Tuberculosis differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
Mohamed riad (talk | contribs) |
Mohamed riad (talk | contribs) |
||
| (5 intermediate revisions by the same user not shown) | |||
| Line 15: | Line 15: | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Bacterial pneumonia]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Bacterial pneumonia]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Sudden onset of symptoms, such as high [[fever]], [[cough]], purulent [[sputum]], [[chest pain]] | | style="padding: 5px 5px; background: #F5F5F5;" |Sudden onset of symptoms, such as high [[fever]], [[cough]], [[purulent]] [[sputum]], [[chest pain]], [[leukocytosis]], chest X-ray shows consolidation. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |[[Bronchogenic carcinoma]] | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |[[Bronchogenic carcinoma]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" |may be asymptomatic, usually at older ages (> 50 years old), [[cough]], [[hemoptysis]], [[weight loss]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |[[Brucellosis]] | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |[[Brucellosis]] | ||
| Line 27: | Line 27: | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |[[Mycoplasmal pneumonia]] | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |[[Mycoplasmal pneumonia]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Gradual onset of [[dry cough]], [[headache]], [[malaise]], [[sore throat]]. Diffuse bilateral infiltrates | | style="padding: 5px 5px; background: #F5F5F5;" |Gradual onset of [[dry cough]], [[headache]], [[malaise]], [[sore throat]]. Diffuse bilateral infiltrates on [[chest X-ray]]. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |[[Sarcoidosis]] | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" |[[Sarcoidosis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Non-caseating granulomas in lungs and other organs, bilateral | | style="padding: 5px 5px; background: #F5F5F5;" |Non-[[caseating]] [[granulomas]] in lungs and other organs, bilateral [[hilar]] [[lymphadenopathy]], mostly in African American females. | ||
|- | |- | ||
| colspan="2" style="padding: 5px 5px; background: #F5F5F5;" |<small>Adapted from Mandell, Douglas, and Bennett's principles and practice of infectious diseases 2010 <ref>{{cite book | last = Mandell | first = Gerald | title = Mandell, Douglas, and Bennett's principles and practice of infectious diseases | publisher = Churchill Livingstone/Elsevier | location = Philadelphia, PA | year = 2010 | isbn = 0443068399 }}</ref> </small> | | colspan="2" style="padding: 5px 5px; background: #F5F5F5;" |<small>Adapted from Mandell, Douglas, and Bennett's principles and practice of infectious diseases 2010 <ref>{{cite book | last = Mandell | first = Gerald | title = Mandell, Douglas, and Bennett's principles and practice of infectious diseases | publisher = Churchill Livingstone/Elsevier | location = Philadelphia, PA | year = 2010 | isbn = 0443068399 }}</ref> </small> | ||
| Line 132: | Line 132: | ||
| | | | ||
*Positive for [[P-ANCA]] | *Positive for [[P-ANCA]] | ||
*Biopsy of the tissue | *Biopsy of the affected tissue shows necrotizing [[granulomas]] <ref name="pmid10377211">{{cite journal |vauthors=Langford CA, Hoffman GS |title=Rare diseases.3: Wegener's granulomatosis |journal=Thorax |volume=54 |issue=7 |pages=629–37 |year=1999 |pmid=10377211 |pmc=1745525 |doi= |url=}}</ref> | ||
|- | |- | ||
| | | | ||
| Line 139: | Line 139: | ||
*Elderly females of 40-50 age group | *Elderly females of 40-50 age group | ||
*Manifestation of [[rheumatoid arthritis]] | *Manifestation of [[rheumatoid arthritis]] | ||
*Presents with other systemic symptoms including symmetric [[arthritis]] of the small joints of the hands and feet | *Presents with other systemic symptoms including symmetric [[arthritis]] of the small joints of the hands and feet and morning stiffness are common manifestations. | ||
| | | | ||
*Pulmonary nodules with cavitation are | *Pulmonary nodules with cavitation are present in the upper lobe ([[Caplan syndrome]]) on Xray. | ||
| | | | ||
*Positive for both [[rheumatoid factor]] and anti-cyclic citrullinated peptide [[Antibody|antibody.]] | *Positive for both [[rheumatoid factor]] and anti-cyclic citrullinated peptide [[Antibody|antibody.]] | ||
| Line 160: | Line 160: | ||
*Additional findings on CT include [[fibrosis]] (honeycomb, linear, or associated with bronchial distortion), pleural thickening, and ground-glass opacities.<ref name="pmid2748828">{{cite journal |vauthors=Brauner MW, Grenier P, Mompoint D, Lenoir S, de Crémoux H |title=Pulmonary sarcoidosis: evaluation with high-resolution CT |journal=Radiology |volume=172 |issue=2 |pages=467–71 |year=1989 |pmid=2748828 |doi=10.1148/radiology.172.2.2748828 |url=}}</ref> | *Additional findings on CT include [[fibrosis]] (honeycomb, linear, or associated with bronchial distortion), pleural thickening, and ground-glass opacities.<ref name="pmid2748828">{{cite journal |vauthors=Brauner MW, Grenier P, Mompoint D, Lenoir S, de Crémoux H |title=Pulmonary sarcoidosis: evaluation with high-resolution CT |journal=Radiology |volume=172 |issue=2 |pages=467–71 |year=1989 |pmid=2748828 |doi=10.1148/radiology.172.2.2748828 |url=}}</ref> | ||
| | | | ||
*Biopsy of lung | *Biopsy of lung reveals non-[[caseating]] [[granuloma]] | ||
|- | |- | ||
| | | | ||
| Line 166: | Line 166: | ||
| | | | ||
*Rare condition and mimics [[asthma]], [[pneumonia]] and [[emphysema]] | *Rare condition and mimics [[asthma]], [[pneumonia]] and [[emphysema]] | ||
*It is | *It is due to [[drug]] or [[toxin]] exposure, [[autoimmune diseases]], [[viral infections]], or [[radiation injury]] | ||
* | *Individuals working in industries are at high risk | ||
*Presents with [[Fever|feve]]<nowiki/>r, [[cough]], [[wheezing]] and [[shortness of breath]] over weeks to months,<ref name="pmid2805873">{{cite journal |vauthors=Cordier JF, Loire R, Brune J |title=Idiopathic bronchiolitis obliterans organizing pneumonia. Definition of characteristic clinical profiles in a series of 16 patients |journal=Chest |volume=96 |issue=5 |pages=999–1004 |year=1989 |pmid=2805873 |doi= |url=}}</ref> | *Presents with [[Fever|feve]]<nowiki/>r, [[cough]], [[wheezing]] and [[shortness of breath]] over weeks to months,<ref name="pmid2805873">{{cite journal |vauthors=Cordier JF, Loire R, Brune J |title=Idiopathic bronchiolitis obliterans organizing pneumonia. Definition of characteristic clinical profiles in a series of 16 patients |journal=Chest |volume=96 |issue=5 |pages=999–1004 |year=1989 |pmid=2805873 |doi= |url=}}</ref> | ||
| | | | ||
| Line 178: | Line 178: | ||
*[[Langerhans cell histiocytosis|Langerhans]] cell [[Langerhans cell histiocytosis|Histiocytosis]]<ref name="pmid22429393">{{cite journal |vauthors=Suri HS, Yi ES, Nowakowski GS, Vassallo R |title=Pulmonary langerhans cell histiocytosis |journal=Orphanet J Rare Dis |volume=7 |issue= |pages=16 |year=2012 |pmid=22429393 |pmc=3342091 |doi=10.1186/1750-1172-7-16 |url=}}</ref> | *[[Langerhans cell histiocytosis|Langerhans]] cell [[Langerhans cell histiocytosis|Histiocytosis]]<ref name="pmid22429393">{{cite journal |vauthors=Suri HS, Yi ES, Nowakowski GS, Vassallo R |title=Pulmonary langerhans cell histiocytosis |journal=Orphanet J Rare Dis |volume=7 |issue= |pages=16 |year=2012 |pmid=22429393 |pmc=3342091 |doi=10.1186/1750-1172-7-16 |url=}}</ref> | ||
| | | | ||
*Exclusively | *Exclusively occurs in smokers, with a peak age of onset 20-40 years. | ||
*Clinical presentation | *Clinical presentation is variable, but symptoms generally include months of dry [[cough]], [[fever]], [[night sweats]] and [[weight loss]]. | ||
*Skin is involved in 80% of the cases, scaly [[erythematous rash]] is typical. | *Skin is involved in 80% of the cases, scaly [[erythematous rash]] is typical. | ||
| | | | ||
| Line 196: | Line 196: | ||
|Neurocysticercosis | |Neurocysticercosis | ||
| | | | ||
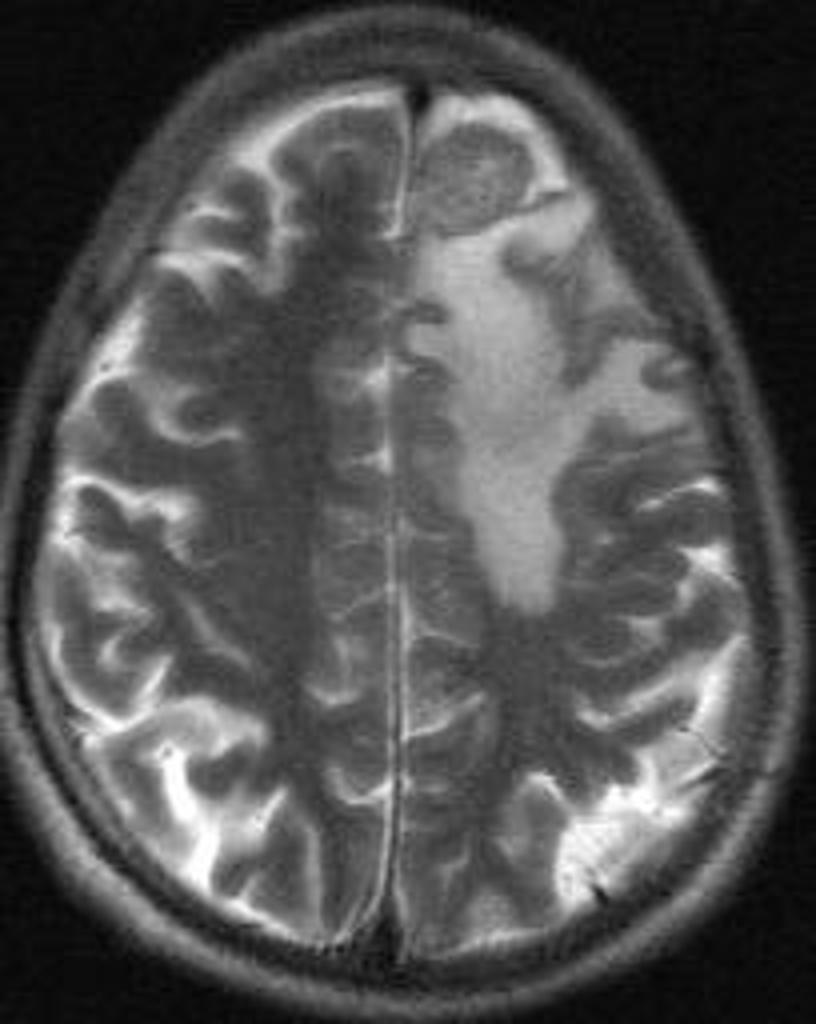
*Presenting symptoms | *Presenting symptoms vary based on the site of the cysticerci. | ||
*[[Parenchymal]] neurocysticercosis causes all the symptoms and signs of [[Space occupying lesion|space occupying lesions]]. | *[[Parenchymal]] neurocysticercosis causes all the symptoms and signs of [[Space occupying lesion|space occupying lesions]]. | ||
*Extraparenchymal neurocysticercosis causes manifestations of [[increased intracranial pressure]] if cysts are present in the [[subarachnoid space]] or in the [[ventricles]], | *Extraparenchymal neurocysticercosis causes manifestations of [[increased intracranial pressure]] if cysts are present in the [[subarachnoid space]] or in the [[ventricles]], the clinical picture of [[spinal cord compression]] if present in the spinal cord or causes eye disease if cysts are present in the [[orbit]]. | ||
| | | | ||
| Line 209: | Line 209: | ||
|[[Brain abscess]] | |[[Brain abscess]] | ||
| | | | ||
*[[Headaches]] are the most common symptom. | *[[Headaches]] are the most common symptom. Often, [[headaches]] occur on the same side of the [[Abscesses|abscess]] and tend to be severe (unresponsive to [[analgesics]]). | ||
*[[Fever]] is not a reliable sign.<ref name="pmid25075836">{{cite journal |vauthors=Brouwer MC, Tunkel AR, McKhann GM, van de Beek D |title=Brain abscess |journal=N. Engl. J. Med. |volume=371 |issue=5 |pages=447–56 |year=2014 |pmid=25075836 |doi=10.1056/NEJMra1301635 |url=}}</ref> | *[[Fever]] is not a reliable sign.<ref name="pmid25075836">{{cite journal |vauthors=Brouwer MC, Tunkel AR, McKhann GM, van de Beek D |title=Brain abscess |journal=N. Engl. J. Med. |volume=371 |issue=5 |pages=447–56 |year=2014 |pmid=25075836 |doi=10.1056/NEJMra1301635 |url=}}</ref> | ||
| Line 216: | Line 216: | ||
*Culture from the CT-guided aspirated lesion helps in identifying the causative agent. | *Culture from the CT-guided aspirated lesion helps in identifying the causative agent. | ||
| | | | ||
*[[Contrast enhanced CT]] | *[[Contrast enhanced CT]] is useful for a rapid assessment of the size and number of the [[abscesses]]. | ||
*[[MRI|MRI:]] [[Diffusion-weighted imaging|Diffusion-weighted imaging (DWI)]] [[MRI]] can differentiate [[brain abscesses]] from [[Brain cyst|cystic brain lesions]] with [[Sensitivity|sensitivit]]<nowiki/>y and [[specificity]] of 96%.<ref name="urlBrain Abscess — NEJM">{{cite web |url=http://www.nejm.org/doi/full/10.1056/NEJMra1301635 |title=Brain Abscess — NEJM |format= |work= |accessdate=}}</ref> | *[[MRI|MRI:]] [[Diffusion-weighted imaging|Diffusion-weighted imaging (DWI)]] [[MRI]] can differentiate [[brain abscesses]] from [[Brain cyst|cystic brain lesions]] with [[Sensitivity|sensitivit]]<nowiki/>y and [[specificity]] of 96%.<ref name="urlBrain Abscess — NEJM">{{cite web |url=http://www.nejm.org/doi/full/10.1056/NEJMra1301635 |title=Brain Abscess — NEJM |format= |work= |accessdate=}}</ref> | ||
| Line 225: | Line 225: | ||
*Most common presenting symptom is [[Headache|dull aching headache]]. | *Most common presenting symptom is [[Headache|dull aching headache]]. | ||
* | *Often, it is associated with other symptoms of [[Increased intracranial pressure|increased intracranial pressure (ICP)]] as [[Seizure|seizures]], [[Visual disturbance|visual disturbances]], [[Nausea and vomiting|nausea, and vomiting]].<ref name="urlPrimary Brain Tumors in Adults - American Family Physician">{{cite web |url=http://www.aafp.org/afp/2008/0515/p1423.html |title=Primary Brain Tumors in Adults - American Family Physician |format= |work= |accessdate=}}</ref> | ||
| | | | ||
| | | | ||
| Line 246: | Line 246: | ||
| | | | ||
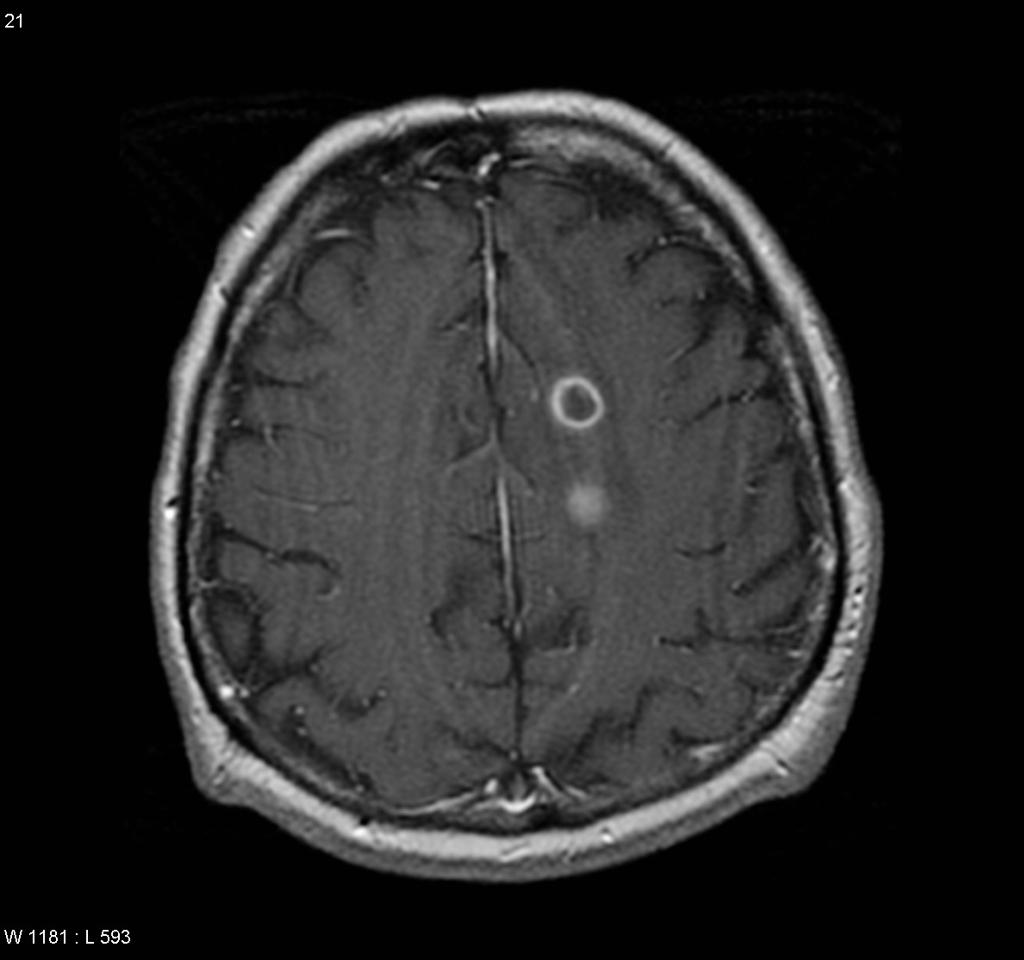
*[[CT]]: [[Contrast enhanced CT|Contrast-enhanced CT]] scan shows a ring enhancing lesion surrounded by an area of hypodensity ([[cerebritis]]) and the resulting [[mass effect]]. | *[[CT]]: [[Contrast enhanced CT|Contrast-enhanced CT]] scan shows a ring enhancing lesion surrounded by an area of hypodensity ([[cerebritis]]) and the resulting [[mass effect]]. | ||
*[[MRI]]: Better than [[CT]] scan in assessing the site and size of the [[tuberculoma]]. Gadolinium-enhanced MRI | *[[MRI]]: Better than [[CT]] scan in assessing the site and size of the [[tuberculoma]]. Gadolinium-enhanced MRI reveals a ring-enhancing lesion between 1-5 cm in size (In NCC, the wall is thicker, [[Calcification|calcifications]] are eccentric and the diameter is less than 2 cm) | ||
|- | |- | ||
|Neurosarcoidosis | |Neurosarcoidosis | ||
| | | | ||
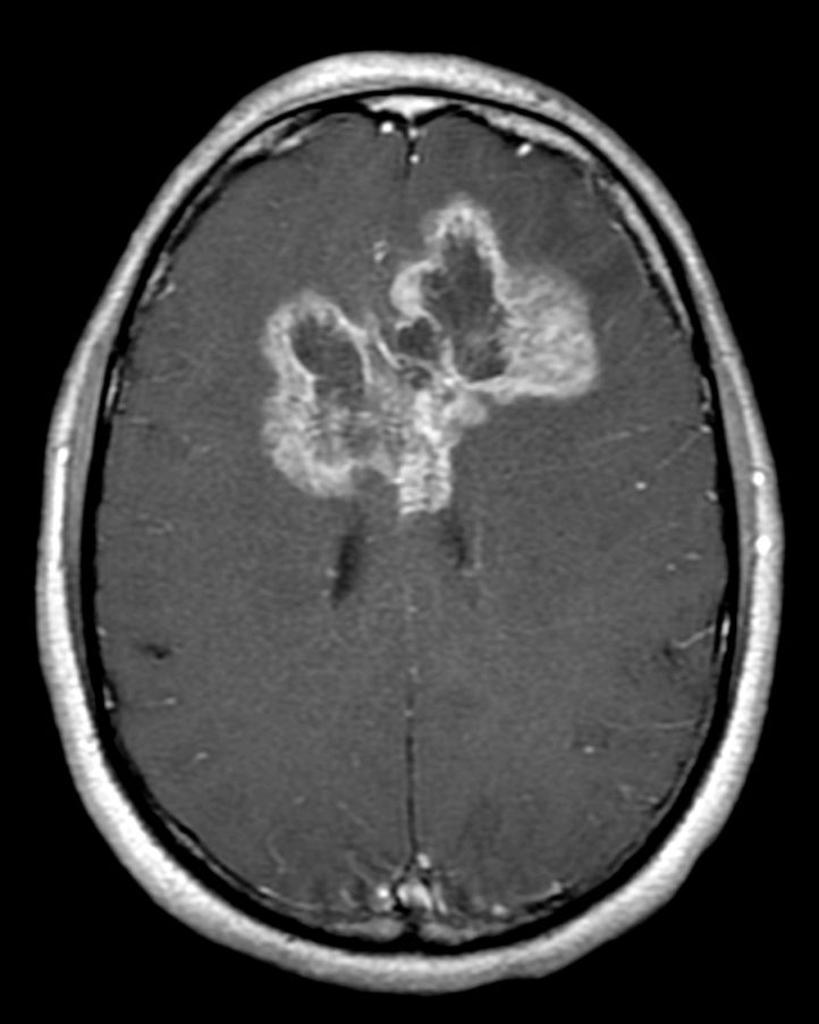
*70% of the patients present with the neurological symptoms rather than the presentation of systemic disease. Common presentations | *70% of the patients present with the neurological symptoms rather than the presentation of systemic disease. Common presentations include:<ref name="urlNeurosarcoidosis">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975794/ |title=Neurosarcoidosis |format= |work= |accessdate=}}</ref> | ||
#Cranial nerve neuropathies: [[Facial palsy]] is the most common presentation. | #[[Cranial nerve]] [[neuropathies]]: [[Facial palsy]] is the most common presentation. | ||
#[[Meningeal]] involvement: diffuse [[Meningitis|meningeal inflammation]] can | #[[Meningeal]] involvement: diffuse [[Meningitis|meningeal inflammation]] can result in diffuse [[Polyneuropathy|basilar polyneuropathy]] in 40% of the patients. with [[neurosarcoidosis]]. | ||
#Inflammatory [[spinal cord]] disease: Inflammatory span | #[[Inflammatory]] [[spinal cord]] disease: Inflammatory span is often more than 3 spinal cord segments that help to distinguish it from [[Multiple sclerosis|Multiple Sclerosis]]. | ||
#[[Peripheral neuropathy]]: [[Polyneuropathy|Asymmetric polyneuropathy]] or [[mononeuritis multiplex]]. It may also manifest as [[Guillain-Barré syndrome|Guillain-Barré syndrome (GBS)]] like presentation. | #[[Peripheral neuropathy]]: [[Polyneuropathy|Asymmetric polyneuropathy]] or [[mononeuritis multiplex]]. It may also manifest as [[Guillain-Barré syndrome|Guillain-Barré syndrome (GBS)]] like presentation. | ||
#[[Hypothalamic pituitary adrenal axis|HPO axis]] involvement: may present as [[diabetes insipidus]]. More than 50% of the cases have | #[[Hypothalamic pituitary adrenal axis|HPO axis]] involvement: may present as [[diabetes insipidus]]. More than 50% of the cases do not have any radiological signs. | ||
| | | | ||
| Line 278: | Line 278: | ||
|} | |} | ||
Pulmonary tuberculosis must be | [[Pulmonary tuberculosis]] must be distinguished from other cavitary lung lesions. | ||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
Pulmonary tuberculosis must be | Pulmonary tuberculosis must be distinguished from other cavitary lung lesions. | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 297: | Line 297: | ||
*Chronic smokers | *Chronic smokers | ||
*Presents with a [[low-grade fever]], absence of [[leukocytosis]], systemic complaints [[weight loss]], [[fatigue]] | *Presents with a [[low-grade fever]], absence of [[leukocytosis]], systemic complaints [[weight loss]], [[fatigue]] | ||
*Absence of factors that | *Absence of predisposing factors that lead to [[gastric content aspiration]], no response to [[antibiotics]] within 10 days | ||
*[[Hemoptysis]] is commonly associated with [[bronchogenic carcinoma]] | *[[Hemoptysis]] is commonly associated with [[bronchogenic carcinoma]] | ||
| | | | ||
| Line 308: | Line 308: | ||
*Pulmonary [[Tuberculosis, pulmonary|Tuberculosis]] | *Pulmonary [[Tuberculosis, pulmonary|Tuberculosis]] | ||
| | | | ||
*Mostly in endemic areas | *Mostly in [[endemic]] areas | ||
*Symptoms include [[productive cough]], [[ | *Symptoms include [[productive cough]], [[fever]], [[night sweats]], and [[weight loss]] | ||
| | | | ||
*CXR and CT | *CXR and CT show [[Internal|cavities]] in the upper lobe of the lung | ||
| | | | ||
*[[Sputum]] smear-positive for [[acid-fast bacilli]] and nucleic acid amplification tests (NAAT) are used on sputum or any sterile fluid for rapid diagnosis and is positive for mycobacteria. | *[[Sputum]] smear-positive for [[acid-fast bacilli]] and nucleic acid amplification tests ([[NAAT]]) are used on sputum or any sterile fluid for rapid diagnosis and is positive for mycobacteria. | ||
|- | |- | ||
| | | | ||
| Line 319: | Line 319: | ||
| | | | ||
*Any age group | *Any age group | ||
*Acute, [[fulminant]] life threating complication of | *Acute, [[fulminant]] life threating complication of previous infection | ||
*>100.4 °F fever, with [[Hemodynamically unstable|hemodynamic]] instability | *>100.4 °F fever, with [[Hemodynamically unstable|hemodynamic]] instability | ||
*Worsening [[pneumonia]]-like symptoms | *Worsening [[pneumonia]]-like symptoms | ||
| | | | ||
*CXR | *CXR shows multiple cavitary lesions | ||
*[[Pleural effusion]] and [[empyema]] are common findings | *[[Pleural effusion]] and [[empyema]] are common findings | ||
| | | | ||
| Line 332: | Line 332: | ||
*Loculated [[empyema]] | *Loculated [[empyema]] | ||
| | | | ||
*Children and elderly are at risk | *Children and elderly are at high risk | ||
*Pleuritic [[chest pain]], [[dry cough]], [[fever]] with chills | *Pleuritic [[chest pain]], [[dry cough]], [[fever]] with chills | ||
| Line 344: | Line 344: | ||
*[[Granulomatosis with polyangiitis]] ([[Wegener's granulomatosis|Wegener's]])<ref name="pmid10377211">{{cite journal |vauthors=Langford CA, Hoffman GS |title=Rare diseases.3: Wegener's granulomatosis |journal=Thorax |volume=54 |issue=7 |pages=629–37 |year=1999 |pmid=10377211 |pmc=1745525 |doi= |url=}}</ref> | *[[Granulomatosis with polyangiitis]] ([[Wegener's granulomatosis|Wegener's]])<ref name="pmid10377211">{{cite journal |vauthors=Langford CA, Hoffman GS |title=Rare diseases.3: Wegener's granulomatosis |journal=Thorax |volume=54 |issue=7 |pages=629–37 |year=1999 |pmid=10377211 |pmc=1745525 |doi= |url=}}</ref> | ||
| | | | ||
*Women are more commonly effected than | *Women are more commonly effected than men<ref name="pmid12541109">{{cite journal |vauthors=Lee KS, Kim TS, Fujimoto K, Moriya H, Watanabe H, Tateishi U, Ashizawa K, Johkoh T, Kim EA, Kwon OJ |title=Thoracic manifestation of Wegener's granulomatosis: CT findings in 30 patients |journal=Eur Radiol |volume=13 |issue=1 |pages=43–51 |year=2003 |pmid=12541109 |doi=10.1007/s00330-002-1422-2 |url=}}</ref> | ||
*Kidneys are also involved | *Kidneys are also involved | ||
*Upper respiratory tract symptoms, perforation of [[nasal septum]], [[chronic sinusitis]], [[otitis media]], [[mastoiditis]]. | *Upper respiratory tract symptoms, perforation of [[nasal septum]], [[chronic sinusitis]], [[otitis media]], [[mastoiditis]]. | ||
| Line 350: | Line 350: | ||
*Renal symptoms, [[hematuria]], red cell [[casts]] | *Renal symptoms, [[hematuria]], red cell [[casts]] | ||
| | | | ||
*Pulmonary nodules with cavities and infiltrates are | *[[Pulmonary]] [[nodules]] with [[cavities]] and infiltrates are common manifestations of CXR | ||
| | | | ||
*Positive for [[P-ANCA]] | *Positive for [[P-ANCA]] | ||
*Biopsy of the tissue | *Biopsy of the affected tissue reveals necrotizing [[granulomas]]<ref name="pmid10377211">{{cite journal |vauthors=Langford CA, Hoffman GS |title=Rare diseases.3: Wegener's granulomatosis |journal=Thorax |volume=54 |issue=7 |pages=629–37 |year=1999 |pmid=10377211 |pmc=1745525 |doi= |url=}}</ref> | ||
|- | |- | ||
| | | | ||
*[[Rheumatoid nodule]] | *[[Rheumatoid nodule]] | ||
| | | | ||
* | *Females of 40-50 age group | ||
*Manifestation of [[rheumatoid arthritis]] | *Manifestation of [[rheumatoid arthritis]] | ||
*Presents with other systemic symptoms including symmetric [[arthritis]] of the small joints of the hands and feet with morning stiffness are | *Presents with other systemic symptoms including symmetric [[arthritis]] of the small joints of the hands and feet with morning stiffness are frequent manifestations | ||
| | | | ||
*Pulmonary nodules with cavitation are | *[[Pulmonary]] [[nodules]] with [[cavitation]] are present in the upper lobe ([[Caplan syndrome]]) on X-ray | ||
| | | | ||
*Positive for both [[rheumatoid factor]] and anti-cyclic citrullinated peptide [[Antibody|antibody.]] | *Positive for both [[rheumatoid factor]] and anti-cyclic citrullinated peptide [[Antibody|antibody.]] | ||
| Line 370: | Line 370: | ||
*[[Sarcoidosis]] | *[[Sarcoidosis]] | ||
| | | | ||
* | *Occur more commonly in African-American females | ||
* | *Usually [[asymptomatic]] except for [[Lymphadenopathy|enlarged lymph nodes]]<ref name="pmid11734441">{{cite journal |vauthors=Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H, Bresnitz EA, DePalo L, Hunninghake G, Iannuzzi MC, Johns CJ, McLennan G, Moller DR, Newman LS, Rabin DL, Rose C, Rybicki B, Weinberger SE, Terrin ML, Knatterud GL, Cherniak R |title=Clinical characteristics of patients in a case control study of [[sarcoidosis]] |journal=Am. J. Respir. Crit. Care Med. |volume=164 |issue=10 Pt 1 |pages=1885–9 |year=2001 |pmid=11734441 |doi=10.1164/ajrccm.164.10.2104046 |url=}}</ref> | ||
*Associated with [[restrictive lung disease]] | *Associated with [[restrictive lung disease]] | ||
*[[Erythema nodosum]] | *[[Erythema nodosum]] | ||
| Line 380: | Line 380: | ||
*On CXR bilateral [[Lymphadenopathy|adenopathy]] and coarse reticular opacities are seen | *On CXR bilateral [[Lymphadenopathy|adenopathy]] and coarse reticular opacities are seen | ||
*CT of the chest demonstrates extensive [[Hilar lymphadenopathy|hilar]] and mediastinal adenopathy | *CT of the chest demonstrates extensive [[Hilar lymphadenopathy|hilar]] and mediastinal adenopathy | ||
*Additional findings on CT include [[fibrosis]] (honeycomb, linear, or associated with bronchial distortion), pleural thickening, and ground-glass opacities.<ref name="pmid2748828">{{cite journal |vauthors=Brauner MW, Grenier P, Mompoint D, Lenoir S, de Crémoux H |title=Pulmonary sarcoidosis: evaluation with high-resolution CT |journal=Radiology |volume=172 |issue=2 |pages=467–71 |year=1989 |pmid=2748828 |doi=10.1148/radiology.172.2.2748828 |url=}}</ref> | *Additional findings on CT include [[fibrosis]] (honeycomb, linear, or associated with bronchial distortion), [[pleural]] thickening, and ground-glass opacities.<ref name="pmid2748828">{{cite journal |vauthors=Brauner MW, Grenier P, Mompoint D, Lenoir S, de Crémoux H |title=Pulmonary sarcoidosis: evaluation with high-resolution CT |journal=Radiology |volume=172 |issue=2 |pages=467–71 |year=1989 |pmid=2748828 |doi=10.1148/radiology.172.2.2748828 |url=}}</ref> | ||
| | | | ||
*Biopsy of lung shows non-[[caseating]] [[granuloma]] | *Biopsy of lung shows non-[[caseating]] [[granuloma]] | ||
| Line 387: | Line 387: | ||
*[[Bronchiolitis obliterans]] ([[Cryptogenic organizing pneumonia]])<ref name="pmid9724431">{{cite journal |vauthors=Murphy J, Schnyder P, Herold C, Flower C |title=Bronchiolitis obliterans organising pneumonia simulating bronchial carcinoma |journal=Eur Radiol |volume=8 |issue=7 |pages=1165–9 |year=1998 |pmid=9724431 |doi=10.1007/s003300050527 |url=}}</ref><ref name="pmid19561910">{{cite journal |vauthors=Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN |title=Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review |journal=Ann Thorac Med |volume=3 |issue=2 |pages=67–75 |year=2008 |pmid=19561910 |pmc=2700454 |doi=10.4103/1817-1737.39641 |url=}}</ref> | *[[Bronchiolitis obliterans]] ([[Cryptogenic organizing pneumonia]])<ref name="pmid9724431">{{cite journal |vauthors=Murphy J, Schnyder P, Herold C, Flower C |title=Bronchiolitis obliterans organising pneumonia simulating bronchial carcinoma |journal=Eur Radiol |volume=8 |issue=7 |pages=1165–9 |year=1998 |pmid=9724431 |doi=10.1007/s003300050527 |url=}}</ref><ref name="pmid19561910">{{cite journal |vauthors=Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN |title=Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review |journal=Ann Thorac Med |volume=3 |issue=2 |pages=67–75 |year=2008 |pmid=19561910 |pmc=2700454 |doi=10.4103/1817-1737.39641 |url=}}</ref> | ||
| | | | ||
*Rare condition and | *Rare condition and resembles [[asthma]], [[pneumonia]] and [[emphysema]] | ||
*It is | *It is due to [[drug]] or [[toxin]] exposure, [[autoimmune diseases]], [[viral infections]], or [[radiation injury]] | ||
*People working in industries are at high risk | *People working in industries are at high risk | ||
*Presents with [[Fever|feve]]<nowiki/>r, [[cough]], [[wheezing]], and [[shortness of breath]] over weeks to months<ref name="pmid2805873">{{cite journal |vauthors=Cordier JF, Loire R, Brune J |title=Idiopathic bronchiolitis obliterans organizing pneumonia. Definition of characteristic clinical profiles in a series of 16 patients |journal=Chest |volume=96 |issue=5 |pages=999–1004 |year=1989 |pmid=2805873 |doi= |url=}}</ref> | *Presents with [[Fever|feve]]<nowiki/>r, [[cough]], [[wheezing]], and [[shortness of breath]] over weeks to months<ref name="pmid2805873">{{cite journal |vauthors=Cordier JF, Loire R, Brune J |title=Idiopathic bronchiolitis obliterans organizing pneumonia. Definition of characteristic clinical profiles in a series of 16 patients |journal=Chest |volume=96 |issue=5 |pages=999–1004 |year=1989 |pmid=2805873 |doi= |url=}}</ref> | ||
| | | | ||
* | *[[CT]] shows patchy [[Consolidation (medicine)|consolidation,]]<nowiki/>usually associated with ground-glass opacities and [[nodules]].<ref name="pmid8109493">{{cite journal |vauthors=Lee KS, Kullnig P, Hartman TE, Müller NL |title=Cryptogenic organizing pneumonia: CT findings in 43 patients |journal=AJR Am J Roentgenol |volume=162 |issue=3 |pages=543–6 |year=1994 |pmid=8109493 |doi=10.2214/ajr.162.3.8109493 |url=}}</ref> | ||
| | | | ||
*Biopsy of the lung<ref name="pmid19561910">{{cite journal |vauthors=Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN |title=Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review |journal=Ann Thorac Med |volume=3 |issue=2 |pages=67–75 |year=2008 |pmid=19561910 |pmc=2700454 |doi=10.4103/1817-1737.39641 |url=}}</ref> | *Biopsy of the lung<ref name="pmid19561910">{{cite journal |vauthors=Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN |title=Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review |journal=Ann Thorac Med |volume=3 |issue=2 |pages=67–75 |year=2008 |pmid=19561910 |pmc=2700454 |doi=10.4103/1817-1737.39641 |url=}}</ref> | ||
| Line 400: | Line 400: | ||
*[[Langerhans cell histiocytosis|Langerhans]] cell [[Langerhans cell histiocytosis|Histiocytosis]]<ref name="pmid22429393">{{cite journal |vauthors=Suri HS, Yi ES, Nowakowski GS, Vassallo R |title=Pulmonary langerhans cell histiocytosis |journal=Orphanet J Rare Dis |volume=7 |issue= |pages=16 |year=2012 |pmid=22429393 |pmc=3342091 |doi=10.1186/1750-1172-7-16 |url=}}</ref> | *[[Langerhans cell histiocytosis|Langerhans]] cell [[Langerhans cell histiocytosis|Histiocytosis]]<ref name="pmid22429393">{{cite journal |vauthors=Suri HS, Yi ES, Nowakowski GS, Vassallo R |title=Pulmonary langerhans cell histiocytosis |journal=Orphanet J Rare Dis |volume=7 |issue= |pages=16 |year=2012 |pmid=22429393 |pmc=3342091 |doi=10.1186/1750-1172-7-16 |url=}}</ref> | ||
| | | | ||
*Exclusively | *Exclusively occurs in smokers, with a peak age of onset 20-40 years | ||
*Clinical presentation | *Clinical presentation is variable, but symptoms usually include months of dry [[cough]], [[fever]], [[night sweats]], and [[weight loss]] | ||
*Skin is involved in 80% of the cases, scaly [[erythematous rash]] is typical | *Skin is involved in 80% of the cases, scaly [[erythematous rash]] is typical | ||
| | | | ||
*Thin-walled cystic cavities are the | *Thin-walled [[cystic]] [[cavities]] are the common radiographic manifestation, seen in over 50% of patients on either [[CXR]] or [[CT scans]].<ref name="pmid2787035">{{cite journal |vauthors=Moore AD, Godwin JD, Müller NL, Naidich DP, Hammar SP, Buschman DL, Takasugi JE, de Carvalho CR |title=Pulmonary histiocytosis X: comparison of radiographic and CT findings |journal=Radiology |volume=172 |issue=1 |pages=249–54 |year=1989 |pmid=2787035 |doi=10.1148/radiology.172.1.2787035 |url=}}</ref> | ||
| | | | ||
*Biopsy of the lung | *[[Biopsy]] of the [[lung]] | ||
|} | |} | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
Latest revision as of 05:25, 28 March 2021

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mashal Awais, M.D.[2]; Alejandro Lemor, M.D. [3]
Overview
Pulmonary tuberculosis should be distinguished from other diseases that cause cough, hemoptysis, fever, night sweat, and weight loss such as: bacterial pneumonia, atypical pneumonia, brucellosis, bronchogenic carcinoma, sarcoidosis, and Hodgkin lymphoma.
Differential Diagnosis
Pulmonary Tuberculosis
| Disease | Findings |
|---|---|
| Bacterial pneumonia | Sudden onset of symptoms, such as high fever, cough, purulent sputum, chest pain, leukocytosis, chest X-ray shows consolidation. |
| Bronchogenic carcinoma | may be asymptomatic, usually at older ages (> 50 years old), cough, hemoptysis, weight loss |
| Brucellosis | Fever, anorexia, night sweats, malaise,back pain , headache, and depression. History of exposure to infected animal |
| Hodgkin lymphoma | Fever, night sweats, pruritus, painless adenopathy, mediastinal mass |
| Mycoplasmal pneumonia | Gradual onset of dry cough, headache, malaise, sore throat. Diffuse bilateral infiltrates on chest X-ray. |
| Sarcoidosis | Non-caseating granulomas in lungs and other organs, bilateral hilar lymphadenopathy, mostly in African American females. |
| Adapted from Mandell, Douglas, and Bennett's principles and practice of infectious diseases 2010 [1] | |
Extra-Pulmonary Tuberculosis
| Extra-Pulmonary Location | Differential Diagnosis |
|---|---|
| Tuberculous Lymphadenitis | Lymphoma, squamous cell carcinoma, papillary thyroid cancer, pyogenic infection |
| Skeletal Tuberculosis | Multiple myeloma, bone metastasis, spinal cord abscess, osteoporosis |
| Tuberculous Arthrits | Bacterial septic arthritis, pseudogout |
| Central Nervous System Tuberculosis | Bacterial meningitis, viral meningitis, encephalitis |
| Tuberculosis Peritonitis | Bacterial peritonitis, chronic peritoneal dialysis |
| Adapted from Asian Spine J. Feb 2014; 8(1): 97–111[2]; Handbook of Clinical Neurology[3]; Circulation Dec 2005 vol.112 no.23 3608-3616[4]; Am J Trop Med Hyg 2013 vol. 88 no. 1 54-64[5] Clin Infect Dis.(2011)53(6):555-562.[6] | |
| Causes of
lung cavities |
Differentiating Features | Differentiating radiological findings | Diagnosis
confirmation |
|---|---|---|---|
|
|
| |
|
|
|
|
|
|
| |
|
|
|
|
|
|
| |
|
|
| |
|
|
||
|
|
| |
|
|
|
| Disease | Prominent clinical features | Lab findings | Radiological findings |
|---|---|---|---|
| Neurocysticercosis |
|
|
|
| Brain abscess |
|
|
|
| Brain tumors |
|
| |
| Brain tuberculoma |
|
|
|
| Neurosarcoidosis |
|
|
|
 |
 |
 |
 |
|---|
Pulmonary tuberculosis must be distinguished from other cavitary lung lesions.
Differential Diagnosis
Pulmonary tuberculosis must be distinguished from other cavitary lung lesions.
| Causes of
lung cavities |
Differentiating Features | Differentiating radiological findings | Diagnosis
confirmation |
|---|---|---|---|
|
|
| |
|
|
|
|
|
|
| |
|
|
|
|
|
| ||
|
|
| |
|
|
||
|
|
| |
|
References
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 0443068399.
- ↑ Moon, Myung-Sang (2014). "Tuberculosis of Spine: Current Views in Diagnosis and Management". Asian Spine Journal. 8 (1): 97. doi:10.4184/asj.2014.8.1.97. ISSN 1976-1902.
- ↑ Garcia-Monco, Juan Carlos (2014). "Tuberculosis". 121: 1485–1499. doi:10.1016/B978-0-7020-4088-7.00100-0. ISSN 0072-9752.
- ↑ Mayosi, B. M. (2005). "Tuberculous Pericarditis". Circulation. 112 (23): 3608–3616. doi:10.1161/CIRCULATIONAHA.105.543066. ISSN 0009-7322.
- ↑ Daher, E. D. F.; da Silva Junior, G. B.; Barros, E. J. G. (2013). "Renal Tuberculosis in the Modern Era". American Journal of Tropical Medicine and Hygiene. 88 (1): 54–64. doi:10.4269/ajtmh.2013.12-0413. ISSN 0002-9637.
- ↑ Fontanilla, J.-M.; Barnes, A.; von Reyn, C. F. (2011). "Current Diagnosis and Management of Peripheral Tuberculous Lymphadenitis". Clinical Infectious Diseases. 53 (6): 555–562. doi:10.1093/cid/cir454. ISSN 1058-4838.
- ↑ 7.0 7.1 7.2 7.3 Chaudhuri MR (1973). "Primary pulmonary cavitating carcinomas". Thorax. 28 (3): 354–66. PMC 470041. PMID 4353362.
- ↑ 8.0 8.1 Mouroux J, Padovani B, Elkaïm D, Richelme H (1996). "Should cavitated bronchopulmonary cancers be considered a separate entity?". Ann. Thorac. Surg. 61 (2): 530–2. doi:10.1016/0003-4975(95)00973-6. PMID 8572761.
- ↑ 9.0 9.1 Onn A, Choe DH, Herbst RS, Correa AM, Munden RF, Truong MT, Vaporciyan AA, Isobe T, Gilcrease MZ, Marom EM (2005). "Tumor cavitation in stage I non-small cell lung cancer: epidermal growth factor receptor expression and prediction of poor outcome". Radiology. 237 (1): 342–7. doi:10.1148/radiol.2371041650. PMID 16183941.
- ↑ 10.0 10.1 10.2 10.3 Langford CA, Hoffman GS (1999). "Rare diseases.3: Wegener's granulomatosis". Thorax. 54 (7): 629–37. PMC 1745525. PMID 10377211.
- ↑ 11.0 11.1 Lee KS, Kim TS, Fujimoto K, Moriya H, Watanabe H, Tateishi U, Ashizawa K, Johkoh T, Kim EA, Kwon OJ (2003). "Thoracic manifestation of Wegener's granulomatosis: CT findings in 30 patients". Eur Radiol. 13 (1): 43–51. doi:10.1007/s00330-002-1422-2. PMID 12541109.
- ↑ 12.0 12.1 Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H, Bresnitz EA, DePalo L, Hunninghake G, Iannuzzi MC, Johns CJ, McLennan G, Moller DR, Newman LS, Rabin DL, Rose C, Rybicki B, Weinberger SE, Terrin ML, Knatterud GL, Cherniak R (2001). "Clinical characteristics of patients in a case control study of sarcoidosis". Am. J. Respir. Crit. Care Med. 164 (10 Pt 1): 1885–9. doi:10.1164/ajrccm.164.10.2104046. PMID 11734441.
- ↑ 13.0 13.1 Brauner MW, Grenier P, Mompoint D, Lenoir S, de Crémoux H (1989). "Pulmonary sarcoidosis: evaluation with high-resolution CT". Radiology. 172 (2): 467–71. doi:10.1148/radiology.172.2.2748828. PMID 2748828.
- ↑ 14.0 14.1 Murphy J, Schnyder P, Herold C, Flower C (1998). "Bronchiolitis obliterans organising pneumonia simulating bronchial carcinoma". Eur Radiol. 8 (7): 1165–9. doi:10.1007/s003300050527. PMID 9724431.
- ↑ 15.0 15.1 15.2 15.3 Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN (2008). "Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review". Ann Thorac Med. 3 (2): 67–75. doi:10.4103/1817-1737.39641. PMC 2700454. PMID 19561910.
- ↑ 16.0 16.1 Cordier JF, Loire R, Brune J (1989). "Idiopathic bronchiolitis obliterans organizing pneumonia. Definition of characteristic clinical profiles in a series of 16 patients". Chest. 96 (5): 999–1004. PMID 2805873.
- ↑ 17.0 17.1 Lee KS, Kullnig P, Hartman TE, Müller NL (1994). "Cryptogenic organizing pneumonia: CT findings in 43 patients". AJR Am J Roentgenol. 162 (3): 543–6. doi:10.2214/ajr.162.3.8109493. PMID 8109493.
- ↑ 18.0 18.1 Suri HS, Yi ES, Nowakowski GS, Vassallo R (2012). "Pulmonary langerhans cell histiocytosis". Orphanet J Rare Dis. 7: 16. doi:10.1186/1750-1172-7-16. PMC 3342091. PMID 22429393.
- ↑ 19.0 19.1 Moore AD, Godwin JD, Müller NL, Naidich DP, Hammar SP, Buschman DL, Takasugi JE, de Carvalho CR (1989). "Pulmonary histiocytosis X: comparison of radiographic and CT findings". Radiology. 172 (1): 249–54. doi:10.1148/radiology.172.1.2787035. PMID 2787035.
- ↑ Brouwer MC, Tunkel AR, McKhann GM, van de Beek D (2014). "Brain abscess". N. Engl. J. Med. 371 (5): 447–56. doi:10.1056/NEJMra1301635. PMID 25075836.
- ↑ "Brain Abscess — NEJM".
- ↑ 22.0 22.1 "Primary Brain Tumors in Adults - American Family Physician".
- ↑ "The Journal of Association of Chest Physicians - Tuberculoma of the brain - A diagnostic dilemma: Magnetic resonance spectroscopy a new ray of hope : Download PDF".
- ↑ 24.0 24.1 "Neurosarcoidosis".