoar, bowel sounds abnormal, breath odor, colitis microscopic, colonic polyp, constipation, dry mouth, duodenitis, dyspepsia, dysphagia, enteritis, eructation, esophagitis, gastric polyp, gastritis, gastroenteritis, gastrointestinal disorders, gastrointestinal hypermotility disorders, GERD, GI ulcers and perforation, hematemesis, hematochezia, hemorrhoids, impaired gastric emptying, irritable bowel syndrome, mucus stools, oral mucosal blistering, painful defecation, proctitis, paresthesia oral, rectal hemorrhage, retching
- General Disorders and Administration Site Conditions: adverse drug reaction, asthenia, chest pain, chills, feeling abnormal, inflammation, mucosal inflammation, nodule, pain, pyrexia
- Hepatobiliary Disorders: biliary colic, cholelithiasis, hepatomegaly
- Immune System Disorders: hypersensitivity
- Infections and Infestations: candida infections, influenza, nasopharyngitis, oral herpes, pharyngitis, sinusitis, viral infection, vulvo-vaginal infection
- Injury, Poisoning and Procedural Complications: falls, fractures, joint sprains, overdose, procedural pain, sunburn
- Laboratory Investigations: ALP increased, ALT increased, AST increased, bilirubin decreased/increased, blood creatinine increased, blood gastrin increased, blood glucose increased, blood potassium increased, liver function test abnormal, platelet count decreased, total protein increased, weight increase
- Metabolism and Nutrition Disorders: appetite changes, hypercalcemia, hypokalemia
- Musculoskeletal and Connective Tissue Disorders: arthralgia, arthritis, muscle cramps, musculoskeletal pain, myalgia
- Nervous System Disorders: altered taste, convulsion, dizziness, headaches, migraine, memory impairment, paresthesia, psychomotor hyperactivity, tremor, trigeminal neuralgia
- Psychiatric Disorders: abnormal dreams, anxiety, depression, insomnia, libido changes
- Renal and Urinary Disorders: dysuria, micturition urgency
- Reproductive System and Breast Disorders: dysmenorrhea, dyspareunia, menorrhagia, menstrual disorder
- Respiratory, Thoracic and Mediastinal Disorders: aspiration, asthma, bronchitis, cough, dyspnoea, hiccups, hyperventilation, respiratory tract congestion, sore throat
- Skin and Subcutaneous Tissue Disorders: acne, dermatitis, erythema, pruritis, rash, skin lesion, urticaria
- Vascular Disorders: deep vein thrombosis, hot flush, hypertension
- Additional adverse reactions that were reported in a long-term uncontrolled study and were considered related to DEXILANT by the treating physician included: anaphylaxis, auditory hallucination, B-cell lymphoma, bursitis, central obesity, cholecystitis acute, dehydration, diabetes mellitus, dysphonia, epistaxis, folliculitis, gout, herpes zoster, hyperlipidemia, hypothyroidism, increased neutrophils, MCHC decrease, neutropenia, rectal tenesmus, restless legs syndrome, somnolence, tonsillitis.
- Other adverse reactions not observed with DEXILANT, but occurring with the racemate lansoprazole can be found in the lansoprazole prescribing information, ADVERSE REACTIONS section.
|postmarketing=
- The following adverse reactions have been identified during post-approval of DEXILANT. As these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Blood and Lymphatic System Disorders: autoimmune hemolytic anemia, idiopathic thrombocytopenic purpura
- Ear and Labyrinth Disorders: deafness
- Eye Disorders: blurred vision
- Gastrointestinal Disorders: oral edema, pancreatitis
- General Disorders and Administration Site Conditions: facial edema
- Hepatobiliary Disorders: drug-induced hepatitis
- Immune System Disorders: anaphylactic shock (requiring emergency intervention), exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis (some fatal)
- Infections and Infestations: Clostridium difficile associated diarrhea
- Metabolism and Nutrition Disorders: hypomagnesemia, hyponatremia
- Musculoskeletal System Disorders: bone fracture
- Nervous System Disorders: cerebrovascular accident, transient ischemic attack
- Renal and Urinary Disorders: acute renal failure
- Respiratory, Thoracic and Mediastinal Disorders: pharyngeal edema, throat tightness
- Skin and Subcutaneous Tissue Disorders: generalized rash, leukocytoclastic vasculitis
|drugInteractions=
- Drugs with pH-Dependent Absorption Pharmacokinetics
- DEXILANT causes inhibition of gastric acid secretion. DEXILANT is likely to substantially decrease the systemic concentrations of the HIV protease inhibitor atazanavir, which is dependent upon the presence of gastric acid for absorption, and may result in a loss of therapeutic effect of atazanavir and the development of HIV resistance. Therefore, DEXILANT should not be co-administered with atazanavir.
- DEXILANT may interfere with the absorption of other drugs where gastric pH is an important determinant of oral bioavailability (e.g., ampicillin esters, digoxin, iron salts, ketoconazole, erlotinib).
- Warfarin
- Co-administration of DEXILANT 90 mg and warfarin 25 mg did not affect the pharmacokinetics of warfarin or INR. However, there have been reports of increased INR and prothrombin time in patients receiving PPIs and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with DEXILANT and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time.
- Tacrolimus
- Concomitant administration of dexlansoprazole and tacrolimus may increase whole blood levels of tacrolimus, especially in transplant patients who are intermediate or poor metabolizers of CYP2C19.
- Clopidogrel
- Concomitant administration of dexlansoprazole and clopidogrel in healthy subjects had no clinically important effect on exposure to the active metabolite of clopidogrel or clopidogrel-induced platelet inhibition. No dose adjustment of clopidogrel is necessary when administered with an approved dose of DEXILANT.
- Methotrexate
- Case reports, published population pharmacokinetic studies, and retrospective analyses suggest that concomitant administration of PPIs and methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite hydroxymethotrexate. However, no formal drug interaction studies of high-dose methotrexate with PPIs have been conducted.
|useInPregnancyFDA=
- Pregnancy Category B
- There are no adequate and well-controlled studies with dexlansoprazole in pregnant women. There were no adverse fetal effects in animal reproduction studies of dexlansoprazole in rabbits. Because animal reproduction studies are not always predictive of human response, DEXILANT should be used during pregnancy only if clearly needed.
- A reproduction study conducted in rabbits at oral dexlansoprazole doses up to approximately nine times the maximum recommended human dexlansoprazole dose (60 mg/day) revealed no evidence of impaired fertility or harm to the fetus due to dexlansoprazole. In addition, reproduction studies performed in pregnant rats with oral lansoprazole at doses up to 40 times the recommended human lansoprazole dose and in pregnant rabbits at oral lansoprazole doses up to 16 times the recommended human lansoprazole dose revealed no evidence of impaired fertility or harm to the fetus due to lansoprazole.
|useInPregnancyAUS=
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Dexlansoprazole in women who are pregnant.
|useInLaborDelivery= There is no FDA guidance on use of Dexlansoprazole during labor and delivery.
|useInNursing=
- It is not known whether dexlansoprazole is excreted in human milk. However, lansoprazole and its metabolites are present in rat milk following the administration of lansoprazole. As many drugs are excreted in human milk, and because of the potential for tumorigenicity shown for lansoprazole in rat carcinogenicity studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
|useInPed= There is no FDA guidance on the use of Dexlansoprazole with respect to pediatric patients.
|useInGeri=
- In clinical studies of DEXILANT, 11% of patients were aged 65 years and over. No overall differences in safety or effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified significant differences in responses between geriatric and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
|useInGender= There is no FDA guidance on the use of Dexlansoprazole with respect to specific gender populations.
|useInRace= There is no FDA guidance on the use of Dexlansoprazole with respect to specific racial populations.
|useInRenalImpair=
- No dosage adjustment of DEXILANT is necessary in patients with renal impairment. The pharmacokinetics of dexlansoprazole in patients with renal impairment are not expected to be altered since dexlansoprazole is extensively metabolized in the liver to inactive metabolites, and no parent drug is recovered in the urine following an oral dose of dexlansoprazole.
|useInHepaticImpair=
- No dosage adjustment for DEXILANT is necessary for patients with mild hepatic impairment (Child-Pugh Class A). DEXILANT 30 mg should be considered for patients with moderate hepatic impairment (Child-Pugh Class B). No studies have been conducted in patients with severe hepatic impairment (Child-Pugh Class C).
|useInReproPotential= There is no FDA guidance on the use of Dexlansoprazole in women of reproductive potentials and males.
|useInImmunocomp= There is no FDA guidance one the use of Dexlansoprazole in patients who are immunocompromised.
|administration=
- Oral
|monitoring=
- Patients taking concomitant warfarin may require monitoring for increases in international normalized ratio (INR) and prothrombin time.
- Consider monitoring magnesium levels prior to initiation of PPI treatment and periodically.
|IVCompat=
There is limited information regarding IV Compatibility of Dexlansoprazole in the drug label.
|overdose=
Acute Overdose
Signs and Symptoms
- There have been no reports of significant overdose of DEXILANT. Multiple doses of DEXILANT 120 mg and a single dose of DEXILANT 300 mg did not result in death or other severe adverse events. However, serious adverse events of hypertension have been reported in association with twice daily doses of DEXILANT 60 mg. Non-serious adverse reactions observed with twice daily doses of DEXILANT 60 mg include hot flashes, contusion, oropharyngeal pain, and weight loss.
Management
- Dexlansoprazole is not expected to be removed from the circulation by hemodialysis. If an overdose occurs, treatment should be symptomatic and supportive.
Chronic Overdose
There is limited information regarding Chronic Overdose of Dexlansoprazole in the drug label.
|drugBox=
| |
Dexlansoprazole
| |
| Systematic (IUPAC) name | |
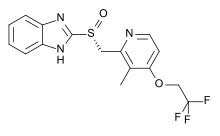
| (R)-(+)2-([3-methyl-4-(2,2,2-trifluoroethoxy)pyridin-2-yl]methylsulfinyl)-1H-benzo[d]imidazole | |
| Identifiers | |
| CAS number | |
| ATC code | A02 |
| PubChem | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 369.363 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | 50% renal and 47% in the feces[1] |
| Therapeutic considerations | |
| Licence data |
|
| Pregnancy cat. |
B(US) |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | Oral |
|mechAction=
- Dexlansoprazole is a PPI that suppresses gastric acid secretion by specific inhibition of the (H+,K+)-ATPase in the gastric parietal cell. By acting specifically on the proton pump, dexlansoprazole blocks the final step of acid production.
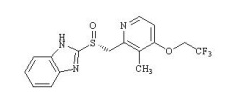
|structure=
- The active ingredient in DEXILANT (dexlansoprazole) delayed-release capsules, a proton pump inhibitor, is (+)-2-[(R)-{[3-methyl-4-(2,2,2-trifluoroethoxy)pyridin-2-yl] methyl} sulfinyl]-1H-benzimidazole, a compound that inhibits gastric acid secretion. Dexlansoprazole is the R-enantiomer of lansoprazole (a racemic mixture of the R- and S-enantiomers). Its empirical formula is: C16H14F3N3O2S, with a molecular weight of 369.36. The structural formula is:
- Dexlansoprazole is a white to nearly white crystalline powder which melts with decomposition at 140°C. Dexlansoprazole is freely soluble in dimethylformamide, methanol, dichloromethane, ethanol, and ethyl acetate; and soluble in acetonitrile; slightly soluble in ether; and very slightly soluble in water; and practically insoluble in hexane.
- Dexlansoprazole is stable when exposed to light. Dexlansoprazole is more stable in neutral and alkaline conditions than acidic conditions.
- DEXILANT is supplied as a dual delayed-release formulation in capsules for oral administration. The capsules contain dexlansoprazole in a mixture of two types of enteric-coated granules with different pH-dependent dissolution profiles.
- DEXILANT is available in two dosage strengths: 30 mg and 60 mg, per capsule. Each capsule contains enteric-coated granules consisting of dexlansoprazole (active ingredient) and the following inactive ingredients: sugar spheres, magnesium carbonate, sucrose, low-substituted hydroxypropyl cellulose, titanium dioxide, hydroxypropyl cellulose, hypromellose 2910, talc, methacrylic acid copolymers, polyethylene glycol 8000, triethyl citrate, polysorbate 80, and colloidal silicon dioxide. The components of the capsule shell include the following inactive ingredients: hypromellose, carrageenan and potassium chloride. Based on the capsule shell color, blue contains FD&C Blue No. 2 aluminum lake; gray contains black ferric oxide; and both contain titanium dioxide.
|PD=
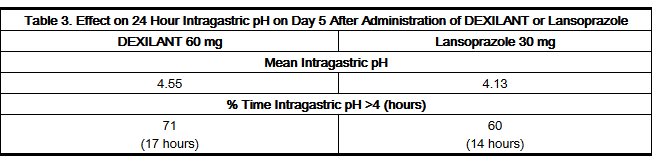
- Antisecretory Activity
- The effects of DEXILANT 60 mg (n=20) or lansoprazole 30 mg (n=23) once daily for five days on 24 hour intragastric pH were assessed in healthy subjects in a multiple-dose crossover study. The results are summarized in Table 3.
- Serum Gastrin Effects
- The effect of DEXILANT on serum gastrin concentrations was evaluated in approximately 3460 patients in clinical trials up to eight weeks and in 1023 patients for up to six to 12 months. The mean fasting gastrin concentrations increased from baseline during treatment with DEXILANT 30 mg and 60 mg doses. In patients treated for more than six months, mean serum gastrin levels increased during approximately the first three months of treatment and were stable for the remainder of treatment. Mean serum gastrin levels returned to pre-treatment levels within one month of discontinuation of treatment.
- Enterochromaffin-Like Cell (ECL) Effects
- There were no reports of ECL cell hyperplasia in gastric biopsy specimens obtained from 653 patients treated with DEXILANT 30 mg, 60 mg or 90 mg for up to 12 months.
- During lifetime exposure of rats dosed daily with up to 150 mg/kg/day of lansoprazole, marked hypergastrinemia was observed followed by ECL cell proliferation and formation of carcinoid tumors, especially in female rats.
- Effect on Cardiac Repolarization
- A study was conducted to assess the potential of DEXILANT to prolong the QT/QTc interval in healthy adult subjects. DEXILANT doses of 90 mg or 300 mg did not delay cardiac repolarization compared to placebo. The positive control (moxifloxacin) produced statistically significantly greater mean maximum and time-averaged QT/QTc intervals compared to placebo.
|PK=
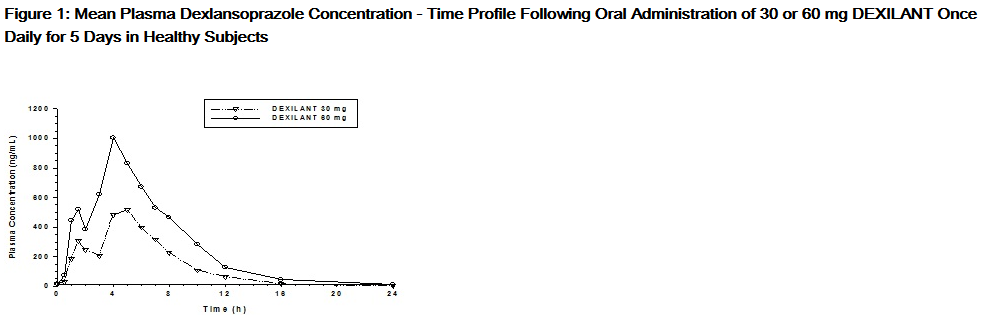
- The dual delayed release formulation of DEXILANT results in a dexlansoprazole plasma concentration-time profile with two distinct peaks; the first peak occurs one to two hours after administration, followed by a second peak within four to five hours (see Figure 1). Dexlansoprazole is eliminated with a half-life of approximately one to two hours in healthy subjects and in patients with symptomatic GERD. No accumulation of dexlansoprazole occurs after multiple, once daily doses of DEXILANT 30 mg or 60 mg, although mean AUCt and Cmax values of dexlansoprazole were slightly higher (less than 10%) on Day 5 than on Day 1.
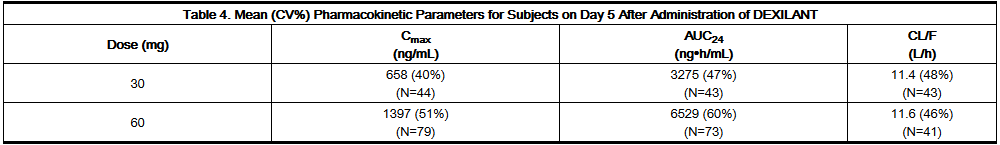
- The pharmacokinetics of dexlansoprazole are highly variable, with percent coefficient of variation (CV%) values for Cmax, AUC, and CL/F of greater than 30% (see Table 4).
- Absorption
- After oral administration of DEXILANT 30 mg or 60 mg to healthy subjects and symptomatic GERD patients, mean Cmax and AUC values of dexlansoprazole increased approximately dose proportionally (see Figure 1).
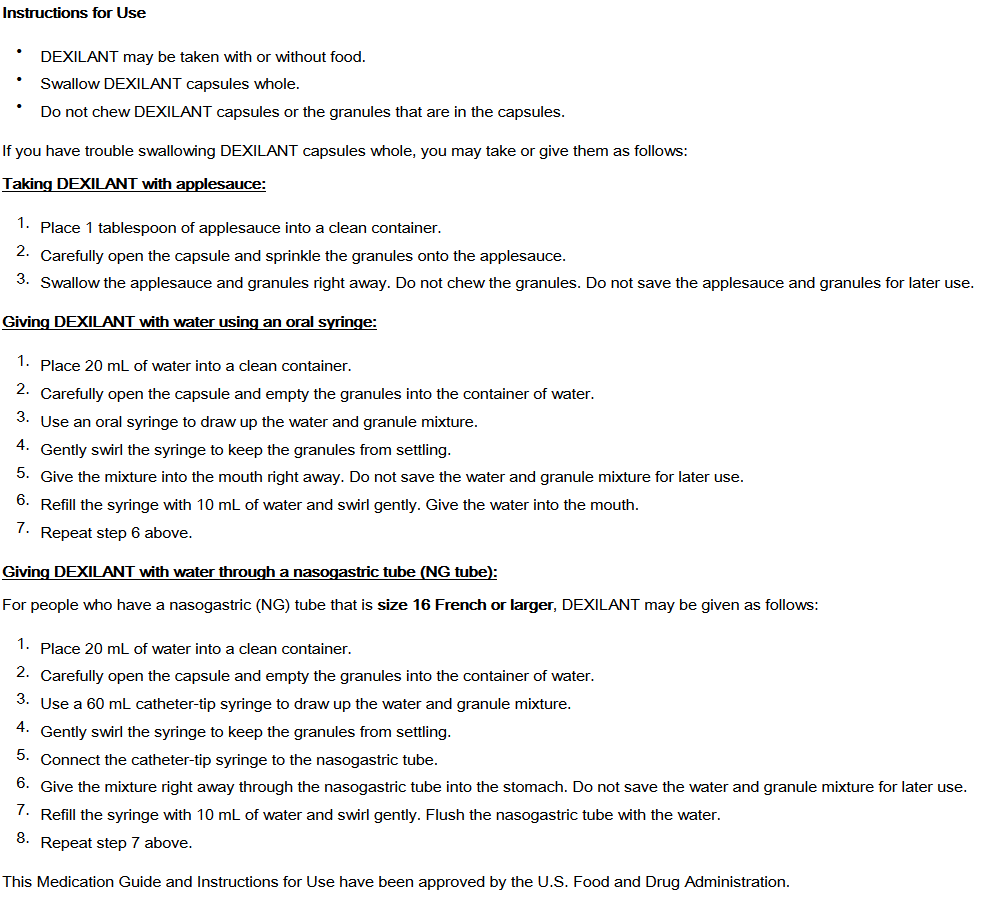
- When granules of DEXILANT 60 mg are mixed with water and dosed via NG tube or orally via syringe, the bioavailability (Cmax and AUC) of dexlansoprazole was similar to that when DEXILANT 60 mg was administered as an intact capsule.
- Distribution
- Plasma protein binding of dexlansoprazole ranged from 96.1% to 98.8% in healthy subjects and was independent of concentration from 0.01 to 20 mcg/mL. The apparent volume of distribution (Vz/F) after multiple doses in symptomatic GERD patients was 40.3 L.
- Metabolism
- Dexlansoprazole is extensively metabolized in the liver by oxidation, reduction, and subsequent formation of sulfate, glucuronide and glutathione conjugates to inactive metabolites. Oxidative metabolites are formed by the cytochrome P450 (CYP) enzyme system including hydroxylation mainly by CYP2C19, and oxidation to the sulfone by CYP3A4.
- CYP2C19 is a polymorphic liver enzyme which exhibits three phenotypes in the metabolism of CYP2C19 substrates; extensive metabolizers (*1/*1), intermediate metabolizers (*1/mutant) and poor metabolizers (mutant/mutant). Dexlansoprazole is the major circulating component in plasma regardless of CYP2C19 metabolizer status. In CYP2C19 intermediate and extensive metabolizers, the major plasma metabolites are 5-hydroxy dexlansoprazole and its glucuronide conjugate, while in CYP2C19 poor metabolizers dexlansoprazole sulfone is the major plasma metabolite.
- Elimination
- Following the administration of DEXILANT, no unchanged dexlansoprazole is excreted in urine. Following the administration of [14C] dexlansoprazole to six healthy male subjects, approximately 50.7% (standard deviation (SD): 9.0%) of the administered radioactivity was excreted in urine and 47.6% (SD: 7.3%) in the feces. Apparent clearance (CL/F) in healthy subjects was 11.4 to 11.6 L/h, respectively, after five days of 30 or 60 mg once daily administration.
- Effect of Food on Pharmacokinetics and Pharmacodynamics
- In food-effect studies in healthy subjects receiving DEXILANT under various fed conditions compared to fasting, increases in Cmax ranged from 12% to 55%, increases in AUC ranged from 9% to 37%, and tmax varied (ranging from a decrease of 0.7 hours to an increase of three hours). No significant differences in mean intragastric pH were observed between fasted and various fed conditions. However, the percentage of time intragastric pH exceeded four over the 24 hour dosing interval decreased slightly when DEXILANT was administered after a meal (57%) relative to fasting (64%), primarily due to a decreased response in intragastric pH during the first four hours after dosing. Because of this, while DEXILANT can be taken without regard to food, some patients may benefit from administering the dose prior to a meal if post-meal symptoms do not resolve under post-fed conditions.
- Special Populations
- Pediatric Use
- The pharmacokinetics of dexlansoprazole in patients under the age of 18 years have not been studied.
- Geriatric Use
- The terminal elimination half-life of dexlansoprazole is significantly increased in geriatric subjects compared to younger subjects (2.23 and 1.5 hours, respectively); this difference is not clinically relevant. Dexlansoprazole exhibited higher systemic exposure (AUC) in geriatric subjects (34.5% higher) than younger subjects. No dosage adjustment is needed in geriatric patients.
- Renal Impairment
- Dexlansoprazole is extensively metabolized in the liver to inactive metabolites, and no parent drug is recovered in the urine following an oral dose of dexlansoprazole. Therefore, the pharmacokinetics of dexlansoprazole are not expected to be altered in patients with renal impairment, and no studies were conducted in subjects with renal impairment. In addition, the pharmacokinetics of lansoprazole were studied in patients with mild, moderate or severe renal impairment; results demonstrated no need for a dose adjustment for this patient population.
- Hepatic Impairment
- In a study of 12 patients with moderately impaired hepatic function who received a single oral dose of DEXILANT 60 mg, plasma exposure (AUC) of bound and unbound dexlansoprazole in the hepatic impairment group was approximately two times greater compared to subjects with normal hepatic function. This difference in exposure was not due to a difference in protein binding between the two liver function groups. No adjustment for DEXILANT is necessary for patients with mild hepatic impairment (Child-Pugh Class A). DEXILANT 30 mg should be considered for patients with moderate hepatic impairment (Child-Pugh Class B). No studies have been conducted in patients with severe hepatic impairment (Child-Pugh Class C).
- Gender
- In a study of 12 male and 12 female healthy subjects who received a single oral dose of DEXILANT 60 mg, females had higher systemic exposure (AUC) (42.8% higher) than males. No dosage adjustment is necessary in patients based on gender.
- Drug-Drug Interactions
- Warfarin
- In a study of 20 healthy subjects, co-administration of DEXILANT 90 mg once daily for 11 days with a single 25 mg oral dose of warfarin on Day 6 did not result in any significant differences in the pharmacokinetics of warfarin or INR compared to administration of warfarin with placebo. However, there have been reports of increased INR and prothrombin time in patients receiving PPIs and warfarin concomitantly [see Drug Interactions (7.2)].
- Cytochrome P 450 Interactions
- Dexlansoprazole is metabolized, in part, by CYP2C19 and CYP3A4 [see Clinical Pharmacology (12.3)].
- In vitro studies have shown that dexlansoprazole is not likely to inhibit CYP isoforms 1A1, 1A2, 2A6, 2B6, 2C8, 2C9, 2D6, 2E1 or 3A4. As such, no clinically relevant interactions with drugs metabolized by these CYP enzymes would be expected. Furthermore, in vivo studies showed that DEXILANT did not have an impact on the pharmacokinetics of coadministered phenytoin (CYP2C9 substrate) or theophylline (CYP1A2 substrate). The subjects' CYP1A2 genotypes in the drug-drug interaction study with theophylline were not determined. Although in vitro studies indicated that DEXILANT has the potential to inhibit CYP2C19 in vivo, an in vivo drug-drug interaction study in mainly CYP2C19 extensive and intermediate metabolizers has shown that DEXILANT does not affect the pharmacokinetics of diazepam (CYP2C19 substrate).
- Clopidogrel
- Clopidogrel is metabolized to its active metabolite in part by CYP2C19. A study of healthy subjects who were CYP2C19 extensive metabolizers, receiving once daily administration of clopidogrel 75 mg alone or concomitantly with DEXILANT 60 mg (n=40), for nine days was conducted. The mean AUC of the active metabolite of clopidogrel was reduced by approximately 9% (mean AUC ratio was 91%, with 90% CI of 86-97%) when DEXILANT was coadministered compared to administration of clopidogrel alone. Pharmacodynamic parameters were also measured and demonstrated that the change in inhibition of platelet aggregation (induced by 5 mcM ADP) was related to the change in the exposure to clopidogrel active metabolite. The clinical significance of this finding is not clear.
Pharmacogenomics
- Effect of CYP2C19 Polymorphism on Systemic Exposure of Dexlansoprazole
- Systemic exposure of dexlansoprazole is generally higher in intermediate and poor metabolizers. In male Japanese subjects who received a single dose of DEXILANT 30 mg or 60 mg (N=2 to 6 subjects/group), mean dexlansoprazole Cmax and AUC values were up to two times higher in intermediate compared to extensive metabolizers; in poor metabolizers, mean Cmax was up to four times higher and mean AUC was up to 12 times higher compared to extensive metabolizers. Though such study was not conducted in Caucasians and African Americans, it is expected dexlansoprazole exposure in these races will be affected by CYP2C19 phenotypes as well.
|nonClinToxic=
Carcinogenesis, Mutagenesis, Impairment of Fertility
- The carcinogenic potential of dexlansoprazole was assessed using lansoprazole studies. In two 24-month carcinogenicity studies, Sprague-Dawley rats were treated orally with lansoprazole at doses of 5 to 150 mg/kg/day, about one to 40 times the exposure on a body surface (mg/m2) basis of a 50 kg person of average height [1.46 m2 body surface area (BSA)] given the recommended human dose of lansoprazole 30 mg/day.
- Lansoprazole produced dose-related gastric ECL cell hyperplasia and ECL cell carcinoids in both male and female rats.
- In rats, lansoprazole also increased the incidence of intestinal metaplasia of the gastric epithelium in both sexes. In male rats, lansoprazole produced a dose-related increase of testicular interstitial cell adenomas. The incidence of these adenomas in rats receiving doses of 15 to 150 mg/kg/day (4 to 40 times the recommended human lansoprazole dose based on BSA) exceeded the low background incidence (range = 1.4 to 10%) for this strain of rat.
- In a 24 month carcinogenicity study, CD-1 mice were treated orally with lansoprazole doses of 15 to 600 mg/kg/day, two to 80 times the recommended human lansoprazole dose based on BSA. Lansoprazole produced a dose-related increased incidence of gastric ECL cell hyperplasia. It also produced an increased incidence of liver tumors (hepatocellular adenoma plus carcinoma). The tumor incidences in male mice treated with 300 and 600 mg lansoprazole/kg/day (40 to 80 times the recommended human lansoprazole dose based on BSA) and female mice treated with 150 to 600 mg lansoprazole/kg/day (20 to 80 times the recommended human lansoprazole dose based on BSA) exceeded the ranges of background incidences in historical controls for this strain of mice. Lansoprazole treatment produced adenoma of rete testis in male mice receiving 75 to 600 mg/kg/day (10 to 80 times the recommended human lansoprazole dose based on BSA).
- A 26 week p53 (+/-) transgenic mouse carcinogenicity study of lansoprazole was not positive.
- Lansoprazole was positive in the Ames test and the in vitro human lymphocyte chromosomal aberration assay. Lansoprazole was not genotoxic in the ex vivo rat hepatocyte unscheduled DNA synthesis (UDS) test, the in vivo mouse micronucleus test or the rat bone marrow cell chromosomal aberration test.
- Dexlansoprazole was positive in the Ames test and in the in vitro chromosome aberration test using Chinese hamster lung cells. Dexlansoprazole was negative in the in vivo mouse micronucleus test.
- The potential effects of dexlansoprazole on fertility and reproductive performance were assessed using lansoprazole studies. Lansoprazole at oral doses up to 150 mg/kg/day (40 times the recommended human lansoprazole dose based on BSA) was found to have no effect on fertility and reproductive performance of male and female rats.
Animal Toxicology and/or Pharmacology
- Reproductive Toxicology Studies
- A reproduction study conducted in rabbits at oral dexlansoprazole doses up to 30 mg/kg/day (approximately nine times the maximum recommended human dexlansoprazole dose [60 mg/day] based on BSA) revealed no evidence of impaired fertility or harm to the fetus due to dexlansoprazole. In addition, reproduction studies performed in pregnant rats with oral lansoprazole at doses up to 150 mg/kg/day (40 times the recommended human lansoprazole dose based on BSA) and in pregnant rabbits at oral lansoprazole doses up to 30 mg/kg/day (16 times the recommended human lansoprazole dose based on BSA) revealed no evidence of impaired fertility or harm to the fetus due to lansoprazole.
|clinicalStudies=
Healing of Erosive Esophagitis
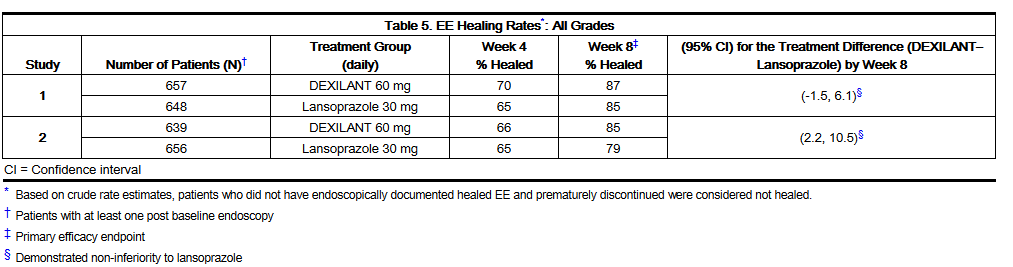
- Two multi-center, double-blind, active-controlled, randomized, eight week studies were conducted in patients with endoscopically confirmed EE. Severity of the disease was classified based on the Los Angeles Classification Grading System (Grades A-D). Patients were randomized to one of the following three treatment groups: DEXILANT 60 mg daily, DEXILANT 90 mg daily or lansoprazole 30 mg daily. Patients who were H. pylori positive or who had Barrett's Esophagus and/or definite dysplastic changes at baseline were excluded from these studies. A total of 4092 patients were enrolled and ranged in age from 18 to 90 years (median age 48 years) with 54% male. Race was distributed as follows: 87% Caucasian, 5% Black and 8% other. Based on the Los Angeles Classification, 71% of patients had mild EE (Grades A and B) and 29% of patients had moderate to severe EE (Grades C and D) before treatment.
- The studies were designed to test non-inferiority. If non-inferiority was demonstrated then superiority would be tested. Although non-inferiority was demonstrated in both studies, the finding of superiority in one study was not replicated in the other.
- The proportion of patients with healed EE at Week 4 or 8 is presented below in Table 5.
- DEXILANT 90 mg was studied and did not provide additional clinical benefit over DEXILANT 60 mg.
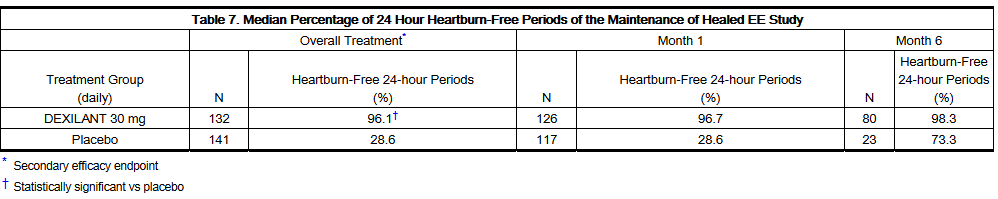
Maintenance of Healed Erosive Esophagitis
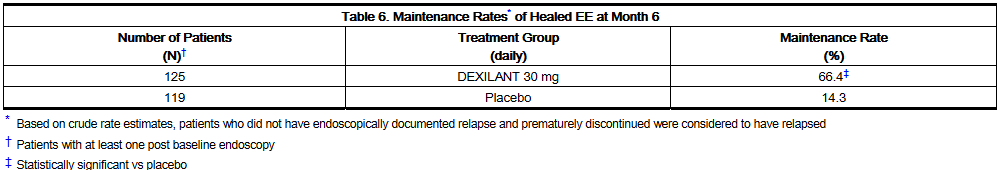
- A multi-center, double-blind, placebo-controlled, randomized study was conducted in patients who successfully completed an EE study and showed endoscopically confirmed healed EE. Maintenance of healing and symptom resolution over a six month period were evaluated with DEXILANT 30 mg or 60 mg once daily compared to placebo. A total of 445 patients were enrolled and ranged in age from 18 to 85 years (median age 49 years), with 52% female. Race was distributed as follows: 90% Caucasian, 5% Black and 5% other.
- Sixty-six percent of patients treated with 30 mg of DEXILANT remained healed over the six-month time period as confirmed by endoscopy (see Table 6).
- DEXILANT 60 mg was studied and did not provide additional clinical benefit over DEXILANT 30 mg.
- The effect of DEXILANT 30 mg on maintenance of relief of heartburn was also evaluated. Upon entry into the maintenance study, a majority of patients' baseline heartburn severity was rated as none. DEXILANT 30 mg demonstrated a statistically significantly higher percent of 24 hour heartburn-free periods compared to placebo over the six month treatment period (see Table 7). The majority of patients treated with placebo discontinued due to relapse of EE between month two and month six.
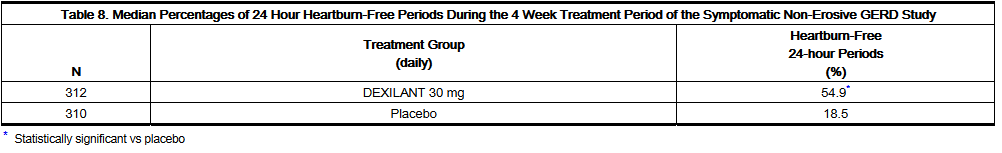
Symptomatic Non-Erosive GERD
- A multi-center, double-blind, placebo-controlled, randomized, four week study was conducted in patients with a diagnosis of symptomatic non-erosive GERD made primarily by presentation of symptoms. These patients who identified heartburn as their primary symptom, had a history of heartburn for 6 months or longer, had heartburn on at least four of seven days immediately prior to randomization and had no esophageal erosions as confirmed by endoscopy. However, patients with symptoms which were not acid-related may not have been excluded using these inclusion criteria. Patients were randomized to one of the following treatment groups: DEXILANT 30 mg daily, 60 mg daily, or placebo. A total of 947 patients were enrolled and ranged in age from 18 to 86 years (median age 48 years) with 71% female. Race was distributed as follows: 82% Caucasian, 14% Black and 4% other.
- DEXILANT 30 mg provided statistically significantly greater percent of days with heartburn-free 24 hour periods over placebo as assessed by daily diary over four weeks (see Table 8). DEXILANT 60 mg was studied and provided no additional clinical benefit over DEXILANT 30 mg.
- A higher percentage of patients on DEXILANT 30 mg had heartburn-free 24 hour periods compared to placebo as early as the first three days of treatment and this was sustained throughout the treatment period (percentage of patients on Day 3: DEXILANT 38% versus placebo 15%; on Day 28: DEXILANT 63% versus placebo 40%).
|howSupplied=
- DEXILANT delayed-release capsules, 30 mg, are opaque, blue and gray with TAP and "30" imprinted on the capsule and supplied as:
- NDC Number: 64764-171-11; Size: Unit dose package of 100
- NDC Number: 64764-171-30; Size: Bottle of 30
- NDC Number: 64764-171-90; Size: Bottle of 90
- NDC Number: 64764-171-19; Size: Bottle of 1000
- DEXILANT delayed-release capsules, 60 mg, are opaque, blue with TAP and "60" imprinted on the capsule and supplied as:
- NDC Number: 64764-175-11; Size: Unit dose package of 100
- NDC Number: 64764-175-30; Size: Bottle of 30
- NDC Number: 64764-175-90; Size: Bottle of 90
- NDC Number: 64764-175-19; Size: Bottle of 1000
- Store at 25°C (77°F); excursions permitted to 15 to 30°C (59 to 86°F).
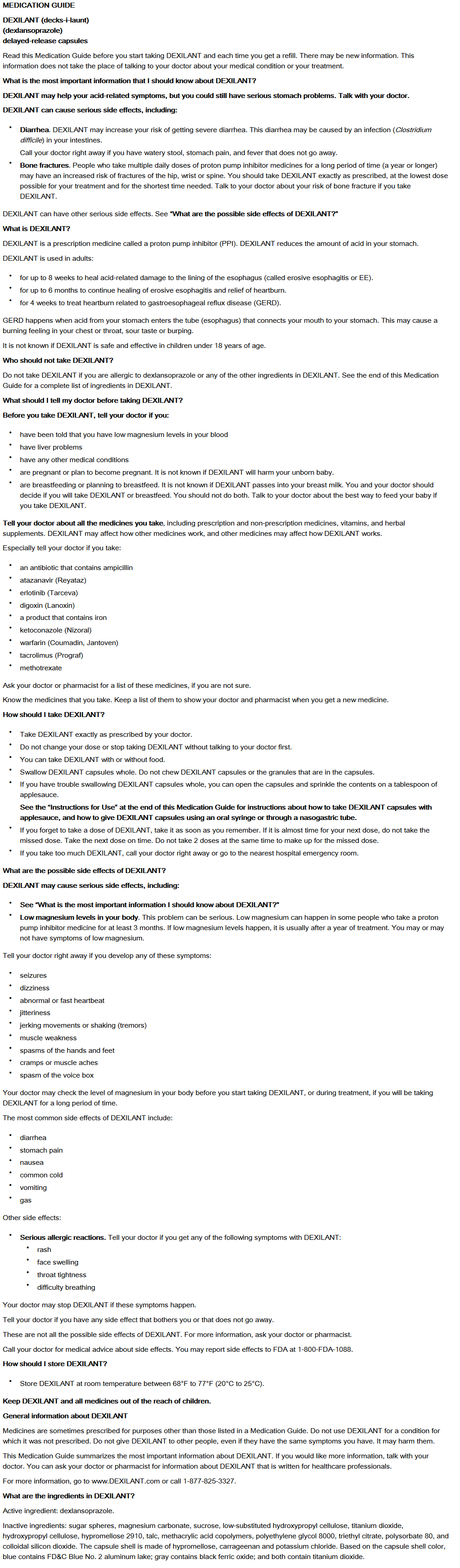
|fdaPatientInfo=
- To ensure the safe and effective use of DEXILANT, this information and instructions provided in the FDA-Approved Medication Guide should be discussed with the patient.
- Inform the patient to watch for signs of an allergic reaction as these could be serious and may require that DEXILANT be discontinued.
- Advise patients to immediately report and seek care for diarrhea that does not improve. This may be a sign of Clostridium difficile associated diarrhea.
- Advise the patient to immediately report and seek care for any cardiovascular or neurological symptoms including palpitations, dizziness, seizures, and tetany as these may be signs of hypomagnesemia.
- Advise the patient to tell their health care provider if they take atazanavir, tacrolimus, warfarin, methotrexate and drugs that are affected by gastric pH changes.
- Advise the patient to follow the dosing instructions in the Medication Guide and inform the patient of the following administration options:
- DEXILANT is available as a delayed-release capsule.
- DEXILANT can be taken without regard to food.
- DEXILANT should be swallowed whole.
- DEXILANT should not be chewed.
- Counsel patients who have difficulty swallowing capsules according to instructions provided in Dosage and Administration (2.3). Advise patients to follow the Instructions for Use that comes with the product.
|alcohol=
- Alcohol-Dexlansoprazole interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
|brandNames=
- Dexilant®[2]
|lookAlike=
|drugShortage=
}}
{{#subobject:
|Page Name=Dexlansoprazole |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Dexlansoprazole |Label Name=Dexlansoprazole11.png
}}
{{#subobject:
|Label Page=Dexlansoprazole |Label Name=Dexlansoprazole12.png
}}
{{#subobject:
|Label Page=Dexlansoprazole |Label Name=Dexlansoprazole13.png
}}
- ↑ Product Information: DEXILANT(R) delayed release oral capsules, dexlansoprazole delayed release oral capsules. Takeda Pharmaceuticals America, Inc., Deerfield, IL, 2010.
- ↑ "DEXILANT (dexlansoprazole) capsule, delayed release [Takeda Pharmaceuticals America, Inc.]".