Sandbox:Cherry
Lab findings
Diagnosis of Cirrhosis
Laboratory findings —
Laboratory abnormalities may be the first indication of cirrhosis.
Common abnormalities include:[1][2]
- Increased serum bilirubin levels [3]
- Abnormal aminotransferase levels [4][5][6][7][8][9][10][11][12][13]
- Elevated alkaline phosphatase / gamma-glutamyl transpeptidase [14][5][15]
- Prolonged prothrombin time
- Elevated international normalized ratio (INR)
- Hyponatremia
- Thrombocytopenia
Liver function tests
- Aminotransferases :[16][17]
- Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are usually moderately elevated
- AST is more often elevated than ALT
- Levels may be normal
- Alkaline phosphatase: [18]
- Alkaline phosphatase is usually elevated
- High levels may be seen in patients with underlying cholestatic liver disease such as:
- Primary sclerosing cholangitis
- Primary biliary cirrhosis
- Higher in CLD due to alcohol use:
- Alcohol causes GGT release from hepatocytes
- Alcohol induces microsomal GGT in liver
- Bilirubin: Bilirubin levels may be normal or raised
- Albumin: Albumin levels reflect synthetic function of the liver
- Serum albumin levels helps grade the severity of cirrhosis
- Hypoalbuminemia is non specific for liver disease: heart failure, nephrotic syndrome, protein losing enteropathy, or malnutrition.
- Prothrombin time – Prothrombin time reflects the degree of hepatic synthetic function.
- Worsening coagulopathy correlates with the severity of hepatic dysfunction.
Serum chemistries :
- Hyponatremia is common in patients with cirrhosis and ascites and is related to an inability to excrete free water. [21]
- Due to ADH elevation
- Reflects poor prognosis
- Progressive rise in serum creatinine: hepatorenal syndrome
Hematologic abnormalities: [22]
- Thrombocytopenia: most common
- Mechanism of thrombocytopenia:
- caused by portal hypertension with congestive splenomegaly: sequesters circulating platelets
- decreased thrombopoietin levels
- Leukopenia/neutropenia: due to hypersplenism with splenic margination.
- Anemia
- Mechanism of anemia:
- Acute and chronic gastrointestinal blood loss
- Folate deficiency
- Direct toxicity due to alcohol
- Hypersplenism
- Bone marrow suppression ( hepatitis-associated aplastic anemia)
- Anemia of chronic disease (inflammation)
- Hemolysis
- Other abnormalities — Globulins tend to be increased [23]
- Disseminated intravascular coagulation
- Fibrinolysis
- Vitamin K deficiency
- Dysfibrinogenemia
- Insulin resistance: nonalcoholic fatty liver disease
- Diabetes: seen in patients with hemochromatosis [24][25]
Radiologic findings:
- Radiologic studies include:[2]
- Abdominal ultrasound
- Computed tomography scan
- Magnetic resonance imaging
- Findings may include:[26][26][27][28][29][30]
- A liver that appears shrunken, irregular, and nodular.
- Evidence of Portal HTN:
- varices
- Ascites
DIAGNOSIS —
- Abdominal imaging (typically ultrasound) helps:
- Evaluate the liver parenchyma
- Detects extrahepatic manifestations of cirrhosis
Laboratory tests:
- AST to platelet ratio index
- FibroTest/FibroSure
Imaging studies:
- Findings on abdominal imaging are viewed in light of other signs of cirrhosis, such as physical examination or laboratory test findings.
- In addition to evaluating the liver, abdominal imaging may reveal:
- Hepatocellular carcinoma
- Extrahepatic findings suggestive of cirrhosis:
- Ascites
- Varices
- Splenomegaly
- Hepatic or portal vein thrombosis
- Imaging may indicate etiology of cirrhosis:
CT
- Computed tomography (CT) scanning complements ultrasound imaging.
- Classical appearances in some diseases:
- Haemochromatosis: where the excess iron deposition causes a dramatic increase in hepatic density.
- A hypertrophied caudate lobe discovered on computed tomographic (CT) scanning, for example, suggests Budd-Chiari syndrome.
MRI[31][32][33][34][35][36][34][37]
- Magnetic resonance imaging (MRI):
- determines the nature of focal lesions such as hepatic metastases
- nodular regeneration
- Decreased signal intensity on magnetic resonance imaging may indicate iron overload from hereditary hemochromatosis.
Ultrasonography: routinely used during the evaluation of cirrhosis
- First-line investigation of choice.
- The first radiologic study obtained due to easy availability.
- Provides information about :
- appearance of the liver
- blood flow within the portal circulation
- less expensive than other imaging modalities
- No exposure to intravenous contrast or radiation
- Noninvasive
- cheap
- safe
- well tolerated
- widely available
- Ultrasound, particularly with colour Doppler imaging :
- measures changes in blood flow in the presence of portal hypertension
- excludes biliary obstruction in patients who present with jaundice
- Early signs of cirrhosis in B-ultrasonography include:
- inhomogeneity of the hepatic tissue
- Irregularity of the hepatic surface
- enlargement of the caudate lobe
- Splenomegaly due to portal HTN
- The diagnostic evaluation of cirrhosis with ultrasonography is based on the direct relation between the extent of fibrosis and the ultrasonographically determined degree of liver stiffness.
- ultrasonography can rule cirrhosis in or out in over 90% of cases , its findings are less than 100% specific because of occasional in -correct measurements and false-positive findings
- Findings:
- Advanced cirrhosis: liver may appear small and nodular
- Surface nodularity and increased echogenicity with irregular appearing areas are consistent with cirrhosis
- Usually atrophy of the right lobe and hypertrophy of the caudate or left lobes.
- Ultrasonography may also be used as a screening test for hepatocellular carcinoma :nodules on ultrasonography warrants further evaluation
- Findings of portal hypertension:
- increased diameter of the portal vein
- presence of collateral veins
- decreased flow within the portal circulation on Doppler imaging
- Ultrasonography is also useful for detecting splenomegaly, ascites, and portal vein thrombosis.
Computed tomography – not routinely used in the diagnosis of cirrhosis
- It provides similar information to ultrasonography, but at the expense of radiation and contrast exposure.
- CT findings:
- Hepatic nodularity
- Atrophy of the right lobe
- Hypertrophy of the caudate or left lobes
- Ascites
- Varices
- CT portal phase imaging:
- Patency of the portal vein can be demonstrated
Magnetic resonance imaging:
- The role of magnetic resonance imaging (MRI) in the diagnosis of cirrhosis is unclear.
- Use is limited by expense
- Poor tolerance of the examination
- Ability to obtain information provided by MRI through other means
- reveal iron overload and provide an estimate of the hepatic iron concentration
- Magnetic resonance angiography (MRA) is more sensitive than ultrasonography for diagnosing complications of cirrhosis:
- portal vein thrombosis
- CT portal phase imaging, MRA can determine the volume and direction of blood flow in the portal vein.
Elastography: [38]
- Increasing scarring of the liver is associated with increasing "stiffness" of the tissue.
Nuclear studies:
- Radionuclide testing can be useful in suggesting the diagnosis of cirrhosis:[39]
- 99mTc sulfur colloid is normally taken up by cells of the reticuloendothelial system
- Cirrhosis: heterogeneity in the uptake of 99mTc sulfur colloid by the liver and increased uptake by the spleen and bone marrow
Endoscopic retrograde cholangiopancreatography
- diagnosis of sclerosing cholangitis
Liver biopsy: [40]
- Cirrhosis is primarily a histological diagnosis.
- Percutaneous liver biopsy remains the cornerstone of diagnosis.
- quick and simple to perform in a cooperative patient with a normal INR and platelet count.
- The gold standard for diagnosing cirrhosis is:
- Examination of an explanted liver, either at autopsy or following liver transplantation, because the architecture of the entire liver can be appreciated.
- Sample of the liver is obtained by:
- Percutaneous
- Transjugular
- Laparoscopic radiographically-guided fine-needle approach.
- Liver biopsy is not necessary if the clinical, laboratory, and radiologic data strongly suggest the presence of cirrhosis and if the results would not alter the patient's management.
- Patient with a history of heavy alcohol use who has ascites, severe coagulopathy, and a shrunken, nodular-appearing liver on ultrasonography.
- Liver biopsy may be suggestive of etiology:
- Metabolic causes of cirrhosis include:
- Hereditary hemochromatosis
- Nonalcoholic steatohepatitis
- Wilson disease
- Alpha-1 antitrypsin deficiency
- Risks:
- haemorrhage
- biliary peritonitis
- haematoma
- perforation of other viscera
- mortality rates of between 0.01% and 0.1%
- Percutaneous biopsy of focal lesions may be performed in combination with either ultrasound or CT imaging.
- Prerequisites:
- normal INR and platelet count.
- May be performed in combination with either ultrasound or CT.
- Patients with moderate coagulopathy:
- Plugged liver biopsy : injection of gelatin sponges or metal coils down the tract after biopsy
- Laparoscopic liver biopsy performed on a sedated patient with moderate coagulopathy
- Advantage: allows direct visualisation of the liver
- Patients with severe clotting disorders:
- Transjugular liver biopsy :
- risk of intraperitoneal bleed is less
- Disadvantages:
- biopsies are small: multiple biopsies required
- taken 'blindly'
rough
Diagnosis of Cirrhosis
Laboratory findings —
Laboratory abnormalities may be the first indication of cirrhosis.
Common abnormalities include:
Increased serum bilirubin levels
Abnormal aminotransferase levels
Elevated alkaline phosphatase / gamma-glutamyl transpeptidase
Prolonged prothrombin time
Elevated international normalized ratio (INR)
Hyponatremia
Thrombocytopenia
Liver function tests . .
●Aminotransferases –
Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are usually moderately elevated
AST is more often elevated than ALT
Levels may be normal
●Alkaline phosphatase –
Alkaline phosphatase is usually elevated
High levels may be seen in patients with underlying cholestatic liver disease such as
primary sclerosing cholangitis
primary biliary cirrhosis
●Gamma-glutamyl transpeptidase –
Non specific
Correlates with ALP levels
Higher in CLD due to alcohol use:
Alcohol causes GGT release from hepatocytes
Alcohol induces microsomal GGT in liver
●Bilirubin – Bilirubin levels may be normal or raised
●Albumin – Albumin levels reflect synthetic function of the liver
Serum albumin levels helps grade the severity of cirrhosis
Hypoalbuminemia is non specific for liver disease: heart failure, nephrotic syndrome, protein losing enteropathy, or malnutrition.
●Prothrombin time – Prothrombin time reflects the degree of hepatic synthetic function.
Worsening coagulopathy correlates with the severity of hepatic dysfunction.
Serum chemistries —
Hyponatremia is common in patients with cirrhosis and ascites and is related to an inability to excrete free water.
Due to ADH elevation
Reflects poor prognosis
progressive rise in serum creatinine: hepatorenal syndrome
Hematologic abnormalities —
Thrombocytopenia:most common
Mechanism of thrombocytopenia:
caused by portal hypertension with congestive splenomegaly: sequesters circulating platelets
Decreased thrombopoietin levels
Leukopenia/neutropenia: due to hypersplenism with splenic margination.
Anemia
Mechanism of anemia:
Acute and chronic gastrointestinal blood loss
Folate deficiency
Direct toxicity due to alcohol
Hypersplenism
Bone marrow suppression ( hepatitis-associated aplastic anemia)
Anemia of chronic disease (inflammation)
Hemolysis
Other abnormalities — Globulins tend to be increased
Disseminated intravascular coagulation
Fibrinolysis
Vitamin K deficiency
Dysfibrinogenemia
Insulin resistance: nonalcoholic fatty liver disease
Diabetes: seen in patients with hemochromatosis
Radiologic findings — Radiologic studies include:
Abdominal ultrasound
Computed tomography scan
Magnetic resonance imaging
Findings may include:
A liver that appears shrunken, irregular, and nodular.
Evidence of Portal HTN:
varices
Ascites
DIAGNOSIS —
Abdominal imaging (typically ultrasound) helps:
Evaluate the liver parenchyma
Detects extrahepatic manifestations of cirrhosis
Laboratory tests — AST to platelet ratio index
FibroTest/FibroSure
Imaging studies — Findings on abdominal imaging are viewed in light of other signs of cirrhosis, such as physical examination or laboratory test findings.
In addition to evaluating the liver, abdominal imaging may reveal:
Hepatocellular carcinoma
Extrahepatic findings suggestive of cirrhosis:
ascites,
varices,
splenomegaly,
hepatic or portal vein thrombosis.
Diagnosis
Diagnosis
-USG: first line investigation of choice
Ultrasound with colour Doppler imaging measures changes in blood flow due to portal hypertension
excludes biliary obstruction in jaundiced patients
safe
cheap
Noninvasive
Early signs of cirrhosis in B-ultrasonography include:
inhomogeneity of the hepatic tissue
Irregularity of the hepatic surface
enlargement of the caudate lobe
Splenomegaly due to portal HTN
The diagnostic evaluation of cirrhosis with ultrasonography is based on the direct relation between the extent of fibrosis and the ultrasonographically determined degree of liver stiffness.
ultrasonography can rule cirrhosis in or out in over 90% of cases , its findings are less than 100% specific because of occasional in -correct measurements and false-positive findings
-Computed tomography (CT) scanning :
Classical appearances in some diseases, eg, haemochromatosis: Heaptic density increases due to excess iron deposition
-Magnetic resonance imaging (MRI)
Helps differentiaiting focal lesions based on their nature:
hepatic metastases
nodular regeneration
-endoscopic retrograde cholangiopancreatography: in diagnosis of sclerosing cholangitis
-Liver biopsy
Cirrhosis is primarily a histological diagnosis
-Prerequisites:
normal INR and platelet count.
-Risks
Haemorrhage
biliary peritonitis
haematoma
perforation of other viscera
mortality rates of between 0.01% and 0.1%
May be performed in combination with either ultrasound or CT.
-Patients with moderate coagulopathy:
Plugged liver biopsy : injection of gelatin sponges or metal
coils down the tract after biopsy.
Laparoscopic liver biopsy performed on a sedated patient with moderate coagulopathy
Advantage: allows direct visualisation of the liver
-patients with severe clotting disorders: Transjugular liver biopsy :
risk of intraperitoneal bleed is less
Disadvantages:
biopsies are small: multiple biopsies required
taken 'blindly'
Findings in liver biopsy
Fibrous septa between the portal fields
Nodules- micronodular, macronodular
In advanced liver disease approaching the stage of cirrhosis:
thrombocytopenia
Impaired hepatic biosynthesis
Low concentration of albumin
Low concentration of cholinesterase
elevation of the international normalized ratio [INR])
impairment of the detoxifying function of the liver : e.g., elevated bilirubin concentration
transaminase levels are generally in the normal range or only mildly elevated.
Ancillary studies include:
Upper abdominal ultrasonography
Gastroscopy
Esophagogastroduo -denoscopy (EGD) : used to demonstrate eso -phageal varices
Assessment of bleeding
Performed in all cases of cirrhosis
Liver biopsy is contraindicated, if the diagnosis of cirrhosis has been clearly established
from the clinical findings and imaging:
evidence of decompensation, with ascites
Labs indicating impaired hepatic biosynthesis
Liver biopsy is indicated :
etiology of liver disease is unclear
stage cannot be determined: length of punch cylinders used for liver biopsy should be atleast 15 mm long, and at least 10 portal fields should be examined per sectional level
diagnosis in doubt
if the biopsy is expected to yield information about the cause of cirrhosis that will affect the treatment choice
Noninvasive diagnostic evaluation of cirrhosis
Laboratory-based methods:
Routine liver function tests [43][44][45][46][47]
Hyaluronic acid concentration
AST-to-platelet ratio index: (APRI) is easily calculated as the quotient of the AST
(GOT)
Platelet count: screening index for advanced fibrosis and cirrhosis
Transient elastography and the acoustic radiation force impulse (ARFI) technique are now well-established methods for the staging of fibrosis in various liver diseases [48] -USG: first line investigation of choice
Ultrasound with colour Doppler imaging measures changes in blood flow due to portal hypertension
excludes biliary obstruction in jaundiced patients safe cheap Noninvasive
Early signs of cirrhosis in B-ultrasonography include:
inhomogeneity of the hepatic tissue Irregularity of the hepatic surface enlargement of the caudate lobe Splenomegaly due to portal HTN
-Computed tomography (CT) scanning : Classical appearances in some diseases, eg, haemochromatosis: Heaptic density increases due to excess iron deposition
-Magnetic resonance imaging (MRI) Helps differentiaiting focal lesions based on their nature: hepatic metastases nodular regeneration
-endoscopic retrograde cholangiopancreatography: in diagnosis of sclerosing cholangitis.
-Liver biopsy Cirrhosis is primarily a histological diagnosis.
-Prerequisites:
normal INR and platelet count.
-Risks Haemorrhage
biliary peritonitis
haematoma
perforation of other viscera
mortality rates of between 0.01% and 0.1%
May be performed in combination with either ultrasound or CT.
-Patients with moderate coagulopathy: Plugged liver biopsy : injection of gelatin sponges or metal coils down the tract after biopsy.
Laparoscopic liver biopsy performed on a sedated patient with moderate coagulopathy Advantage: allows direct visualisation of the liver
-patients with severe clotting disorders: Transjugular liver biopsy :
risk of intraperitoneal bleed is less
Disadvantages: biopsies are small: multiple biopsies required taken 'blindly'
Findings in liver biopsy Fibrous septa between the portal fields Nodules- micronodular, macronodular
In advanced liver disease approaching the stage of cirrhosis:
thrombocytopenia
Impaired hepatic biosynthesis
Low concentration of albumin
Low concentration of cholinesterase
elevation of the international normalized ratio [INR])
impairment of the detoxifying function of the liver : e.g., elevated bilirubin concentration transaminase levels are generally in the normal range or only mildly elevated.
Findings in liver biopsy
Fibrous septa between the portal fields
Nodules- micronodular, macronodular
In advanced liver disease approaching the stage of cirrhosis:
thrombocytopenia
Impaired hepatic biosynthesis
Low concentration of albumin
Low concentration of cholinesterase
Elevation of the international normalized ratio [INR])
Impairment of the detoxifying function of the liver : e.g., elevated bilirubin concentration
transaminase levels are generally in the normal range or only mildly elevated.
Ancillary studies include:
Upper abdominal ultrasonography
Gastroscopy
Esophagogastroduo -denoscopy (EGD) : used to demonstrate eso -phageal varices
Assessment of bleeding
Performed in all cases of cirrhosis
Liver biopsy is contraindicated, if the diagnosis of cirrhosis has been clearly established
from the clinical findings and imaging:
Evidence of decompensation, with ascites
Labs indicating impaired hepatic biosynthesis
Liver biopsy is indicated :
Etiology of liver disease is unclear
Stage cannot be determined: length of punch cylinders used for liver biopsy should be atleast 15 mm long, and at least 10 portal fields should be examined per sectional level
Diagnosis in doubt
If the biopsy is expected to yield information about the cause of cirrhosis that will affect the treatment choice
Noninvasive diagnostic evaluation of cirrhosis
Laboratory-based methods:
Routine liver function tests
Hyaluronic acid concentration
AST-to-platelet ratio index: (APRI) is easily calculated as the quotient of the AST
(GOT)
Platelet count: screening index for advanced fibrosis and cirrhosis
Transient elastography and the acoustic radiation force impulse (ARFI) technique are now well-established methods for the staging of fibrosis in various liver diseases
Is Liver Biopsy the Gold Standard
in the Diagnosis of Cirrhosis?
Liver biopsy is the gold standard in the diagnosis of cirrhosis, it is an imperfect test.
It is an invasive procedure with complications:
Sampling errors
Death
Measurement of hepatic venous pressure gradient (HVPG):
Indirect measure of sinusoidal pressure obtained through hepatic vein catheterization, has a greater diagnostic accuracy than liver biopsy.
Very accurate in predicting the development of disease progression and the presence of significant fibrosis.
HVPG measurement of 6 mmHg or greater indicates the presence of cirrhosis.
HVPG addresses a larger area of hepatic parenchyma than liver biopsy, since the pressure obtained is
the average pressure of many sinusoids, thus reducing the possibility of sampling error due to
the presence of fibrosis heterogeneity within the diseased liver.
Noninvasive tests including serum markers, ultrasound, and liver and/or spleen stiffness measurements have become important tools in ruling in or excluding cirrhosis with a high diagnostic accuracy and may substitute for liver biopsy in the diagnosis of cirrhosis.
Laboratory findings —
Laboratory abnormalities may be the first indication of cirrhosis.
Common abnormalities include:
Increased serum bilirubin levels
abnormal aminotransferases
elevated alkaline phosphatase/gamma-glutamyl transpeptidase
prolonged prothrombin time
elevated international normalized ratio (INR)
Hyponatremia
Thrombocytopenia
Cherry
Physical Examination

GIF maker

Source:Wikimedia commons[49]

Source:Wikimedia commons

Source:Wikimedia commons
Physical Examination
- Physical examination of patients with cirrhosis is usually remarkable for: jaundice, spider angiomata, ascites, asterixis, spleenomegaly and palmar erythema.
Appearance of the Patient
- Patients with cirrhosis usually appear weak due to constitutional symptoms such as weight loss, anorexia and muscle atrophy. Yellowish discoloration of skin and abdominal distension may also be present due to ascites.
- Normal/low blood pressure with normal pulse pressure.
Skin
- Jaundice : yellow discoloration of the skin, eyes, and mucus membranes due to increased bilirubin (at least 2-3 mg/dL or 30 mmol/L). Urine may also appear dark.
- Pallor
- Bruises
- Palmar erythema on the thenar and hypothenar eminences, due to altered sex hormone metabolism.
- Spider angiomata: Increased estradiol levels lead to the formation of vascular lesions consisting of central arterioles surrounded by smaller vessels [50]
- Telangiectasias or spider veins: small dilated blood vessels near the surface of the skin.
HEENT
- Abnormalities of the head/hair may include thinning of hair on the scalp due to hyperestrogenism
- Kayser-Fleischer rings : dark rings that appear to encircle the iris of the eye in patients with Wilson's disease.
- Parotid gland enlargement
- Fetor hepaticus: severe portal-systemic shunting leads to increased levels of dimethyl sulfide leads to a sweet pungent smell in the breath
Abdomen
- Inspection:
- Palpation:
- Fluid wave
- Hepatomegaly may be present in initial stages. The liver may also be normal or shrunken.
- Spleenomegaly may be present in patients with cirrhosis from nonalcoholic etiologies, due to portal hypertension
- Percussion:
- Flank dullness may be present due to ascites (needs approximately 1500ml for detection)
- Auscultation:
- Cruveilhier-Baumgarten murmur: venous hum that may be present in patients with portal hypertension.
- Mechanism: due to collateral connections between remnant of the umbilical vein and the portal system
- Location: Epigastrium
- Exacerbating factors: Valsalva maneuver
- Diminished by: application of pressure on the skin above the umbilicus
- Cruveilhier-Baumgarten murmur: venous hum that may be present in patients with portal hypertension.
Genitourinary
- Testicular atrophy
- Inversion of the normal male pubic hair pattern
Neuromuscular
- Hepatic encephalopathy may have signs of:
- Alteration of mental status
- Confusion
- Coma
- Asterixis (bilateral but asynchronous flapping motions of outstretched, dorsiflexed hands) is seen in patients with hepatic encephalopathy.
Extremities
- edema of the lower extremities
- Muscle atrophy
- Nail changes:
- Muehrcke nails: paired horizontal white bands separated by normal color due to hypoalbuminemia
- Terry nails: the proximal two-thirds of the nail plate appears white, whereas the distal one-third is red due to hypoalbuminemia
- Clubbing: the angle between the nail plate and proximal nail fold is greater than 180 degrees
- Severe clubbing:
- "Drum stick" appearance of distal fingers
- Hypertrophic osteoarthropathy: chronic proliferative periostitis of the long bones
- Dupuytren's contracture may cause flexion deformities of the fingers: This occurs due to shortening and thickening of the palmar fascia, due to collagen deposition and fibroblastic proliferation.
- Asterixis in cases with hepatic encephalopathy
Chest findings
- Gynecomastia: due to increased estradiol levels
- Loss of chest or axillary hair
Other findings
History
Psychosocial history
- Past history of abuse
Past Medical history
- History of
Menstrual history
- History of
Family history
- Family history of:
Medication history
- History of medication use should be obtained as many drugs such as opioids cause constipation as a side effect.
Causes
| Drugs and Toxins | Infections | Autoimmune | Metabolic | Biliary obstruction(Secondary bilary cirrhosis) | Vascular | Miscellaneous |
|---|---|---|---|---|---|---|
| Alcohol | Hepatitis B | Primary Biliary Cirrhosis | Wilson's disease | Cystic fibrosis | Chronic RHF | Sarcoidosis |
| Methotrexate | Hepatitis C | Autoimmune hepatitis | Hemochromatosis | Biliary atresia | Budd-Chiari syndrome | Intestinal
bypass operations for obesity |
| Isoniazid | Schistosoma japonicum | Primary Sclerosing Cholangitis | Alpha-1 antitrypsin deficiency | Bile duct strictures | Veno-occlusive disease | Cryptogenic: unknown |
| Methyldopa | Porphyria | Gallstones | ||||
| Glycogen storage diseases (such as Galactosaemia, Abetalipoproteinaemia) |
Cirrhosis
Pathophysiology [51][52][53][54][55][56]
- When an injured issue is replaced by a collagenous scar, it is termed as fibrosis.
- When fibrosis of the liver reaches an advanced stage where distortion of the hepatic vasculature also occurs, it is termed as cirrhosis of the liver.
- The cellular mechanisms responsible for cirrhosis are similar regardless of the type of initial insult and site of injury within the liver lobule.
- Viral hepatitis involves the periportal region, whereas involvement in alcoholic liver disease is largely pericentral.
- If the damage progresses, panlobular cirrhosis may result.
- Cirrhosis involves the following steps: [57]
- Inflammation
- Hepatic stellate cell activation
- Angiogenesis
- Fibrogenesis
- Kupffer cells are hepatic macrophages responsible for Hepatic Stellate cell activation during injury.
- The hepatic stellate cell (also known as the perisinusoidal cell or Ito cell) plays a key role in the pathogenesis of liver fibrosis/cirrhosis.
- Hepatic stellate cells(HSC) are usually located in the subendothelial space of Disse and become activated to a myofibroblast-like phenotype in areas of liver injury.
- Collagen and non collagenous matrix proteins responsible for fibrosis are produced by the activated Hepatic Stellate Cells(HSC).
- Hepatocyte damage causes the release of lipid peroxidases from injured cell membranes leading to necrosis of parenchymal cells.
- Activated HSC produce numerous cytokines and their receptors, such as PDGF and TGF-f31 which are responsible for fibrogenesis.
- The matrix formed due to HSC activation is deposited in the space of Disse and leads to loss of fenestrations of endothelial cells, which is a process called capillarization.
- Cirrhosis leads to hepatic microvascular changes characterised by [58]
- formation of intra hepatic shunts (due to angiogenesis and loss of parenchymal cells)
- hepatic endothelial dysfunction
- The endothelial dysfunction is characterised by [59]
- insufficient release of vasodilators, such as nitric oxide due to oxidative stress
- increased production of vasoconstrictors (mainly adrenergic stimulation and activation of endothelins and RAAS)
- Fibrosis eventually leads to formation of septae that grossly distort the liver architecture which includes both the liver parenchyma and the vasculature. A cirrhotic liver compromises hepatic sinusoidal exchange by shunting arterial and portal blood directly into the central veins (hepatic outflow). Vascularized fibrous septa connect central veins with portal tracts leading to islands of hepatocytes surrounded by fibrous bands without central veins.[13][60][61]
- The formation of fibrotic bands is accompanied by regenerative nodule formation in the hepatic parenchyma.
- Advancement of cirrhosis may lead to parenchymal dysfunction and development of portal hypertension.
- Portal HTN results from the combination of the following:
- Structural disturbances associated with advanced liver disease account for 70% of total hepatic vascular resistance.
- Functional abnormalities such as endothelial dysfunction and increased hepatic vascular tone account for 30% of total hepatic vascular resistance.
Pathogenesis of Cirrhosis due to Alcohol:
- More than 66 percent of all American adults consume alcohol.
- Cirrhosis due to alcohol accounts for approximately forty percent of mortality rates due to cirrhosis.
- Mechanisms of alcohol-induced damage include:
- Impaired protein synthesis, secretion, glycosylation
- Ethanol intake leads to elevated accumulation of intracellular triglycerides by:
- Lipoprotein secretion
- Decreased fatty acid oxidation
- Increased fatty acid uptake
- Alcohol is converted by Alcohol dehydrogenase to acetaldehyde.
- Due to the high reactivity of acetaldehyde, it forms acetaldehyde-protein adducts which cause damage to cells by:
- Trafficking of hepatic proteins
- Interrupting microtubule formation
- Interfering with enzyme activities
- Damage of hepatocytes leads to the formation of reactive oxygen species that activate Kupffer cells.[56]
- Kupffer cell activation leads to the production of profibrogenic cytokines that stimulates stellate cells.
- Stellate cell activation leads to the production of extracellular matrix and collagen.
- Portal triads develop connections with central veins due to connective tissue formation in pericentral and periportal zones, leading to the formation of regenerative nodules.
- Shrinkage of the liver occurs over years due to repeated insults that lead to:
- Loss of hepatocytes
- Increased production and deposition of collagen
Pathology
- There are four stages of Cirrhosis as it progresses:
- Chronic nonsuppurative destructive cholangitis - inflammation and necrosis of portal tracts with lymphocyte infiltration leading to the destruction of the bile ducts.
- Development of biliary stasis and fibrosis
- Periportal fibrosis progresses to bridging fibrosis
- Increased proliferation of smaller bile ductules leading to regenerative nodule formation.
Classification
|
Cirrhosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case studies |
|
Sandbox:Cherry On the Web |
|
American Roentgen Ray Society Images of Sandbox:Cherry |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Charmaine Patel, M.D. [2]
Overview
Cirrhosis of the liver can be classified using two methods; classification based on etiology, and classification based on morphology. Currently, classifying cirrhosis based on morphology is not used, as it requires an invasive procedure to examine the gross appearance of the liver, and it provides little diagnostic value. Classifying cirrhosis according to etiology is a more accepted form of classification, as it can be attained through non-invasive laboratory testing, and has a higher diagnostic value.
Classification Based on Etiology
Cirrhosis can be classified by its etiology. This is the most widely accepted method of classification.
Alcoholic Cirrhosis
This is the most common cause of cirrhosis, and is caused by continuous and prolonged alcohol abuse. The American Academy of Family Physicians estimate that 60-70 percent of all cases of cirrhosis are a result of alcohol abuse.
Post-Necrotic Cirrhosis
This type of cirrhosis occurs after a massive event causes liver cell death. Viral hepatitis is the most common cause for this type of cirrhosis. Agents that are toxic to the liver can also cause this type of cirrhosis, as well as certain types of carcinomas.
Biliary Cirrhosis
This type of cirrhosis results from any diseases that cause biliary obstruction. There is usually a blockage in the bile duct and there may also be inflammation. The excess bile in the liver causes tissue destruction. It commonly results in jaundice.
Cardiac Cirrhosis
This type of cirrhosis is caused by congestive heart failure causing poor circulation of oxygenated blood to the liver. This results in liver cell death, and the subsequent replacement of dead cells by fibrous tissue.
Genetic Disorder
This is when the cirrhosis is caused by a genetic disorder such as hemochromatosis, Wilson's disease, or alpha-1 antitrypsin deficiency.
Malnutrition
This category contains cirrhosis caused by various forms of malnutrition, particularly chronic starvation.
Classification Based on Morphology
Cirrhosis has historically been classified upon the nodular morphology that is seen on upon the gross appearance of the liver. Accurate assessment of the liver morphology can only be obtained through surgery, biopsy, or autopsy, therefore more recently, more non-invasive means of classifying and determining the causes of cirrhosis are used.
| Micronodular | Macronodular | Mixed |
|---|---|---|
| Micronodular cirrhosis is characterized by nodules that are less than 3mm in diameter | Macronodular cirrhosis is characterized by nodules that are more than 3mm in diameter | Micronodular cirrhosis can often progress into macronodular cirrhosis. During this transformation, a mixed form of cirrhosis may be seen.[62] |
Causes:
|
Causes:
|
Mixed nodular cirrhosis is also seen in Indian childhood cirrhosis. [63] |
Video codes
Normal video
{{#ev:youtube|x6e9Pk6inYI}}
Video in table
Floating video
| Title |
| https://https://www.youtube.com/watch?v=ypYI_lmLD7g%7C350}} |
Redirect
- REDIRECTEsophageal web
synonym website
https://mq.b2i.sg/snow-owl/#!terminology/snomed/10743008
Image

Image to the right
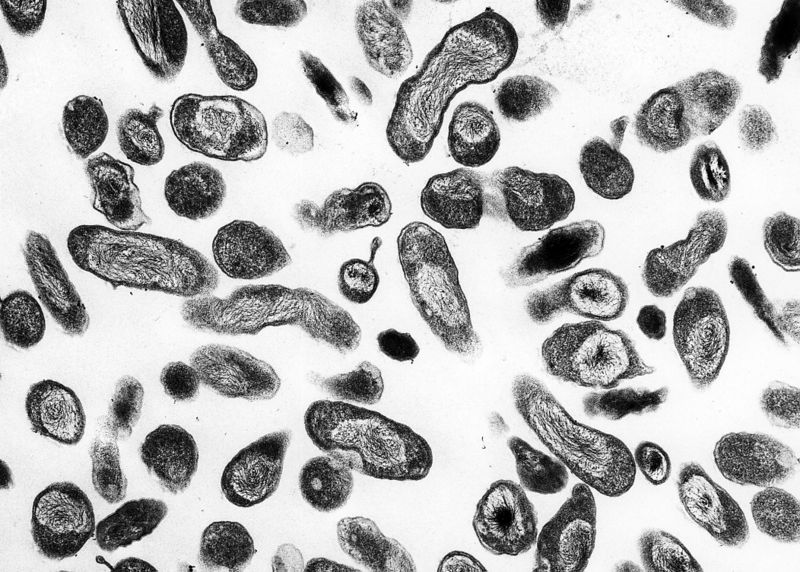 |
Image and text to the right
<figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline> </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
Gallery
-
Histopathology of a pancreatic endocrine tumor (insulinoma). Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[64]
-
Histopathology of a pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[64]
-
Histopathology of a pancreatic endocrine tumor (insulinoma). Insulin immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[64]
References
- ↑ Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ (2012). "The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology". Gastroenterology. 142 (7): 1592–609. doi:10.1053/j.gastro.2012.04.001. PMID 22656328.
- ↑ 2.0 2.1 Udell JA, Wang CS, Tinmouth J, FitzGerald JM, Ayas NT, Simel DL, Schulzer M, Mak E, Yoshida EM (2012). "Does this patient with liver disease have cirrhosis?". JAMA. 307 (8): 832–42. doi:10.1001/jama.2012.186. PMID 22357834.
- ↑ Krzeski P, Zych W, Kraszewska E, Milewski B, Butruk E, Habior A (1999). "Is serum bilirubin concentration the only valid prognostic marker in primary biliary cirrhosis?". Hepatology. 30 (4): 865–9. doi:10.1002/hep.510300415. PMID 10498635.
- ↑ Pratt DS, Kaplan MM (2000). "Evaluation of abnormal liver-enzyme results in asymptomatic patients". N. Engl. J. Med. 342 (17): 1266–71. doi:10.1056/NEJM200004273421707. PMID 10781624.
- ↑ 5.0 5.1 Kwo PY, Cohen SM, Lim JK (2017). "ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries". Am. J. Gastroenterol. 112 (1): 18–35. doi:10.1038/ajg.2016.517. PMID 27995906.
- ↑ Ruhl CE, Everhart JE (2010). "Trunk fat is associated with increased serum levels of alanine aminotransferase in the United States". Gastroenterology. 138 (4): 1346–56, 1356.e1–3. doi:10.1053/j.gastro.2009.12.053. PMC 2847039. PMID 20060831.
- ↑ Prati D, Taioli E, Zanella A, Della Torre E, Butelli S, Del Vecchio E, Vianello L, Zanuso F, Mozzi F, Milani S, Conte D, Colombo M, Sirchia G (2002). "Updated definitions of healthy ranges for serum alanine aminotransferase levels". Ann. Intern. Med. 137 (1): 1–10. PMID 12093239.
- ↑ Piton A, Poynard T, Imbert-Bismut F, Khalil L, Delattre J, Pelissier E, Sansonetti N, Opolon P (1998). "Factors associated with serum alanine transaminase activity in healthy subjects: consequences for the definition of normal values, for selection of blood donors, and for patients with chronic hepatitis C. MULTIVIRC Group". Hepatology. 27 (5): 1213–9. doi:10.1002/hep.510270505. PMID 9581673.
- ↑ Kaplan MM (2002). "Alanine aminotransferase levels: what's normal?". Ann. Intern. Med. 137 (1): 49–51. PMID 12093245.
- ↑ Nannipieri M, Gonzales C, Baldi S, Posadas R, Williams K, Haffner SM, Stern MP, Ferrannini E (2005). "Liver enzymes, the metabolic syndrome, and incident diabetes: the Mexico City diabetes study". Diabetes Care. 28 (7): 1757–62. PMID 15983331.
- ↑ Liangpunsakul S, Chalasani N (2012). "What should we recommend to our patients with NAFLD regarding alcohol use?". Am. J. Gastroenterol. 107 (7): 976–8. doi:10.1038/ajg.2012.20. PMC 3766378. PMID 22764020.
- ↑ Cohen JA, Kaplan MM (1979). "The SGOT/SGPT ratio--an indicator of alcoholic liver disease". Dig. Dis. Sci. 24 (11): 835–8. PMID 520102.
- ↑ 13.0 13.1 Schuppan D, Afdhal NH (2008). "Liver cirrhosis". Lancet. 371 (9615): 838–51. doi:10.1016/S0140-6736(08)60383-9. PMC 2271178. PMID 18328931.
- ↑ Cabrera-Abreu JC, Green A (2002). "Gamma-glutamyltransferase: value of its measurement in paediatrics". Ann. Clin. Biochem. 39 (Pt 1): 22–5. doi:10.1258/0004563021901685. PMID 11853185.
- ↑ Moussavian SN, Becker RC, Piepmeyer JL, Mezey E, Bozian RC (1985). "Serum gamma-glutamyl transpeptidase and chronic alcoholism. Influence of alcohol ingestion and liver disease". Dig. Dis. Sci. 30 (3): 211–4. PMID 2857631.
- ↑ Sheth SG, Flamm SL, Gordon FD, Chopra S (1998). "AST/ALT ratio predicts cirrhosis in patients with chronic hepatitis C virus infection". Am. J. Gastroenterol. 93 (1): 44–8. doi:10.1111/j.1572-0241.1998.044_c.x. PMID 9448172.
- ↑ Williams AL, Hoofnagle JH (1988). "Ratio of serum aspartate to alanine aminotransferase in chronic hepatitis. Relationship to cirrhosis". Gastroenterology. 95 (3): 734–9. PMID 3135226.
- ↑ 18.0 18.1 Ellis G, Goldberg DM, Spooner RJ, Ward AM (1978). "Serum enzyme tests in diseases of the liver and biliary tree". Am. J. Clin. Pathol. 70 (2): 248–58. PMID 696683.
- ↑ Goldberg DM (1980). "Structural, functional, and clinical aspects of gamma-glutamyltransferase". CRC Crit Rev Clin Lab Sci. 12 (1): 1–58. PMID 6104563.
- ↑ Barouki R, Chobert MN, Finidori J, Aggerbeck M, Nalpas B, Hanoune J (1983). "Ethanol effects in a rat hepatoma cell line: induction of gamma-glutamyltransferase". Hepatology. 3 (3): 323–9. PMID 6132864.
- ↑ Papadakis MA, Fraser CL, Arieff AI (1990). "Hyponatraemia in patients with cirrhosis". Q. J. Med. 76 (279): 675–88. PMID 2217672.
- ↑ Qamar AA, Grace ND, Groszmann RJ, Garcia-Tsao G, Bosch J, Burroughs AK, Ripoll C, Maurer R, Planas R, Escorsell A, Garcia-Pagan JC, Patch D, Matloff DS, Makuch R, Rendon G (2009). "Incidence, prevalence, and clinical significance of abnormal hematologic indices in compensated cirrhosis". Clin. Gastroenterol. Hepatol. 7 (6): 689–95. doi:10.1016/j.cgh.2009.02.021. PMC 4545534. PMID 19281860.
- ↑ Triger DR, Wright R (1973). "Hyperglobulinaemia in liver disease". Lancet. 1 (7818): 1494–6. PMID 4123153.
- ↑ Bianchi G, Marchesini G, Zoli M, Bugianesi E, Fabbri A, Pisi E (1994). "Prognostic significance of diabetes in patients with cirrhosis". Hepatology. 20 (1 Pt 1): 119–25. PMID 8020880.
- ↑ Petrides AS, Vogt C, Schulze-Berge D, Matthews D, Strohmeyer G (1994). "Pathogenesis of glucose intolerance and diabetes mellitus in cirrhosis". Hepatology. 19 (3): 616–27. PMID 8119686.
- ↑ 26.0 26.1 Becker CD, Scheidegger J, Marincek B (1986). "Hepatic vein occlusion: morphologic features on computed tomography and ultrasonography". Gastrointest Radiol. 11 (4): 305–11. PMID 3533689.
- ↑ Di Lelio A, Cestari C, Lomazzi A, Beretta L (1989). "Cirrhosis: diagnosis with sonographic study of the liver surface". Radiology. 172 (2): 389–92. doi:10.1148/radiology.172.2.2526349. PMID 2526349.
- ↑ Sanford NL, Walsh P, Matis C, Baddeley H, Powell LW (1985). "Is ultrasonography useful in the assessment of diffuse parenchymal liver disease?". Gastroenterology. 89 (1): 186–91. PMID 3891495.
- ↑ Giorgio A, Amoroso P, Lettieri G, Fico P, de Stefano G, Finelli L, Scala V, Tarantino L, Pierri P, Pesce G (1986). "Cirrhosis: value of caudate to right lobe ratio in diagnosis with US". Radiology. 161 (2): 443–5. doi:10.1148/radiology.161.2.3532188. PMID 3532188.
- ↑ Simonovský V (1999). "The diagnosis of cirrhosis by high resolution ultrasound of the liver surface". Br J Radiol. 72 (853): 29–34. doi:10.1259/bjr.72.853.10341686. PMID 10341686.
- ↑ Ernst O, Sergent G, Bonvarlet P, Canva-Delcambre V, Paris JC, L'Herminé C (1997). "Hepatic iron overload: diagnosis and quantification with MR imaging". AJR Am J Roentgenol. 168 (5): 1205–8. doi:10.2214/ajr.168.5.9129412. PMID 9129412.
- ↑ Bonkovsky HL, Rubin RB, Cable EE, Davidoff A, Rijcken TH, Stark DD (1999). "Hepatic iron concentration: noninvasive estimation by means of MR imaging techniques". Radiology. 212 (1): 227–34. doi:10.1148/radiology.212.1.r99jl35227. PMID 10405746.
- ↑ Gandon Y, Guyader D, Heautot JF, Reda MI, Yaouanq J, Buhé T, Brissot P, Carsin M, Deugnier Y (1994). "Hemochromatosis: diagnosis and quantification of liver iron with gradient-echo MR imaging". Radiology. 193 (2): 533–8. doi:10.1148/radiology.193.2.7972774. PMID 7972774.
- ↑ 34.0 34.1 Ito K, Mitchell DG, Hann HW, Kim Y, Fujita T, Okazaki H, Honjo K, Matsunaga N (1999). "Viral-induced cirrhosis: grading of severity using MR imaging". AJR Am J Roentgenol. 173 (3): 591–6. doi:10.2214/ajr.173.3.10470885. PMID 10470885.
- ↑ Ito K, Mitchell DG, Gabata T, Hussain SM (1999). "Expanded gallbladder fossa: simple MR imaging sign of cirrhosis". Radiology. 211 (3): 723–6. doi:10.1148/radiology.211.3.r99ma31723. PMID 10352597.
- ↑ Ito K, Mitchell DG, Hann HW, Outwater EK, Kim Y, Fujita T, Okazaki H, Honjo K, Matsunaga N (1998). "Progressive viral-induced cirrhosis: serial MR imaging findings and clinical correlation". Radiology. 207 (3): 729–35. doi:10.1148/radiology.207.3.9609897. PMID 9609897.
- ↑ Finn JP, Kane RA, Edelman RR, Jenkins RL, Lewis WD, Muller M, Longmaid HE (1993). "Imaging of the portal venous system in patients with cirrhosis: MR angiography vs duplex Doppler sonography". AJR Am J Roentgenol. 161 (5): 989–94. doi:10.2214/ajr.161.5.8273643. PMID 8273643.
- ↑ Friedrich-Rust M, Ong MF, Martens S, Sarrazin C, Bojunga J, Zeuzem S, Herrmann E (2008). "Performance of transient elastography for the staging of liver fibrosis: a meta-analysis". Gastroenterology. 134 (4): 960–74. doi:10.1053/j.gastro.2008.01.034. PMID 18395077.
- ↑ McLaren MI, Fleming JS, Walmsley BH, Ackery DM, Taylor I, Karran SJ (1985). "Dynamic liver scanning in cirrhosis". Br J Surg. 72 (5): 394–6. PMID 3995244.
- ↑ Williams EJ, Iredale JP (1998). "Liver cirrhosis". Postgrad Med J. 74 (870): 193–202. PMC 2360862. PMID 9683971.
- ↑ Tannapfel A, Dienes HP, Lohse AW (2012). "The indications for liver biopsy". Dtsch Arztebl Int. 109 (27–28): 477–83. doi:10.3238/arztebl.2012.0477. PMC 3402072. PMID 22833761.
- ↑ Schirmacher P, Fleig WE, Tannapfel A, Langner C, Dries V, Terracciano L, Denk H, Dienes HP (2004). "[Bioptic diagnosis of chronic hepatitis. Results of an evidence-based consensus conference of the German Society of Pathology, of the German Society for Digestive and Metabolic Diseases and of Compensated Hepatitis (HepNet)]". Pathologe (in German). 25 (5): 337–48. doi:10.1007/s00292-004-0692-7. PMID 15278290.
- ↑ Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, Lok AS (2003). "A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C". Hepatology. 38 (2): 518–26. doi:10.1053/jhep.2003.50346. PMID 12883497.
- ↑ Forns X, Ampurdanès S, Llovet JM, Aponte J, Quintó L, Martínez-Bauer E, Bruguera M, Sánchez-Tapias JM, Rodés J (2002). "Identification of chronic hepatitis C patients without hepatic fibrosis by a simple predictive model". Hepatology. 36 (4 Pt 1): 986–92. doi:10.1053/jhep.2002.36128. PMID 12297848.
- ↑ Vallet-Pichard A, Mallet V, Nalpas B, Verkarre V, Nalpas A, Dhalluin-Venier V, Fontaine H, Pol S (2007). "FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest". Hepatology. 46 (1): 32–6. doi:10.1002/hep.21669. PMID 17567829.
- ↑ Imbert-Bismut F, Ratziu V, Pieroni L, Charlotte F, Benhamou Y, Poynard T (2001). "Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study". Lancet. 357 (9262): 1069–75. doi:10.1016/S0140-6736(00)04258-6. PMID 11297957.
- ↑ Rosenberg WM, Voelker M, Thiel R, Becka M, Burt A, Schuppan D, Hubscher S, Roskams T, Pinzani M, Arthur MJ (2004). "Serum markers detect the presence of liver fibrosis: a cohort study". Gastroenterology. 127 (6): 1704–13. PMID 15578508.
- ↑ Castera L, Pinzani M (2010). "Biopsy and non-invasive methods for the diagnosis of liver fibrosis: does it take two to tango?". Gut. 59 (7): 861–6. doi:10.1136/gut.2010.214650. PMID 20581229.
- ↑ "Category:Histopathology of cirrhosis - Wikimedia Commons".
- ↑ Li CP, Lee FY, Hwang SJ; et al. (1999). "Spider angiomas in patients with liver cirrhosis: role of alcoholism and impaired liver function". Scand. J. Gastroenterol. 34 (5): 520–3. PMID 10423070.
- ↑ Arthur MJ, Iredale JP (1994). "Hepatic lipocytes, TIMP-1 and liver fibrosis". J R Coll Physicians Lond. 28 (3): 200–8. PMID 7932316.
- ↑ Friedman SL (1993). "Seminars in medicine of the Beth Israel Hospital, Boston. The cellular basis of hepatic fibrosis. Mechanisms and treatment strategies". N. Engl. J. Med. 328 (25): 1828–35. doi:10.1056/NEJM199306243282508. PMID 8502273.
- ↑ Iredale JP (1996). "Matrix turnover in fibrogenesis". Hepatogastroenterology. 43 (7): 56–71. PMID 8682489.
- ↑ Gressner AM (1994). "Perisinusoidal lipocytes and fibrogenesis". Gut. 35 (10): 1331–3. PMC 1374996. PMID 7959178.
- ↑ Iredale JP (2007). "Models of liver fibrosis: exploring the dynamic nature of inflammation and repair in a solid organ". J. Clin. Invest. 117 (3): 539–48. doi:10.1172/JCI30542. PMC 1804370. PMID 17332881.
- ↑ 56.0 56.1 Arthur MJ (2002). "Reversibility of liver fibrosis and cirrhosis following treatment for hepatitis C". Gastroenterology. 122 (5): 1525–8. PMID 11984538.
- ↑ Wanless IR, Wong F, Blendis LM, Greig P, Heathcote EJ, Levy G (1995). "Hepatic and portal vein thrombosis in cirrhosis: possible role in development of parenchymal extinction and portal hypertension". Hepatology. 21 (5): 1238–47. PMID 7737629.
- ↑ Fernández M, Semela D, Bruix J, Colle I, Pinzani M, Bosch J (2009). "Angiogenesis in liver disease". J. Hepatol. 50 (3): 604–20. doi:10.1016/j.jhep.2008.12.011. PMID 19157625.
- ↑ García-Pagán JC, Gracia-Sancho J, Bosch J (2012). "Functional aspects on the pathophysiology of portal hypertension in cirrhosis". J. Hepatol. 57 (2): 458–61. doi:10.1016/j.jhep.2012.03.007. PMID 22504334.
- ↑ Desmet VJ, Roskams T (2004). "Cirrhosis reversal: a duel between dogma and myth". J. Hepatol. 40 (5): 860–7. doi:10.1016/j.jhep.2004.03.007. PMID 15094237.
- ↑ Wanless IR, Nakashima E, Sherman M (2000). "Regression of human cirrhosis. Morphologic features and the genesis of incomplete septal cirrhosis". Arch. Pathol. Lab. Med. 124 (11): 1599–607. doi:10.1043/0003-9985(2000)124<1599:ROHC>2.0.CO;2. PMID 11079009.
- ↑ Fauerholdt L, Schlichting P, Christensen E, Poulsen H, Tygstrup N, Juhl E (1983). "Conversion of micronodular cirrhosis into macronodular cirrhosis". Hepatology. 3 (6): 928–31. PMID 6629323.
- ↑ Nayak NC, Ramalingaswami V (1975). "Indian childhood cirrhosis". Clin Gastroenterol. 4 (2): 333–49. PMID 47794.
- ↑ 64.0 64.1 64.2 Neuroendocrine tumor of the pancreas. Libre Pathology. http://librepathology.org/wiki/index.php/Neuroendocrine_tumour_of_the_pancreas
REFERENCES
![Histopathology of a pancreatic endocrine tumor (insulinoma). Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[64]](/images/2/2f/Pancreatic_insulinoma_histology_2.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[64]](/images/a/a3/Pancreatic_insulinoma_histopathology_3.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Insulin immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[64]](/images/d/d5/Pancreatic_insulinoma_histology_4.JPG)