Crizotinib
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Stefano Giannoni [2]; Sree Teja Yelamanchili, MBBS [3]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Crizotinib is a tyrosine kinase inhibitor that is FDA approved for the treatment of metastatic non-small cell lung cancer (NSCLC) whose tumors are anaplastic lymphoma kinase (ALK)-positive. Common adverse reactions include vision disorders, nausea, diarrhea, vomiting, constipation, edema, elevated transaminases, and fatigue.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Metastatic Non-Small Cell Lung Cancer
- Patient Selection: based on the presence of ALK positivity in tumor specimens
- Dosage: 250 mg orally twice daily until disease progression or no longer tolerated by the patient.
- Recommended dose of crizotinib in patients with severe renal impairment (creatinine clearance <30 mL/min) not requiring dialysis is 250 mg orally, once daily
Dose Modification
- Reduce dose as below, if one or more dose reductions are necessary due to adverse reactions of Grade 3 or 4 severity, as defined by NCI Common Terminology Criteria for Adverse Events (CTCAE) version 4.0:
- First dose reduction: Crizotinib 200 mg taken orally twice daily
- Second dose reduction: Crizotinib 250 mg taken orally once daily
- Permanently discontinue if unable to tolerate Crizotinib 250 mg taken once daily
Dose reduction guidelines are provided in Tables 1 and 2.
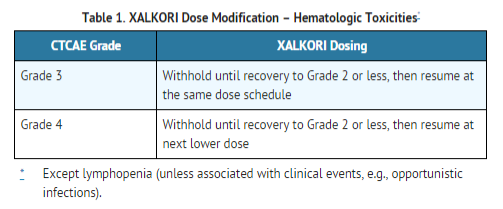
Monitor complete blood counts including differential white blood cell counts monthly and as clinically indicated, with more frequent repeat testing if Grade 3 or 4 abnormalities are observed, or if fever or infection occurs.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Crizotinib in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Crizotinib in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Crizotinib FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Crizotinib in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Crizotinib in pediatric patients.
Contraindications
- None
Warnings
Hepatotoxicity
- Drug-induced hepatotoxicity with fatal outcome occurred in 2 (0.2%) of the 1225 patients treated with crizotinib across three main clinical trials. Concurrent elevations in alanine aminotransferase (ALT) greater than three times the upper limit of normal and total bilirubin greater than two times the upper limit of normal, with normal alkaline phosphatase, occurred in 7 patients (0.6%). Additionally, elevations in ALT greater than five times the upper limit of normal occurred in 109 patients (9.2%). Eight patients (0.7%) required permanent discontinuation due to elevated transaminases.
- These laboratory findings were generally reversible upon dosing interruption.
- Transaminase elevations generally occurred within the first 2 months of treatment.
- Monitor with liver function tests including ALT and total bilirubin every 2 weeks during the first 2 months of treatment, then once a month and as clinically indicated, with more frequent repeat testing for increased liver transaminases, alkaline phosphatase, or total bilirubin in patients who develop transaminase elevations.
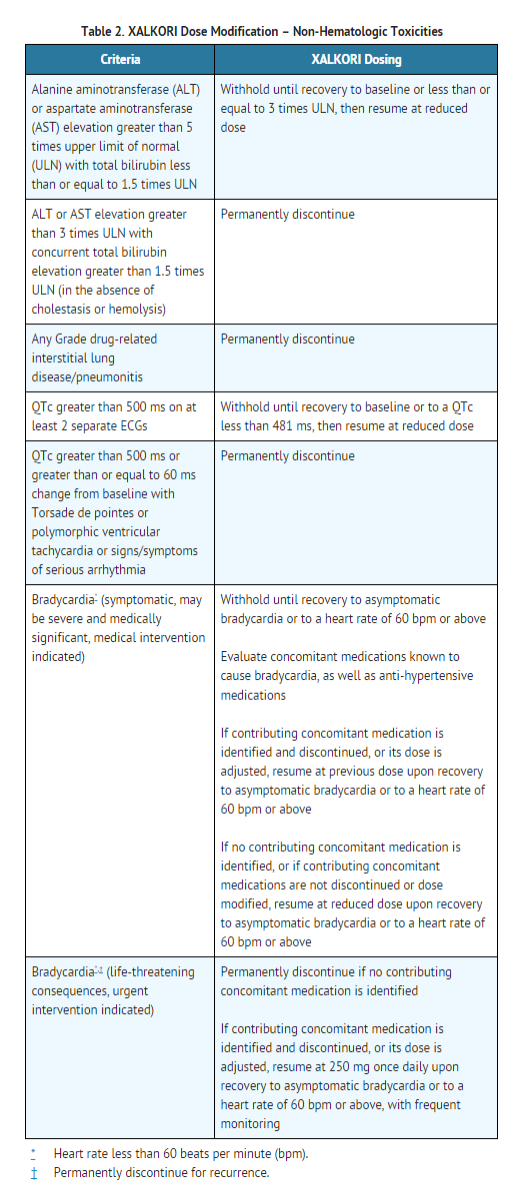
- Temporarily suspend, dose reduce, or permanently discontinue crizotinib as described in Table 2.
Interstitial Lung Disease Pneumonitis
- Severe, life-threatening, or fatal interstitial lung disease (ILD)/pneumonitis can occur in patients treated with crizotinib.
- Across clinical trials (n=1225), 31 crizotinib-treated patients (2.5%) had any grade ILD, 11 patients (0.9%) had Grade 3 or 4, and 6 patients (0.5%) had fatal cases.
- These cases generally occurred within 2 months after the initiation of treatment.
- Monitor patients for pulmonary symptoms indicative of ILD/pneumonitis.
- Exclude other potential causes of ILD/pneumonitis, and permanently discontinue crizotinib in patients diagnosed with drug-related ILD/pneumonitis.
QT Interval Prolongation
- QTc prolongation can occur in patients treated with crizotinib. Across clinical trials (n=1225), QTc prolongation (all grades) was observed in 34 (2.7%) patients and QTc greater than 500 ms on at least 2 separate ECGs occurred in 17(1.4%) patients.
- Avoid use of crizotinib in patients with congenital long QT syndrome. Consider periodic monitoring with electrocardiograms (ECGs) and electrolytes in patients with congestive heart failure, bradyarrhythmias, electrolyte abnormalities, or who are taking medications that are known to prolong the QT interval.
- Permanently discontinue crizotinib in patients who develop QTc greater than 500 ms or greater than or equal to 60 ms change from baseline with Torsade de pointes or polymorphic ventricular tachycardia or signs/symptoms of serious arrhythmia.
- Withhold crizotinib in patients who develop QTc greater than 500 ms on at least 2 separate ECGs until recovery to a QTc less than or equal to 480 ms, then resume crizotinib at a reduced dose as described in Table 2.
Bradycardia
- Symptomatic bradycardia can occur in patients receiving crizotinib.
- Across clinical trials, bradycardia with a heart rate less than 50 beats per minute occurred in 11% of 1174 patients treated with crizotinib.
- In Study 1, Grade 3 syncope occurred in 2.9% of crizotinib-treated patients and in none of the chemotherapy-treated patients.
- Avoid using crizotinib in combination with other agents known to cause bradycardia (e.g., beta-blockers, non-dihydropyridine calcium channel blockers, clonidine and digoxin) to the extent possible.
- Monitor heart rate and blood pressure regularly.
- In cases of symptomatic bradycardia that is not life-threatening, hold crizotinib until recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or above, re-evaluate the use of concomitant medications, and adjust the dose of crizotinib.
- Permanently discontinue for life-threatening bradycardia due to crizotinib; however, if associated with concomitant medications known to cause bradycardia or hypotension, hold crizotinib until recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or above, and if concomitant medications can be adjusted or discontinued, restart crizotinib at 250 mg once daily with frequent monitoring.
Embryofetal Toxicity
- Crizotinib can cause fetal harm when administered to a pregnant woman based on its mechanism of action.
- In nonclinical studies in rats, crizotinib was embryotoxic and fetotoxic at exposures similar to those observed in humans at the recommended clinical dose of 250 mg twice daily.
- There are no adequate and well-controlled studies in pregnant women using crizotinib.
- If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, apprise the patient of the potential hazard to a fetus.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
- Safety evaluation of crizotinib is based on more than 1200 patients with ALK-positive metastatic NSCLC who received crizotinib as monotherapy at a starting oral dose of 250 mg twice daily continuously.
- The most common adverse reactions (≥25%) of crizotinib are vision disorder, nausea, diarrhea, vomiting, constipation, edema, elevated transaminases, and fatigue.
ALK-positive metastatic NSCLC-Study 1
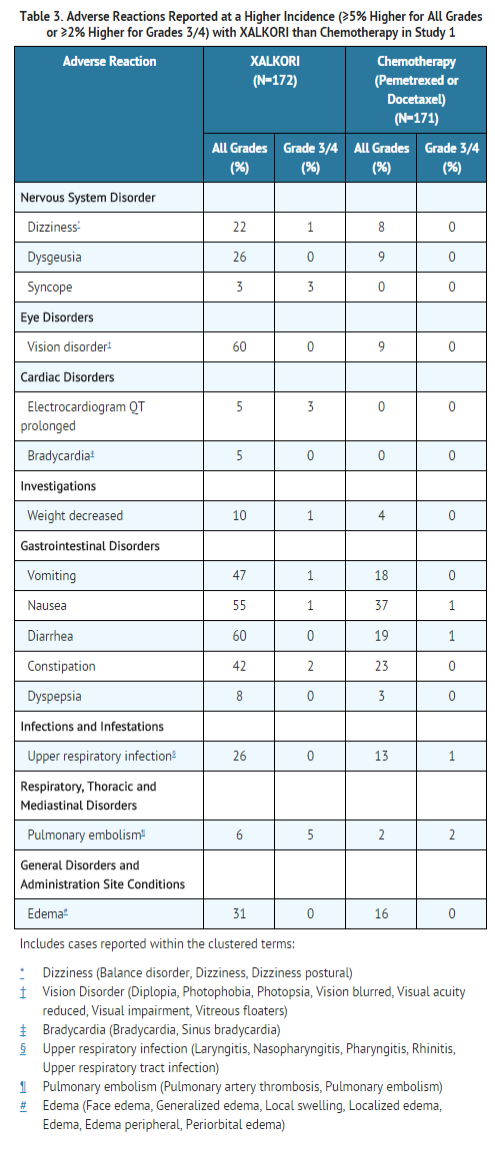
- The data in Table 3 are derived from 343 patients with ALK-positive metastatic NSCLC enrolled in a randomized, multicenter, active-controlled, open-label trial (Study 1).
- Patients in the crizotinib arm (n=172) received crizotinib 250 mg orally twice daily until documented disease progression, intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit.
- A total of 171 patients in the chemotherapy arm received pemetrexed 500 mg/m2 (n=99) or docetaxel 75 mg/m2 (n=72) by intravenous infusion every three weeks until documented disease progression, intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit.
- Patients in the chemotherapy arm received pemetrexed unless they had received pemetrexed as part of first-line or maintenance treatment.
- The median duration of study treatment was 7.1 months for patients who received crizotinib and 2.8 months for patients who received chemotherapy.
- Across the 347 patients who were randomized to study treatment (343 received at least one dose of study treatment), the median age was 50 years; 84% of patients in the crizotinib arm and 87% of patients in the chemotherapy arm were younger than 65 years.
- A total of 57% of patients on crizotinib and 55% of chemotherapy patients were female. Forty-six percent (46%) of crizotinib-treated and 45% of chemotherapy-treated patients were from Asia.
- Serious adverse reactions were reported in 64 patients (37.2%) treated with crizotinib and 40 patients (23.4%) in the chemotherapy arm.
- The most frequent serious adverse reactions reported in patients treated with crizotinib were:
- Pneumonia (4.1%)
- Pulmonary embolism (3.5%)
- Dyspnea (2.3%)
- Interstitial lung disease (ILD; 2.9%).
- Fatal adverse reactions in crizotinib-treated patients in Study 1 occurred in 9 (5%) patients, consisting of:
- Dose reductions due to adverse reactions were required in 16% of crizotinib-treated patients.
- The most frequent adverse reactions that led to dose reduction in the patients treated with crizotinib were alanine aminotransferase (ALT) elevation (7.6%) including some patients with concurrent aspartate aminotransferase (AST) elevation, QTc prolongation (2.9%), and neutropenia (2.3%).
- Discontinuation of therapy in crizotinib-treated patients for adverse reactions was 17.0%.
- The most frequent adverse reactions that led to discontinuation in crizotinib-treated patients were:
- ILD(1.7%)
- ALT elevation
- AST elevation (1.2%)
- Dyspnea (1.2%)
- Pulmonary embolism (1.2%)
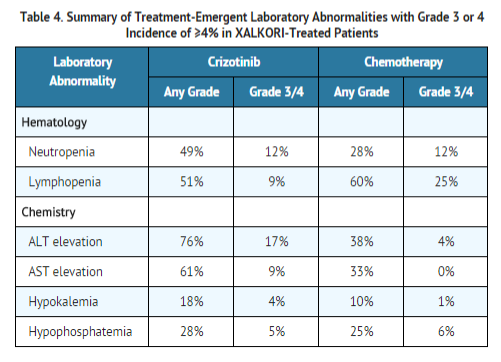
- Tables 3 and 4 summarize common Adverse Reactions and Laboratory Abnormalities in crizotinib-treated patients.
- Additional adverse reactions occurring at an overall incidence between 1% and 30% in patients treated with crizotinib included:
- Decreased appetite (27%)
- Fatigue (27%)
- Neuropathy (19%; dysesthesia, gait disturbance, hypoesthesia, muscular weakness, neuralgia, peripheral neuropathy, parasthesia, peripheral sensory neuropathy, polyneuropathy, burning sensation in skin)
- Rash (9%),
- ILD (4%; acute respiratory distress syndrome, ILD, pneumonitis), renal cyst (4%), and hepatic failure (1%).
ALK-positive metastatic NSCLC- Study 2
- The safety analysis population in Study 2 included 934 patients with ALK-positive metastatic NSCLC who received crizotinib in a clinical trial. *The median duration of treatment was 23 weeks.
- Dosing interruptions and reductions due to treatment-related adverse events occurred in 23% and 12% of patients, respectively.
- The rate of treatment-related adverse events resulting in permanent discontinuation was 5%.
- The most common adverse reactions (≥25%) included vision disorder (55%), nausea (51%), vomiting (46%), diarrhea (46%), edema (39%), constipation (38%), and fatigue (26%).
Description of selected adverse drug reactions
Vision disorders
- Most commonly:
- visual impairment
- photopsia
- blurred vision, or vitreous floaters, occurred in 691 (56%) patients across clinical trials (n=1225).
- The majority (99%) of these patients had Grade 1 or 2 visual adverse reactions.
- Across clinical studies, one patient had a treatment-related grade 3 vision abnormality.
- Based on the Visual Symptom Assessment Questionnaire (VSAQ-ALK), patients treated with crizotinib in Study 1 reported a higher incidence of visual disturbances compared to patients treated with chemotherapy. The onset of vision disorders generally started within the first week of drug administration.
- The majority of patients on the crizotinib arm in Study 1 (> 50%) reported visual disturbances; these visual disturbances occurred at a frequency of 4–7 days each week, lasted up to 1 minute, and had mild or no impact (scores 0 to 3 out of a maximum score of 10) on daily activities as captured in a patient questionnaire.
Neuropathy
- Neuropathy, most commonly sensory in nature, occurred in 235 (19%) of 1225 patients.
- Most events (95%) were Grade 1 or Grade 2 in severity.
Renal Cysts
- Renal cysts occurred in 7 (4%) patients treated with crizotinib and 1 (1%) patient treated with chemotherapy in Study 1.
- The majority of renal cysts in crizotinib-treated patients were complex. *Local cystic invasion beyond the kidney occurred, in some cases with imaging characteristics suggestive of abscess formation. However, across clinical trials no renal abscesses were confirmed by microbiology tests.
Postmarketing Experience
There is limited information regarding Crizotinib Postmarketing Experience in the drug label.
Drug Interactions
Drugs That May Increase Crizotinib Plasma Concentrations
- Coadministration of crizotinib with strong CYP3A inhibitors increases crizotinib plasma concentrations.
- Avoid concomitant use of strong CYP3A inhibitors, including but not limited to atazanavir, clarithromycin, indinavir, itraconazole, ketoconazole, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, troleandomycin, and voriconazole. *Avoid grapefruit or grapefruit juice which may also increase plasma concentrations of crizotinib.
- Exercise caution with concomitant use of moderate CYP3A inhibitors.
Drugs That May Decrease Crizotinib Plasma Concentrations
- Coadministration of crizotinib with strong CYP3A inducers decreases crizotinib plasma concentrations.
- Avoid concomitant use of strong CYP3A inducers, including but not limited to carbamazepine, phenobarbital, phenytoin, rifabutin, rifampin, and St. John's Wort.
Drugs Whose Plasma Concentrations May Be Altered By Crizotinib
- Crizotinib inhibits CYP3A both in vitro and in vivo.
- Avoid concomitant use of CYP3A substrates with narrow therapeutic range, including but not limited to alfentanil, cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus in patients taking crizotinib. *If concomitant use of these CYP3A substrates with narrow therapeutic range is required in patients taking crizotinib, dose reductions of the CYP3A substrates may be required due to adverse reactions.
Use in Specific Populations
Pregnancy
- Crizotinib can cause fetal harm when administered to a pregnant woman based on its mechanism of action.
- There are no adequate and well-controlled studies of crizotinib in pregnant women.
- In nonclinical studies in rats, crizotinib was embryotoxic and fetotoxic at exposures similar to those observed in humans at the recommended clinical dose of 250 mg twice daily.
- Crizotinib was administered to pregnant rats and rabbits during organogenesis to study the effects on embryo-fetal development.
- Postimplantation loss was increased at doses ≥ 50 mg/kg/day (approximately 0.6 times the AUC at the recommended human dose) in rats.
- No teratogenic effects were observed in rats at doses up to the maternally toxic dose of 200 mg/kg/day (approximately 2.7 times the AUC at the recommended human dose) or in rabbits at doses of up to 60 mg/kg/day (approximately 1.6 times the AUC at the recommended human dose), though fetal body weights were reduced at these doses.
- Advise women of childbearing potential to avoid becoming pregnant while receiving crizotinib.
- Women of childbearing potential who are receiving this drug, or partners of women of childbearing potential receiving this drug, should use adequate contraceptive methods during therapy and for at least 90 days after completing therapy.
- If this drug is used during pregnancy, or if the patient or their partner becomes pregnant while taking this drug, apprise the patient of the potential hazard to a fetus.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Crizotinib in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Crizotinib during labor and delivery.
Nursing Mothers
- It is not known whether crizotinib is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from crizotinib, consider whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- The safety and efficacy of crizotinib in pediatric patients has not been established.
- Decreased bone formation in growing long bones was observed in immature rats at 150 mg/kg/day following once daily dosing for 28 days (approximately 5.4 times the AUC in adult patients at the recommended human dose).
- Other toxicities of potential concern to pediatric patients have not been evaluated in juvenile animals.
Geriatic Use
- Of crizotinib treated patients in Study 1, 27 (16%) were 65 years or older, in Study 2, 152 (16%) were 65 years or older, and in Study 3, 16 (13%) were 65 years or older.
- No overall differences in safety or effectiveness were observed between these patients and younger patients.
Gender
- No clinically relevant effect of gender on the exposure of crizotinib based on the population pharmacokinetic analysis from Studies 1, 2 and 3.
Race
- No clinically relevant difference in the exposure of crizotinib between Asian patients (N=523) and non-Asian patients
Renal Impairment
- No starting dose adjustment is needed for patients with mild (creatinine clearance [CLcr] 60–89 mL/min) or moderate (CLcr 30–59 mL/min) renal impairment based on a population pharmacokinetic analysis.
- Increased exposure to crizotinib occurred in patients with severe renal impairment (CLcr <30 mL/min) not requiring dialysis. Administer crizotinib at a dose of 250 mg taken orally once daily in patients with severe renal impairment not requiring dialysis
Hepatic Impairment
- Crizotinib has not been studied in patients with hepatic impairment. As crizotinib is extensively metabolized in the liver, hepatic impairment is likely to increase plasma crizotinib concentrations.
- Clinical studies excluded patients with AST or ALT greater than 2.5 × ULN, or greater than 5 × ULN, if due to liver metastases.
- Patients with total bilirubin greater than 1.5 × ULN were also excluded. Therefore, use caution in patients with hepatic impairment
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Crizotinib in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Crizotinib in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
- Monitor with liver function tests including ALT and total bilirubin every 2 weeks during the first 2 months of treatment, then once a month.
- Monitor with electrocardiograms and electrolytes in patients who have a history of or predisposition for QTc prolongation, or who are taking medications that prolong QT.
- Monitor heart rate and blood pressure regularly, as it can cause bradycardia.
- Monitor complete blood counts including differential white blood cell counts monthly.
- Monitor patients for pulmonary symptoms indicative of ILD/pneumonitis.
IV Compatibility
There is limited information regarding the compatibility of Crizotinib and IV administrations.
Overdosage
- There have been no known cases of crizotinib overdose.
- There is no antidote for crizotinib.
Pharmacology
 | |
| Clinical data | |
|---|---|
| Trade names | crizotinib |
| Synonyms | PF-02341066 1066 |
| MedlinePlus | a612018 |
| [[Regulation of therapeutic goods |Template:Engvar data]] |
|
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 43% |
| Protein binding | 91% |
| Metabolism | Hepatic (CYP3A4/CYP3A5-mediated) |
| Elimination half-life | 42 hours |
| Excretion | Faeces (63%), urine (22%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C21H22Cl2FN5O |
| Molar mass | 450.337 g/mol |
| 3D model (JSmol) | |
| |
| |
| | |
Mechanism of Action
- Crizotinib is an inhibitor of receptor tyrosine kinases including ALK, Hepatocyte Growth Factor Receptor (HGFR, c-Met), ROS1 (c-ros), and Recepteur d'Origine Nantais (RON).
- Translocations can affect the ALK gene resulting in the expression of oncogenic fusion proteins.
- The formation of ALK fusion proteins results in activation and dysregulation of the gene's expression and signaling which can contribute to increased cell proliferation and survival in tumors expressing these proteins.
- Crizotinib demonstrated concentration-dependent inhibition of ALK, ROS1, and c-Met phosphorylation in cell-based assays using tumor cell lines and demonstrated antitumor activity in mice bearing tumor xenografts that expressed EML4- or NPM-ALK fusion proteins or c-Met.
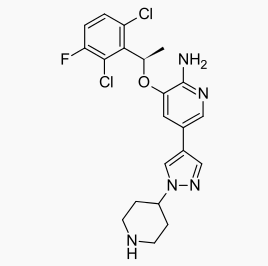
Structure
- The molecular formula for crizotinib is C21H22Cl2FN5O.
- The molecular weight is 450.34 Daltons.
- Crizotinib is described chemically as (R)-3-[1-(2,6-Dichloro-3-fluorophenyl)ethoxy]-5-[1-(piperidin-4-yl)-1H-pyrazol-4-yl]pyridin-2-amine.
The chemical structure of crizotinib is shown below:
- Crizotinib is a white to pale-yellow powder with a pKa of 9.4 (piperidinium cation) and 5.6 (pyridinium cation).
- The solubility of crizotinib in aqueous media decreases over the range pH 1.6 to pH 8.2 from greater than 10 mg/mL to less than 0.1 mg/mL.
- The log of the distribution coefficient (octanol/water) at pH 7.4 is 1.65.
Pharmacodynamics
Cardiac Electrophysiology
- The QT interval prolongation potential of crizotinib was assessed in all patients who received crizotinib 250 mg twice daily.
- Serial ECGs in triplicate were collected following a single dose and at steady state to evaluate the effect of crizotinib on QT intervals.
- Sixteen of 1167 patients (1.4%) were found to have QTcF (corrected QT by the Fridericia method) greater than or equal to 500 msec and 51 of 1136 patients (4.4%) had an increase from baseline QTcF greater than or equal to 60 msec by automated machine-read evaluation of ECG. A pharmacokinetic/pharmacodynamic analysis suggested a concentration-dependent increase in QTcF
Pharmacokinetics
Absorption
- Following a single oral dose, crizotinib was absorbed with median time to achieve peak concentration of 4 to 6 hours.
- Following crizotinib 250 mg twice daily, steady state was reached within 15 days and remained stable, with a median accumulation ratio of 4.8.
- Steady-state systemic exposure (Cmin and AUC) appeared to increase in a greater than dose proportional manner over the dose range of 200–300 mg twice daily.
- The mean absolute bioavailability of crizotinib was 43% (range: 32% to 66%) following a single 250 mg oral dose.
- A high-fat meal reduced crizotinib AUCinf and Cmax by approximately 14%. crizotinib can be administered with or without food.
Distribution
- The geometric mean volume of distribution (Vss) of crizotinib was 1,772 L following intravenous administration of a 50 mg dose, indicating extensive distribution into tissues from the plasma.
- Binding of crizotinib to human plasma proteins in vitro is 91% and is independent of drug concentration. In vitro studies suggested that crizotinib is a substrate for P-glycoprotein (P-gp). The blood-to-plasma concentration ratio is approximately 1.
Metabolism
- Crizotinib is predominantly metabolized by CYP3A4/5.
- The primary metabolic pathways in humans were oxidation of the piperidine ring to crizotinib lactam and O-dealkylation, with subsequent Phase 2 conjugation of O-dealkylated metabolites.
Elimination
- Following single doses of crizotinib, the mean apparent plasma terminal half-life of crizotinib was 42 hours in patients.
- Following the administration of a single 250 mg radiolabeled crizotinib dose to healthy subjects, 63% and 22% of the administered dose was recovered in feces and urine, respectively.
- Unchanged crizotinib represented approximately 53% and 2.3% of the administered dose in feces and urine, respectively.
- The mean apparent clearance (CL/F) of crizotinib was lower at steady state (60 L/h) after 250 mg twice daily than that after a single 250 mg oral dose (100 L/h), which was likely due to autoinhibition of CYP3A by crizotinib after multiple dosing.
Drug interactions
CYP3A inhibitors:
- Coadministration of a single 150 mg oral dose of crizotinib with ketoconazole (200 mg twice daily), a strong CYP3A inhibitor, increased crizotinib AUCinf and Cmax values by approximately 3.2-fold and 1.4-fold, respectively, compared to crizotinib alone. However, the magnitude of effect of CYP3A inhibitors on steady-state crizotinib exposure has not been evaluated.
CYP3A inducers:
- Coadministration of a single 250 mg oral dose of crizotinib with rifampin (600 mg once daily), a strong CYP3A inducer, decreased crizotinib AUCinf and Cmax by 82% and 69%, respectively, compared to crizotinib alone. However, the magnitude of effect of CYP3A inducers on steady-state crizotinib exposure has not been evaluated.
Gastric pH elevating medications:
- In healthy subjects, coadministration of a single 250 mg oral dose of crizotinib following administration of esomeprazole 40 mg daily for 5 days did not result in a clinically relevant change in crizotinib exposure (AUCinf decreased by 10% and no change in Cmax).
CYP3A substrates:
- Coadministration of crizotinib (250 mg twice daily for 28 days) in patients increased the AUCinf of oral midazolam 3.7-fold compared to midazolam alone, suggesting that crizotinib is a moderate inhibitor of CYP3A.
Other CYP substrates:
- In vitro studies suggest that clinical drug-drug interactions as a result of crizotinib-mediated inhibition of the metabolism of substrates for CYP1A2, CYP2C8, CYP2C9, CYP2C19, or CYP2D6 are unlikely to occur.
- Crizotinib is an inhibitor of CYP2B6 in vitro. Therefore, crizotinib may increase plasma concentrations of coadministered drugs that are predominantly metabolized by CYP2B6.
- An in vitro study suggests that clinical drug-drug interactions as a result of crizotinib-mediated induction of the metabolism of substrates for CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, or CYP3A are unlikely to occur.
UGT substrates:
- In vitro studies suggest that clinical drug-drug interactions as a result of crizotinib-mediated inhibition of the metabolism of drugs that are substrates for UGT1A1, UGT1A4, UGT1A6, UGT1A9 or UGT2B7 are unlikely to occur.
Substrates of transporters:
- Crizotinib inhibited P-glycoprotein (P-gp) in vitro at clinically relevant concentrations. Therefore, crizotinib has the potential to increase plasma concentrations of coadministered drugs that are substrates of P-gp.
- Crizotinib inhibited the hepatic uptake transporter, organic cation transporter 1 (OCT1), and renal uptake transporter, organic cation transporter 2 (OCT2), in vitro at clinically relevant concentrations. Therefore, crizotinib has the potential to increase plasma concentrations of coadministered drugs that are substrates of OCT1 or OCT2.
- Crizotinib did not inhibit the human hepatic uptake transport proteins OATP1B1 or OATP1B3, or the renal uptake transport proteins OAT1 or OAT3 in vitro at clinically relevant concentrations.
Effect on other transport proteins:
- Crizotinib did not inhibit the hepatic efflux bile salt export pump transporter (BSEP) in vitro at clinically relevant concentrations.
Specific populations
Hepatic Impairment:
- As crizotinib is extensively metabolized in the liver, hepatic impairment is likely to increase plasma crizotinib concentrations. However, crizotinib has not been studied in patients with hepatic impairment.
- Clinical studies excluded patients with ALT or AST greater than 2.5 × ULN or greater than 5 × ULN if due to liver metastases.
- Patients with total bilirubin greater than 1.5 × ULN were also excluded. *The population pharmacokinetic analysis using the data from Studies 1, 2 and 3 suggested that baseline total bilirubin (0.1 to 2.1 mg/dL) or AST levels (7 to 124 U/L) did not have a clinically relevant effect on the exposure of crizotinib.
Renal impairment:
- The pharmacokinetics of crizotinib were evaluated using a population pharmacokinetic analysis in patients with mild (CLcr 60–89 mL/min, N=433) and moderate (CLcr 30–59 mL/min, N=137) renal impairment enrolled in Studies 1, 2, and 3.
- Mild or moderate renal impairment has no clinically relevant effect on the exposure of crizotinib.
- A study was conducted in 7 patients with severe renal impairment (CLcr <30 mL/min) who did not require dialysis and 8 patients with normal renal function (CLcr ≥ 90 mL/min).
- All patients received a single 250 mg oral dose of crizotinib.
- The mean AUCinf for crizotinib increased by 79% and the mean Cmax increased by 34% in patients with severe renal impairment compared to those with normal renal function.
- Similar changes in AUCinf and Cmax were observed for the active metabolite of crizotinib.
Ethnicity:
- No clinically relevant difference in the exposure of crizotinib between Asian patients (N=523) and non-Asian patients (N=691).
Age:
- Age has no effect on the exposure of crizotinib based on the population pharmacokinetic analysis from Studies 1, 2 and 3.
Body weight and gender:
- No clinically relevant effect of body weight or gender on the exposure of crizotinib based on the population pharmacokinetic analysis from Studies 1, 2 and 3.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with crizotinib have not been conducted.
- Crizotinib was genotoxic in an in vitro micronucleus assay in Chinese Hamster Ovary cultures, in an in vitro human lymphocyte chromosome aberration assay, and in in vivo rat bone marrow micronucleus assays.
- Crizotinib was not mutagenic in vitro in the bacterial reverse mutation (Ames) assay.
- No specific studies with crizotinib have been conducted in animals to evaluate the effect on fertility; however, crizotinib is considered to have the potential to impair reproductive function and fertility in humans based on findings in repeat-dose toxicity studies in the rat.
- Findings observed in the male reproductive tract included testicular pachytene spermatocyte degeneration in rats given greater than or equal to 50 mg/kg/day for 28 days (greater than 1.7 times the AUC at the recommended human dose). *Findings observed in the female reproductive tract included single-cell necrosis of ovarian follicles of a rat given 500 mg/kg/day (approximately 10 times the recommended human daily dose on a mg/m2 basis) for 3 days.
Clinical Studies
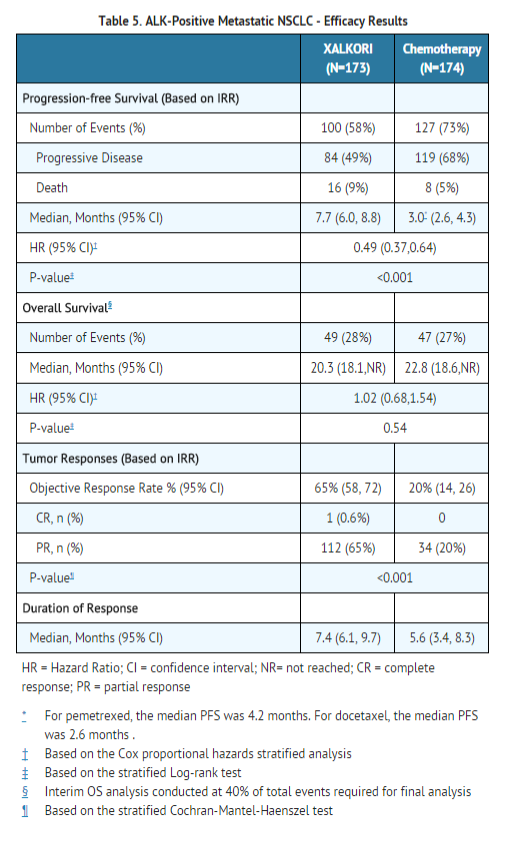
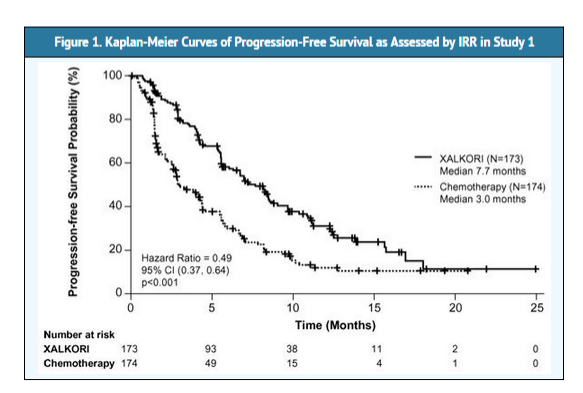
ALK-positive metastatic NSCLC-Study 1
- The efficacy and safety of crizotinib as monotherapy for the treatment of 347 patients with metastatic ALK-positive NSCLC, previously treated with one platinum-based chemotherapy regimen, was demonstrated in a randomized, multicenter, open-label, active-controlled study (Study 1).
- The major efficacy outcome was progression-free survival (PFS) as assessed by independent radiology review (IRR).
- Additional efficacy outcomes included objective response rate (ORR) as assessed by IRR and overall survival (OS).
- Patients were randomized to receive crizotinib 250 mg orally twice daily (n=173) or chemotherapy (n=174).
- Chemotherapy consisted of pemetrexed 500 mg/m2 (if pemetrexed naïve; n=99) or docetaxel 75 mg/m2 (n=72) intravenously (IV) every 21 days. *Patients in both treatment arms continued treatment until documented disease progression, intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit.
- Randomization was stratified by ECOG performance status (0–1, 2), brain metastases (present, absent), and prior EGFR tyrosine kinase inhibitor treatment (yes, no).
- Patients were required to have ALK-positive NSCLC as identified by the FDA-approved assay, Vysis ALK Break-Apart FISH Probe Kit, prior to randomization. A total of 112 (64%) patients randomized to the chemotherapy arm subsequently received crizotinib after disease progression.
- The demographic characteristics of the overall study population were 56% female, median age of 50 years, baseline ECOG performance status 0 (39%) or 1 (52%), 52% White and 45% Asian, 4% current smokers, 33% past-smokers, and 63% never smokers.
- The disease characteristics were metastatic disease in at least 95% of patients and at least 93% of patients' tumors were classified as adenocarcinoma histology.
- Study 1 demonstrated a statistically significant improvement in PFS in the patients treated with crizotinib. Table 5 and Figure 1 summarize the efficacy results.
Single-arm studies in ALK-positive metastatic NSCLC- Studies 2 and 3
- The safety and anti-tumor activity of single-agent crizotinib in the treatment of metastatic ALK-positive NSCLC was demonstrated in two multinational, single-arm studies (Studies 2 and 3).
- The major outcome in both studies was investigator-assessed ORR according to RECIST.
- Patients in both studies received 250 mg of crizotinib orally twice daily.
- In Study 2 (n=934) the demographic characteristics were 57% female, median age of 52 years, baseline ECOG performance status of 0/1 (82%) or 2/3 (18%), 52% White and 44% Asian, 4% current smokers, 30% past-smokers, and 66% never smokers.
- The disease characteristics were 92% metastatic; 94% of the cancers were classified as adenocarcinoma histology.
- Of the 934 ALK-positive metastatic NSCLC patients who received crizotinib in Study 2, 765 were ALK-positive as identified by Vysis ALK Break-Apart FISH Probe Kit and evaluable for response; demographic characteristics were similar to that of the overall population for this study.
- The median duration of treatment was 5.5 months. Based on investigator assessments, there were 8 complete and 357 partial responses for an ORR of 48% (95% CI: 44, 51) and the median DR was 11.0 months.
- In Study 3 (n=119) the demographic characteristics were 50% female, median age of 51 years, baseline ECOG performance status of 0 (35%) or 1 (53%), 62% White and 29% Asian, less than 1% were current smokers, 27% past-smokers, and 72% never smokers.
- The disease characteristics were 96% metastatic, 98% of the cancers were classified as adenocarcinoma histology, and 13% had no prior systemic therapy for metastatic disease.
- In Study 3, 119 patients with metastatic ALK-positive NSCLC were treated with crizotinib with a median duration of treatment of 32 weeks. Based on investigator assessments, the ORR was 61% (95% CI: 52%, 70%) and the median DR was 11.1 months.
How Supplied
250 mg capsules
- Hard gelatin capsule with pink opaque cap and body, printed with black ink "CRZ 250" on the body; available in:
- Bottles of 60 capsules: NDC 0069-8140-20
200 mg capsules
- Hard gelatin capsule with pink opaque cap and white opaque body, printed with black ink "CRZ 200" on the body; available in:
- Bottles of 60 capsules: NDC 0069-8141-20
Storage
- Store at room temperature 20° to 25°C (68° to 77°F); excursions permitted between 15° to 30°C (59° to 86°F)
Images
Drug Images
{{#ask: Page Name::Crizotinib |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
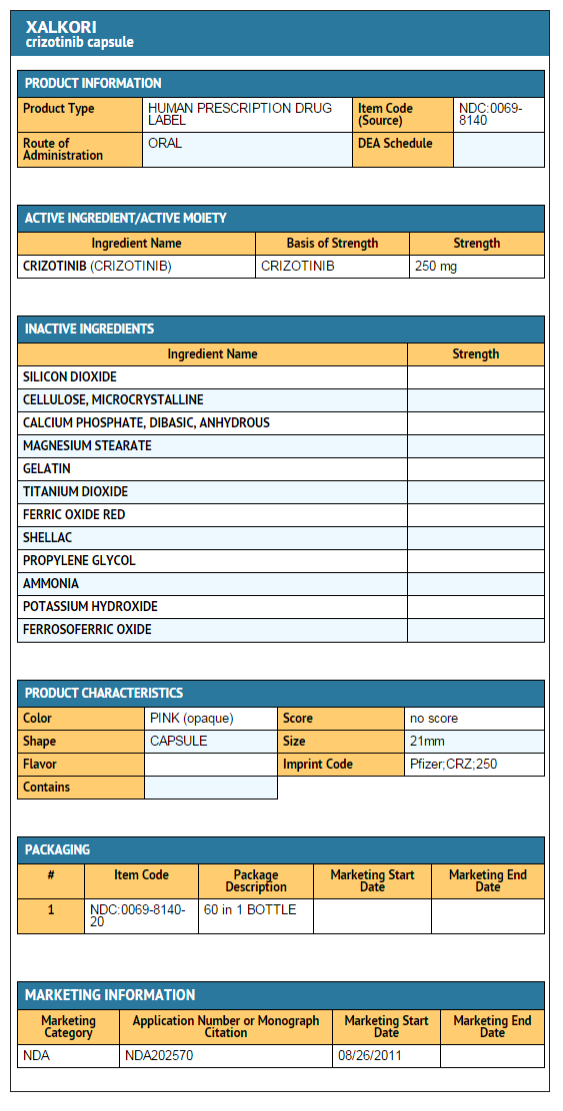
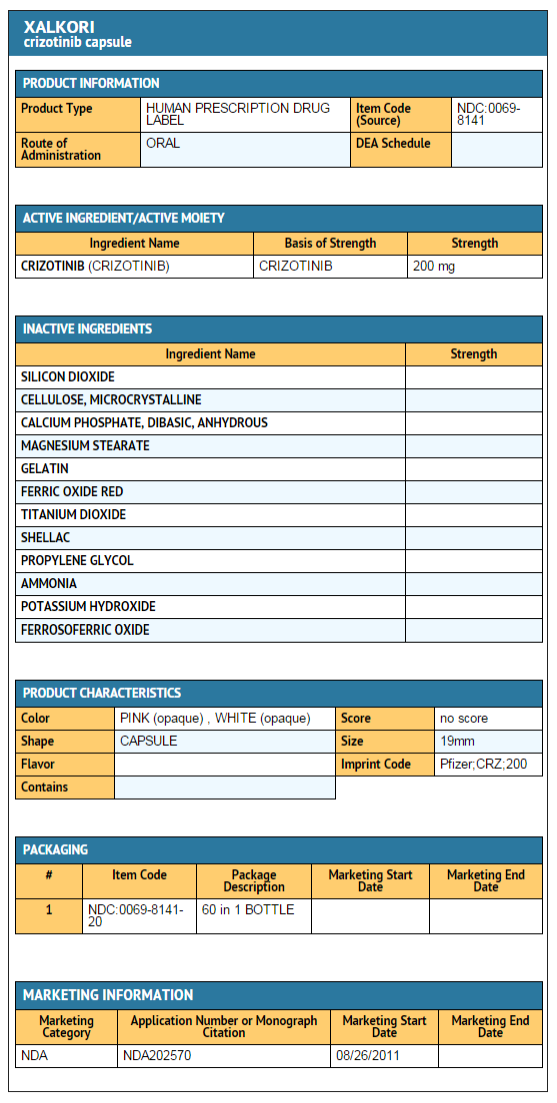
{{#ask: Label Page::Crizotinib |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Inform patients of the symptoms of hepatotoxicity, and that they should be reported immediately.
- Advise patients to immediately report any new or worsening pulmonary symptoms.
- Inform patients that symptoms of bradycardia including dizziness, lightheadedness, and syncope can occur while taking crizotinib.
- Advise patients to report these symptoms and to inform their physician about the use of any heart or blood pressure medications.
- Inform patients that nausea, diarrhea, vomiting, and constipation are the most commonly reported gastrointestinal adverse events occurring in patients who received crizotinib.
- Nausea and vomiting began most commonly during the first few days of treatment.
- Inform patients that visual changes such as perceived flashes of light, blurry vision, light sensitivity, and floaters are commonly reported adverse events and may occur while driving or operating machinery.
- The onset of visual disorders most commonly occurs during the first week of treatment.
- Inform patients to avoid grapefruit or grapefruit juice while taking crizotinib.
- Advise patients to inform their health care providers of all concomitant medications, including prescription medicines, over-the-counter drugs, vitamins, and herbal products.
- Advise patients to take crizotinib with or without food and swallow crizotinib capsules whole.
- If a patient misses a dose, advise the patient to take it as soon as remembered unless it is less than 6 hours until the next dose, in which case, advise the patient not to take the missed dose.
- If a patient vomits after taking a dose of crizotinib, advise the patient not to take an extra dose, but to take the next dose at the regular time.
- Inform patients of childbearing potential to use adequate contraceptive methods during therapy and for at least 90 days after completing therapy. *Advise patients to inform their doctor if they or their partners are pregnant or think they may be pregnant. Also advise patients not to breastfeed while taking crizotinib.
Precautions with Alcohol
Alcohol-Crizotinib interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Crizotinib[1]
Look-Alike Drug Names
There is limited information regarding Crizotinib Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Crizotinib |Label Name=Crizotinib package 1.png
}}
{{#subobject:
|Label Page=Crizotinib |Label Name=Crizotinib Package 2.png
}}
- Pages with script errors
- Articles with changed CASNo identifier
- Articles with changed KEGG identifier
- Articles with changed EBI identifier
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Drug has EMA link
- Drugboxes which contain changes to verified fields
- Drugboxes which contain changes to watched fields
- Drug
- Chemotherapeutic agents