Tissue plasminogen activator: Difference between revisions
No edit summary |
Matt Pijoan (talk | contribs) m (1 revision imported) |
||
| (6 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | {{Infobox_gene}} | ||
'''Tissue plasminogen activator''' (abbreviated '''tPA''' or '''PLAT''') is a [[protein]] involved in the breakdown of blood [[clot]]s. It is a [[serine protease]] ({{EC number|3.4.21.68}}) found on [[endothelial cell]]s, the cells that line the [[blood vessel]]s. As an [[enzyme]], it [[catalysis|catalyzes]] the conversion of [[plasminogen]] to [[plasmin]], the major enzyme responsible for clot breakdown. Human tPA has a molecular weight of ~70 kDa in the single-chain form.<ref name="tPA Human">{{cite web|url=https://www.sigmaaldrich.com/catalog/product/sigma/t5451?lang=en®ion=US|title=Tissue plasminogen activator human|publisher=Sigma-Aldrich|author=|date=9 July 2017|accessdate=11 May 2018}}</ref> | |||
}} | |||
{{ | |||
''' | tPA can be manufactured using [[Recombinant DNA|recombinant]] [[Biotechnology#Pharmaceutical products|biotechnology]] techniques; tPA produced by such means are referred to as '''recombinant tissue plasminogen activator''' ('''rtPA'''). Specific rtPAs include [[alteplase]], [[reteplase]], and [[tenecteplase]]. They are used in [[clinical medicine]] to treat [[embolic]] or [[thrombotic]] [[stroke]]. The use of this protein is contraindicated in [[hemorrhagic stroke]] and head trauma. The antidote for tPA in case of toxicity is [[aminocaproic acid]]. | ||
== | == Medical uses == | ||
tPA is used in some cases of diseases that feature [[blood clot]]s, such as [[pulmonary embolism]], [[myocardial infarction]], and [[stroke]], in a medical treatment called [[thrombolysis]]. The most common use is for ischemic stroke. It can either be administered systemically, in the case of acute [[myocardial infarction]], [[stroke|acute ischemic stroke]], and most cases of acute massive [[pulmonary embolism]], or administered through an arterial catheter directly to the site of occlusion in the case of peripheral arterial [[thrombus|thrombi]] and thrombi in the proximal deep veins of the leg.<ref name="Rivera-Bou">{{cite journal|url=http://emedicine.medscape.com/article/811234-overview+eMedicine+Specialties|title=Thrombolytic Therapy|date=2008-11-20|journal=|publisher=Medscape|vauthors=Rivera-Bou WL, Cabanas JG, Villanueva SE}}</ref> | |||
[[ | [[File:T-PA.png|thumb|A theoretical structure of the full t-PA enzyme in humans. Sugar residues are the light cyan-grey molecules, and the different domains are marked in different colours]] | ||
== | === Ischemic stroke === | ||
== | ==== Statistics ==== | ||
There have been twelve large scale, high-quality trials of rtPA in acute ischemic stroke. A meta-analysis of these trials concluded that rtPA given within 6 hours of a stroke significantly increased the odds of being alive and independent at final follow-up, particularly in patients treated within 3 hours. However a significant mortality rate was noted, mostly from intracranial haemorrhage at 7 days, but later mortality was not significant amongst treated and non-treated patients.<ref name="pmid22632907">{{cite journal | vauthors = Wardlaw JM, Murray V, Berge E, del Zoppo G, Sandercock P, Lindley RL, Cohen G | title = Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis | journal = Lancet | volume = 379 | issue = 9834 | pages = 2364–72 | date = June 2012 | pmid = 22632907 | pmc = 3386494 | doi = 10.1016/S0140-6736(12)60738-7 }}</ref> | |||
It has been suggested that if tPA is effective in ischemic stroke, it must be administered as early as possible after the onset of [[stroke#Signs and symptoms|stroke symptoms]], given that patients present to an ED in a timely manner.<ref name="pmid22632907" /><ref name="pmid22818644">{{cite journal | vauthors = DeMers G, Meurer WJ, Shih R, Rosenbaum S, Vilke GM | title = Tissue plasminogen activator and stroke: review of the literature for the clinician | journal = The Journal of Emergency Medicine | volume = 43 | issue = 6 | pages = 1149–54 | date = December 2012 | pmid = 22818644 | doi = 10.1016/j.jemermed.2012.05.005 }}</ref> Many national guidelines including the AHA have interpreted this cohort of studies as suggesting that there are specific subgroups who may benefit from tPA and thus recommend its use within a limited time window after the event. Protocol guidelines require its use intravenously within the first three hours of the event, after which its detriments may outweigh its benefits. | |||
For example, the Canadian Stroke Network guideline states "All patients with ''disabling'' acute ischemic stroke who can be treated within 4.5 hours of symptom onset should be evaluated without delay to determine their eligibility for treatment" with tPA.<ref name="CSN2010">{{cite book | vauthors = Lindsay, Gubitz G, Bayley M, Hill MD, Davies-Schinkel C, Singh S, Phillips S | agency = Canadian Stroke Strategy Best Practices and Standards Writing Group | title = Canadian best practice recommendations for stroke care | publisher = Canadian Stroke Network | location = Ottawa, ON | pages = 55–84 | chapter-url = http://www.guideline.gov/content.aspx?id=34088 | access-date = 30 November 2013 | chapter = Hyperacute stroke management | date = Dec 8, 2010 | archive-url = https://web.archive.org/web/20131203004044/http://www.guideline.gov/content.aspx?id=34088 | archive-date = 3 December 2013 | dead-url = yes | df = dmy-all }}</ref> Delayed presentation to the ED leads to decreased eligibility; as few as 3% of people qualify for this treatment.<ref>{{cite journal | vauthors = Hemmen T | title = Patient delay in acute stroke response | journal = European Journal of Neurology | volume = 15 | issue = 4 | pages = 315–6 | date = April 2008 | pmid = 18353121 | pmc = 2677077 | doi = 10.1111/j.1468-1331.2008.02083.x }}</ref> Similarly in the United States, the window of administration used to be 3 hours from onset of symptoms, but the newer guidelines also recommend use up to 4.5 hours after symptom onset, depending on the patient's presentation, past medical history, current [[Comorbidity|comorbidities]] and medication usage.<ref name="pmid19407232">{{cite journal | vauthors = Davis SM, Donnan GA | title = 4.5 hours: the new time window for tissue plasminogen activator in stroke | journal = Stroke | volume = 40 | issue = 6 | pages = 2266–7 | date = June 2009 | pmid = 19407232 | doi = 10.1161/STROKEAHA.108.544171 }}</ref> tPA appears to show benefit not only for large artery occlusions but also for [[lacunar stroke]]s. Since tPA dissolves [[blood clot]]s, there is risk of [[hemorrhage]] with its use. | |||
== | ==== Administration criteria ==== | ||
Use of tPA in the United States in treatment of patients who are eligible for its use, have no contraindications, and arrival at the treating facility less than 3 hours after onset of symptoms, is reported to have doubled from 2003 to 2011. Use on patients with mild deficits, of nonwhite race/ethnicity, and oldest old age increased. However, many patients who were eligible for treatment were not treated.<ref name="Medpage82313">{{cite web | url = http://www.medpagetoday.com/Cardiology/Strokes/41156 | title = Clot-Busting Drugs Used More Often in Stroke |vauthors=Bankhead C, Agus ZS | date = 2013-08-23 | format = | website = | publisher = Medpage Today }}</ref><ref name="AHA82013">{{cite journal | vauthors = Schwamm LH, Ali SF, Reeves MJ, Smith EE, Saver JL, Messe S, Bhatt DL, Grau-Sepulveda MV, Peterson ED, Fonarow GC | title = Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at Get With The Guidelines-Stroke hospitals | journal = Circulation: Cardiovascular Quality and Outcomes | volume = 6 | issue = 5 | pages = 543–9 | date = September 2013 | pmid = 24046398 | doi = 10.1161/CIRCOUTCOMES.111.000095 | quote = The frequency of IV tPA use among all AIS patients, regardless of contraindications, nearly doubled from 2003 to 2011. Treatment with tPA has expanded to include more patients with mild deficits, nonwhite race/ethnicity, and oldest old age }}</ref> | |||
== | tPA has also been given to patients with acute ischemic stroke above age 90 years old. Although a small fraction of patients 90 years and above treated with tPA for acute ischemic stroke recover, most patients have a poor 30-day functional outcome or die.<ref name="PMID 19339651">{{cite journal | vauthors = Mateen FJ, Nasser M, Spencer BR, Freeman WD, Shuaib A, Demaerschalk BM, Wijdicks EF | title = Outcomes of intravenous tissue plasminogen activator for acute ischemic stroke in patients aged 90 years or older | journal = Mayo Clinic Proceedings | volume = 84 | issue = 4 | pages = 334–8 | date = April 2009 | pmid = 19339651 | pmc = 2665978 | doi = 10.1016/S0025-6196(11)60542-9 }}</ref> Nonagenarians may do as well as octogenarians following treatment with IV-tPA for acute ischemic stroke.<ref name="PMID 20576948">{{cite journal | vauthors = Mateen FJ, Buchan AM, Hill MD | title = Outcomes of thrombolysis for acute ischemic stroke in octogenarians versus nonagenarians | journal = Stroke | volume = 41 | issue = 8 | pages = 1833–5 | date = August 2010 | pmid = 20576948 | doi = 10.1161/STROKEAHA.110.586438 }}</ref> In addition, people with [[frostbite]] treated with tPA had fewer [[amputation]]s than those not treated with tPA.<ref name="pmid17576891">{{cite journal | vauthors = Twomey JA, Peltier GL, Zera RT | title = An open-label study to evaluate the safety and efficacy of tissue plasminogen activator in treatment of severe frostbite | journal = J Trauma | volume = 59 | issue = 6 | pages = 1350–1354 | year = 2005 | doi=10.1097/01.ta.0000195517.50778.2e}}; and repeated by {{cite journal | vauthors = Bruen KJ, Ballard JR, Morris SE, Cochran A, Edelman LS, Saffle JR | title = Reduction of the incidence of amputation in frostbite injury with thrombolytic therapy | journal = Archives of Surgery | volume = 142 | issue = 6 | pages = 546–51; discussion 551–3 | date = June 2007 | pmid = 17576891 | doi = 10.1001/archsurg.142.6.546 }}</ref> | ||
{{ | |||
== | ==== General consensus on use ==== | ||
There is consensus amongst stroke specialists that tPA is the standard of care for eligible stroke patients, and benefits outweigh the risks. There is significant debate mainly in the emergency medicine community regarding recombinant tPA's effectiveness in [[ischemic stroke]]. The NNT Group on [[evidence-based medicine]] concluded that it was inappropriate to combine these twelve trials into a single analysis, because of substantial clinical heterogeneity (i.e., variations in study design, setting, and population characteristics).<ref name=NNT2013>{{cite web|last=Newman|first=David|title=Thrombolytics for Acute Ischemic Stroke: No benefit found|url=http://www.thennt.com/nnt/thrombolytics-for-stroke/|publisher=NNT Group|access-date=30 November 2013|date=March 25, 2013}}</ref> Examining each study individually, the NNT group noted that two of these studies showed benefit to patients given tPA (and that, using analytical methods that they think flawed); four studies showed harm and had to be stopped before completion; and the remaining studies showed neither benefit nor harm. On the basis of this evidence, the NNT Group recommended against the use of tPA in acute ischaemic stroke.<ref name=NNT2013 /> The NNT Group notes that the case for the 3-hour time window arises largely from analysis of two trials: NINDS-2 and subgroup results from IST-3. "However, presuming that early (0-3h) administration is better than later administration (3-4.5h or 4.5-6h) the subgroup results of IST-3 suggest an implausible biological effect in which early administration is beneficial, 3-4.5h administration is harmful, and 4.5-6h administration is again beneficial."<ref name=NNT2013 /> Indeed, even the original publication of the IST-3 trial found that time-window effects were not significant predictors of outcome (p=0.61).<ref name=IST-3>{{cite journal | vauthors = Sandercock P, Wardlaw JM, Lindley RI, Dennis M, Cohen G, Murray G, Innes K, Venables G, Czlonkowska A, Kobayashi A, Ricci S, Murray V, Berge E, Slot KB, Hankey GJ, Correia M, Peeters A, Matz K, Lyrer P, Gubitz G, Phillips SJ, Arauz A | title = The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial | journal = Lancet | volume = 379 | issue = 9834 | pages = 2352–63 | date = June 2012 | pmid = 22632908 | pmc = 3386495 | doi = 10.1016/S0140-6736(12)60768-5 }}</ref> In the UK, concerns by stroke specialists have led to a review by the [[Medicines and Healthcare products Regulatory Agency]].<ref name=BBC>{{cite news|last1=Brimelow|first1=Adam|title=Safety review into stroke clot-buster drug alteplase|url=https://www.bbc.co.uk/news/health-28900824|website=BBC News|publisher=British Broadcasting Corporation|access-date=29 June 2015|date=2014-08-22}}</ref> | |||
== | === Pulmonary embolism=== | ||
Pulmonary embolism (blood clots that have moved to the lung arteries) is usually treated with [[heparin]] generally followed by [[warfarin]]. If pulmonary embolism causes severe instability due to high pressure on the heart ("massive PE") and leads to low blood pressure, recombinant tPA is recommended.<ref name=ESC2014>{{cite journal | vauthors = Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, Gibbs JS, Huisman MV, Humbert M, Kucher N, Lang I, Lankeit M, Lekakis J, Maack C, Mayer E, Meneveau N, Perrier A, Pruszczyk P, Rasmussen LH, Schindler TH, Svitil P, Vonk Noordegraaf A, Zamorano JL, Zompatori M | title = 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism | journal = European Heart Journal | volume = 35 | issue = 43 | pages = 3033–69, 3069a–3069k | date = November 2014 | pmid = 25173341 | doi = 10.1093/eurheartj/ehu283 }}</ref><ref name=NICECG144>{{NICE|144|Venous thromboembolic diseases: the management of venous thromboembolic diseases and the role of thrombophilia testing|2012}}</ref><ref>{{cite journal | vauthors = Hirsh J, Guyatt G, Albers GW, Harrington R, Schünemann HJ | title = Executive summary: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) | journal = Chest | volume = 133 | issue = 6 Suppl | pages = 71S–109S | date = June 2008 | pmid = 18574259 | doi = 10.1378/chest.08-0693 }}</ref> | |||
=== Recombinant tissue plasminogen activators (r-tPA) === | |||
tPA was first produced by recombinant DNA techniques at Genentech in 1982.{{citation needed|date=August 2017}} | |||
Tissue-type plasminogen activators were initially identified and isolated from mammalian tissues after which a [[Complementary DNA|cDNA library]] was established with the use of [[reverse transcriptase]] and [[Messenger RNA|mRNA]] from human melanoma cells. The aforementioned <ins>[[Messenger RNA|mRNA]] </ins>was isolated using antibody based [[immunoprecipitation]]. The resulting cDNA library was subsequently screened via [[sequence analysis]] and compared to a whole [[Genomic library|genome library]] for confirmation of specific protein isolation and accuracy. cDNA was cloned into a synthetic [[plasmid]] and initially expressed in ''E. coli'' cells, followed by yeast cells with successful results confirmed via sequencing before attempting in mammalian cells. The transformants were selected with the use of [[Methotrexate]]. Methotrexate strengthens selection by inhibiting [[Dihydrofolate reductase|DHFR]] activity which then compels the cells to express more DHFR (exogenous) and consequently more recombinant protein to survive. The highly active transformants were then subsequently placed in a [[Industrial fermentation|industrial fermenter]]. The tPA which was then secreted into the culture medium was isolated and collected for therapeutic use. For pharmaceutical purposes, tPA was the first pharmaceutical drug produced synthetically with the use of mammalian cells, specifically Chinese hamster ovarian cells ([[Chinese hamster ovary cell|CHO]]). Recombinant tPA is commonly referred to as r-tPA and sold under multiple brand names.<ref>{{Cite news|url=http://www.biologydiscussion.com/dna/pharmaceutical-products-of-recombinant-dna-technology/10015.|title=Pharmaceutical Products of Recombinant DNA Technology|date=2015-09-21|work=Biology Discussion|access-date=2017-12-10}}</ref><ref>{{cite journal | vauthors = Pennica D, Holmes WE, Kohr WJ, Harkins RN, Vehar GA, Ward CA, Bennett WF, Yelverton E, Seeburg PH, Heyneker HL, Goeddel DV, Collen D | title = Cloning and expression of human tissue-type plasminogen activator cDNA in E. coli | journal = Nature | volume = 301 | issue = 5897 | pages = 214–21 | date = January 1983 | pmid = 6337343 | doi = 10.1038/301214a0 }}</ref> | |||
{| class="wikitable" | |||
|+Commercial r-tPA | |||
!Product Name | |||
!Notes | |||
|- | |||
|Activase ([[Alteplase]]) | |||
|FDA-approved for treatment of [[myocardial infarction]] with ST-elevation (STEMI), acute [[ischemic stroke]] (AIS), acute massive [[pulmonary embolism]], and [[central venous access device]]s (CVAD).<ref name=":0">{{Cite journal|date=2017-05-02|title=Thrombolytic Therapy: Background, Thrombolytic Agents, Thrombolytic Therapy for Acute Myocardial Infarction|url=http://emedicine.medscape.com/article/811234-overview+eMedicine+Specialties}}</ref> | |||
|- | |||
|[[Reteplase]] | |||
|FDA-approved for [[acute myocardial infarction]], where it has more convenient administration and faster thrombolysis than alteplase. This is because it is a second generation engineered TPA, hence its half life is up to 20 minutes which allows it to be administered as a bolus injection rather than an infusion like Alteplase.<ref name=":0" /> | |||
|- | |||
|[[Tenecteplase]] | |||
|Indicated in [[acute myocardial infarction]], showing fewer bleeding complications but otherwise similar mortality rates after one year compared to Alteplase.<ref name=":0" /> | |||
|- | |||
|[[Desmoteplase]] | |||
|Currently under clinical development. | |||
|} | |||
== Interactions == | |||
Tissue plasminogen activator has been shown to [[Protein-protein interaction|interact]] with: | |||
{{div col|colwidth=20em}} | |||
* [[Fibrinogen alpha chain]]<ref name = pmid11170397>{{cite journal | vauthors = Tsurupa G, Medved L | title = Identification and characterization of novel tPA- and plasminogen-binding sites within fibrin(ogen) alpha C-domains | journal = Biochemistry | volume = 40 | issue = 3 | pages = 801–8 | date = January 2001 | pmid = 11170397 | doi = 10.1021/bi001789t }}</ref><ref name = pmid3088041>{{cite journal | vauthors = Ichinose A, Takio K, Fujikawa K | title = Localization of the binding site of tissue-type plasminogen activator to fibrin | journal = The Journal of Clinical Investigation | volume = 78 | issue = 1 | pages = 163–9 | date = July 1986 | pmid = 3088041 | pmc = 329545 | doi = 10.1172/JCI112546 }}</ref> | |||
* [[LRP1]]<ref name = pmid10632583>{{cite journal | vauthors = Zhuo M, Holtzman DM, Li Y, Osaka H, DeMaro J, Jacquin M, Bu G | title = Role of tissue plasminogen activator receptor LRP in hippocampal long-term potentiation | journal = The Journal of Neuroscience | volume = 20 | issue = 2 | pages = 542–9 | date = January 2000 | pmid = 10632583 | doi = }}</ref><ref name = pmid1502153>{{cite journal | vauthors = Orth K, Madison EL, Gething MJ, Sambrook JF, Herz J | title = Complexes of tissue-type plasminogen activator and its serpin inhibitor plasminogen-activator inhibitor type 1 are internalized by means of the low density lipoprotein receptor-related protein/alpha 2-macroglobulin receptor | journal = Proceedings of the National Academy of Sciences of the United States of America | volume = 89 | issue = 16 | pages = 7422–6 | date = August 1992 | pmid = 1502153 | pmc = 49722 | doi = 10.1073/pnas.89.16.7422 }}</ref> | |||
* [[SERPINI1]]<ref name = pmid12354288>{{cite journal | vauthors = Parmar PK, Coates LC, Pearson JF, Hill RM, Birch NP | title = Neuroserpin regulates neurite outgrowth in nerve growth factor-treated PC12 cells | journal = Journal of Neurochemistry | volume = 82 | issue = 6 | pages = 1406–15 | date = September 2002 | pmid = 12354288 | doi = 10.1046/j.1471-4159.2002.01100.x }}</ref> | |||
{{Div col end}} | |||
== Function == | |||
[[File:Fibrinolysis.png|left|thumb|250px|A simplified illustration demonstrates clot breakdown ([[fibrinolysis]]), with blue arrows denoting stimulation, and red arrows inhibition.]] | |||
tPA and plasmin are the key enzymes of the fibrinolytic pathway in which tPA mediated plasmin generation occurs. | |||
To be specific, tPA cleaves the zymogen plasminogen at its Arg561 - Val562 peptide bond, into the serine protease plasmin.{{citation needed|date=August 2017}} | |||
Increased enzymatic activity causes [[hyperfibrinolysis]], which manifests as excessive bleeding and/or an increase of the vascular permeability.<ref name="Marcos-Contreras_2016">{{cite journal | vauthors = Marcos-Contreras OA, Martinez de Lizarrondo S, Bardou I, Orset C, Pruvost M, Anfray A, Frigout Y, Hommet Y, Lebouvier L, Montaner J, Vivien D, Gauberti M | title = Hyperfibrinolysis increases blood-brain barrier permeability by a plasmin- and bradykinin-dependent mechanism | journal = Blood | volume = 128 | issue = 20 | pages = 2423–2434 | date = November 2016 | pmid = 27531677 | doi = 10.1182/blood-2016-03-705384 }}</ref> Decreased activity leads to [[wiktionary:hypofibrinolysis|hypofibrinolysis]] which can result in [[thrombosis]] or [[embolism]]. | |||
In ischemic stroke patients, decreased tPA activity was reported to be associated with an increase in plasma P-selectin concentration.<ref name="pmid15916851">{{cite journal | vauthors = Wang J, Li J, Liu Q | title = Association between platelet activation and fibrinolysis in acute stroke patients | journal = Neuroscience Letters | volume = 384 | issue = 3 | pages = 305–9 | date = August 2005 | pmid = 15916851 | doi = 10.1016/j.neulet.2005.04.090 }}</ref> | |||
Tissue plasminogen activator also plays a role in [[cell migration]] and [[tissue remodeling]].{{citation needed|date=August 2017}} | |||
=== Physiology and regulation === | |||
[[File:Tpa pathways .png|thumb| | |||
In vivo mechanism of action of tPA within the fibrinolytic system. tPA can go one of three ways in the body; (1) uptaken by the liver and cleared through receptors therein, (2) inhibited by a plasminogen activator inhibitor (PAI) and subsequently cleared from the liver, or (3) through the activation of plasminogen to plasmin for degradation to result in fibrin degradation product (FDP).<ref name=":1" /><ref name=":2">{{cite journal | vauthors = Gravanis I, Tsirka SE | title = Tissue-type plasminogen activator as a therapeutic target in stroke | journal = Expert Opinion on Therapeutic Targets | volume = 12 | issue = 2 | pages = 159–70 | date = February 2008 | pmid = 18208365 | doi = 10.1517/14728222.12.2.159 | pmc = 3824365 }}</ref> | |||
|440x440px]] | |||
Once in the body, tPA has three main routes it can take, with one resulting in desired [[Thrombolysis|thrombolytic]] activity (see figure). For starters, following administration and release, tPA can be absorbed by the liver and cleared from the body through receptors present therein. One of the specific receptors responsible for this processes is a [[scavenger protein]], specifically the [[LDL-receptor-related protein-associated protein|LDL Receptor Related Protein]] ([[LRP1]]).<ref name=":2" /> tPA additionally can be bound by a plasminogen activator inhibitor ([[Plasminogen activator inhibitor-1|PAI]]), resulting in inactivation of its activity, and following clearing from the body by the liver. Lastly, tPA can bind plasminogen cleaving off the bound [[plasmin]] from it. Plasmin, another type of [[protease]], can either be bound by a plasmin inhibitor, or work to degrade [[fibrin]] clots, which is the highest utilized and desired pathway.<ref name=":1">{{Cite web|url=http://diapharma.com/tissue-plasminogen-activator-tpa/|title=Tissue Plasminogen Activator (tPA) {{!}}|website=diapharma.com|access-date=2017-12-10}}</ref> | |||
== Genetics == | |||
Tissue plasminogen activator is a [[protein]] encoded by the ''PLAT'' [[gene]], which is located on [[chromosome 8]]. The [[primary transcript]] produced by this gene undergoes [[alternative splicing]], producing three distinct [[messenger RNA]]s.{{citation needed|date=August 2017}} | |||
== See also == | |||
{{Portal|Molecular and cellular biology}} | |||
* [[Ultrasound-enhanced systemic thrombolysis]] | |||
{{Clear}} | |||
== References == | |||
{{Reflist|32em}} | |||
== Further reading == | |||
{{Refbegin|35em}} | |||
* {{cite journal | vauthors = Rijken DC | title = Relationships between structure and function of tissue-type plasminogen activator | journal = Klinische Wochenschrift | volume = 66 Suppl 12 | issue = | pages = 33–9 | year = 1988 | pmid = 3126346 | doi = }} | |||
* {{cite journal | vauthors = Bode W, Renatus M | title = Tissue-type plasminogen activator: variants and crystal/solution structures demarcate structural determinants of function | journal = Current Opinion in Structural Biology | volume = 7 | issue = 6 | pages = 865–72 | date = December 1997 | pmid = 9434908 | doi = 10.1016/S0959-440X(97)80159-5 }} | |||
* {{cite journal | vauthors =Collen D, Billiau A, Edy J, De Somer P | title = Identification of the human plasma protein which inhibits fibrinolysis associated with malignant cells | journal = Biochim Biophys Acta |year=1977 | volume = 499 | issue = 2 | pages = 194–201 |doi=10.1016/0304-4165(77)90002-2 | pmid = 198009 |url=https://www.sciencedirect.com/science/article/pii/0304416577900022 | |||
}} | |||
* {{cite journal | vauthors = Anglés-Cano E, Rojas G | title = Apolipoprotein(a): structure-function relationship at the lysine-binding site and plasminogen activator cleavage site | journal = Biological Chemistry | volume = 383 | issue = 1 | pages = 93–9 | date = January 2002 | pmid = 11928826 | doi = 10.1515/BC.2002.009 }} | |||
* {{cite journal | vauthors = Wang J, Li J, Liu Q | title = Association between platelet activation and fibrinolysis in acute stroke patients | journal = Neuroscience Letters | volume = 384 | issue = 3 | pages = 305–9 | date = August 2005 | pmid = 15916851 | doi = 10.1016/j.neulet.2005.04.090 }} | |||
* {{cite journal | vauthors = Ny T, Wahlberg P, Brändström IJ | title = Matrix remodeling in the ovary: regulation and functional role of the plasminogen activator and matrix metalloproteinase systems | journal = Molecular and Cellular Endocrinology | volume = 187 | issue = 1–2 | pages = 29–38 | date = February 2002 | pmid = 11988309 | doi = 10.1016/S0303-7207(01)00711-0 }} | |||
* {{cite journal | vauthors = Teesalu T, Kulla A, Asser T, Koskiniemi M, Vaheri A | title = Tissue plasminogen activator as a key effector in neurobiology and neuropathology | journal = Biochemical Society Transactions | volume = 30 | issue = 2 | pages = 183–9 | date = April 2002 | pmid = 12023848 | doi = 10.1042/BST0300183 }} | |||
* {{cite journal | vauthors = Pang PT, Lu B | title = Regulation of late-phase LTP and long-term memory in normal and aging hippocampus: role of secreted proteins tPA and BDNF | journal = Ageing Research Reviews | volume = 3 | issue = 4 | pages = 407–30 | date = November 2004 | pmid = 15541709 | doi = 10.1016/j.arr.2004.07.002 }} | |||
* {{cite journal | vauthors = Sheehan JJ, Tsirka SE | title = Fibrin-modifying serine proteases thrombin, tPA, and plasmin in ischemic stroke: a review | journal = Glia | volume = 50 | issue = 4 | pages = 340–50 | date = June 2005 | pmid = 15846799 | doi = 10.1002/glia.20150 }} | |||
* {{cite journal | vauthors = Wang J, Rogove AD, Tsirka AE, Tsirka SE | title = Protective role of tuftsin fragment 1-3 in an animal model of intracerebral hemorrhage | journal = Annals of Neurology | volume = 54 | issue = 5 | pages = 655–64 | date = November 2003 | pmid = 14595655 | doi = 10.1002/ana.10750 }} | |||
{{Refend}} | |||
== External links == | |||
* [http://atvb.ahajournals.org/content/29/8/1151.full History of Discovery: The Tissue-Type Plasminogen Activator Story], Collen, D., Lijnen, H.R. | |||
* [http://www.gene.com/media/press-releases/4185/1982-07-23/tpa-produced-by-recombinant-dna-techniqu Genentech Press Release 1982] | |||
* [http://www.americanheart.org/presenter.jhtml?identifier=4751 Tissue Plasminogen Activator] from the [[American Heart Association]] | |||
* [http://www.sciam.com/article.cfm?chanID=sa004&articleID=00055D80-04DC-12D8-BDFD83414B7F0000 Widening the Window : Strategies to buy time in treating ischemic stroke] - Scientific American (August 2005) | |||
* [https://www.youtube.com/watch?v=3MtWO4MGNCI Study expands window for effective stroke treatment] - explained on YouTube | |||
{{PDB Gallery|geneid=5327}} | |||
{{Coagulation}} | {{Coagulation}} | ||
{{Antithrombotics}} | |||
{{Serine endopeptidases}} | {{Serine endopeptidases}} | ||
{{ | {{Enzymes}} | ||
{{ | |||
[[Category: | {{DEFAULTSORT:Tissue Plasminogen Activator}} | ||
[[Category:Antithrombotic enzymes]] | |||
[[Category:EC 3.4.21]] | [[Category:EC 3.4.21]] | ||
Latest revision as of 08:49, 10 January 2019
| VALUE_ERROR (nil) | |||||||
|---|---|---|---|---|---|---|---|
| Identifiers | |||||||
| Aliases | |||||||
| External IDs | GeneCards: [1] | ||||||
| Orthologs | |||||||
| Species | Human | Mouse | |||||
| Entrez |
|
| |||||
| Ensembl |
|
| |||||
| UniProt |
|
| |||||
| RefSeq (mRNA) |
|
| |||||
| RefSeq (protein) |
|
| |||||
| Location (UCSC) | n/a | n/a | |||||
| PubMed search | n/a | n/a | |||||
| Wikidata | |||||||
| |||||||
Tissue plasminogen activator (abbreviated tPA or PLAT) is a protein involved in the breakdown of blood clots. It is a serine protease (EC 3.4.21.68) found on endothelial cells, the cells that line the blood vessels. As an enzyme, it catalyzes the conversion of plasminogen to plasmin, the major enzyme responsible for clot breakdown. Human tPA has a molecular weight of ~70 kDa in the single-chain form.[1]
tPA can be manufactured using recombinant biotechnology techniques; tPA produced by such means are referred to as recombinant tissue plasminogen activator (rtPA). Specific rtPAs include alteplase, reteplase, and tenecteplase. They are used in clinical medicine to treat embolic or thrombotic stroke. The use of this protein is contraindicated in hemorrhagic stroke and head trauma. The antidote for tPA in case of toxicity is aminocaproic acid.
Medical uses
tPA is used in some cases of diseases that feature blood clots, such as pulmonary embolism, myocardial infarction, and stroke, in a medical treatment called thrombolysis. The most common use is for ischemic stroke. It can either be administered systemically, in the case of acute myocardial infarction, acute ischemic stroke, and most cases of acute massive pulmonary embolism, or administered through an arterial catheter directly to the site of occlusion in the case of peripheral arterial thrombi and thrombi in the proximal deep veins of the leg.[2]
Ischemic stroke
Statistics
There have been twelve large scale, high-quality trials of rtPA in acute ischemic stroke. A meta-analysis of these trials concluded that rtPA given within 6 hours of a stroke significantly increased the odds of being alive and independent at final follow-up, particularly in patients treated within 3 hours. However a significant mortality rate was noted, mostly from intracranial haemorrhage at 7 days, but later mortality was not significant amongst treated and non-treated patients.[3]
It has been suggested that if tPA is effective in ischemic stroke, it must be administered as early as possible after the onset of stroke symptoms, given that patients present to an ED in a timely manner.[3][4] Many national guidelines including the AHA have interpreted this cohort of studies as suggesting that there are specific subgroups who may benefit from tPA and thus recommend its use within a limited time window after the event. Protocol guidelines require its use intravenously within the first three hours of the event, after which its detriments may outweigh its benefits.
For example, the Canadian Stroke Network guideline states "All patients with disabling acute ischemic stroke who can be treated within 4.5 hours of symptom onset should be evaluated without delay to determine their eligibility for treatment" with tPA.[5] Delayed presentation to the ED leads to decreased eligibility; as few as 3% of people qualify for this treatment.[6] Similarly in the United States, the window of administration used to be 3 hours from onset of symptoms, but the newer guidelines also recommend use up to 4.5 hours after symptom onset, depending on the patient's presentation, past medical history, current comorbidities and medication usage.[7] tPA appears to show benefit not only for large artery occlusions but also for lacunar strokes. Since tPA dissolves blood clots, there is risk of hemorrhage with its use.
Administration criteria
Use of tPA in the United States in treatment of patients who are eligible for its use, have no contraindications, and arrival at the treating facility less than 3 hours after onset of symptoms, is reported to have doubled from 2003 to 2011. Use on patients with mild deficits, of nonwhite race/ethnicity, and oldest old age increased. However, many patients who were eligible for treatment were not treated.[8][9]
tPA has also been given to patients with acute ischemic stroke above age 90 years old. Although a small fraction of patients 90 years and above treated with tPA for acute ischemic stroke recover, most patients have a poor 30-day functional outcome or die.[10] Nonagenarians may do as well as octogenarians following treatment with IV-tPA for acute ischemic stroke.[11] In addition, people with frostbite treated with tPA had fewer amputations than those not treated with tPA.[12]
General consensus on use
There is consensus amongst stroke specialists that tPA is the standard of care for eligible stroke patients, and benefits outweigh the risks. There is significant debate mainly in the emergency medicine community regarding recombinant tPA's effectiveness in ischemic stroke. The NNT Group on evidence-based medicine concluded that it was inappropriate to combine these twelve trials into a single analysis, because of substantial clinical heterogeneity (i.e., variations in study design, setting, and population characteristics).[13] Examining each study individually, the NNT group noted that two of these studies showed benefit to patients given tPA (and that, using analytical methods that they think flawed); four studies showed harm and had to be stopped before completion; and the remaining studies showed neither benefit nor harm. On the basis of this evidence, the NNT Group recommended against the use of tPA in acute ischaemic stroke.[13] The NNT Group notes that the case for the 3-hour time window arises largely from analysis of two trials: NINDS-2 and subgroup results from IST-3. "However, presuming that early (0-3h) administration is better than later administration (3-4.5h or 4.5-6h) the subgroup results of IST-3 suggest an implausible biological effect in which early administration is beneficial, 3-4.5h administration is harmful, and 4.5-6h administration is again beneficial."[13] Indeed, even the original publication of the IST-3 trial found that time-window effects were not significant predictors of outcome (p=0.61).[14] In the UK, concerns by stroke specialists have led to a review by the Medicines and Healthcare products Regulatory Agency.[15]
Pulmonary embolism
Pulmonary embolism (blood clots that have moved to the lung arteries) is usually treated with heparin generally followed by warfarin. If pulmonary embolism causes severe instability due to high pressure on the heart ("massive PE") and leads to low blood pressure, recombinant tPA is recommended.[16][17][18]
Recombinant tissue plasminogen activators (r-tPA)
tPA was first produced by recombinant DNA techniques at Genentech in 1982.[citation needed]
Tissue-type plasminogen activators were initially identified and isolated from mammalian tissues after which a cDNA library was established with the use of reverse transcriptase and mRNA from human melanoma cells. The aforementioned mRNA was isolated using antibody based immunoprecipitation. The resulting cDNA library was subsequently screened via sequence analysis and compared to a whole genome library for confirmation of specific protein isolation and accuracy. cDNA was cloned into a synthetic plasmid and initially expressed in E. coli cells, followed by yeast cells with successful results confirmed via sequencing before attempting in mammalian cells. The transformants were selected with the use of Methotrexate. Methotrexate strengthens selection by inhibiting DHFR activity which then compels the cells to express more DHFR (exogenous) and consequently more recombinant protein to survive. The highly active transformants were then subsequently placed in a industrial fermenter. The tPA which was then secreted into the culture medium was isolated and collected for therapeutic use. For pharmaceutical purposes, tPA was the first pharmaceutical drug produced synthetically with the use of mammalian cells, specifically Chinese hamster ovarian cells (CHO). Recombinant tPA is commonly referred to as r-tPA and sold under multiple brand names.[19][20]
| Product Name | Notes |
|---|---|
| Activase (Alteplase) | FDA-approved for treatment of myocardial infarction with ST-elevation (STEMI), acute ischemic stroke (AIS), acute massive pulmonary embolism, and central venous access devices (CVAD).[21] |
| Reteplase | FDA-approved for acute myocardial infarction, where it has more convenient administration and faster thrombolysis than alteplase. This is because it is a second generation engineered TPA, hence its half life is up to 20 minutes which allows it to be administered as a bolus injection rather than an infusion like Alteplase.[21] |
| Tenecteplase | Indicated in acute myocardial infarction, showing fewer bleeding complications but otherwise similar mortality rates after one year compared to Alteplase.[21] |
| Desmoteplase | Currently under clinical development. |
Interactions
Tissue plasminogen activator has been shown to interact with:
Function
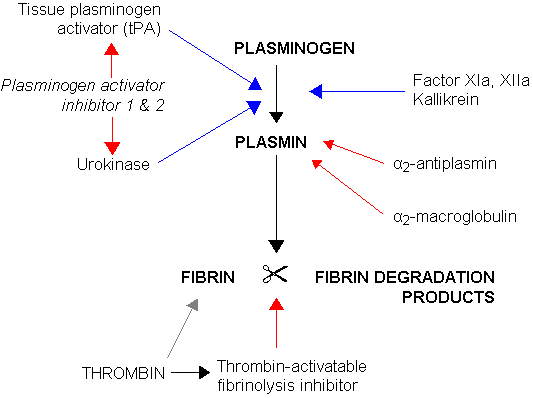
tPA and plasmin are the key enzymes of the fibrinolytic pathway in which tPA mediated plasmin generation occurs.
To be specific, tPA cleaves the zymogen plasminogen at its Arg561 - Val562 peptide bond, into the serine protease plasmin.[citation needed]
Increased enzymatic activity causes hyperfibrinolysis, which manifests as excessive bleeding and/or an increase of the vascular permeability.[27] Decreased activity leads to hypofibrinolysis which can result in thrombosis or embolism.
In ischemic stroke patients, decreased tPA activity was reported to be associated with an increase in plasma P-selectin concentration.[28]
Tissue plasminogen activator also plays a role in cell migration and tissue remodeling.[citation needed]
Physiology and regulation
Once in the body, tPA has three main routes it can take, with one resulting in desired thrombolytic activity (see figure). For starters, following administration and release, tPA can be absorbed by the liver and cleared from the body through receptors present therein. One of the specific receptors responsible for this processes is a scavenger protein, specifically the LDL Receptor Related Protein (LRP1).[30] tPA additionally can be bound by a plasminogen activator inhibitor (PAI), resulting in inactivation of its activity, and following clearing from the body by the liver. Lastly, tPA can bind plasminogen cleaving off the bound plasmin from it. Plasmin, another type of protease, can either be bound by a plasmin inhibitor, or work to degrade fibrin clots, which is the highest utilized and desired pathway.[29]
Genetics
Tissue plasminogen activator is a protein encoded by the PLAT gene, which is located on chromosome 8. The primary transcript produced by this gene undergoes alternative splicing, producing three distinct messenger RNAs.[citation needed]
See also
References
- ↑ "Tissue plasminogen activator human". Sigma-Aldrich. 9 July 2017. Retrieved 11 May 2018.
- ↑ Rivera-Bou WL, Cabanas JG, Villanueva SE (2008-11-20). "Thrombolytic Therapy". Medscape.
- ↑ 3.0 3.1 Wardlaw JM, Murray V, Berge E, del Zoppo G, Sandercock P, Lindley RL, Cohen G (June 2012). "Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis". Lancet. 379 (9834): 2364–72. doi:10.1016/S0140-6736(12)60738-7. PMC 3386494. PMID 22632907.
- ↑ DeMers G, Meurer WJ, Shih R, Rosenbaum S, Vilke GM (December 2012). "Tissue plasminogen activator and stroke: review of the literature for the clinician". The Journal of Emergency Medicine. 43 (6): 1149–54. doi:10.1016/j.jemermed.2012.05.005. PMID 22818644.
- ↑ Lindsay, Gubitz G, Bayley M, Hill MD, Davies-Schinkel C, Singh S, Phillips S (8 December 2010). "Hyperacute stroke management". Canadian best practice recommendations for stroke care. Ottawa, ON: Canadian Stroke Network. Canadian Stroke Strategy Best Practices and Standards Writing Group. pp. 55–84. Archived from the original on 3 December 2013. Retrieved 30 November 2013.
- ↑ Hemmen T (April 2008). "Patient delay in acute stroke response". European Journal of Neurology. 15 (4): 315–6. doi:10.1111/j.1468-1331.2008.02083.x. PMC 2677077. PMID 18353121.
- ↑ Davis SM, Donnan GA (June 2009). "4.5 hours: the new time window for tissue plasminogen activator in stroke". Stroke. 40 (6): 2266–7. doi:10.1161/STROKEAHA.108.544171. PMID 19407232.
- ↑ Bankhead C, Agus ZS (2013-08-23). "Clot-Busting Drugs Used More Often in Stroke". Medpage Today.
- ↑ Schwamm LH, Ali SF, Reeves MJ, Smith EE, Saver JL, Messe S, Bhatt DL, Grau-Sepulveda MV, Peterson ED, Fonarow GC (September 2013). "Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at Get With The Guidelines-Stroke hospitals". Circulation: Cardiovascular Quality and Outcomes. 6 (5): 543–9. doi:10.1161/CIRCOUTCOMES.111.000095. PMID 24046398.
The frequency of IV tPA use among all AIS patients, regardless of contraindications, nearly doubled from 2003 to 2011. Treatment with tPA has expanded to include more patients with mild deficits, nonwhite race/ethnicity, and oldest old age
- ↑ Mateen FJ, Nasser M, Spencer BR, Freeman WD, Shuaib A, Demaerschalk BM, Wijdicks EF (April 2009). "Outcomes of intravenous tissue plasminogen activator for acute ischemic stroke in patients aged 90 years or older". Mayo Clinic Proceedings. 84 (4): 334–8. doi:10.1016/S0025-6196(11)60542-9. PMC 2665978. PMID 19339651.
- ↑ Mateen FJ, Buchan AM, Hill MD (August 2010). "Outcomes of thrombolysis for acute ischemic stroke in octogenarians versus nonagenarians". Stroke. 41 (8): 1833–5. doi:10.1161/STROKEAHA.110.586438. PMID 20576948.
- ↑ Twomey JA, Peltier GL, Zera RT (2005). "An open-label study to evaluate the safety and efficacy of tissue plasminogen activator in treatment of severe frostbite". J Trauma. 59 (6): 1350–1354. doi:10.1097/01.ta.0000195517.50778.2e.; and repeated by Bruen KJ, Ballard JR, Morris SE, Cochran A, Edelman LS, Saffle JR (June 2007). "Reduction of the incidence of amputation in frostbite injury with thrombolytic therapy". Archives of Surgery. 142 (6): 546–51, discussion 551–3. doi:10.1001/archsurg.142.6.546. PMID 17576891.
- ↑ 13.0 13.1 13.2 Newman, David (March 25, 2013). "Thrombolytics for Acute Ischemic Stroke: No benefit found". NNT Group. Retrieved 30 November 2013.
- ↑ Sandercock P, Wardlaw JM, Lindley RI, Dennis M, Cohen G, Murray G, Innes K, Venables G, Czlonkowska A, Kobayashi A, Ricci S, Murray V, Berge E, Slot KB, Hankey GJ, Correia M, Peeters A, Matz K, Lyrer P, Gubitz G, Phillips SJ, Arauz A (June 2012). "The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial". Lancet. 379 (9834): 2352–63. doi:10.1016/S0140-6736(12)60768-5. PMC 3386495. PMID 22632908.
- ↑ Brimelow, Adam (2014-08-22). "Safety review into stroke clot-buster drug alteplase". BBC News. British Broadcasting Corporation. Retrieved 29 June 2015.
- ↑ Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, Gibbs JS, Huisman MV, Humbert M, Kucher N, Lang I, Lankeit M, Lekakis J, Maack C, Mayer E, Meneveau N, Perrier A, Pruszczyk P, Rasmussen LH, Schindler TH, Svitil P, Vonk Noordegraaf A, Zamorano JL, Zompatori M (November 2014). "2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism". European Heart Journal. 35 (43): 3033–69, 3069a–3069k. doi:10.1093/eurheartj/ehu283. PMID 25173341.
- ↑ National Institute for Health and Clinical Excellence. Clinical guideline 144: Venous thromboembolic diseases: the management of venous thromboembolic diseases and the role of thrombophilia testing. London, 2012.
- ↑ Hirsh J, Guyatt G, Albers GW, Harrington R, Schünemann HJ (June 2008). "Executive summary: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition)". Chest. 133 (6 Suppl): 71S–109S. doi:10.1378/chest.08-0693. PMID 18574259.
- ↑ "Pharmaceutical Products of Recombinant DNA Technology". Biology Discussion. 2015-09-21. Retrieved 2017-12-10.
- ↑ Pennica D, Holmes WE, Kohr WJ, Harkins RN, Vehar GA, Ward CA, Bennett WF, Yelverton E, Seeburg PH, Heyneker HL, Goeddel DV, Collen D (January 1983). "Cloning and expression of human tissue-type plasminogen activator cDNA in E. coli". Nature. 301 (5897): 214–21. doi:10.1038/301214a0. PMID 6337343.
- ↑ 21.0 21.1 21.2 "Thrombolytic Therapy: Background, Thrombolytic Agents, Thrombolytic Therapy for Acute Myocardial Infarction". 2017-05-02.
- ↑ Tsurupa G, Medved L (January 2001). "Identification and characterization of novel tPA- and plasminogen-binding sites within fibrin(ogen) alpha C-domains". Biochemistry. 40 (3): 801–8. doi:10.1021/bi001789t. PMID 11170397.
- ↑ Ichinose A, Takio K, Fujikawa K (July 1986). "Localization of the binding site of tissue-type plasminogen activator to fibrin". The Journal of Clinical Investigation. 78 (1): 163–9. doi:10.1172/JCI112546. PMC 329545. PMID 3088041.
- ↑ Zhuo M, Holtzman DM, Li Y, Osaka H, DeMaro J, Jacquin M, Bu G (January 2000). "Role of tissue plasminogen activator receptor LRP in hippocampal long-term potentiation". The Journal of Neuroscience. 20 (2): 542–9. PMID 10632583.
- ↑ Orth K, Madison EL, Gething MJ, Sambrook JF, Herz J (August 1992). "Complexes of tissue-type plasminogen activator and its serpin inhibitor plasminogen-activator inhibitor type 1 are internalized by means of the low density lipoprotein receptor-related protein/alpha 2-macroglobulin receptor". Proceedings of the National Academy of Sciences of the United States of America. 89 (16): 7422–6. doi:10.1073/pnas.89.16.7422. PMC 49722. PMID 1502153.
- ↑ Parmar PK, Coates LC, Pearson JF, Hill RM, Birch NP (September 2002). "Neuroserpin regulates neurite outgrowth in nerve growth factor-treated PC12 cells". Journal of Neurochemistry. 82 (6): 1406–15. doi:10.1046/j.1471-4159.2002.01100.x. PMID 12354288.
- ↑ Marcos-Contreras OA, Martinez de Lizarrondo S, Bardou I, Orset C, Pruvost M, Anfray A, Frigout Y, Hommet Y, Lebouvier L, Montaner J, Vivien D, Gauberti M (November 2016). "Hyperfibrinolysis increases blood-brain barrier permeability by a plasmin- and bradykinin-dependent mechanism". Blood. 128 (20): 2423–2434. doi:10.1182/blood-2016-03-705384. PMID 27531677.
- ↑ Wang J, Li J, Liu Q (August 2005). "Association between platelet activation and fibrinolysis in acute stroke patients". Neuroscience Letters. 384 (3): 305–9. doi:10.1016/j.neulet.2005.04.090. PMID 15916851.
- ↑ 29.0 29.1 "Tissue Plasminogen Activator (tPA)". diapharma.com. Retrieved 2017-12-10.
- ↑ 30.0 30.1 Gravanis I, Tsirka SE (February 2008). "Tissue-type plasminogen activator as a therapeutic target in stroke". Expert Opinion on Therapeutic Targets. 12 (2): 159–70. doi:10.1517/14728222.12.2.159. PMC 3824365. PMID 18208365.
Further reading
- Rijken DC (1988). "Relationships between structure and function of tissue-type plasminogen activator". Klinische Wochenschrift. 66 Suppl 12: 33–9. PMID 3126346.
- Bode W, Renatus M (December 1997). "Tissue-type plasminogen activator: variants and crystal/solution structures demarcate structural determinants of function". Current Opinion in Structural Biology. 7 (6): 865–72. doi:10.1016/S0959-440X(97)80159-5. PMID 9434908.
- Collen D, Billiau A, Edy J, De Somer P (1977). "Identification of the human plasma protein which inhibits fibrinolysis associated with malignant cells". Biochim Biophys Acta. 499 (2): 194–201. doi:10.1016/0304-4165(77)90002-2. PMID 198009.
- Anglés-Cano E, Rojas G (January 2002). "Apolipoprotein(a): structure-function relationship at the lysine-binding site and plasminogen activator cleavage site". Biological Chemistry. 383 (1): 93–9. doi:10.1515/BC.2002.009. PMID 11928826.
- Wang J, Li J, Liu Q (August 2005). "Association between platelet activation and fibrinolysis in acute stroke patients". Neuroscience Letters. 384 (3): 305–9. doi:10.1016/j.neulet.2005.04.090. PMID 15916851.
- Ny T, Wahlberg P, Brändström IJ (February 2002). "Matrix remodeling in the ovary: regulation and functional role of the plasminogen activator and matrix metalloproteinase systems". Molecular and Cellular Endocrinology. 187 (1–2): 29–38. doi:10.1016/S0303-7207(01)00711-0. PMID 11988309.
- Teesalu T, Kulla A, Asser T, Koskiniemi M, Vaheri A (April 2002). "Tissue plasminogen activator as a key effector in neurobiology and neuropathology". Biochemical Society Transactions. 30 (2): 183–9. doi:10.1042/BST0300183. PMID 12023848.
- Pang PT, Lu B (November 2004). "Regulation of late-phase LTP and long-term memory in normal and aging hippocampus: role of secreted proteins tPA and BDNF". Ageing Research Reviews. 3 (4): 407–30. doi:10.1016/j.arr.2004.07.002. PMID 15541709.
- Sheehan JJ, Tsirka SE (June 2005). "Fibrin-modifying serine proteases thrombin, tPA, and plasmin in ischemic stroke: a review". Glia. 50 (4): 340–50. doi:10.1002/glia.20150. PMID 15846799.
- Wang J, Rogove AD, Tsirka AE, Tsirka SE (November 2003). "Protective role of tuftsin fragment 1-3 in an animal model of intracerebral hemorrhage". Annals of Neurology. 54 (5): 655–64. doi:10.1002/ana.10750. PMID 14595655.
External links
- History of Discovery: The Tissue-Type Plasminogen Activator Story, Collen, D., Lijnen, H.R.
- Genentech Press Release 1982
- Tissue Plasminogen Activator from the American Heart Association
- Widening the Window : Strategies to buy time in treating ischemic stroke - Scientific American (August 2005)
- Study expands window for effective stroke treatment - explained on YouTube