Congenital adrenal hyperplasia: Difference between revisions
Undo revision 1465293 by Mehrian.jafari (talk) |
|||
| (21 intermediate revisions by 5 users not shown) | |||
| Line 16: | Line 16: | ||
==Overview== | ==Overview== | ||
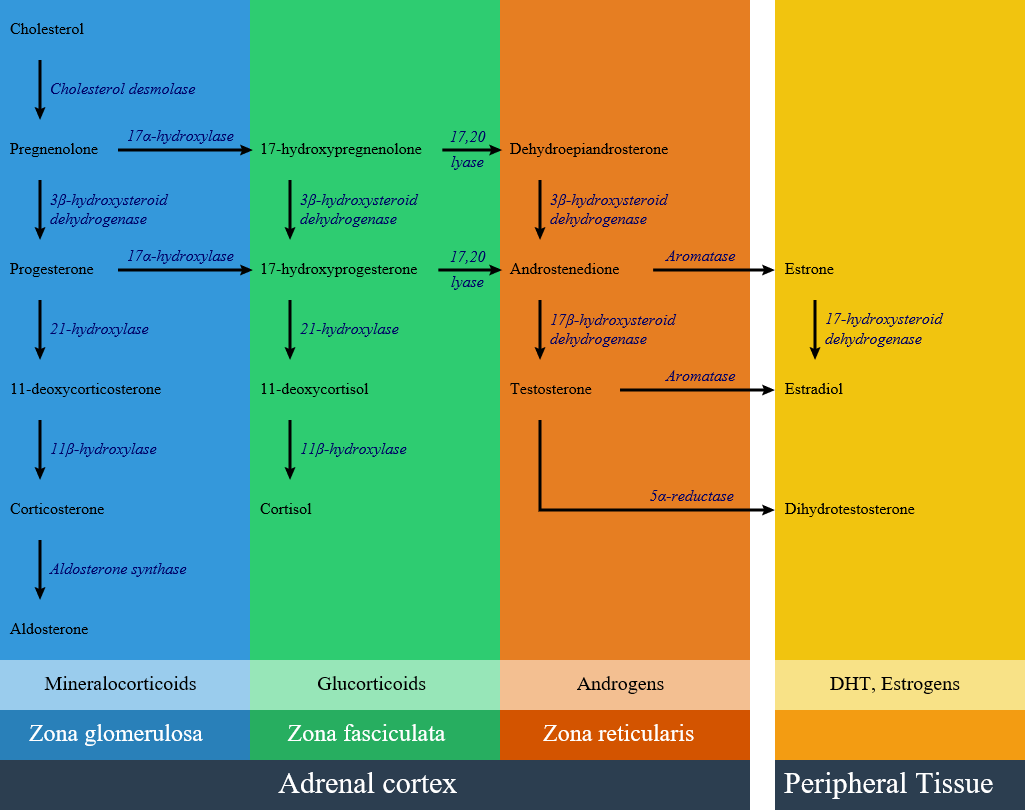
Congenital adrenal hyperplasia consists of several disorders | Congenital adrenal hyperplasia consists of several disorders resulting from defective [[enzymes]] and [[proteins]] involved in [[steroid]] and [[cortisol]] synthesis pathways. Defects in [[steroid]] [[biosynthesis]] are caused by several [[genetic mutations]] and may lead to [[delayed puberty]], [[precocious puberty]] or [[ambiguous genitalia]] in specific disorders. The decrease in [[cortisol]] level leads to the release of the inhibitory feedback on [[corticotropin]] ([[ACTH]]) production. The high [[ACTH]] level causes increase [[cortisol]] precursors and overproduction of other [[hormones]]. The most common cause of congenital adrenal hyperplasia is a [[21-hydroxylase deficiency]], which accounts for more than 95% of cases. Other causes include [[17 alpha-hydroxylase deficiency]], [[11β-hydroxylase deficiency]], [[3 beta-hydroxysteroid dehydrogenase deficiency]], [[Cytochrome P450-oxidoreductase (POR) deficiency (ORD)]], and [[congenital lipoid adrenal hyperplasia]]. | ||
==Classification== | ==Classification== | ||
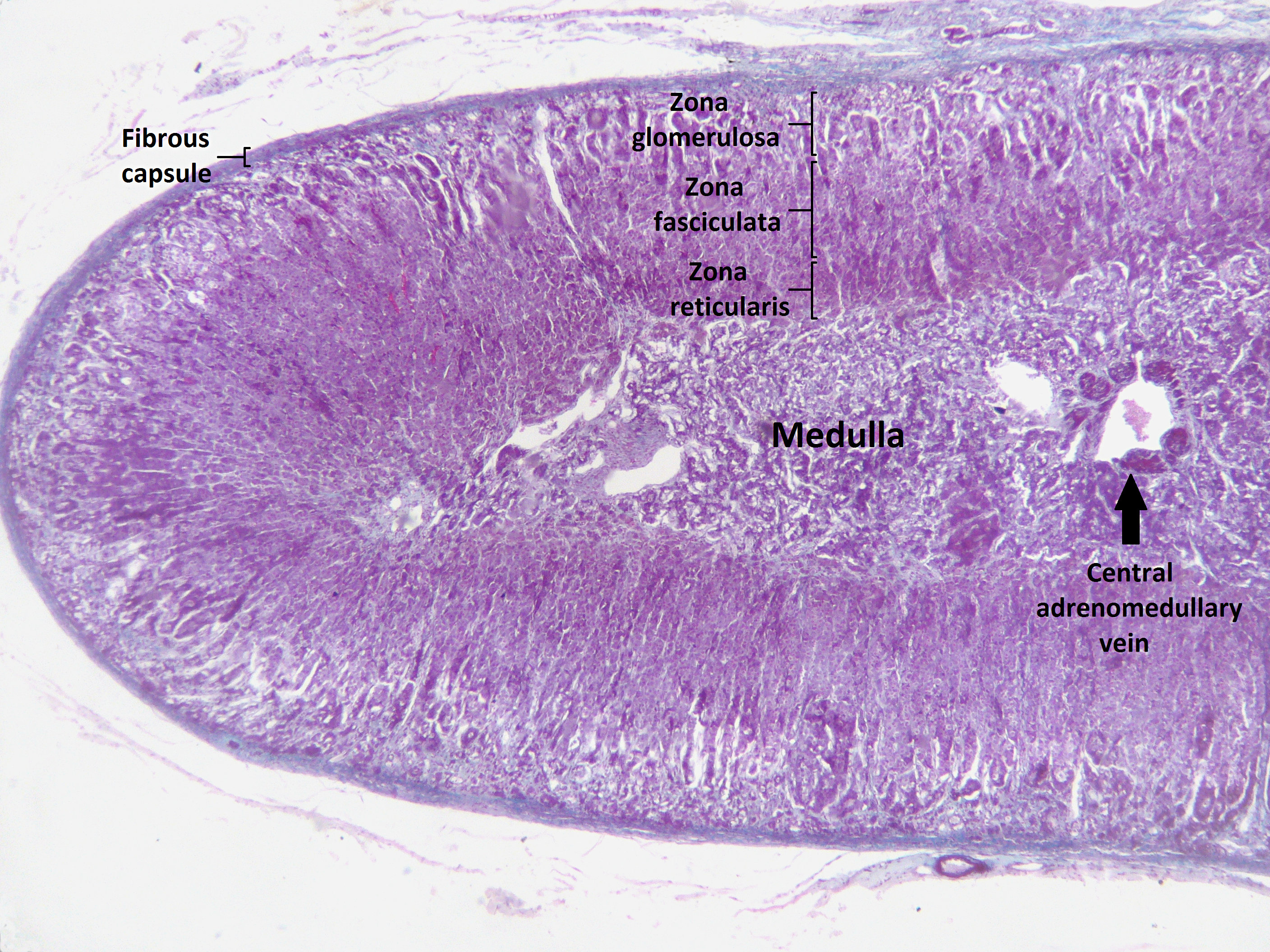
Congenital adrenal hyperplasia (CAH) is classified into seven types based on the [[genetic]] causes that lead to [[hyperplasia]] and hormonal imbalance. CAH is hyperplasia of different layer of [[Adrenal cortex]]. Within the [[adrenal cortex]], there are three layers named zones; each of them has a distinct cell type and secrete specific hormones. | Congenital adrenal hyperplasia (CAH) is classified into seven types based on the [[genetic]] causes that lead to [[hyperplasia]] and [[Hormone|hormonal]] imbalance. CAH is [[hyperplasia]] of different layer of [[Adrenal cortex]]. Within the [[adrenal cortex]], there are three layers named zones; each of them has a distinct cell type and secrete specific [[hormones]]. | ||
==== [[Adrenal cortex]] zones based on the hormonal synthesis ability and location: ==== | ==== [[Adrenal cortex]] zones based on the hormonal synthesis ability and location: ==== | ||
<div style="-webkit-user-select: none;"> | <div style="-webkit-user-select: none;"> | ||
* Zona glumerulosa: | * Zona glumerulosa: | ||
** The outer layer of [[adrenal cortex|adrenal cortex.]] | ** The outer layer of [[adrenal cortex|adrenal cortex.]] | ||
** Laying directly under the [[Adrenal gland|adrenal]] capsule. | ** Laying directly under the [[Adrenal gland|adrenal]] [[capsule]]. | ||
** Secretion: [[Aldosterone]] synthesis. | ** Secretion: [[Aldosterone]] synthesis. | ||
* Zona fasciculate: | * Zona fasciculate: | ||
| Line 51: | Line 50: | ||
[[image:Adrenal Steroids.png|thumb|800px|center|Adrenal steroid synthesis pathways in adrenal cortex and related enzymes <ref name="urlFile:Adrenal Steroids Pathways.svg - Wikimedia Commons">{{cite web |url=https://commons.wikimedia.org/wiki/File:Adrenal_Steroids_Pathways.svg|title=File:Adrenal Steroids Pathways.svg - Wikimedia Commons |format= |work= |accessdate=}}</ref>]] | [[image:Adrenal Steroids.png|thumb|800px|center|Adrenal steroid synthesis pathways in adrenal cortex and related enzymes <ref name="urlFile:Adrenal Steroids Pathways.svg - Wikimedia Commons">{{cite web |url=https://commons.wikimedia.org/wiki/File:Adrenal_Steroids_Pathways.svg|title=File:Adrenal Steroids Pathways.svg - Wikimedia Commons |format= |work= |accessdate=}}</ref>]] | ||
==== Summary and | ==== Summary and important Characteristics of the different congenital adrenal hyperplasia subtypes: <ref name="pmid2164530">{{cite journal |vauthors=Moreira AC, Leal AM, Castro M |title=Characterization of adrenocorticotropin secretion in a patient with 17 alpha-hydroxylase deficiency |journal=J. Clin. Endocrinol. Metab. |volume=71 |issue=1 |pages=86–91 |year=1990 |pmid=2164530 |doi=10.1210/jcem-71-1-86 |url=}}</ref><ref name="pmid999330">{{cite journal |vauthors=Heremans GF, Moolenaar AJ, van Gelderen HH |title=Female phenotype in a male child due to 17-alpha-hydroxylase deficiency |journal=Arch. Dis. Child. |volume=51 |issue=9 |pages=721–3 |year=1976 |pmid=999330 |pmc=1546244 |doi= |url=}}</ref><ref name="pmid226795">{{cite journal |vauthors=Biglieri EG |title=Mechanisms establishing the mineralocorticoid hormone patterns in the 17 alpha-hydroxylase deficiency syndrome |journal=J. Steroid Biochem. |volume=11 |issue=1B |pages=653–7 |year=1979 |pmid=226795 |doi= |url=}}</ref>==== | ||
<div style="-webkit-user-select: none;"> | <div style="-webkit-user-select: none;"> | ||
{| class="wikitable" align="center" style="border: 0px; font-size: 90%; margin: 3px;" | {| class="wikitable" align="center" style="border: 0px; font-size: 90%; margin: 3px;" | ||
| Line 74: | Line 73: | ||
* Female: [[Ambiguous genitalia]] | * Female: [[Ambiguous genitalia]] | ||
* Male: Normal or scrotal pigmentation and large phallus | * Male: Normal or scrotal [[pigmentation]] and large phallus | ||
| align="center" style="padding: 5px 5px; background: " |↓ | | align="center" style="padding: 5px 5px; background: " |↓ | ||
| align="center" style="padding: 5px 5px; background: " |↓↓ | | align="center" style="padding: 5px 5px; background: " |↓↓ | ||
| Line 137: | Line 136: | ||
* Female: [[Ambiguous genitalia]] | * Female: [[Ambiguous genitalia]] | ||
* Male: Normal or scrotal pigmentation and large phallus | * Male: Normal or scrotal pigmentation and large [[Phallus (embryology)|phallus]] | ||
| align="center" style="padding: 5px 5px; background: " |↓ | | align="center" style="padding: 5px 5px; background: " |↓ | ||
| align="center" style="padding: 5px 5px; background: " |↑ | | align="center" style="padding: 5px 5px; background: " |↑ | ||
| Line 192: | Line 191: | ||
| align="center" style="padding: 5px 5px; background: " |None of precursors increased | | align="center" style="padding: 5px 5px; background: " |None of precursors increased | ||
| align="center" style="padding: 5px 5px; background: " |↓ | | align="center" style="padding: 5px 5px; background: " |↓ | ||
|[[Gene mutation|Gene mutations]] on chromosome 8, codes for a protein called steroid acute regulatory protein (StAR) | |[[Gene mutation|Gene mutations]] on [[Chromosome 8 (human)|chromosome 8]], codes for a [[protein]] called [[steroid]] acute regulatory protein (StAR) | ||
|} | |} | ||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
Congenital adrenal hyperplasia can present with different symptoms such as: | |||
* [[Ambiguous genitalia]] | |||
* [[Virilization]] and [[hirsutism]] in female | |||
* [[Primary amenorrhea]] | |||
* Low reninemic [[hypertension]] | |||
Differential diagnosis for each of these symptoms are described in below tables. | |||
===[[Congenital adrenal hyperplasia]] must be differentiated from diseases that cause [[ambiguous genitalia]]:<ref name="pmid17875484">{{cite journal |vauthors=Hughes IA, Nihoul-Fékété C, Thomas B, Cohen-Kettenis PT |title=Consequences of the ESPE/LWPES guidelines for diagnosis and treatment of disorders of sex development |journal=Best Pract. Res. Clin. Endocrinol. Metab. |volume=21 |issue=3 |pages=351–65 |year=2007 |pmid=17875484 |doi=10.1016/j.beem.2007.06.003 |url=}}</ref><ref name="pmid10857554">{{cite journal |vauthors=White PC, Speiser PW |title=Congenital adrenal hyperplasia due to 21-hydroxylase deficiency |journal=Endocr. Rev. |volume=21 |issue=3 |pages=245–91 |year=2000 |pmid=10857554 |doi=10.1210/edrv.21.3.0398 |url=}}</ref>=== | ===[[Congenital adrenal hyperplasia]] must be differentiated from diseases that cause [[ambiguous genitalia]]:<ref name="pmid17875484">{{cite journal |vauthors=Hughes IA, Nihoul-Fékété C, Thomas B, Cohen-Kettenis PT |title=Consequences of the ESPE/LWPES guidelines for diagnosis and treatment of disorders of sex development |journal=Best Pract. Res. Clin. Endocrinol. Metab. |volume=21 |issue=3 |pages=351–65 |year=2007 |pmid=17875484 |doi=10.1016/j.beem.2007.06.003 |url=}}</ref><ref name="pmid10857554">{{cite journal |vauthors=White PC, Speiser PW |title=Congenital adrenal hyperplasia due to 21-hydroxylase deficiency |journal=Endocr. Rev. |volume=21 |issue=3 |pages=245–91 |year=2000 |pmid=10857554 |doi=10.1210/edrv.21.3.0398 |url=}}</ref>=== | ||
| Line 269: | Line 275: | ||
| colspan="2" | | | colspan="2" | | ||
* Maternal serum [[androgen]] concentrations (usually [[testosterone]] and [[androstenedione]]) are high | * Maternal serum [[androgen]] concentrations (usually [[testosterone]] and [[androstenedione]]) are high | ||
* If [[virilization]] is caused by exogenous hormone administration, the values may be low because the offending hormone is usually a synthetic [[steroid]] not measured in assays for [[testosterone]] or other [[androgens]] | * If [[virilization]] is caused by exogenous [[hormone]] administration, the values may be low because the offending hormone is usually a synthetic [[steroid]] not measured in assays for [[testosterone]] or other [[androgens]] | ||
| | | | ||
* [[Androgen]] excess in mother | * [[Androgen]] excess in mother | ||
| Line 610: | Line 616: | ||
| align="center" style="padding: 5px 5px; background: " | | | align="center" style="padding: 5px 5px; background: " | | ||
[[Turner syndrome|45 XO]] | [[Turner syndrome|45 XO]] | ||
|} | |||
=== [[17 alpha-hydroxylase deficiency]] and [[11β-hydroxylase deficiency]] can cause low reninemic [[hypertension]] and should be differentiate from other causes of [[pseudohyperaldosteronism]] (low renin): === | |||
{| class="wikitable" | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" + |Pseudohyperaldosteronism causes | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" + |Etiology | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" + |Clinical features | |||
! colspan="4" align="center" style="background:#4479BA; color: #FFFFFF;" + |Labratory | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" + |Treatment | |||
|- | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Elevated mineralocorticoid | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Renin | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Aldosterone | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Other | |||
|- | |||
| rowspan="9" |Endogenous causes | |||
|[[17 alpha-hydroxylase deficiency]] | |||
|Mutations in the [[CYP17A1]] gene | |||
| | |||
* [[Ambiguous genitalia]] in male | |||
* [[Hypertension]] | |||
* [[Primary amenorrhea]] | |||
* Absence of [[secondary sexual characteristics]] | |||
* Minimal [[body hair]] | |||
| rowspan="2" |[[Deoxycorticosterone]] ([[Deoxycorticosterone|DOC]]) | |||
| rowspan="2" |↓ | |||
| rowspan="2" |↓ | |||
|[[Cortisol]] ↓ | |||
| rowspan="2" |[[Corticosteroids]] | |||
|- | |||
|[[11β-hydroxylase deficiency]] | |||
|Mutations in the [[CYP11B1]] gene | |||
| | |||
* [[Ambiguous genitalia]] in female | |||
* [[Hypertension]] and [[hypokalemia]] | |||
* [[Virilization]] | |||
|[[Cortisol]] ↓ | |||
|- | |||
|Apparent mineralocorticoid excess syndrome (AME) | |||
|Genetic or acquired defect of 11-HSD gene | |||
* [[Cortisone]] decreases and [[cortisol]] accumulates and binds to [[aldosterone]] receptors | |||
| | |||
* Severe juvenile [[hypertension]] | |||
* [[Hypercalciuria]], [[nephrocalcinosis]], [[polyuria]] (due to [[hypokalemia]]-induced [[nephrogenic diabetes insipidus]]) | |||
* [[Renal failure]] | |||
|[[Cortisol]] has [[mineralocorticoid]] effects | |||
|↓ | |||
|↓ | |||
|Urinary free [[cortisone]] ↓↓ | |||
|[[Dexamethasone]] and/or [[mineralocorticoid]] blockers | |||
|- | |||
|[[Liddle's syndrome|Liddle’s syndrome]] (Pseudohyperaldosteronism type 1) | |||
|Mutation of the epithelial [[sodium]] channels ([[ENaC]]) [[gene]] in the distal [[renal tubules]] | |||
| | |||
* [[Hypertension]] | |||
* [[Hypokalemia]] | |||
|No extra [[mineralocorticoid]] presents, and mutations in [[Sodium|Na]] channels mimic [[aldosterone]] mechanism | |||
|↓ | |||
|↓ | |||
|[[Cortisol]] ↓ | |||
|[[Amiloride]] or [[triamterene]] | |||
|- | |||
|[[Cushing’s syndrome]] | |||
| | |||
* The main pathogenetic mechanism is linked to the excess | |||
of [[cortisol]] which saturates 11-HSD2 activity, | |||
* This allows [[cortisol]] to bind [[mineralocorticoid receptor]] | |||
|Rapid [[Obesity|weight gain]], particularly of the [[trunk]] and [[face]] with [[limbs]] sparing ([[central obesity]]) | |||
* Proximal [[muscle weakness]] | |||
* A [[round face]] often referred to as a "[[moon face]]" | |||
* Excess [[sweating]] | |||
* [[Headache]] | |||
|[[Cortisol]] has [[mineralocorticoid]] effects | |||
|↓ | |||
| | |||
* ↓ if excess [[cortisol]] saturates 11-HSD2 enzyme activity | |||
* ↑ in direct activation of [[renin]] [[angiotensin]] system activation by [[glucocorticoids]] | |||
|Urinary free [[cortisol]] markedly ↑↑ | |||
| | |||
* [[Pasireotide]], [[Cabergoline]], [[Ketoconazole]], and [[Metyrapone]] | |||
* Adrenalectomy | |||
|- | |||
|Insensitivity to [[glucocorticoids]] (Chrousos syndrome) | |||
|Mutations in [[glucocorticoid receptor]] (GR) gene | |||
| | |||
* [[Hypertension]] | |||
* Adrenal [[hyperandrogenism]] | |||
|[[Deoxycorticosterone]] ([[Deoxycorticosterone|DOC]]) | |||
|↓ | |||
|↓ | |||
|[[Cortisol]] | |||
|[[Dexamethasone]] | |||
|- | |||
|[[Cortisol]]-secreting adrenocortical [[carcinoma]] | |||
|Multifactorial | |||
| | |||
Rapid [[Obesity|weight gain]], particularly of the [[trunk]] and [[face]] with [[limbs]] sparing ([[central obesity]]) | |||
* Proximal [[muscle weakness]] | |||
* A [[round face]] often referred to as a "[[moon face]]" | |||
* Excess [[sweating]] | |||
* [[Headache]] | |||
|[[Cortisol]] has [[mineralocorticoid]] effects | |||
|↓ | |||
| | |||
* ↓ if excess [[cortisol]] saturates 11-HSD2 enzyme activity | |||
* ↑ in direct activation of [[renin]] [[angiotensin]] system activation by [[glucocorticoids]] | |||
|Urinary free [[cortisol]] markedly ↑↑ | |||
|[[Surgery]] | |||
|- | |||
|Geller’s syndrome | |||
|[[Mutation]] of [[mineralocorticoid]] (MR) receptor that alters its specificity and allows [[progesterone]] to bind MR | |||
|Severe [[hypertension]] particularly during [[pregnancy]] | |||
|[[Progesterone]] has [[mineralocorticoid]] effects | |||
|↓ | |||
|↓ | |||
| - | |||
|[[mineralocorticoid]] blockers | |||
|- | |||
|Gordon’s syndrome (Pseudohypoaldosteronism type 2) | |||
|Mutations of at least four genes have been identified, including WNK1 and WNK4 | |||
| | |||
* [[Hypertension]] | |||
* [[Hyperkalemia]] | |||
* Normal renal function | |||
|No excess mineralocorticoid; an increased activity of the thiazide-sensitive Na–Cl co-transporter in the distal tubule | |||
|↓ | |||
|Normal | |||
|Hyperkalemia | |||
|thiazide diuretics and/or dietary sodium restriction | |||
|- | |||
| rowspan="4" |Exogenous causes | |||
|Corticosteroids with mineralocorticoid activity | |||
|Fludrocortisone or fluoroprednisolone can mimic the action of aldosterone, | |||
| | |||
* [[Hypertension]] | |||
* [[Hypokalemia]] | |||
|Medications such as fludrocortisone | |||
|↓ | |||
|↓ | |||
| - | |||
|Change the treatment | |||
|- | |||
|Licorice ingestion | |||
|[[Glycyrrhetinic acid]] that binds [[mineralocorticoid]] receptor and blocks 11-HSD2 at the level of classical target tissues of [[aldosterone]] | |||
| | |||
* [[Hypertension]] | |||
* [[Hypokalemia]] | |||
|<nowiki>-</nowiki> | |||
|↓ | |||
|↓ | |||
|Urinary free cortisol Moderate ↑ | |||
|Discontinue licorice | |||
|- | |||
|Grapefruit | |||
|High assumption of naringenin, a component of grapefruit, can also block 11-HSD | |||
| | |||
* [[Hypertension]] | |||
| - | |||
|↓ | |||
|↓ | |||
| - | |||
|Discontinue grapefruit | |||
|- | |||
|[[Estrogens]] | |||
|[[Estrogens]] can retain [[sodium]] and water by different mechanisms, causing: | |||
* Increased blood pressure values and suppressing the [[renin]] [[aldosterone]] system, on the other side inducing secondary hyperaldosteronism due to the stimulation of the synthesis of [[angiotensinogen]] | |||
| | |||
* [[Hypertension]] | |||
* [[Headache]] | |||
* [[Edema]] | |||
* [[Weight gain]] | |||
|<nowiki>-</nowiki> | |||
|↓ | |||
|↓ | |||
| - | |||
|Discontinue [[estrogens]] | |||
|} | |||
==== CAH must be differentiated from other causes of irregular menses and [[hirsutism]]: ==== | |||
{| class="wikitable" | |||
!Disease | |||
!Differentiating Features | |||
|- | |||
|[[Pregnancy]] | |||
| | |||
* Pregnancy always should be excluded in a patient with a history of [[amenorrhea]] | |||
* Features include amenorrhea or [[oligomenorrhea]], abnormal [[uterine bleeding]], [[Nausea and vomiting|nausea/vomiting]], cravings, [[weight gain]] (although not in the early stages and not if vomiting), [[polyuria]], [[abdominal cramps]] and [[constipation]], [[fatigue]], [[dizziness]]/[[lightheadedness]], and [[Hyperpigmentation|increased pigmentation]] (moles, [[nipples]]) | |||
* [[Uterus|Uterine]] enlargement is detectable on [[abdominal examination]] at approximately 14 weeks of [[gestation]] | |||
* [[Ectopic pregnancy]] may cause oligomenorrhea, amenorrhea, or abnormal uterine bleeding with [[abdominal pain]] and sometimes subtle or absent physical symptoms and signs of [[pregnancy]] | |||
|- | |||
|Hypothalamic amenorrhea | |||
| | |||
* Diagnosis of exclusion | |||
* Seen in athletes, people on crash diets, patients with significant systemic illness, and those experiencing undue [[stress]] or [[anxiety]] | |||
* Predisposing features are as follows [[weight loss]], particularly if features of [[anorexia nervosa]] are present or the [[BMI]] is <19 kg/m2 | |||
* Recent administration of depot [[Medroxyprogesterone acetate|medroxyprogesterone]], which may suppress [[ovarian]] activity for 6 months to a year | |||
* Use of [[dopamine agonists]] (eg, antidepressants) and major [[tranquilizers]] | |||
* [[Hyperthyroidism]] | |||
* In patients with weight loss related to anorexia nervosa, fine hair growth ([[lanugo]]) may occur all over the body, but it differs from [[hirsutism]] in its fineness and wide distribution | |||
|- | |||
|[[Primary amenorrhea]] | |||
| | |||
* Causes include [[reproductive system]] abnormalities, [[chromosomal]] abnormalities, or [[delayed puberty]] | |||
* If [[secondary sexual characteristics]] are present, an [[anatomic]] abnormality (eg, [[imperforate hymen]], which is rare) should be considered | |||
* If secondary sexual characteristics are absent, a chromosomal abnormality (eg, [[Turner syndrome]] ) or [[delayed puberty]] should be considered | |||
|- | |||
|[[Cushing's syndrome|Cushing syndrome]] | |||
| | |||
* [[Cushing syndrome]] is due to excessive [[glucocorticoid]] secretion from the [[adrenal glands]], either primarily or secondary to stimulation from [[Pituitary gland|pituitary]] or ectopic hormones; can also be caused by exogenous [[steroid]] use | |||
* Features include [[hypertension]], [[weight gain]] (central distribution), [[acne]], and abdominal striae Patients have [[Hyponatremia|low plasma sodium levels]] and elevated plasma cortisol levels on [[dexamethasone]] suppression testing | |||
|- | |||
|[[Hyperprolactinemia]] | |||
| | |||
* Mild [[hyperprolactinemia]] may occur as part of [[PCOS]]-related hormonal dysfunction | |||
* Other causes include [[stress]], [[lactation]], and use of [[dopamine antagonists]] | |||
* A [[prolactinoma]] of the [[pituitary gland]] is an uncommon cause and should be suspected if [[prolactin]] levels are very high (>200 ng/mL) | |||
* Physical examination findings are usually normal | |||
* As in patients with PCOS, hyperprolactinemia may be associated with mild [[galactorrhea]] and [[oligomenorrhea]] or [[amenorrhea]]; however, galactorrhea also can occur with [[nipple]] stimulation and/or [[stress]] when prolactin levels are within normal ranges | |||
* A large [[prolactinoma]] may cause [[headaches]] and [[visual field]] disturbance due to pressure on the [[optic chiasm]], classically a gradually increasing bi-temporal hemianopsia | |||
|- | |||
|Ovarian or adrenal tumor | |||
| | |||
* Benign [[Ovarian tumor|ovarian tumors]] and ovarian cancer are rare causes of excessive [[androgen]] secretion; [[adrenocortical]] [[tumors]] also can increase the production of [[sex hormones]] | |||
* [[Abdominal swelling]] or [[mass]], [[abdominal pain]] due to fluid leakage or [[torsion]], [[dyspareunia]], abdominal [[ascites]], and features of [[metastatic]] disease may be present | |||
* Features of androgenization include [[hirsutism]], [[weight gain]], [[oligomenorrhea]] or [[amenorrhea]], [[acne]], [[clitoral hypertrophy]], deepening of the voice, and high [[Androgen|serum androgen]] (eg, [[testosterone]], other androgens) levels | |||
* In patients with an androgen-secreting tumor, serum testosterone is not suppressed by [[dexamethasone]] | |||
|- | |||
|[[Congenital adrenal hyperplasia]] | |||
| | |||
* Congenital adrenal hyperplasia is a rare [[genetic]] condition resulting from 21-hydroxylase deficiency | |||
* The late-onset form presents at or around menarche Patients have features of androgenization and [[subfertility]] | |||
* Affects approximately 1% of hirsute patients More common in Ashkenazi Jews (19%), inhabitants of the former Yugoslavia (12%), and Italians (6%) | |||
* Associated with high levels of [[17-hydroxyprogesterone]] | |||
* A short [[adrenocorticotropic hormone]] stimulation test with measurement of serum17-hydroxyprogesterone confirms the diagnostic assays of a variety of androgenic hormones help define other rare adrenal enzyme deficiencies, which present similarly to [[21-hydroxylase deficiency]] | |||
|- | |||
|Anabolic steroid abuse | |||
| | |||
* [[Anabolic steroid|Anabolic steroids]] are synthetic hormones that imitate the actions of [[testosterone]] by increasing [[muscle]] bulk and strength | |||
* Should be considered if the patient is a serious sportswoman or bodybuilder | |||
* Features include [[virilization]] (including [[acne]] and [[hirsutism]]), often increased muscle bulk in male pattern, [[oligomenorrhea]] or [[amenorrhea]], [[clitoromegaly]], [[gastritis]], [[hepatomegaly]], [[alopecia]], and aggression | |||
* Altered [[liver function test]] results are seen | |||
|- | |||
|[[Hirsutism]] | |||
| | |||
* [[Hirsutism]] is excessive facial and body hair, usually coarse and in a male pattern of distribution | |||
* Approximately 10% of women report unwanted facial hair | |||
* There is often a family history and typically some Mediterranean or Middle Eastern ancestry | |||
* May also result from use of certain [[medications]], both [[androgens]], and others including [[danazol]], [[glucocorticoids]], [[cyclosporine]], and [[phenytoin]] | |||
* [[Menstrual cycle|Menstrual]] history is normal | |||
* When the cause is [[Genetics|genetic]], the excessive hair, especially on the face (upper lip), is present throughout adulthood, and there is no virilization | |||
* When secondary to medications, the excessive hair is of new onset, and other features of virilization, such as [[acne]] and deepened voice, may be present | |||
|} | |} | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
Latest revision as of 15:57, 23 April 2018
This page contains general information about Congenital adrenal hyperplasia. For more information on specific types, please visit the pages on 21-hydroxylase deficiency, 17 alpha-hydroxylase deficiency, 11β-hydroxylase deficiency, 3 beta-hydroxysteroid dehydrogenase deficiency, cytochrome P450-oxidoreductase (POR) deficiency (ORD), congenital lipoid adrenal hyperplasia.
| Adrenal insufficiency | |
 | |
|---|---|
| Adrenal gland |
|
Congenital adrenal hyperplasia main page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mehrian Jafarizade, M.D [2]
Synonyms and keywords: Congenital adrenal hyperplasia; CAH; Adrenal hyperplasia.
Overview
Congenital adrenal hyperplasia consists of several disorders resulting from defective enzymes and proteins involved in steroid and cortisol synthesis pathways. Defects in steroid biosynthesis are caused by several genetic mutations and may lead to delayed puberty, precocious puberty or ambiguous genitalia in specific disorders. The decrease in cortisol level leads to the release of the inhibitory feedback on corticotropin (ACTH) production. The high ACTH level causes increase cortisol precursors and overproduction of other hormones. The most common cause of congenital adrenal hyperplasia is a 21-hydroxylase deficiency, which accounts for more than 95% of cases. Other causes include 17 alpha-hydroxylase deficiency, 11β-hydroxylase deficiency, 3 beta-hydroxysteroid dehydrogenase deficiency, Cytochrome P450-oxidoreductase (POR) deficiency (ORD), and congenital lipoid adrenal hyperplasia.
Classification
Congenital adrenal hyperplasia (CAH) is classified into seven types based on the genetic causes that lead to hyperplasia and hormonal imbalance. CAH is hyperplasia of different layer of Adrenal cortex. Within the adrenal cortex, there are three layers named zones; each of them has a distinct cell type and secrete specific hormones.
Adrenal cortex zones based on the hormonal synthesis ability and location:
- Zona glumerulosa:
- The outer layer of adrenal cortex.
- Laying directly under the adrenal capsule.
- Secretion: Aldosterone synthesis.
- Zona fasciculate:
- The middle part of adrenal cortex
- Laying under zona glumerulosa
- Secretion: Cortisol synthesis
- Zona reticularis:
- The inner part of adrenal cortex
- Laying between zona fasciculate and adrenal medulla
- Secretion: Androgen synthesis
Impairment of each pathway and enzyme may lead to a specific subtype of congenital adrenal hyperplasia include:
- 21-hydroxylase deficiency
- 17 alpha-hydroxylase deficiency
- 11β-hydroxylase deficiency
- 3 beta-hydroxysteroid dehydrogenase deficiency
- Cytochrome P450-oxidoreductase (POR) deficiency (ORD)
- Congenital lipoid adrenal hyperplasia
Summary and important Characteristics of the different congenital adrenal hyperplasia subtypes: [2][3][4]
| Disease | History and symptoms | Laboratory findings | Defective gene | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Blood pressure | Genitalia | Cortisol | Aldosterone | Androgens | Estrogens | Increased hormone precursors | Potassium levels | |||
| 21-hydroxylase deficiency | Classic type, salt-wasting | ↓ |
|
↓ | ↓↓ | ↑ | Relatively low | ↑ | ||
| Classic type, non-salt-wasting | Normal |
|
↓ | ↓ | ↑ | Relatively low | Normal | CYP21A1 and CYP21A2 gene | ||
| Non-classic type | Normal |
|
Normal | Normal | ↑ | Relatively low |
|
Normal | ||
| 17-α hydroxylase deficiency | ↑ |
|
Normal corticosterone
Normal cortisol |
↑ | ↓ | ↓ | ↓ | CYP17A1 | ||
| 11-β hydroxylase deficiency | ↑ |
|
↓ | ↑ | ↑ | Relatively low |
|
↓ | CYP11B1 | |
| 3 beta-hydroxysteroid dehydrogenase deficiency | ↓ |
|
↓ | ↓ | Male:↓
Female:↑ |
↓ | ↑ | HSD3B2 | ||
| Cytochrome P450-oxidoreductase (POR) deficiency (ORD) | Normal |
|
↓ | Normal | ↓ | ↓ | Normal | Mutations in the flavoprotein co-factor of the enzymes CYP17A1, CYP21A2, and CYP19A1 (aromatase). | ||
| Congenital lipoid adrenal hyperplasia | ↓ |
|
↓ | ↓ | ↓ | ↓ | None of precursors increased | ↓ | Gene mutations on chromosome 8, codes for a protein called steroid acute regulatory protein (StAR) | |
Differential Diagnosis
Congenital adrenal hyperplasia can present with different symptoms such as:
- Ambiguous genitalia
- Virilization and hirsutism in female
- Primary amenorrhea
- Low reninemic hypertension
Differential diagnosis for each of these symptoms are described in below tables.
Congenital adrenal hyperplasia must be differentiated from diseases that cause ambiguous genitalia:[5][6]
| Disease | Steroid status | Important clinical findings | |
|---|---|---|---|
| Increased | Decreased | ||
| Classic type of 21-hydroxylase deficiency |
|
| |
| 11-β hydroxylase deficiency |
|
| |
| 17-α hydroxylase deficiency |
| ||
| 3 beta-hydroxysteroid dehydrogenase deficiency |
| ||
| Gestational hyperandrogenism |
|
| |
Congenital adrenal hyperplasia must be differentiated from diseases that cause virilization and hirsutism in female:[7][6][8]
| Disease | Steroid status | Other laboratory | Important clinical findings |
|---|---|---|---|
| Non-classic type of 21-hydroxylase deficiency | Increased:
|
|
|
| 11-β hydroxylase deficiency | Increased:
Decreased: |
|
|
| 3 beta-hydroxysteroid dehydrogenase deficiency | Increased:
Decreased: |
|
|
| Polycystic ovary syndrome |
|
|
|
| Adrenal tumors |
|
|
|
| Ovarian virilizing tumor |
|
|
|
| Cushing's syndrome |
|
||
| Hyperprolactinemia |
|
|
Some types of congenital adrenal hyperplasia must be differentiated from diseases with primary amenorrhea:[9][2][3][4][10][11][12][13]
| Disease | Cause | Differentiating | ||||||
|---|---|---|---|---|---|---|---|---|
| Findings | Uterus | Breast development | Testosterone | LH | FSH | Karyotyping | ||
| 3 beta-hydroxysteroid dehydrogenase deficiency |
|
Yes in female |
Yes in female |
↓ |
Normal |
Normal |
||
| 17-alpha-hydroxylase deficiency |
|
No |
No |
↓ |
Normal |
Normal |
||
| Gonadal dysgenesis |
|
|
Yes |
Yes |
↓ |
↑ |
↑ |
|
| Testicular regression syndrome |
|
|
No |
No |
↓ |
↑ |
↑ |
|
| LH receptor defects |
|
No |
No |
↓ |
↑ |
↑ |
||
| 5-alpha-reductase type 2 deficiency |
|
No |
No |
Normal male range |
High to normal |
High to normal |
||
| Androgen insensitivity syndrome |
|
|
No |
Yes |
Normal male range |
Normal |
Normal |
|
| Mullerian agenesis |
|
No |
Yes |
Normal female range |
Normal |
Normal |
||
| Primary ovarian insufficiency |
|
|
Yes |
Yes |
Normal female range |
↑ |
↑ |
|
| Hypogonadotropic hypogonadism |
|
|
Yes |
No |
Normal female range |
Low |
Normal |
|
|
|
Yes |
Yes |
Normal female range |
↑ |
↑ |
||
17 alpha-hydroxylase deficiency and 11β-hydroxylase deficiency can cause low reninemic hypertension and should be differentiate from other causes of pseudohyperaldosteronism (low renin):
| Pseudohyperaldosteronism causes | Disease | Etiology | Clinical features | Labratory | Treatment | |||
|---|---|---|---|---|---|---|---|---|
| Elevated mineralocorticoid | Renin | Aldosterone | Other | |||||
| Endogenous causes | 17 alpha-hydroxylase deficiency | Mutations in the CYP17A1 gene |
|
Deoxycorticosterone (DOC) | ↓ | ↓ | Cortisol ↓ | Corticosteroids |
| 11β-hydroxylase deficiency | Mutations in the CYP11B1 gene |
|
Cortisol ↓ | |||||
| Apparent mineralocorticoid excess syndrome (AME) | Genetic or acquired defect of 11-HSD gene
|
|
Cortisol has mineralocorticoid effects | ↓ | ↓ | Urinary free cortisone ↓↓ | Dexamethasone and/or mineralocorticoid blockers | |
| Liddle’s syndrome (Pseudohyperaldosteronism type 1) | Mutation of the epithelial sodium channels (ENaC) gene in the distal renal tubules | No extra mineralocorticoid presents, and mutations in Na channels mimic aldosterone mechanism | ↓ | ↓ | Cortisol ↓ | Amiloride or triamterene | ||
| Cushing’s syndrome |
of cortisol which saturates 11-HSD2 activity,
|
Rapid weight gain, particularly of the trunk and face with limbs sparing (central obesity)
|
Cortisol has mineralocorticoid effects | ↓ |
|
Urinary free cortisol markedly ↑↑ |
| |
| Insensitivity to glucocorticoids (Chrousos syndrome) | Mutations in glucocorticoid receptor (GR) gene |
|
Deoxycorticosterone (DOC) | ↓ | ↓ | Cortisol | Dexamethasone | |
| Cortisol-secreting adrenocortical carcinoma | Multifactorial |
Rapid weight gain, particularly of the trunk and face with limbs sparing (central obesity)
|
Cortisol has mineralocorticoid effects | ↓ |
|
Urinary free cortisol markedly ↑↑ | Surgery | |
| Geller’s syndrome | Mutation of mineralocorticoid (MR) receptor that alters its specificity and allows progesterone to bind MR | Severe hypertension particularly during pregnancy | Progesterone has mineralocorticoid effects | ↓ | ↓ | - | mineralocorticoid blockers | |
| Gordon’s syndrome (Pseudohypoaldosteronism type 2) | Mutations of at least four genes have been identified, including WNK1 and WNK4 |
|
No excess mineralocorticoid; an increased activity of the thiazide-sensitive Na–Cl co-transporter in the distal tubule | ↓ | Normal | Hyperkalemia | thiazide diuretics and/or dietary sodium restriction | |
| Exogenous causes | Corticosteroids with mineralocorticoid activity | Fludrocortisone or fluoroprednisolone can mimic the action of aldosterone, | Medications such as fludrocortisone | ↓ | ↓ | - | Change the treatment | |
| Licorice ingestion | Glycyrrhetinic acid that binds mineralocorticoid receptor and blocks 11-HSD2 at the level of classical target tissues of aldosterone | - | ↓ | ↓ | Urinary free cortisol Moderate ↑ | Discontinue licorice | ||
| Grapefruit | High assumption of naringenin, a component of grapefruit, can also block 11-HSD | - | ↓ | ↓ | - | Discontinue grapefruit | ||
| Estrogens | Estrogens can retain sodium and water by different mechanisms, causing:
|
- | ↓ | ↓ | - | Discontinue estrogens | ||
CAH must be differentiated from other causes of irregular menses and hirsutism:
| Disease | Differentiating Features |
|---|---|
| Pregnancy |
|
| Hypothalamic amenorrhea |
|
| Primary amenorrhea |
|
| Cushing syndrome |
|
| Hyperprolactinemia |
|
| Ovarian or adrenal tumor |
|
| Congenital adrenal hyperplasia |
|
| Anabolic steroid abuse |
|
| Hirsutism |
|
References
- ↑ "File:Adrenal Steroids Pathways.svg - Wikimedia Commons".
- ↑ Jump up to: 2.0 2.1 Moreira AC, Leal AM, Castro M (1990). "Characterization of adrenocorticotropin secretion in a patient with 17 alpha-hydroxylase deficiency". J. Clin. Endocrinol. Metab. 71 (1): 86–91. doi:10.1210/jcem-71-1-86. PMID 2164530.
- ↑ Jump up to: 3.0 3.1 Heremans GF, Moolenaar AJ, van Gelderen HH (1976). "Female phenotype in a male child due to 17-alpha-hydroxylase deficiency". Arch. Dis. Child. 51 (9): 721–3. PMC 1546244. PMID 999330.
- ↑ Jump up to: 4.0 4.1 Biglieri EG (1979). "Mechanisms establishing the mineralocorticoid hormone patterns in the 17 alpha-hydroxylase deficiency syndrome". J. Steroid Biochem. 11 (1B): 653–7. PMID 226795.
- ↑ Hughes IA, Nihoul-Fékété C, Thomas B, Cohen-Kettenis PT (2007). "Consequences of the ESPE/LWPES guidelines for diagnosis and treatment of disorders of sex development". Best Pract. Res. Clin. Endocrinol. Metab. 21 (3): 351–65. doi:10.1016/j.beem.2007.06.003. PMID 17875484.
- ↑ Jump up to: 6.0 6.1 White PC, Speiser PW (2000). "Congenital adrenal hyperplasia due to 21-hydroxylase deficiency". Endocr. Rev. 21 (3): 245–91. doi:10.1210/edrv.21.3.0398. PMID 10857554.
- ↑ Hohl A, Ronsoni MF, Oliveira M (2014). "Hirsutism: diagnosis and treatment". Arq Bras Endocrinol Metabol. 58 (2): 97–107. PMID 24830586. Vancouver style error: initials (help)
- ↑ Melmed, Shlomo (2016). Williams textbook of endocrinology. Philadelphia, PA: Elsevier. ISBN 978-0323297387.=
- ↑ Maimoun L, Philibert P, Cammas B, Audran F, Bouchard P, Fenichel P, Cartigny M, Pienkowski C, Polak M, Skordis N, Mazen I, Ocal G, Berberoglu M, Reynaud R, Baumann C, Cabrol S, Simon D, Kayemba-Kay's K, De Kerdanet M, Kurtz F, Leheup B, Heinrichs C, Tenoutasse S, Van Vliet G, Grüters A, Eunice M, Ammini AC, Hafez M, Hochberg Z, Einaudi S, Al Mawlawi H, Nuñez CJ, Servant N, Lumbroso S, Paris F, Sultan C (2011). "Phenotypical, biological, and molecular heterogeneity of 5α-reductase deficiency: an extensive international experience of 55 patients". J. Clin. Endocrinol. Metab. 96 (2): 296–307. doi:10.1210/jc.2010-1024. PMID 21147889.
- ↑ Saenger P (1996). "Turner's syndrome". N. Engl. J. Med. 335 (23): 1749–54. doi:10.1056/NEJM199612053352307. PMID 8929268.
- ↑ Bastian C, Muller JB, Lortat-Jacob S, Nihoul-Fékété C, Bignon-Topalovic J, McElreavey K, Bashamboo A, Brauner R (2015). "Genetic mutations and somatic anomalies in association with 46,XY gonadal dysgenesis". Fertil. Steril. 103 (5): 1297–304. doi:10.1016/j.fertnstert.2015.01.043. PMID 25813279.
- ↑ Imperato-McGinley J, Guerrero L, Gautier T, Peterson RE (1974). "Steroid 5alpha-reductase deficiency in man: an inherited form of male pseudohermaphroditism". Science. 186 (4170): 1213–5. PMID 4432067.
- ↑ Schnitzer JJ, Donahoe PK (2001). "Surgical treatment of congenital adrenal hyperplasia". Endocrinol. Metab. Clin. North Am. 30 (1): 137–54. PMID 11344932.