Tuberculosis differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
Mohamed riad (talk | contribs) |
Mohamed riad (talk | contribs) |
||
| Line 281: | Line 281: | ||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
Pulmonary tuberculosis must be | Pulmonary tuberculosis must be distinguished from other cavitary lung lesions. | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 297: | Line 297: | ||
*Chronic smokers | *Chronic smokers | ||
*Presents with a [[low-grade fever]], absence of [[leukocytosis]], systemic complaints [[weight loss]], [[fatigue]] | *Presents with a [[low-grade fever]], absence of [[leukocytosis]], systemic complaints [[weight loss]], [[fatigue]] | ||
*Absence of factors that | *Absence of predisposing factors that lead to [[gastric content aspiration]], no response to [[antibiotics]] within 10 days | ||
*[[Hemoptysis]] is commonly associated with [[bronchogenic carcinoma]] | *[[Hemoptysis]] is commonly associated with [[bronchogenic carcinoma]] | ||
| | | | ||
| Line 308: | Line 308: | ||
*Pulmonary [[Tuberculosis, pulmonary|Tuberculosis]] | *Pulmonary [[Tuberculosis, pulmonary|Tuberculosis]] | ||
| | | | ||
*Mostly in endemic areas | *Mostly in [[endemic]] areas | ||
*Symptoms include [[productive cough]], [[ | *Symptoms include [[productive cough]], [[fever]], [[night sweats]], and [[weight loss]] | ||
| | | | ||
*CXR and CT | *CXR and CT show [[Internal|cavities]] in the upper lobe of the lung | ||
| | | | ||
*[[Sputum]] smear-positive for [[acid-fast bacilli]] and nucleic acid amplification tests (NAAT) are used on sputum or any sterile fluid for rapid diagnosis and is positive for mycobacteria. | *[[Sputum]] smear-positive for [[acid-fast bacilli]] and nucleic acid amplification tests ([[NAAT]]) are used on sputum or any sterile fluid for rapid diagnosis and is positive for mycobacteria. | ||
|- | |- | ||
| | | | ||
| Line 319: | Line 319: | ||
| | | | ||
*Any age group | *Any age group | ||
*Acute, [[fulminant]] life threating complication of | *Acute, [[fulminant]] life threating complication of previous infection | ||
*>100.4 °F fever, with [[Hemodynamically unstable|hemodynamic]] instability | *>100.4 °F fever, with [[Hemodynamically unstable|hemodynamic]] instability | ||
*Worsening [[pneumonia]]-like symptoms | *Worsening [[pneumonia]]-like symptoms | ||
| Line 332: | Line 332: | ||
*Loculated [[empyema]] | *Loculated [[empyema]] | ||
| | | | ||
*Children and elderly are at risk | *Children and elderly are at high risk | ||
*Pleuritic [[chest pain]], [[dry cough]], [[fever]] with chills | *Pleuritic [[chest pain]], [[dry cough]], [[fever]] with chills | ||
| Line 344: | Line 344: | ||
*[[Granulomatosis with polyangiitis]] ([[Wegener's granulomatosis|Wegener's]])<ref name="pmid10377211">{{cite journal |vauthors=Langford CA, Hoffman GS |title=Rare diseases.3: Wegener's granulomatosis |journal=Thorax |volume=54 |issue=7 |pages=629–37 |year=1999 |pmid=10377211 |pmc=1745525 |doi= |url=}}</ref> | *[[Granulomatosis with polyangiitis]] ([[Wegener's granulomatosis|Wegener's]])<ref name="pmid10377211">{{cite journal |vauthors=Langford CA, Hoffman GS |title=Rare diseases.3: Wegener's granulomatosis |journal=Thorax |volume=54 |issue=7 |pages=629–37 |year=1999 |pmid=10377211 |pmc=1745525 |doi= |url=}}</ref> | ||
| | | | ||
*Women are more commonly effected than | *Women are more commonly effected than men<ref name="pmid12541109">{{cite journal |vauthors=Lee KS, Kim TS, Fujimoto K, Moriya H, Watanabe H, Tateishi U, Ashizawa K, Johkoh T, Kim EA, Kwon OJ |title=Thoracic manifestation of Wegener's granulomatosis: CT findings in 30 patients |journal=Eur Radiol |volume=13 |issue=1 |pages=43–51 |year=2003 |pmid=12541109 |doi=10.1007/s00330-002-1422-2 |url=}}</ref> | ||
*Kidneys are also involved | *Kidneys are also involved | ||
*Upper respiratory tract symptoms, perforation of [[nasal septum]], [[chronic sinusitis]], [[otitis media]], [[mastoiditis]]. | *Upper respiratory tract symptoms, perforation of [[nasal septum]], [[chronic sinusitis]], [[otitis media]], [[mastoiditis]]. | ||
| Line 350: | Line 350: | ||
*Renal symptoms, [[hematuria]], red cell [[casts]] | *Renal symptoms, [[hematuria]], red cell [[casts]] | ||
| | | | ||
*Pulmonary nodules with cavities and infiltrates are | *[[Pulmonary]] [[nodules]] with [[cavities]] and infiltrates are common manifestations of CXR | ||
| | | | ||
*Positive for [[P-ANCA]] | *Positive for [[P-ANCA]] | ||
*Biopsy of the tissue | *Biopsy of the affected tissue reveals necrotizing [[granulomas]]<ref name="pmid10377211">{{cite journal |vauthors=Langford CA, Hoffman GS |title=Rare diseases.3: Wegener's granulomatosis |journal=Thorax |volume=54 |issue=7 |pages=629–37 |year=1999 |pmid=10377211 |pmc=1745525 |doi= |url=}}</ref> | ||
|- | |- | ||
| | | | ||
*[[Rheumatoid nodule]] | *[[Rheumatoid nodule]] | ||
| | | | ||
* | *Females of 40-50 age group | ||
*Manifestation of [[rheumatoid arthritis]] | *Manifestation of [[rheumatoid arthritis]] | ||
*Presents with other systemic symptoms including symmetric [[arthritis]] of the small joints of the hands and feet with morning stiffness are | *Presents with other systemic symptoms including symmetric [[arthritis]] of the small joints of the hands and feet with morning stiffness are frequent manifestations | ||
| | | | ||
*Pulmonary nodules with cavitation are located in the upper lobe ([[Caplan syndrome]]) on X-ray | *Pulmonary nodules with cavitation are located in the upper lobe ([[Caplan syndrome]]) on X-ray | ||
| Line 370: | Line 370: | ||
*[[Sarcoidosis]] | *[[Sarcoidosis]] | ||
| | | | ||
* | *Occur more commonly in African-American females | ||
* | *Usually [[asymptomatic]] except for [[Lymphadenopathy|enlarged lymph nodes]]<ref name="pmid11734441">{{cite journal |vauthors=Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H, Bresnitz EA, DePalo L, Hunninghake G, Iannuzzi MC, Johns CJ, McLennan G, Moller DR, Newman LS, Rabin DL, Rose C, Rybicki B, Weinberger SE, Terrin ML, Knatterud GL, Cherniak R |title=Clinical characteristics of patients in a case control study of sarcoidosis |journal=Am. J. Respir. Crit. Care Med. |volume=164 |issue=10 Pt 1 |pages=1885–9 |year=2001 |pmid=11734441 |doi=10.1164/ajrccm.164.10.2104046 |url=}}</ref> | ||
*Associated with [[restrictive lung disease]] | *Associated with [[restrictive lung disease]] | ||
*[[Erythema nodosum]] | *[[Erythema nodosum]] | ||
| Line 387: | Line 387: | ||
*[[Bronchiolitis obliterans]] ([[Cryptogenic organizing pneumonia]])<ref name="pmid9724431">{{cite journal |vauthors=Murphy J, Schnyder P, Herold C, Flower C |title=Bronchiolitis obliterans organising pneumonia simulating bronchial carcinoma |journal=Eur Radiol |volume=8 |issue=7 |pages=1165–9 |year=1998 |pmid=9724431 |doi=10.1007/s003300050527 |url=}}</ref><ref name="pmid19561910">{{cite journal |vauthors=Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN |title=Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review |journal=Ann Thorac Med |volume=3 |issue=2 |pages=67–75 |year=2008 |pmid=19561910 |pmc=2700454 |doi=10.4103/1817-1737.39641 |url=}}</ref> | *[[Bronchiolitis obliterans]] ([[Cryptogenic organizing pneumonia]])<ref name="pmid9724431">{{cite journal |vauthors=Murphy J, Schnyder P, Herold C, Flower C |title=Bronchiolitis obliterans organising pneumonia simulating bronchial carcinoma |journal=Eur Radiol |volume=8 |issue=7 |pages=1165–9 |year=1998 |pmid=9724431 |doi=10.1007/s003300050527 |url=}}</ref><ref name="pmid19561910">{{cite journal |vauthors=Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN |title=Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review |journal=Ann Thorac Med |volume=3 |issue=2 |pages=67–75 |year=2008 |pmid=19561910 |pmc=2700454 |doi=10.4103/1817-1737.39641 |url=}}</ref> | ||
| | | | ||
*Rare condition and | *Rare condition and resembles [[asthma]], [[pneumonia]] and [[emphysema]] | ||
*It is | *It is due to [[drug]] or [[toxin]] exposure, [[autoimmune diseases]], [[viral infections]], or [[radiation injury]] | ||
*People working in industries are at high risk | *People working in industries are at high risk | ||
*Presents with [[Fever|feve]]<nowiki/>r, [[cough]], [[wheezing]], and [[shortness of breath]] over weeks to months<ref name="pmid2805873">{{cite journal |vauthors=Cordier JF, Loire R, Brune J |title=Idiopathic bronchiolitis obliterans organizing pneumonia. Definition of characteristic clinical profiles in a series of 16 patients |journal=Chest |volume=96 |issue=5 |pages=999–1004 |year=1989 |pmid=2805873 |doi= |url=}}</ref> | *Presents with [[Fever|feve]]<nowiki/>r, [[cough]], [[wheezing]], and [[shortness of breath]] over weeks to months<ref name="pmid2805873">{{cite journal |vauthors=Cordier JF, Loire R, Brune J |title=Idiopathic bronchiolitis obliterans organizing pneumonia. Definition of characteristic clinical profiles in a series of 16 patients |journal=Chest |volume=96 |issue=5 |pages=999–1004 |year=1989 |pmid=2805873 |doi= |url=}}</ref> | ||
| | | | ||
* | *[[CT]] shows patchy [[Consolidation (medicine)|consolidation,]]<nowiki/>usually associated with ground-glass opacities and [[nodules]].<ref name="pmid8109493">{{cite journal |vauthors=Lee KS, Kullnig P, Hartman TE, Müller NL |title=Cryptogenic organizing pneumonia: CT findings in 43 patients |journal=AJR Am J Roentgenol |volume=162 |issue=3 |pages=543–6 |year=1994 |pmid=8109493 |doi=10.2214/ajr.162.3.8109493 |url=}}</ref> | ||
| | | | ||
*Biopsy of the lung<ref name="pmid19561910">{{cite journal |vauthors=Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN |title=Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review |journal=Ann Thorac Med |volume=3 |issue=2 |pages=67–75 |year=2008 |pmid=19561910 |pmc=2700454 |doi=10.4103/1817-1737.39641 |url=}}</ref> | *Biopsy of the lung<ref name="pmid19561910">{{cite journal |vauthors=Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN |title=Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review |journal=Ann Thorac Med |volume=3 |issue=2 |pages=67–75 |year=2008 |pmid=19561910 |pmc=2700454 |doi=10.4103/1817-1737.39641 |url=}}</ref> | ||
| Line 400: | Line 400: | ||
*[[Langerhans cell histiocytosis|Langerhans]] cell [[Langerhans cell histiocytosis|Histiocytosis]]<ref name="pmid22429393">{{cite journal |vauthors=Suri HS, Yi ES, Nowakowski GS, Vassallo R |title=Pulmonary langerhans cell histiocytosis |journal=Orphanet J Rare Dis |volume=7 |issue= |pages=16 |year=2012 |pmid=22429393 |pmc=3342091 |doi=10.1186/1750-1172-7-16 |url=}}</ref> | *[[Langerhans cell histiocytosis|Langerhans]] cell [[Langerhans cell histiocytosis|Histiocytosis]]<ref name="pmid22429393">{{cite journal |vauthors=Suri HS, Yi ES, Nowakowski GS, Vassallo R |title=Pulmonary langerhans cell histiocytosis |journal=Orphanet J Rare Dis |volume=7 |issue= |pages=16 |year=2012 |pmid=22429393 |pmc=3342091 |doi=10.1186/1750-1172-7-16 |url=}}</ref> | ||
| | | | ||
*Exclusively | *Exclusively occurs in smokers, with a peak age of onset 20-40 years | ||
*Clinical presentation | *Clinical presentation is variable, but symptoms usually include months of dry [[cough]], [[fever]], [[night sweats]], and [[weight loss]] | ||
*Skin is involved in 80% of the cases, scaly [[erythematous rash]] is typical | *Skin is involved in 80% of the cases, scaly [[erythematous rash]] is typical | ||
| | | | ||
*Thin-walled cystic cavities are the | *Thin-walled [[cystic]] [[cavities]] are the common radiographic manifestation, seen in over 50% of patients on either CXR or CT scans.<ref name="pmid2787035">{{cite journal |vauthors=Moore AD, Godwin JD, Müller NL, Naidich DP, Hammar SP, Buschman DL, Takasugi JE, de Carvalho CR |title=Pulmonary histiocytosis X: comparison of radiographic and CT findings |journal=Radiology |volume=172 |issue=1 |pages=249–54 |year=1989 |pmid=2787035 |doi=10.1148/radiology.172.1.2787035 |url=}}</ref> | ||
| | | | ||
*Biopsy of the lung | *Biopsy of the lung | ||
Revision as of 05:22, 28 March 2021

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mashal Awais, M.D.[2]; Alejandro Lemor, M.D. [3]
Overview
Pulmonary tuberculosis should be distinguished from other diseases that cause cough, hemoptysis, fever, night sweat, and weight loss such as: bacterial pneumonia, atypical pneumonia, brucellosis, bronchogenic carcinoma, sarcoidosis, and Hodgkin lymphoma.
Differential Diagnosis
Pulmonary Tuberculosis
| Disease | Findings |
|---|---|
| Bacterial pneumonia | Sudden onset of symptoms, such as high fever, cough, purulent sputum, chest pain, leukocytosis, chest X-ray shows consolidation. |
| Bronchogenic carcinoma | may be asymptomatic, usually at older ages (> 50 years old), cough, hemoptysis, weight loss |
| Brucellosis | Fever, anorexia, night sweats, malaise,back pain , headache, and depression. History of exposure to infected animal |
| Hodgkin lymphoma | Fever, night sweats, pruritus, painless adenopathy, mediastinal mass |
| Mycoplasmal pneumonia | Gradual onset of dry cough, headache, malaise, sore throat. Diffuse bilateral infiltrates on chest X-ray. |
| Sarcoidosis | Non-caseating granulomas in lungs and other organs, bilateral hilar lymphadenopathy, mostly in African American females. |
| Adapted from Mandell, Douglas, and Bennett's principles and practice of infectious diseases 2010 [1] | |
Extra-Pulmonary Tuberculosis
| Extra-Pulmonary Location | Differential Diagnosis |
|---|---|
| Tuberculous Lymphadenitis | Lymphoma, squamous cell carcinoma, papillary thyroid cancer, pyogenic infection |
| Skeletal Tuberculosis | Multiple myeloma, bone metastasis, spinal cord abscess, osteoporosis |
| Tuberculous Arthrits | Bacterial septic arthritis, pseudogout |
| Central Nervous System Tuberculosis | Bacterial meningitis, viral meningitis, encephalitis |
| Tuberculosis Peritonitis | Bacterial peritonitis, chronic peritoneal dialysis |
| Adapted from Asian Spine J. Feb 2014; 8(1): 97–111[2]; Handbook of Clinical Neurology[3]; Circulation Dec 2005 vol.112 no.23 3608-3616[4]; Am J Trop Med Hyg 2013 vol. 88 no. 1 54-64[5] Clin Infect Dis.(2011)53(6):555-562.[6] | |
| Causes of
lung cavities |
Differentiating Features | Differentiating radiological findings | Diagnosis
confirmation |
|---|---|---|---|
|
|
| |
|
|
|
|
|
|
| |
|
|
|
|
|
|
| |
|
|
| |
|
|
||
|
|
| |
|
|
|
| Disease | Prominent clinical features | Lab findings | Radiological findings |
|---|---|---|---|
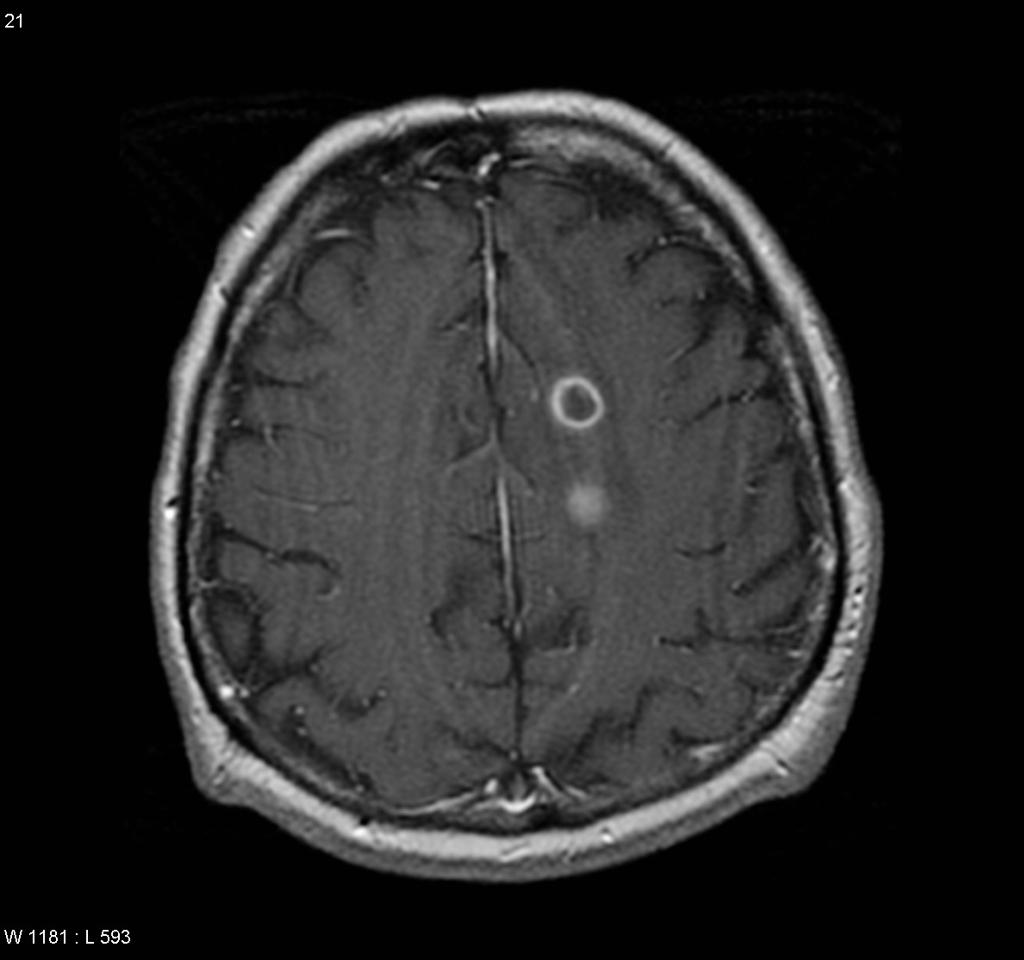
| Neurocysticercosis |
|
|
|
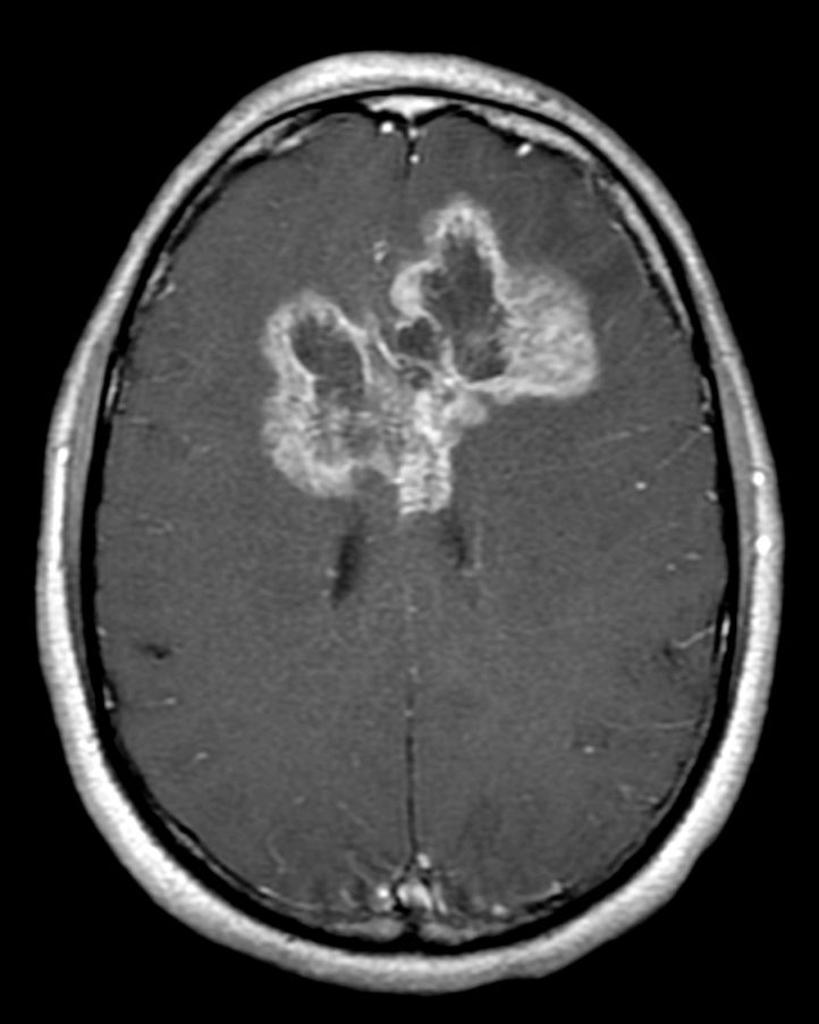
| Brain abscess |
|
|
|
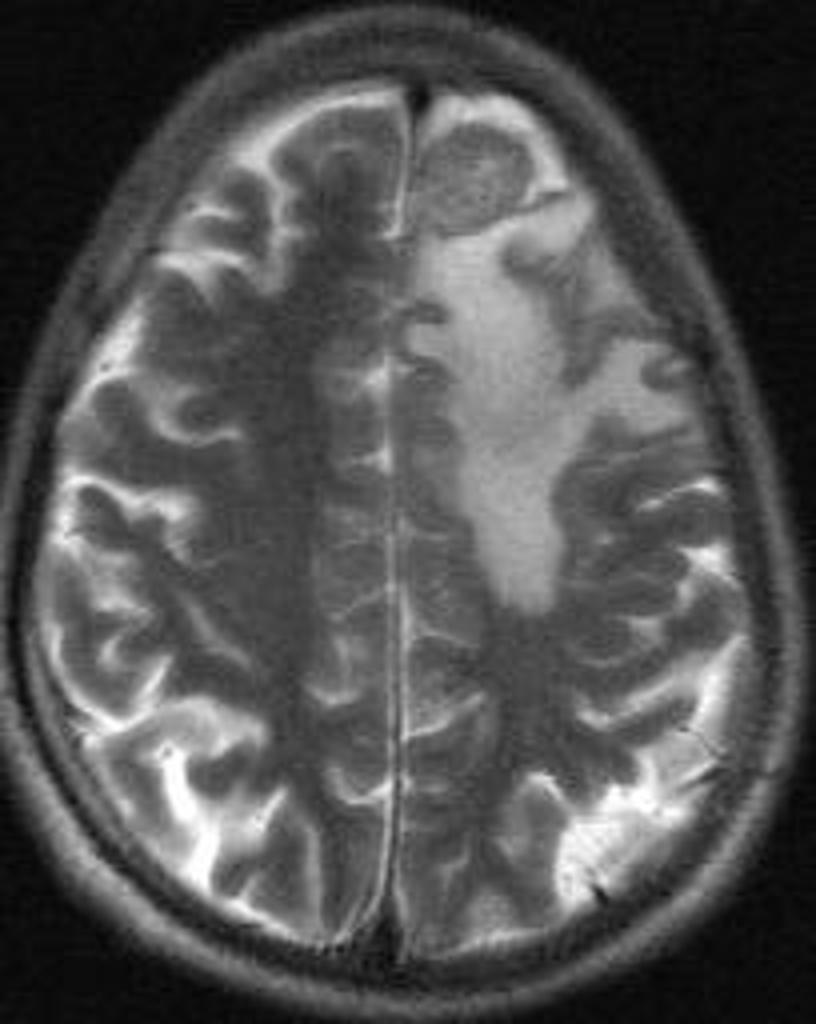
| Brain tumors |
|
| |
| Brain tuberculoma |
|
|
|
| Neurosarcoidosis |
|
|
|
 |
 |
 |
 |
|---|
Pulmonary tuberculosis must be distinguished from other cavitary lung lesions.
Differential Diagnosis
Pulmonary tuberculosis must be distinguished from other cavitary lung lesions.
| Causes of
lung cavities |
Differentiating Features | Differentiating radiological findings | Diagnosis
confirmation |
|---|---|---|---|
|
|
| |
|
|
|
|
|
|
| |
|
|
|
|
|
| ||
|
|
| |
|
|
||
|
|
| |
|
|
References
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 0443068399.
- ↑ Moon, Myung-Sang (2014). "Tuberculosis of Spine: Current Views in Diagnosis and Management". Asian Spine Journal. 8 (1): 97. doi:10.4184/asj.2014.8.1.97. ISSN 1976-1902.
- ↑ Garcia-Monco, Juan Carlos (2014). "Tuberculosis". 121: 1485–1499. doi:10.1016/B978-0-7020-4088-7.00100-0. ISSN 0072-9752.
- ↑ Mayosi, B. M. (2005). "Tuberculous Pericarditis". Circulation. 112 (23): 3608–3616. doi:10.1161/CIRCULATIONAHA.105.543066. ISSN 0009-7322.
- ↑ Daher, E. D. F.; da Silva Junior, G. B.; Barros, E. J. G. (2013). "Renal Tuberculosis in the Modern Era". American Journal of Tropical Medicine and Hygiene. 88 (1): 54–64. doi:10.4269/ajtmh.2013.12-0413. ISSN 0002-9637.
- ↑ Fontanilla, J.-M.; Barnes, A.; von Reyn, C. F. (2011). "Current Diagnosis and Management of Peripheral Tuberculous Lymphadenitis". Clinical Infectious Diseases. 53 (6): 555–562. doi:10.1093/cid/cir454. ISSN 1058-4838.
- ↑ 7.0 7.1 7.2 7.3 Chaudhuri MR (1973). "Primary pulmonary cavitating carcinomas". Thorax. 28 (3): 354–66. PMC 470041. PMID 4353362.
- ↑ 8.0 8.1 Mouroux J, Padovani B, Elkaïm D, Richelme H (1996). "Should cavitated bronchopulmonary cancers be considered a separate entity?". Ann. Thorac. Surg. 61 (2): 530–2. doi:10.1016/0003-4975(95)00973-6. PMID 8572761.
- ↑ 9.0 9.1 Onn A, Choe DH, Herbst RS, Correa AM, Munden RF, Truong MT, Vaporciyan AA, Isobe T, Gilcrease MZ, Marom EM (2005). "Tumor cavitation in stage I non-small cell lung cancer: epidermal growth factor receptor expression and prediction of poor outcome". Radiology. 237 (1): 342–7. doi:10.1148/radiol.2371041650. PMID 16183941.
- ↑ 10.0 10.1 10.2 10.3 Langford CA, Hoffman GS (1999). "Rare diseases.3: Wegener's granulomatosis". Thorax. 54 (7): 629–37. PMC 1745525. PMID 10377211.
- ↑ 11.0 11.1 Lee KS, Kim TS, Fujimoto K, Moriya H, Watanabe H, Tateishi U, Ashizawa K, Johkoh T, Kim EA, Kwon OJ (2003). "Thoracic manifestation of Wegener's granulomatosis: CT findings in 30 patients". Eur Radiol. 13 (1): 43–51. doi:10.1007/s00330-002-1422-2. PMID 12541109.
- ↑ 12.0 12.1 Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H, Bresnitz EA, DePalo L, Hunninghake G, Iannuzzi MC, Johns CJ, McLennan G, Moller DR, Newman LS, Rabin DL, Rose C, Rybicki B, Weinberger SE, Terrin ML, Knatterud GL, Cherniak R (2001). "Clinical characteristics of patients in a case control study of sarcoidosis". Am. J. Respir. Crit. Care Med. 164 (10 Pt 1): 1885–9. doi:10.1164/ajrccm.164.10.2104046. PMID 11734441.
- ↑ 13.0 13.1 Brauner MW, Grenier P, Mompoint D, Lenoir S, de Crémoux H (1989). "Pulmonary sarcoidosis: evaluation with high-resolution CT". Radiology. 172 (2): 467–71. doi:10.1148/radiology.172.2.2748828. PMID 2748828.
- ↑ 14.0 14.1 Murphy J, Schnyder P, Herold C, Flower C (1998). "Bronchiolitis obliterans organising pneumonia simulating bronchial carcinoma". Eur Radiol. 8 (7): 1165–9. doi:10.1007/s003300050527. PMID 9724431.
- ↑ 15.0 15.1 15.2 15.3 Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN (2008). "Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review". Ann Thorac Med. 3 (2): 67–75. doi:10.4103/1817-1737.39641. PMC 2700454. PMID 19561910.
- ↑ 16.0 16.1 Cordier JF, Loire R, Brune J (1989). "Idiopathic bronchiolitis obliterans organizing pneumonia. Definition of characteristic clinical profiles in a series of 16 patients". Chest. 96 (5): 999–1004. PMID 2805873.
- ↑ 17.0 17.1 Lee KS, Kullnig P, Hartman TE, Müller NL (1994). "Cryptogenic organizing pneumonia: CT findings in 43 patients". AJR Am J Roentgenol. 162 (3): 543–6. doi:10.2214/ajr.162.3.8109493. PMID 8109493.
- ↑ 18.0 18.1 Suri HS, Yi ES, Nowakowski GS, Vassallo R (2012). "Pulmonary langerhans cell histiocytosis". Orphanet J Rare Dis. 7: 16. doi:10.1186/1750-1172-7-16. PMC 3342091. PMID 22429393.
- ↑ 19.0 19.1 Moore AD, Godwin JD, Müller NL, Naidich DP, Hammar SP, Buschman DL, Takasugi JE, de Carvalho CR (1989). "Pulmonary histiocytosis X: comparison of radiographic and CT findings". Radiology. 172 (1): 249–54. doi:10.1148/radiology.172.1.2787035. PMID 2787035.
- ↑ Brouwer MC, Tunkel AR, McKhann GM, van de Beek D (2014). "Brain abscess". N. Engl. J. Med. 371 (5): 447–56. doi:10.1056/NEJMra1301635. PMID 25075836.
- ↑ "Brain Abscess — NEJM".
- ↑ 22.0 22.1 "Primary Brain Tumors in Adults - American Family Physician".
- ↑ "The Journal of Association of Chest Physicians - Tuberculoma of the brain - A diagnostic dilemma: Magnetic resonance spectroscopy a new ray of hope : Download PDF".
- ↑ 24.0 24.1 "Neurosarcoidosis".