Amobarbital sodium
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Stefano Giannoni [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Amobarbital sodium is a barbiturate that is FDA approved for the treatment of insomnia.Also it is use as a sedative and for preanesthesic purpose.. Common adverse reactions include dizziness, headache, somnolence and confusion.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
The dose of amobarbital sodium must be individualized with full knowledge of its particular characteristics and recommended rate of administration. Factors of consideration are the patient’s age, weight, and condition. The maximum single dose for an adult is 1 g.
Sedative
- 30 to 50 mg given 2 or 3 times daily.
Insomnia
- It is use as an Hypnotic for the short-term treatment of insomnia, since it appears to lose its effectiveness for sleep induction and sleep maintenance after 2 weeks.
- 65 to 200 mg at bedtime.
Preanesthetic
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Amobarbital sodium in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Amobarbital sodium in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Amobarbital sodium FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Amobarbital sodium in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Amobarbital sodium in pediatric patients.
Contraindications
- Hypersensitivity to barbiturates
- Patients with a history of manifest or latent porphyria
- Patients with marked impairment of liver function or respiratory disease in which dyspnea or obstruction is evident
Warnings
Habit Forming
- Amobarbital sodium may be habit forming.
- Tolerance, psychological and physical dependence may occur with continued use *Patients who have psychological dependence on barbiturates may increase the dosage or decrease the dosage interval without consulting a physician and may subsequently develop a physical dependence on barbiturates.
- In order to minimize the possibility of overdosage or the development of dependence, the prescribing and dispensing of sedative-hypnotic barbiturates should be limited to the amount required for the interval until the next appointment.
- Abrupt cessation after prolonged use in a person who is dependent on the drug may result in withdrawal symptoms, including delirium, convulsions, and possibly death.
- Barbiturates should be withdrawn gradually from any patient known to be taking excessive doses over long periods of time.
Intravenous Administration
- Too rapid administration may cause respiratory depression, apnea, laryngo- spasm, or vasodilation with fall in blood pressure.
Acute or Chronic Pain
- Caution should be exercised when barbiturates are administered to patients with acute or chronic pain, because paradoxical excitement could be induced or important symptoms could be masked. However, the use of barbiturates as sedatives in the postoperative surgical period and as adjuncts to cancer chemotherapy is well established.
Usage in Pregnancy
- Barbiturates can cause fetal damage when administered to a pregnant woman.
*Retrospective, case-controlled studies have suggested a connection between the maternal consumption of barbiturates and a higher than expected incidence of fetal abnormalities. - Barbiturates readily cross the placental barrier and are distributed throughout fetal tissues; the highest concentrations are found in the placenta, fetal liver, and brain.
- Fetal blood levels approach maternal blood levels following parenteral administration.
- Withdrawal symptoms occur in infants born to women who receive barbiturates throughout the last trimester of pregnancy.
- If amobarbital sodium is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
Synergistic Effects
- The concomitant use of alcohol or other CNS depressants may produce additive CNS- depressant effects.
Adverse Reactions
Clinical Trials Experience
The following adverse reactions and their incidence were compiled from surveillance of thousands of hospitalized patients who received barbiturates. Because such patients may be less aware of certain of the milder adverse effects of barbiturates, the incidence of these reactions may be somewhat higher in fully ambulatory patients.
More than 1 in 100 Patients
- The most common adverse reaction, estimated to occur at a rate of 1 to 3 patients per 100, is the following:
Nervous System
Less than 1 in 100 Patients
- Adverse reactions estimated to occur at a rate of less than 1 in 100 patients are listed below, grouped by organ system and by decreasing order of occurrence:
Nervous System
- Agitation
- Confusion
- Hyperkinesia
- Ataxia
- CNS depression
- Nightmares
- Nervousness
- Psychiatric disturbance
- Hallucinations
- Insomnia
- Anxiety
- Dizziness
- Abnormality in thinking
Respiratory System
- Hypoventilation
- Apnea
- Postoperative atelectasis
Cardiovascular System
Digestive System
Other Reported Reactions
- Headache
- Injection site reactions
- Hypersensitivity reactions (angioedema, skin rashes, exfoliative dermatitis)
- Fever
- Liver damage
- Megaloblastic anemia following chronic phenobarbital use
Postmarketing Experience
There is limited information regarding Amobarbital sodium Postmarketing Experience in the drug label.
Drug Interactions
Most reports of clinically significant drug interactions occurring with the barbiturates have involved phenobarbital. However, the application of these data to other barbiturates appears valid and warrants serial blood level determinations of the relevant drugs when there are multiple therapies.
Anticoagulants
- Phenobarbital lowers the plasma levels of dicumarol and causes a decrease in anticoagulant activity as measured by the prothrombin time.
- Barbiturates can induce hepatic microsomal enzymes, resulting in increased metabolism and decreased anticoagulant response of oral anticoagulants (eg, warfarin, acenocoumarol, dicumarol, and phenprocoumon).
- Patients stabilized on anticoagulant therapy may require dosage adjustments if barbiturates are added to or withdrawn from their dosage regimen.
Corticosteroids
- Barbiturates appear to enhance the metabolism of exogenous corticosteroids, probably through the induction of hepatic microsomal enzymes.
- Patients stabilized on corticosteroid therapy may require dosage adjustments if barbiturates are added to or withdrawn from their dosage regimen.
Griseofulvin
- Phenobarbital appears to interfere with the absorption of orally administered griseofulvin, thus decreasing its blood level.
- The effect of the resultant decreased blood levels of griseofulvin on therapeutic response has not been established. However, it would be preferable to avoid concomitant administration of these drugs.
Doxycycline
- Phenobarbital has been shown to shorten the half-life of doxycycline for as long as 2 weeks after barbiturate therapy is discontinued.
- This mechanism is probably through the induction of hepatic microsomal enzymes that metabolize the antibiotic.
- If amobarbital sodium and doxycycline are administered concurrently, the clinical response to doxycycline should be monitored closely.
Phenytoin, Sodium Valproate, Valproic Acid
- The effect of barbiturates on the metabolism of phenytoin appears to be variable.
- Some investigators report an accelerating effect, whereas others report no effect. Because the effect of barbiturates on the metabolism of phenytoin is not predictable, phenytoin and barbiturate blood levels should be monitored more frequently if these drugs are given concurrently.
- Sodium valproate and valproic acid appear to increase the amobarbital sodium serum levels; therefore, amobarbital sodium blood levels should be closely monitored and appropriate dosage adjustments made as clinically indicated.
CNS Depressants
- The concomitant use of other CNS depressants, including other sedatives or hypnotics, antihistamines, tranquilizers, or alcohol, may produce additive depressant effects.
Monoamine Oxidase Inhibitors (MAOIs)
- MAOIs prolong the effects of barbiturates, probably because metabolism of the barbiturate is inhibited.
Estradiol, Estrone, Progesterone, and Other Steroidal Hormones
- Pretreatment with or concurrent administration of phenobarbital may decrease the effect of estradiol by increasing its metabolism.
- There have been reports of patients treated with antiepileptic drugs (eg, phenobarbital) who become pregnant while taking oral contraceptives.
- An alternate contraceptive method might be suggested to women taking barbiturates.
Use in Specific Populations
Pregnancy
- Barbiturates can cause fetal damage when administered to a pregnant woman.
*Retrospective, case-controlled studies have suggested a connection between the maternal consumption of barbiturates and a higher than expected incidence of fetal abnormalities. - Barbiturates readily cross the placental barrier and are distributed throughout fetal tissues; the highest concentrations are found in the placenta, fetal liver, and brain.
- Fetal blood levels approach maternal blood levels following parenteral administration.
- Withdrawal symptoms occur in infants born to women who receive barbiturates throughout the last trimester of pregnancy.
- If amobarbital sodium is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
Nonteratogenic Effects
- Reports of infants suffering from long-term barbiturate exposure in utero included the acute withdrawal syndrome of seizures and hyperirritability from birth to a delayed onset of up to 14 days
Pregnancy Category (AUS): C
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Amobarbital sodium in women who are pregnant.
Labor and Delivery
- Hypnotic doses of barbiturates do not appear to impair uterine activity significantly during labor.
- Full anesthetic doses of barbiturates decrease the force and frequency of uterine contractions.
- Administration of sedative-hypnotic barbiturates to the mother during labor may result in respiratory depression in the newborn.
- Premature infants are particularly susceptible to the depressant effects of barbiturates.
- If barbiturates are used during labor and delivery, resuscitation equipment should be available.
- Data are not available to evaluate the effect of barbiturates when forceps delivery or other intervention is necessary or to determine the effect of barbiturates on the later growth, development, and functional maturation of the child.
Nursing Mothers
- Caution should be exercised when amobarbital sodium is administered to a nursing woman because small amounts of barbiturates are excreted in the milk.
Pediatric Use
- Safety and effectiveness have not been established in children below the age of 6 years.
- Children, barbiturates repeatedly produce excitement rather than depression.
Geriatic Use
- Elderly or debilitated patients may react to barbiturates with marked excitement, depression, or confusion.
Gender
There is no FDA guidance on the use of Amobarbital sodium with respect to specific gender populations.
Race
There is no FDA guidance on the use of Amobarbital sodium with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Amobarbital sodium in patients with renal impairment.
Hepatic Impairment
- Barbiturates should be administered with caution and initially in reduced doses.
- Barbiturates should not be administered to patients showing the premonitory signs of hepatic coma.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Amobarbital sodium in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Amobarbital sodium in patients who are immunocompromised.
Administration and Monitoring
Administration
Intramuscular Use
- Intramuscular injection of the sodium salts of barbiturates should be made deeply into a large muscle.
- The average intramuscular dose ranges from 65 mg to 0.5 g.
- A volume of 5 mL (irrespective of concentration) should not be exceeded at any one site because of possible tissue irritation.
- Twenty percent solutions may be used so that a small volume can contain a large dose.
- After IM injection of a hypnotic dose, the patient’s vital signs should be monitored.
- Superficial intramuscular or subcutaneous injections may be painful and may produce sterile abscesses or sloughs.
Intravenous Use
- Intravenous injection is restricted to conditions in which other routes are not feasible, either because the patient is unconscious (as in cerebral hemorrhage, eclampsia, or status epilepticus), because the patient resists (as in delirium), or because prompt action is imperative.
- Slow IV injection is essential, and patients should be carefully observed during administration.
- This requires that blood pressure, respiration, and cardiac function be maintained, vital signs be recorded and equipment for resuscitation and artificial ventilation be available.
- The rate of IV injection for adults should not exceed 50 mg/min to prevent sleep or sudden respiratory depression.
- The final dosage is determined to a great extent by the patient’s reaction to the slow administration of the drug.
Monitoring
- After IM injection of a hypnotic dose, the patient’s vital signs should be monitored.
- Prolonged therapy with barbiturates should be accompanied by periodic evaluation of organ systems, including hematopoietic, renal, and hepatic systems
IV Compatibility
- Solutions of amobarbital sodium should be made up aseptically with Sterile Water for Injection.
- The accompanying table will aid in preparing solutions of various concentrations.
- Ordinarily, a 10% solution is used.
- After Sterile Water for Injection is added, the vial should be rotated to facilitate solution of the powder.
- Do not shake the vial.
- Several minutes may be required for the drug to dissolve completely, but under no circumstances should a solution be injected if it has not become absolutely clear within 5 minutes. Also, a solution that forms a precipitate after clearing should not be used.
- Amobarbital sodium hydrolyzes in solution or on exposure to air.
- Not more than 30 minutes should elapse from the time the vial is opened until its contents are injected.
- Prior to administration, parenteral drug products should be inspected visually for particulate matter and discoloration whenever solution containers permit.

Overdosage
- The toxic dose of barbiturates varies considerably.
- In general, an oral dose of 1 g of most barbiturates produces serious poisoning in an adult.
- Toxic effects and fatalities have occurred following overdoses of amobarbital sodium alone and in combination with other CNS depressants.
- Death commonly occurs after 2 to 10 g of ingested barbiturate.
- The sedated, therapeutic blood levels of amobarbital range between 2 to 10 mcg/mL; the usual lethal blood level ranges from 40 to 80 mcg/mL.
- Barbiturate intoxication may be confused with alcoholism, bromide intoxication, and various neurologic disorders.
- Potential tolerance must be considered when evaluating significance of dose and plasma concentration.
Signs and Symptoms
- Symptoms of oral overdose may occur within 15 minutes beginning with CNS depression, absent or sluggish reflexes, underventilation, hypotension, and hypothermia and may progress to pulmonary edema and death.
- Hemorrhagic blisters may develop, especially at pressure points.
- In extreme overdose, all electrical activity in the brain may cease, in which case a “flat” EEG normally equated with clinical death cannot be accepted.
- This effect is fully reversible unless hypoxic damage occurs.
- Consideration should be given to the possibility of barbiturate intoxication even in situations that appear to involve trauma.
- Complications such as pneumonia, pulmonary edema, cardiac arrhythmias, congestive heart failure, and renal failure may occur.
- Uremia may increase CNS sensitivity to barbiturates if renal function is impaired.
- Differential diagnosis should include hypoglycemia, head trauma, cerebrovascular accidents, convulsive states, and diabetic coma.
Treatment
- To obtain up-to-date information about the treatment of overdose, a good resource is your certified Regional Poison Control Center.
- In managing overdosage, consider the possibility of multiple drug overdoses, interaction among drugs, and unusual drug kinetics in your patient.
- Protect the patient’s airway and support ventilation and perfusion. *Meticulously monitor and maintain, within acceptable limits, the patient’s vital signs, blood gases, serum electrolytes, etc.
- Absorption of drugs from the gastrointestinal tract may be decreased by giving activated charcoal, which, in many cases, is more effective than emesis or lavage; consider charcoal instead of or in addition to gastric emptying. *Repeated doses of charcoal over time may hasten elimination of some drugs that have been absorbed.
- Safeguard the patient’s airway when employing gastric emptying or charcoal.
- Diuresis and peritoneal dialysis are of little value; hemodialysis and hemoperfusion enhance drug clearance and should be considered in serious poisoning.
- If the patient has chronically abused sedatives, withdrawal reactions may be manifest following acute overdose.
Pharmacology
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Pregnancy category |
|
| Routes of administration | Oral, IM, IV, Rectal |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | Hepatic |
| Elimination half-life | 8–42 hours |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C11H18N2O3 |
| Molar mass | 226.272 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Mechanism of Action
- Barbiturates are capable of producing all levels of CNS mood alteration, from excitation to mild sedation, hypnosis, and deep coma.
- Overdosage can produce death.
- In high enough therapeutic doses, barbiturates induce anesthesia.
- Barbiturates depress the sensory cortex, decrease motor activity, alter cerebellar function, and produce drowsiness, sedation, and hypnosis.
- Barbiturate-induced sleep differs from physiologic sleep.
- Sleep laboratory studies have demonstrated that barbiturates reduce the amount of time spent in the rapid eye movement (REM) phase of sleep or the dreaming stage.
- Also, Stages III and IV sleep are decreased.
- Following abrupt cessation of barbiturates used regularly, patients may experience markedly increased dreaming, nightmares, and/or insomnia. Therefore, withdrawal of a single therapeutic dose over 5 or 6 days has been recommended to lessen the REM rebound and disturbed sleep that contribute to the drug withdrawal syndrome (for example, the dose should be decreased from 3 to 2 doses/day for 1 week).
- In studies, secobarbital sodium and pentobarbital sodium have been found to lose most of their effectiveness for both inducing and maintaining sleep by the end of 2 weeks of continued drug administration, even with the use of multiple doses.
- As with secobarbital sodium and pentobarbital sodium, other barbiturates (including amobarbital) might be expected to lose their effectiveness for inducing and maintaining sleep after about 2 weeks.
- The short-, intermediate-, and to a lesser degree, long-acting barbiturates have been widely prescribed for treating insomnia. Although the clinical literature abounds with claims that the short-acting barbiturates are superior for producing sleep whereas the intermediate-acting compounds are more effective in maintaining sleep, controlled studies have failed to demonstrate these differential effects. Therefore, as sleep medications, the barbiturates are of limited value beyond short-term use.
- Barbiturates have little analgesic action at subanesthetic doses. Rather, in subanesthetic doses, these drugs may increase the reaction to painful stimuli.
- All barbiturates exhibit anticonvulsant activity in anesthetic doses. However, of the drugs in this class, only phenobarbital, mephobarbital, and metharbital are effective as oral anticonvulsants in subhypnotic doses.
- Barbiturates are respiratory depressants, and the degree of respiratory depression is dependent upon the dose.
- With hypnotic doses, respiratory depression produced by barbiturates is similar to that which occurs during physiologic sleep and is accompanied by a slight decrease in blood pressure and heart rate.
- Studies in laboratory animals have shown that barbiturates cause reduction in the tone and contractility of the uterus, ureters, and urinary bladder. However, concentrations of the drugs required to produce this effect in humans are not reached with sedative-hypnotic doses.
Structure
- Amobarbital sodium is a white, friable, granular powder that is odorless, has a bitter taste, and is hygroscopic.
- It is very soluble in water, soluble in alcohol, and practically insoluble in ether and chloroform. Amobarbital sodium is sodium 5-ethyl-5-isopentylbarbiturate and has the empirical formula C11H17N2NaO3Its molecular weight is 248.26.
It has the following structural formula:

Pharmacodynamics
There is limited information regarding Amobarbital sodium Pharmacodynamics in the drug label.
Pharmacokinetics
- Barbiturates are absorbed in varying degrees following oral or parenteral administration.
- The salts are more rapidly absorbed than are the acids.
- The rate of absorption is increased if the sodium salt is ingested as a dilute solution or taken on an empty stomach.
- The onset of action for oral administration of barbiturates varies from 20 to 60 minutes.
- For intramuscular (IM) administration, the onset of action is slightly faster.
- Following intravenous (IV) administration, the onset of action ranges from almost immediately for pentobarbital sodium to 5 minutes for phenobarbital sodium.
- Maximal CNS depression may not occur until 15 minutes or more after IV administration for phenobarbital sodium.
- Duration of action, which is related to the rate at which the barbiturates are redistributed throughout the body, varies among persons and in the same person from time to time.
- Amobarbital sodium, an intermediate-acting barbiturate, is a CNS depressant. *For the oral form, the onset of sedative and hypnotic action is 3/4 to 1 hour, with a duration of action ranging from 6 to 8 hours.
- These values should serve as a guide but not be used to predict exact duration of effect.
- No studies have demonstrated that the different routes of administration are equivalent with respect to bioavailability.
- Barbiturates are weak acids that are absorbed and rapidly distributed to all tissues and fluids, with high concentrations in the brain, liver, and kidneys.
- Lipid solubility of the barbiturates is the dominant factor in their distribution within the body.
- The more lipid soluble the barbiturate, the more rapidly it penetrates all tissues of the body.
- Barbiturates are bound to plasma and tissue proteins to a varying degree, with the degree of binding increasing directly as a function of lipid solubility.
- Phenobarbital has the lowest lipid solubility, lowest plasma binding, lowest brain protein binding, the longest delay in onset of activity, and the longest duration of action.
- At the opposite extreme is secobarbital, which has the highest lipid solubility, highest plasma protein binding, highest brain protein binding, the shortest delay in onset of activity, and the shortest duration of action. *Amobarbital sodium is classified as an intermediate barbiturate.
- The plasma half-life for amobarbital sodium in adults ranges between 16 and 40 hours, with a mean of 25 hours.
- Barbiturates are metabolized primarily by the hepatic microsomal enzyme system, and the metabolic products are excreted in the urine and, less commonly, in the feces.
- Only a negligible amount of amobarbital sodium is eliminated unchanged in the urine.
Nonclinical Toxicology
Carcinogenesis
Animal Data
Phenobarbital sodium is carcinogenic in mice and rats after lifetime adminis- tration. In mice, it produced benign and malignant liver cell tumors. In rats, benign liver cell tumors were observed very late in life.
Human Data
In a 29-year epidemiologic study of 9,136 patients who were treated on an anticonvulsant protocol that included phenobarbital, results indicated a higher than normal incidence of hepatic carcinoma. Previously, some of these patients had been treated with thorotrast, a drug that is known to produce hepatic carcinomas. Thus, this study did not provide sufficient evidence that phenobarbital sodium is carcinogenic in humans. A retrospective study of 84 children with brain tumors matched to 73 normal controls and 78 cancer controls (malignant disease other than brain tumors) suggested an association between exposure to barbiturates prenatally and an increased incidence of brain tumors.
Clinical Studies
There is limited information regarding Amobarbital sodium Clinical Studies in the drug label.
How Supplied
- Amobarbital sodium Vials 0.5 g (dry powder) are available as follows:
1 UNIT-PACK NDC 42998-303-01
Storage
- Store at 59° to 86°F (15° to 30°C).
Images
Drug Images
{{#ask: Page Name::Amobarbital sodium |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
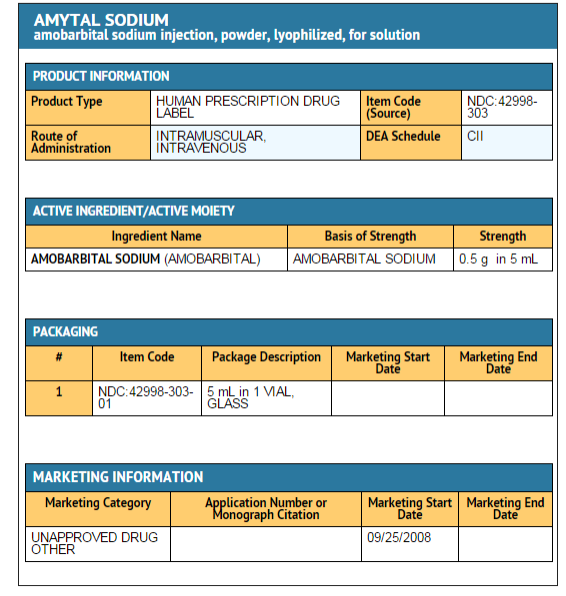
{{#ask: Label Page::Amobarbital sodium |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
The following information should be given to patients receiving barbiturates.
- The use of barbiturates carries with it an associated risk of psychological and/or physical dependence.
- Barbiturates may impair the mental and/or physical abilities required for the performance of potentially hazardous tasks, such as driving a car or operating machinery.
- The patient should be cautioned accordingly.
- Alcohol should not be consumed while taking barbiturates.
- The concurrent use of the barbiturates with other CNS depressants (eg, alcohol, narcotics, tranquilizers, and antihistamines) may result in additional CNS-depressant effects.
Precautions with Alcohol
- Alcohol should not be consumed while taking barbiturates. The concurrent use of the barbiturates with other CNS depressants (eg, alcohol, narcotics, tranquilizers, and antihistamines) may result in additional CNS-depressant effects.
Brand Names
- Amytal[1]
Look-Alike Drug Names
There is limited information regarding Amobarbital sodium Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Amobarbital sodium |Label Name=Amobarbital package.png
}}