Community acquired pneumonia resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Chetan Lokhande, M.B.B.S [2]
Overview
A lower respiratory tract infection in a previously normal individual acquired through normal social contact rather than contracting it in a hospital. Community-acquired pneumonia is a disease in which individuals who have not recently been hospitalized develop an infection of the lungs. CAP is a common illness and can affect people of all ages. It often causes problems like breathing difficulties, fever, chest pains, and a cough. CAP occurs when the alveoli become filled with fluid and cannot work effectively. It occurs throughout the world and is a leading cause of illness and death. Causes of CAP include bacteria, viruses, fungi, and parasites. CAP can be diagnosed by its symptoms and a physical examination alone, though x-rays, examinations of the sputum, and other tests are often used. CAP is primarily treated with antibiotic medication. Some forms of CAP can be prevented by vaccination.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. Complications of community acquired pneumonia, such as pleural effusion, lung abscess, bacteremia and septicemia are life-threatening conditions and must be treated as such irrespective of the causes.
Common Causes
Following are the causes listed according to the microbiological etiology
- Typical Bacteria
- Streptococcus pneumoniae
- Haemophilus influenzae
- Escherichia coli
- Klebsiella pneumoniae
- Pseudomonas aeruginosa
- Atypical Bacteria
- Viruses
Following are the causes listed according to the the location of the patient[1][2][3]
- Outpatient
- Streptococcus pneumoniae
- Mycoplasma pneumoniae
- Haemophilus influenzae
- Chlamydophila pneumoniae
- Influenza A and B, adenovirus, respiratory syncytial virus, parainfluenza
- Inpatient (non-ICU)
- Streptococcus pneumoniae
- Mycoplasma pneumoniae
- Haemophilus influenzae
- Legionella
- Aspiration
- Influenza A and B, adenovirus, respiratory syncytial virus, parainfluenza
- Yersinia enterocolitica
- Inpatient (ICU)
- Streptococcus pneumoniae
- Staphylococcus aureus
- Legionella
- Gram-negative bacilli
- Haemophilus influenzae
- Acinetobacter baumannii
Management
Shown below is an algorithm depicting the management of community acquired pneumonia according to the Infectious Diseases Society of America (IDSA) and Thoracic Society Consensus Guidelines on the Management of Community Acquired Pneumonia in Adults.[4][5]
Examine the patient: ❑ General examination:
❑ Respiratory examination:
❑ Look for specific signs
❑ Check for severity signs
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Order Labs: ❑ Order complete blood count (CBC) ❑ Check Blood urea nitrogen (BUN) ❑ Order a chest X-ray ❑ Perform sputum gram stain ❑ Sputum culture ❑ Blood culture ❑ If suspecting atypical pneumonia obtain:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Infiltrates on a chest X-ray 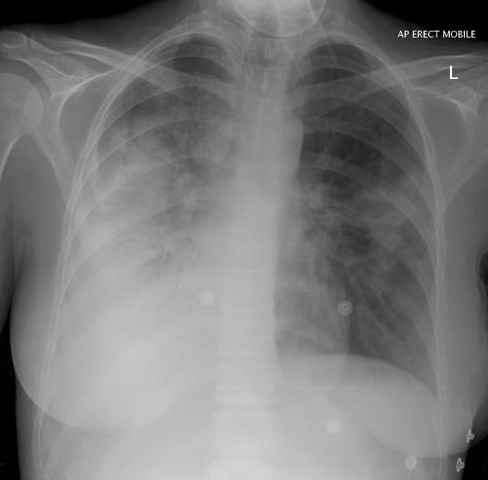 | ❑ No infiltrates on a chest X-ray | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Start oxygenation if needed
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Start empiric therapy based on the severity while awaiting culture results | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Outpatients With no recent antibiotic exposure and no comorbidities ❑ PSI score <70 = Risk Class I and II | Outpatients With recent antibiotic exposure and no comorbidities ❑ PSI score <70 = Risk Class I and II | Hospitalized patient not in the ICU ❑ PSI score > 71-90 = Risk Class III | Critically ill patients in the ICU ❑ PSI score 91 = Risk Class IV and V | ||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Azithromycin Oral: 500 mg on day 1 followed by 250 mg once daily on days 2-5 I.V.: 500 mg as a single dose OR ❑ Clarithromycin 250 mg every 12 hours for 7-14 days or 1000 mg once daily for 7 days OR ❑ Erythromycin 250-500 mg every 6-12 hours; maximum: 4 g daily OR ❑ Doxycycline Oral, I.V.: 100 mg twice daily | ❑ Levofloxacin 500 mg every 24 hours for 7-14 days or 750 mg every 24 hours for 5 days OR ❑ Moxifloxacin Oral, I.V.: 400 mg every 24 hours for 7-14 days OR ❑ Gemifloxacin Oral: 320 mg once daily for 5 or 7 days OR ❑ Amoxicillin Oral: 875 mg every 12 hours or 500 mg every 8 hours 3 times daily OR ❑ Amoxicillin-clavulanate 2 gm 2 times daily OR Other alternatives include ❑ Ceftriaxone I.V: 1 g once daily, 2 g daily for patients at risk OR ❑ Cefpodoxime Oral: 200 mg every 12 hours for 14 days OR ❑ Cefuroxime I.M., I.V.: 750 mg every 8 hours | ❑ Ceftriaxone 1g IV daily OR ❑ Cefotaxime 1g IV q8h PLUS ❑ Azithromycin Oral: 500 mg on day 1 followed by 250 mg once daily on days 2-5 I.V.: 500 mg as a single dose or Clarithromycin 250 mg every 12 hours for 7-14 days or 1000 mg once daily for 7 days OR ❑ Respiratory fluoroquinolone (Moxifloxacin Oral, I.V.: 400 mg every 24 hours for 7-14 days) PLUS Macrolide OR ❑ Doxycycline Oral, I.V.: 100 mg twice daily | ❑ Cefotaxime I.M., I.V.: 1 g every 12 hours OR ❑ Ceftriaxone I.V: 1 g once daily, 2 g daily for patients at risk OR ❑ Ampicillin-sulbactam I.V.: 1500-3000 mg every 6 hours PLUS ❑ Azithromycin Oral: 500 mg on day 1 followed by 250 mg once daily on days 2-5 OR ❑ Ciprofloxacin 500-750 mg twice daily for 7-14 days OR ❑ Levofloxacin 500 mg every 24 hours for 7-14 days or 750 mg every 24 hours for 5 day OR ❑ Moxifloxacin Oral, I.V.: 400 mg every 24 hours for 7-14 days OR ❑ Gemifloxacin Oral: 320 mg once daily for 5 or 7 days PLUS ❑ Aztreonam I.V.: 2 g every 6-8 hours; maximum: 8 g daily. For penicillin allergy | ||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ If culture results are available then treat accordingly ❑ Order a few diagnostic tests if culture results
❑ If no response to treatment then look for | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Pleural Effusion | ❑ Empyema | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Perform thoracocentesis and analyse ❑ pH ❑ Cell count ❑ Gram stain ❑ Bacterial culture ❑ Protein ❑ Lactate dehydrogenase | Drain the empyema | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
The PSI Algorithm
The PSI Algorithm is detailed below. An online, automated PSI calculator is available on the US AHRQ website.
| Step 1: Stratify to Risk Class I vs. Risk Classes II-V | |||
| Presence of: | |||
| Over 50 years of age | Yes/No | ||
| Altered mental status | Yes/No | ||
| Pulse ≥125/minute | Yes/No | ||
| Respiratory rate >30/minute | Yes/No | ||
| Systolic blood pressure ≥90 mm Hg | Yes/No | ||
| Temperature <35°C or ≥40°C | Yes/No | ||
| History of: | |||
| Neoplastic disease | Yes/No | ||
| Congestive heart failure | Yes/No | ||
| Cerebrovascular disease | Yes/No | ||
| Renal disease | Yes/No | ||
| Liver disease | Yes/No | ||
| If any "Yes", then proceed to Step 2 | |||
| If all "No" then assign to Risk Class I | |||
| Step 2: Stratify to Risk Class II vs III vs IV vs V | |||
| Demographics | Points Assigned | ||
| If Male | +Age (yr) | ||
| If Female | +Age (yr) - 10 | ||
| Nursing home resident | +10 | ||
| Comorbidity | |||
| Neoplastic disease | +30 | ||
| Liver disease | +20 | ||
| Congestive heart failure | +10 | ||
| Cerebrovascular disease | +10 | ||
| Renal disease | +10 | ||
| Physical Exam Findings | |||
| Altered mental status | +20 | ||
| Pulse ≥125/minute | +20 | ||
| Respiratory rate >30/minute | +20 | ||
| Systolic blood pressure ≥90 mm Hg | +15 | ||
| Temperature <35°C or ≥40°C | +10 | ||
| Lab and Radiolographic Findings | |||
| Arterial pH <7.35 | +30 | ||
| Blood urea nitrogen ≥30 mg/dl (9 mmol/liter) | +20 | ||
| Sodium <90 mmol/liter | +20 | ||
| Glucose ≥250 mg/dl (14 mmol/liter) | +10 | ||
| Hematocrit <30% | +10 | ||
| Partial pressure of arterial O2 <60mmHg | +10 | ||
| Pleural effusion | +10 | ||
| ∑ <70 = Risk Class II | |||
| ∑ 71-90 = Risk Class III | |||
| ∑ 91-130 = Risk Class IV | |||
| ∑ >130 = Risk Class V | |||
CURB-65
CURB-65 is a clinical prediction rule that has been validated for predicting mortality in community-acquired pneumonia[6] and infection of any site[7]. The CURB-65 is based on the earlier CURB score[8] and is recommended by the British Thoracic Society for the assessment of severity of pneumonia.[9]
The score is an acronym for each of the risk factors measured. Each risk factor scores one point, for a maximum score of 5:
- Confusion (defined as an AMT of 8 or less)
- Urea greater than 7 mmol/l (Blood Urea Nitrogen > 20)
- Respiratory rate of 30 breaths per minute or greater
- Blood pressure less than 90 systolic or diastolic blood pressure 60 or less
- Age 65 or older
Do's
- Obtain a sputum gram stain, sputum culture and blood cultures before initiating antibiotic therapy.
- Provide coverage for Streptococcus pneumoniae and atypical bacteria like (Mycoplasma, Chlamydophila, Legionella ).[5]
- Consider acute and convalescent serologic testing to identify atypical pathogens like C.pneumoniae, Q fever and Hantavirus.
- Perform aggressive fluid resuscitation, prompt antibiotic initiation, measure arterial blood gas in all patients who have borderline hypoxemia or lactate.[10]
- Treat co-existing illness like asthma and COPD with bronchodilators.
- Start empirical therapy with coverage for Pseudomonas aeruginosa and MRSA if patient is hospitalized for more than 2 days.[11]
- Give high priority to patients with elevated blood urea nitrogen (BUN), confusion and high respiratory rate.[12]
- First antibiotic dose should be administered within 6 hours of admission into the emergency room.[13]
- Shock is an exception where antibiotic should be started within an hour of hypotension. A decrease in 8% of survival rate for each hour of delay is noted.[14]
- Treat with antibiotics for atleast 5-7 days.
- Narrow down antibiotic therapy as soon as a specific microbiological etiology is identified.
- Chest X-ray should be performed and checked for signs of consolidation, cavitation or interstitial infiltrates.
- Use fibre-optic bronchoscopy in immunocompromised individuals to detect less common organisms, do a tissue biopsy and identify anatomic lesions if any.
Dont's
- Inadvertently use of antibiotic for patients without community-acquired pneumonia who require treatment within 4 hours may increase the risk of Clostridium difficile colitis.[15] Hence, use antibiotics judiciously.
- Don't discontinue antibiotics till the patient is afebrile for 48 to 72 hours and has signs of clinical improvement.
References
- ↑ Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM, Musher DM, Niederman MS, Torres A, Whitney CG (2007). "Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults". Clinical Infectious Diseases : an Official Publication of the Infectious Diseases Society of America. 44 Suppl 2: S27–72. doi:10.1086/511159. PMID 17278083. Unknown parameter
|month=ignored (help) - ↑ Wong, KK.; Fistek, M.; Watkins, RR. (2013). "Community-acquired pneumonia caused by Yersinia enterocolitica in an immunocompetent patient". J Med Microbiol. 62 (Pt 4): 650–1. doi:10.1099/jmm.0.053488-0. PMID 23242642. Unknown parameter
|month=ignored (help) - ↑ Oh, YJ.; Song, SH.; Baik, SH.; Lee, HH.; Han, IM.; Oh, DH. (2013). "A case of fulminant community-acquired Acinetobacter baumannii pneumonia in Korea". Korean J Intern Med. 28 (4): 486–90. doi:10.3904/kjim.2013.28.4.486. PMID 23864808. Unknown parameter
|month=ignored (help) - ↑ "http://cid.oxfordjournals.org/content/44/Supplement_2/S27.full.pdf+html". Retrieved 13 March 2014. External link in
|title=(help) - ↑ 5.0 5.1 "MMS: Error".
- ↑ Lim WS, van der Eerden MM, Laing R; et al. (2003). "Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study". Thorax. 58 (5): 377–82. PMID 12728155.
- ↑ Howell MD, Donnino MW, Talmor D, Clardy P, Ngo L, Shapiro NI (2007). "Performance of severity of illness scoring systems in emergency department patients with infection". Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 14 (8): 709–14. doi:10.1197/j.aem.2007.02.036. PMID 17576773.
- ↑ Lim WS, Macfarlane JT, Boswell TC; et al. (2001). "Study of community acquired pneumonia aetiology (SCAPA) in adults admitted to hospital: implications for management guidelines". Thorax. 56 (4): 296–301. PMID 11254821.
- ↑ "BTS Guidelines for the Management of Community Acquired Pneumonia in Adults". Thorax. 56 Suppl 4: IV1–64. 2001. PMID 11713364.
- ↑ Rivers, E.; Nguyen, B.; Havstad, S.; Ressler, J.; Muzzin, A.; Knoblich, B.; Peterson, E.; Tomlanovich, M. (2001). "Early goal-directed therapy in the treatment of severe sepsis and septic shock". N Engl J Med. 345 (19): 1368–77. doi:10.1056/NEJMoa010307. PMID 11794169. Unknown parameter
|month=ignored (help) - ↑ "Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia". Am J Respir Crit Care Med. 171 (4): 388–416. 2005. doi:10.1164/rccm.200405-644ST. PMID 15699079. Unknown parameter
|month=ignored (help) - ↑ Lim, HF.; Phua, J.; Mukhopadhyay, A.; Ngerng, WJ.; Chew, MY.; Sim, TB.; Kuan, WS.; Mahadevan, M.; Lim, TK. (2013). "IDSA/ATS minor criteria aided pre-ICU resuscitation in severe community-acquired pneumonia". Eur Respir J. doi:10.1183/09031936.00081713. PMID 24176994. Unknown parameter
|month=ignored (help) - ↑ Wilson, KC.; Schünemann, HJ. (2011). "An appraisal of the evidence underlying performance measures for community-acquired pneumonia". Am J Respir Crit Care Med. 183 (11): 1454–62. doi:10.1164/rccm.201009-1451PP. PMID 21239689. Unknown parameter
|month=ignored (help) - ↑ Kumar, A.; Roberts, D.; Wood, KE.; Light, B.; Parrillo, JE.; Sharma, S.; Suppes, R.; Feinstein, D.; Zanotti, S. (2006). "Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock". Crit Care Med. 34 (6): 1589–96. doi:10.1097/01.CCM.0000217961.75225.E9. PMID 16625125. Unknown parameter
|month=ignored (help) - ↑ Meehan, TP.; Fine, MJ.; Krumholz, HM.; Scinto, JD.; Galusha, DH.; Mockalis, JT.; Weber, GF.; Petrillo, MK.; Houck, PM. (1997). "Quality of care, process, and outcomes in elderly patients with pneumonia". JAMA. 278 (23): 2080–4. PMID 9403422. Unknown parameter
|month=ignored (help)