Addison's disease
| Addison's disease | |
| ICD-10 | E27.1-E27.2 |
|---|---|
| ICD-9 | 255.4 |
| DiseasesDB | 222 |
| MedlinePlus | 000378 |
| eMedicine | med/42 |
| MeSH | D000224 |
|
WikiDoc Resources for Addison's disease |
|
Articles |
|---|
|
Most recent articles on Addison's disease Most cited articles on Addison's disease |
|
Media |
|
Powerpoint slides on Addison's disease |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Addison's disease |
|
Clinical Trials |
|
Ongoing Trials on Addison's disease at Clinical Trials.gov Trial results on Addison's disease Clinical Trials on Addison's disease at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Addison's disease NICE Guidance on Addison's disease
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Addison's disease Discussion groups on Addison's disease Patient Handouts on Addison's disease Directions to Hospitals Treating Addison's disease Risk calculators and risk factors for Addison's disease
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Addison's disease |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Addison's disease (also known as chronic adrenal insufficiency, hypocortisolism or hypocorticism) is a rare endocrine disorder in which the adrenal gland produces insufficient amounts of steroid hormones (glucocorticoids and often mineralocorticoids). It may develop in children as well as adults, and may occur as the result of a large number of underlying causes.
The condition is named after Dr Thomas Addison, the British physician who first described the condition in his 1855 On the Constitutional and Local Effects of Disease of the Suprarenal Capsules.[1] The adjective "Addisonian" is used for features of the condition, as well as patients with Addison's disease.[2]
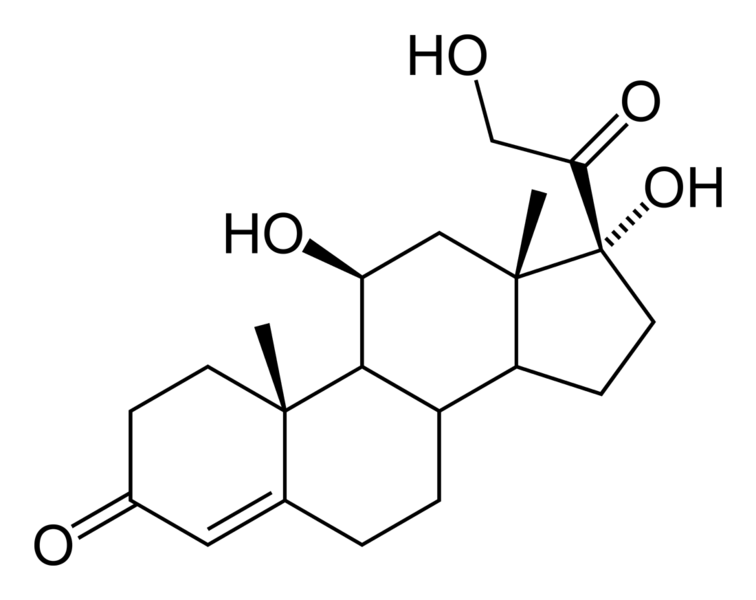
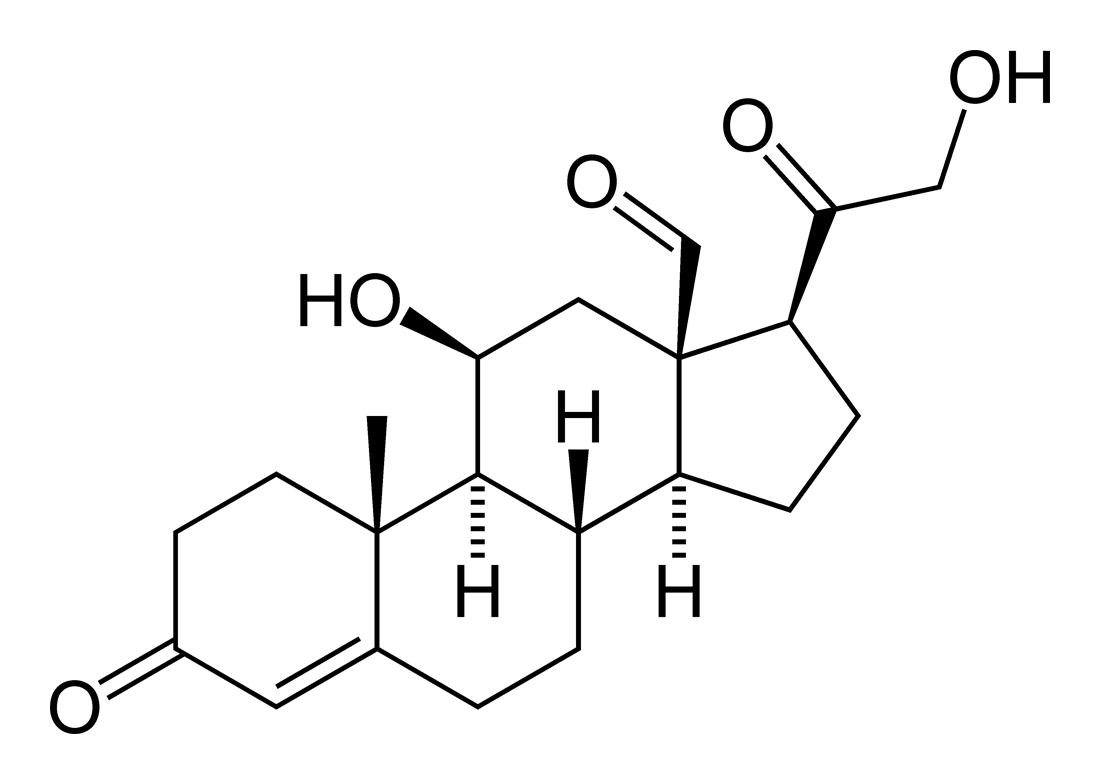
The condition is generally diagnosed with blood tests, medical imaging and additional investigations.[2] Treatment is with replacement of the hormones (oral hydrocortisone and fludrocortisone). If the disease is caused by an underlying problem, this is addressed. Regular follow-up and monitoring for other health problems is necessary.[2]
Causes
Causes of adrenal insufficiency can be grouped by the way in which they cause the adrenals to produce insufficient cortisol. These are adrenal dysgenesis (the gland has not formed adequately during development), impaired steroidogenesis (the gland is present but is biochemically unable to produce cortisol) or adrenal destruction (disease processes leading to the gland being damaged).[2]
- Adrenal dysgenesis
All causes in this category are genetic, and generally very rare. These include mutations to the SF1 transcription factor, congenital adrenal hypoplasia (AHC) due to DAX-1 gene mutations and mutations to the ACTH receptor gene (or related genes, such as in the Triple A or Allgrove syndrome). DAX-1 mutations may cluster in a syndrome with glycerol kinase deficiency with a number of other symptoms when DAX-1 is deleted together with a number of other genes.[2]
- Impaired steroidogenesis
To form cortisol, the adrenal gland requires cholesterol, which is then converted biochemically into steroid hormones. Interruptions in the delivery of cholesterol include Smith-Lemli-Opitz syndrome and abetalipoproteinemia. Of the synthesis problems, congenital adrenal hyperplasia is the most common (in various forms: 21-hydroxylase, 17α-hydroxylase, 11β-hydroxylase and 3β-hydroxysteroid dehydrogenase), lipod CAH due to deficiency of StAR and mitochondrial DNA mutations.[2]
- Adrenal destruction
Autoimmune destruction of the adrenal cortex (often due to antibodies against the enzyme 21-Hydroxylase) is a common cause of Addison's in teenagers and adults. This may be isolated or in the context of autoimmune polyendocrine syndrome (APS type 1 or 2). Adrenal destruction is also a feature of adrenoleukodystrophy (ALD), and when the adrenal glands are involved in metastasis (seeding of cancer cells from elsewhere in the body), hemorrhage (e.g. in Waterhouse-Friderichsen syndrome or antiphospholipid syndrome), particular infections (tuberculosis, histoplasmosis, coccidioidomycosis), deposition of abnormal protein in amyloidosis. Some medications interfere with steroid synthesis enzymes (e.g. ketoconazole), while others accelerate the normal breakdown of hormones by the liver (e.g. rifampicin, phenytoin).[2]
Complete differential diagnosis of causes of Addison's disease [3]
Primary Adrenocoritcal Insufficiency (Addison's disease)
- Autoimmune/idiopathic
- Congenital
- Congenital adrenal hyperplasia
- Familial glucocorticoid deficiency
- Glucocorticoid deficiency 1
- Adrenal leukodystrophy
- Adrenal aplasia/hypoplasia
- Iatrogenic
- Radiation (therapy)
- Bilateral adrenalectomy
- Fungal
- Cryptococcosis
- Blastomycosis
- Syphilis
- Coccidiomycosis
- Tuberculosis (20% of all Addison's)
- Hemorrhage, infarction
- Trauma
- Surgery
- Sepsis
- Embolus
- Anticoagulation
- Arteritis
- Hypotension
- Neonatal
- Thrombosis
- Coagulopathy
- Infections
- Neoplasm
- Uremia
- Coma
- Infiltrative
- Volume/electrolyte disorders
- Drugs
Secondary (pituitary) or Tertiary (hypothalamic) Adrenocortical Insufficiency
- Drug withdrawal
- After surgery of cortisol-secreting tumor
Signs and symptoms
Symptoms
The symptoms of Addison's disease develop insidiously, and it may take some time to be recognized. The most common symptoms are fatigue, muscle weakness, weight loss, vomiting, diarrhea, headache, sweating, changes in mood and personality and joint and muscle pains. Some have marked cravings for salty foods due to the urinary losses of sodium.[2]
Clinical signs
On examination, the following may be noticed:[2]
- Low blood pressure that falls further when standing (orthostatic hypotension)
- Darkening (hyperpigmentation) of the skin, including areas not exposed to the sun; characteristic sites are skin creases (e.g. of the hands), nipples, and the inside of the cheek (buccal mucosa), also old scars may darken.
- Signs of conditions that often occur together with Addison's: goiter and vitiligo
Addisonian crisis
An "Addisonian crisis" or "adrenal crisis" is a constellation of symptoms that indicate severe adrenal insufficiency. This may be the result of either previously undiagnosed Addison's disease, a disease process suddenly affecting adrenal function (such as adrenal hemorrhage), or an intercurrent problem (e.g. infection, trauma) in the setting of known Addison's disease. Additionally, this situation may develop in those on long-term oral glucocorticoids who have suddenly ceased taking their medication. It is also a concern in the setting of myxedema coma; thyroxine given in that setting without glucocorticoids may precipitate a crisis.
Untreated, an Addisonian crisis can be fatal. It is a medical emergency, usually requiring hospitalization. Characteristic symptoms are:[4]
- Sudden penetrating pain in the legs, lower back or abdomen
- Severe vomiting and diarrhea, resulting in dehydration
- Low blood pressure
- Loss of consciousness/Syncope
- Hypoglycemia
- Confusion, psychosis
- Convulsions
Diagnosis
Suggestive features
Routine investigations may show:[2]
- Hypoglycemia, low blood sugar (worse in children)
- Hyponatraemia (low blood sodium levels)
- Hyperkalemia (raised blood potassium levels), due to loss of production of the hormone aldosterone
- Eosinophilia and lymphocytosis (increased number of eosinophils or lymphocytes, two types of white blood cells)
Testing
In suspected cases of Addison's disease, one needs to demonstrate that adrenal hormone levels are low even after appropriate stimulation with synthetic pituitary hormone tetracosactide. Two tests are performed, the short and the long test.
The short test compares blood cortisol levels before and after 250 micrograms of tetracosactide (IM/IV) is given. If, one hour later, plasma cortisol exceeds 170 nmol/L and has risen by at least 330 nmol/L to at least 690 nmol/L, adrenal failure is excluded. If the short test is abnormal, the long test is used to differentiate between primary adrenal failure and secondary adrenocortical failure.
The long test uses 1 mg tetracosactide (IM). Blood is taken 1, 4, 8, and 24 hours later. Normal plasma cortisol level should reach 1000 nmol/L by 4 hours. In primary Addison's disease, the cortisol level is reduced at all stages whereas in secondary corticoadrenal insufficiency, a delayed but normal response is seen.
Other tests that may be performed to distinguish between various causes of hypoadrenalism are renin and adrenocorticotropic hormone levels, as well as medical imaging - usually in the form of ultrasound, computed tomography or magnetic resonance imaging (MRI).
Treatment
Maintenance treatment
Treatment for Addison's disease involves replacing the missing cortisol (usually in the form of hydrocortisone tablets) in a dosing regimen that mimics the physiological concentrations of cortisol. Treatment must usually be continued for life. In addition, many patients require fludrocortisone as replacement for the missing aldosterone. Caution must be exercised when the person with Addison's disease becomes unwell, has surgery or becomes pregnant. Medication may need to be increased during times of stress, infection, or injury.
Addisonian crisis
Treatment for an acute attack, an Addisonian crisis, usually involves intravenous (into blood veins) injections of:
- Cortisone (cortisol)
- Saline solution (basically a salt water, same clear IV bag as used to treat dehydration)
- Glucose
Surgery
Surgeries may require significant adjustments to medication regimens prior to, during, and following any surgical procedure. The best preparation for any surgery, regardless of how minor or routine it may normally be, is to speak to one's primary physician about the procedure and medication implications well in advance of the surgery.
Pregnancy
Many women with Addison's have given birth successfully and without complication, both through natural labor and through cesarean delivery. Both of these methods will require different preventative measures relating to Addison's medications and dosages. As is always the case, thorough communication with one's primary physician is the best course of action. Occasionally, oral intake of medications will cause debilitating nausea and vomiting, and thus the woman may be switched to injected medications until delivery. [5] Addison's treatment courses by the mother are generally considered safe for baby during pregnancy.
Epidemiology
The frequency rate of Addison's disease in the human population is sometimes estimated at roughly 1 in 100,000.[6] Some research and information sites put the number closer to 40-60 cases per 1 million population. (1/25,000-1/16,600)[7] (Determining accurate numbers for Addison's is problematic at best and some incidence figures are thought to be underestimates.[8]) Addison's can afflict persons of any age, gender, or ethnicity, but typically presents in adults between 30 and 50 years of age. Women are slightly more likely to develop Addison's according to some studies. Research has shown no significant predispositions based on ethnicity.[7]
Prognosis
While treatment solutions for Addison's disease are far from precise, overall long-term prognosis is typically good. Because of individual physiological differences, each person with Addison's must work closely with their physician to adjust their medication dosage and schedule to find the most effective routine. Once this is accomplished (and occasional adjustments must be made from time to time, especially during periods of travel, stress, or other medical conditions), symptomology is usually greatly reduced or occasionally eliminated so long as the person continues their dosage schedule.
Canine hypoadrenocorticism
The condition is relatively rare, but has been diagnosed in all breeds of dogs. In general, it is underdiagnosed, and one has to have a clinical suspicion of it as an underlying disorder for many presenting complaints. Females are overrepresented, and the disease often appears in middle age (4-7 years), although any age or gender may be affected.
Hypoadrenocorticism is treated with prednisolone and/or fludrocortisone (Florinef (r)) or a monthly injection called Percorten V (desoxycorticosterone pivlate (DOCP)). Routine blood work is necessary periodically to assess therapy.
Most of the medications used in the therapy of hypoadrenocorticism cause excessive thirst and urination. It is absolutely vital to provide fresh drinking water for the canine sufferer.
If the owner knows about an upcoming stressful situation (shows, traveling etc.), patients generally need an increased dose of prednisone to help deal with the added stress. Avoidance of stress is important for dogs with hypoadrenocorticism.
Famous Addisonians
- President John F. Kennedy was one of the best-known Addison's disease sufferers.
- Popular singer Helen Reddy.[9]
- Scientist Eugene Merle Shoemaker Co-discoverer of the Comet Shoemaker-Levy 9.[10]
- French Carmelite nun and religious writer Blessed Elizabeth of the Trinity [11]
- Some have suggested that Jane Austen was an avant la lettre case, but others have disputed this.[12]
- According to Dr. Carl Abbott, a Canadian medical researcher, Charles Dickens may also have been afflicted.[13]
- Osama bin-Laden - may be an Addisonian: Lawrence Wright (The Looming Tower, 2006, p. 139) notes that bin-Laden manifests all the key symptoms: "low blood pressure, weight loss, muscle fatigue, stomach irritability, sharp back pains, dehydration, and an abnormal craving for salt". Bin-Laden is known to have been consuming large amounts of the drug Arcalion to treat his symptoms.
See also
References
- ↑ Thomas Addison. On The Constitutional And Local Effects Of Disease Of The Supra-Renal Capsules (HTML reprint). London: Samuel Highley.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Ten S, New M, Maclaren N (2001). "Clinical review 130: Addison's disease 2001". J. Clin. Endocrinol. Metab. 86 (7): 2909–22. PMID 11443143.
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:14-15
- ↑ Addison's Disease National Endocrine and Metabolic Diseases Information Service. Retrieved on 26 October, 2007.
- ↑ "addison's disease".
- ↑ [http://www.medicinenet.com/addison_disease/article.htm "Addison Disease � Health information regarding this hormonal (endocrine) disorder on MedicineNet.com"]. replacement character in
|title=at position 17 (help) - ↑ 7.0 7.1 "eMedicine - Addison Disease : Article by Sylvester Odeke".
- ↑ "medhelp".
- ↑ "The Australian Addison's Disease Association".
- ↑ "Eugene Shoemaker (1928-1997)".
- ↑ "catholic-forum.com".
- ↑ Upfal A (2005). "Jane Austen's lifelong health problems and final illness: New evidence points to a fatal Hodgkin's disease and excludes the widely accepted Addison's". J Med Ethics Med Humanities. 31: 3–11.
- ↑ L. Williams; et al. (1991). "The Nineteenth Century: Victorian Period". The Year's Work in English Studies. Oxford University Press. 72 (1): 314–360. doi:10.1093/ywes/72.1.314.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (2004). "NIH Publication No. 04–3054: Addison's disease". Endocrine and Metabolic Diseases Information Service. National Institute for Health. Unknown parameter
|month=ignored (help)
External links
- Overview of Addison's Disease from the Mayo Clinic
- Addison's Disease Research Today - monthly online journal summarizing recent primary literature on Addison's disease
- National Adrenal Diseases Foundation
- Addison's information from MedicineNet
- "Addison's Disease: The Facts You Need to Know (MedHelp.org)
- The Addison & Cushing International Federation (ACIF)
- Addison's disease info from SeekWellness.com
- Information about Addison's disease in canines (dogs)
- Antibodies to adrenal gland
- Immunofluorescence images
- Endocrine and Metabolic Diseases Information Service
Support groups
- Addison's Disease Self Help Group (ADSHG) - UK support group
- Australian Addison's Disease Association - Australian support and information group
- Nederlandse Vereniging voor Addison en Cushing Patiënten - Dutch support and information group with information and documentation in English
- Addresses of patient organisations and support groups around the world
bg:Адисонова болест cs:Addisonova choroba da:Addisons sygdom de:Nebennierenrindeninsuffizienz it:Morbo di Addison he:מחלת אדיסון ms:Penyakit Addison nl:Ziekte van Addison sk:Addisonova choroba fi:Addisonin tauti sv:Addisons sjukdom Template:SIB