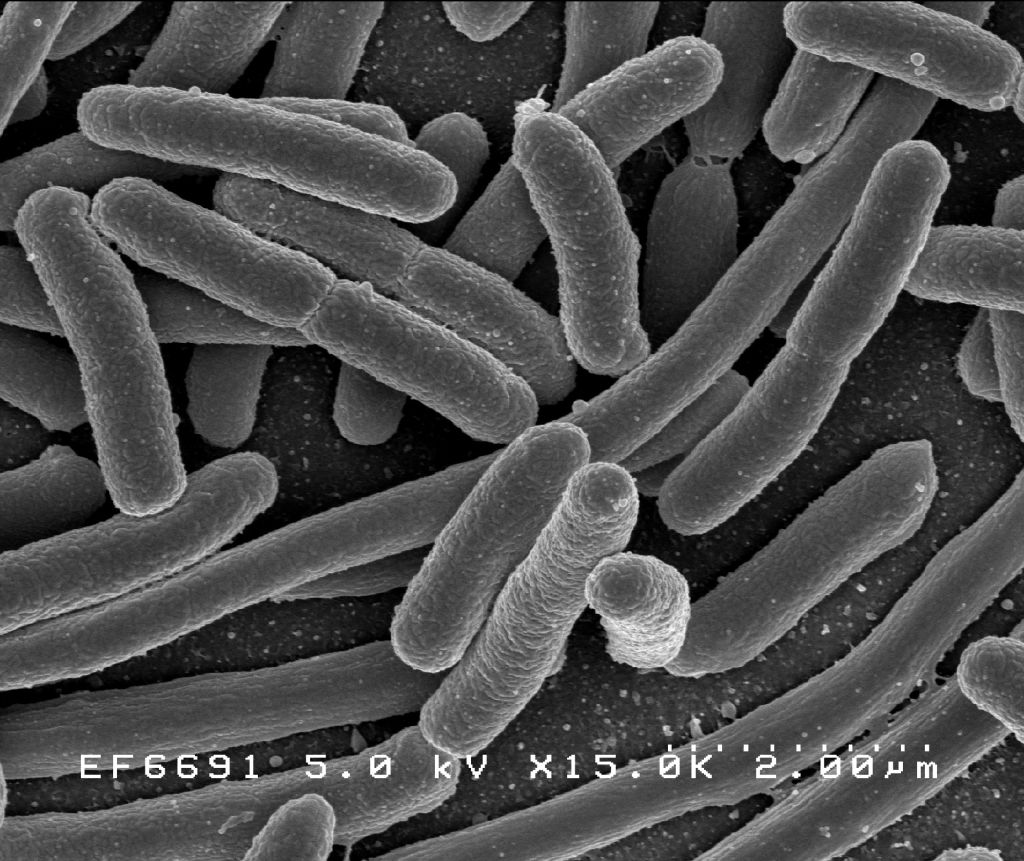
Escherichia coli
This page is about microbiologic aspects of the organism. To view a list of E. coli organ-based infections, click here.
To view specific information about E. coli O157:H7 strain, click here.
| Escherichia coli | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | ||||||||||||||
| Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Escherichia coli (Migula 1895) Castellani and Chalmers 1919 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Escherichia coli (Template:PronEng) (E. coli), is a bacterium that is commonly found in the lower intestine of warm-blooded animals. Most E. coli strains are harmless, but some, such as serotype O157:H7, can cause serious food poisoning in humans, and are occasionally responsible for costly product recalls.[1][2] The harmless strains are part of the normal flora of the gut, and can benefit their hosts by producing vitamin K2, or by preventing the establishment of pathogenic bacteria within the intestine.[3][4][5]
E. coli is not always confined to the intestine, and its ability to survive for brief periods outside the body makes it an ideal indicator organism to test environmental samples for fecal contamination.[6][7] The bacteria can also be grown easily and its genetics are comparatively simple and easily-manipulated, making it one of the best-studied prokaryotic model organisms, and an important species in biotechnology. E. coli was discovered by a German pediatrician and bacteriologist Theodor Escherich in 1885, and is now classified as part of the Enterobacteriaceae family of gamma-proteobacteria.[6][8]
Strains
A strain of E. coli is a sub-group within the species that has unique characteristics distinguishing it from other E. coli strains. These differences are often detectable only on the molecular level; however, they may result in changes to the physiology or life cycle of the bacterium. For example, a strain may gain pathogenic capacity, the ability to use a unique carbon source, the ability to inhabit a particular ecological niche, or the ability to resist antimicrobial agents. Different strains of E. coli are often host-specific, making it possible to determine the source of fecal contamination in environmental samples. Depending on which E. coli strains are present in a water sample, for example, assumptions can be made about whether the contamination originated from a human, other mammal, or bird source.
New strains of E. coli evolve through the natural biological process of mutation, and some strains develop traits that can be harmful to a host animal. Although virulent strains typically cause no more than a bout of diarrhea in healthy adult humans, particularly virulent strains, such as O157:H7 or O111:B4, can cause serious illness or death in the elderly, the very young, or the immunocompromised.[4]
Biology and Biochemistry
E. coli is Gram-negative, facultative anaerobic and non-sporulating. It can live on a wide variety of substrates. E. coli uses mixed-acid fermentation in anaerobic conditions, producing lactate, succinate, ethanol, acetate, and carbon dioxide. Since many pathways in mixed-acid fermentation produce hydrogen gas, these pathways require the levels of hydrogen to be low, as is the case when E. coli lives together with hydrogen-consuming organisms such as methanogens or sulfate-reducing bacteria.[9]
Optimal growth of E. coli occurs at 37°C, but some laboratory strains can multiply at temperatures of up to 49°C.[10] Growth can be driven by aerobic or anaerobic respiration, using a large variety of redox pairs, including the oxidation of pyruvic acid, formic acid, hydrogen and amino acids, and the reduction of substrates such as oxygen, nitrate, dimethyl sulfoxide and trimethylamine N-oxide.[11]
Strains that possess flagella can swim and are motile, but other strains lack flagellum. The flagella of E. coli have a peritrichous arrangement.[12]
E. coli and related bacteria possess the ability to transfer DNA via bacterial conjugation, transduction or transformation, which allows genetic material to spread horizontally through an existing population. It is believed that this process led to the spread of shiga toxin from Shigella to E. coli O157:H7.
Normal Role
E. coli normally colonizes an infant's gastrointestinal tract within 40 hours of birth, arriving with food or water or from the individuals handling the child. In the bowel, it adheres to the mucus of the large intestine. It is the primary facultative organism of the human gastrointestinal tract.[13] As long as these bacteria do not acquire genetic elements encoding for virulence factors, they remain benign commensals.[14]
Role in Disease
Virulent strains of E. coli can cause gastroenteritis, urinary tract infections, and neonatal meningitis. In rarer cases, virulent strains are also responsible for peritonitis, mastitis, septicemia and Gram-negative pneumonia.[13] Recently it is thought that E. coli and certain other foodborne illnesses can sometimes trigger serious health problems months or years after patients survived that initial bout. Food poisoning can be a long-term problem.
Virulence properties
Enteric E. coli (EC) are classified on the basis of serological characteristics and virulence properties.[13]
Virotypes include:
- Enterotoxigenic E. coli (ETEC) – It is the causative agent of diarrhea (without fever) in humans, pigs, sheep, goats, cattle, dogs, and horses. ETEC uses fimbrial adhesins (projections from the bacterial cell surface) to bind enterocytes in the small intestine. ETEC can produce two proteinaceous enterotoxins: the larger of the two proteins, LT enterotoxin, is similar to cholera toxin in structure and function, while the smaller protein, ST enterotoxin causes cGMP accumulation in the target cells and a subsequent secretion of fluid and electrolytes into the intestinal lumen. ETEC strains are non-invasive, and they do not leave the intestinal lumen.
- Enteropathogenic E. coli (EPEC) – It is the causative agent of diarrhea in humans, rabbits, dogs, cats and horses. Like ETEC, EPEC also causes diarrhea, but the molecular mechanism of colonization and etiology are different. EPEC lack fimbriae, ST and LT toxins, but they utilize an adhesin known as intimin to bind host intestinal cells. This virotype has an array of virulence factors that are similar to those found in Shigella, and may posses a shiga toxin. Adherence to the intestinal mucosa causes a rearrangement of actin in the host cell, causing significant deformation. EPEC cells are moderately-invasive (i.e. they enter host cells) and elicit an inflammatory response. Changes in intestinal cell ultrastructure due to "attachment and effacement" is likely the prime cause of diarrhea in those afflicted with EPEC.
- Enteroinvasive E. coli (EIEC) – It is found only in humans. EIEC infection causes a syndrome that is identical to Shigellosis, with profuse diarrhea and high fever. EIEC are highly invasive, and they utilize adhesin proteins to bind to and enter intestinal cells. They produce no toxins, but can cause severe damage to the intestinal wall through mechanical cell destruction.
- Enterohemorrhagic E. coli (EHEC) – It is found in humans, cattle, and goats. The sole member of this virotype is strain O157:H7, which causes bloody diarrhea and no fever. EHEC can cause hemolytic uremic syndrome and sudden kidney failure. It uses bacterial fimbriae for attachment and is moderately invasive. It possesses a phage-encoded Shiga toxin that can elicit an intense inflammatory response.
- Enteroaggregative E. coli (EAggEC) – It is found only in humans. This strain is named "aggregative" because their fimbriae aggregate tissue culture cells. EAggEC binds to the intestinal mucosa while being non-invasive and causes watery diarrhea without fever. It produces a hemolysin and an ST enterotoxin similar to that of ETEC.
Gastrointestinal infection

Certain strains of E. coli, such as O157:H7, O121 and O104:H21, produce toxins. Food poisoning caused by E. coli are usually associated with eating unwashed vegetables and meat contaminated post-slaughter. O157:H7 is further notorious for causing serious and even life-threatening complications such as Hemolytic Uremic Syndrome (HUS). This particular strain is linked to the 2006 United States E. coli outbreak of fresh spinach and the most recent multistate outbreak linked to romaine lettuce from the Central Coastal growing regions in northern and central California. Severity of the illness varies considerably; it can be fatal, particularly to young children, the elderly, or the immunocompromised, but is more often mild. E. coli can harbor both heat-stable and heat-labile enterotoxins. The latter, termed LT, contains one 'A' subunit and five 'B' subunits arranged into one holotoxin, and is highly similar in structure and function to Cholera toxins. The 'B' subunits assist in adherence and entry of the toxin into host intestinal cells, while the 'A' subunit is cleaved and prevents cells from absorbing water, causing diarrhea. LT is secreted by the Type 2 secretion pathway.[15]
If E. coli escapes the intestinal tract through a perforation (for example from an ulcer, a ruptured appendix, or a surgical error) and enters the abdomen, it usually causes peritonitis that can be fatal without prompt treatment. E. coli is extremely sensitive to antibiotics such as streptomycin or gentamicin and treatment with these antibiotics is usually effective.E. coli can also quickly acquire drug resistance which can be troublesome.[16]
Intestinal mucosa-associated E. coli is observed in increased numbers in patients with inflammatory bowel disease such as Crohn's disease and ulcerative colitis.[17] Invasive strains of E. coli exist in high numbers in the inflamed tissue, and the number of bacteria in the inflammatory foci correlates with the severity of the bowel inflammation.[18]
Epidemiology of gastrointestinal infection
Transmission of pathogenic E. coli often occurs via fecal-oral route. Common sources of contamination include: unhygienic food preparation, farm contamination due to manure fertilization, irrigation of crops with contaminated greywater or raw sewage, feral pigs on cropland, or direct consumption of sewage-contaminated water.[19][14][20][21][22][23][24]
Dairy and beef cattle are the primary reservoirs of E. coli O157:H7. They can carry it while being asymptomatic and shed it in their feces. Food products associated with E. coli outbreaks include raw ground beef, raw seed sprouts or spinach, raw milk, unpasteurized juice, lettuce (as observed in the most recent [October-November 2018] multistate outbreak of Shiga toxin-producing Escherichia coli O157:H7 (E. coli O157:H7) infections linked to romaine lettuce from the Central Coastal growing regions in northern and central California), and foods contaminated by infected food workers via fecal-oral route.[19][21][25][26]
According to the U.S. Food and Drug Administration, the fecal-oral cycle of transmission can be disrupted by cooking food properly, preventing cross-contamination, instituting barriers such as gloves for food workers, pasteurization of juice or dairy, proper hand washing requirements, and instituting health care policies requiring food industry employees to seek medical care when they are ill.[19]
Shiga toxin-producing E. coli (STEC), specifically serotype O157:H7, can also be transmitted by flies. Tranmission can also occur via direct contact with farm animals, petting zoo animals, and airborne particles found in animal-rearing environments.[27][28][29][30][31][32][33]
Urinary tract infection
Uropathogenic E. coli (UPEC) is responsible for approximately 90% of urinary tract infections (UTI) seen in individuals with ordinary anatomy. In ascending infections, fecal bacteria colonize the urethra and spread up the urinary tract to the bladder. Women are 14-times more likely to suffer from an ascending UTI as compared to men because of the anatomical difference in the urethral length.[13]
Uropathogenic E. coli utilize P fimbriae (pyelonephritis-associated pili) to bind urinary tract epithelium and colonize the bladder. These adhesins specifically bind D-galactose-D-galactose moieties on the P blood group antigen of erythrocytes and uroepithelial cells. Approximately 1% of the human population lacks this receptor, and its presence or absence dictates an individual's susceptibility to urinary tract infections caused by E. coli. Uropathogenic E. coli produce alpha- and beta-hemolysins, which cause lysis of urinary tract cells.[13]
UPEC can evade the body's innate immune defenses (e.g. the complement system) by invading superficial umbrella cells to form intracellular bacterial communities (IBCs). It can also have the ability to form K antigen and capsular polysaccharides that contribute to biofilm formation. Biofilm-producing E. coli is recalcitrant to immune factors and antibiotic therapy and can be responsible for chronic urinary tract infections. K antigen-producing E. coli commonly cause infection of the upper urinary tract.[13][34][35]
Descending infections, though relatively rare, occur when E. coli enters the upper urinary tract (kidneys, bladder or ureters) from the blood stream.
Diagnosis
Enteropathogenic E. coli (EPEC) and Enterotoxigenic E. coli (ETEC) - UTI or GIT infections in infants are caused by EPEC which present as watery diarrhea, meaning that PMN's will not be observed in the stool neither with methylene blue nor Gram stain. Gram negative rods, with no particular arrangement, are seen on Gram stain. On MacConkey agar inoculated with stool, deep red colonies are produced as the organism is lactose positive, and this utilization will cause the medium's pH to drop leading to darkening of the medium. Growth on Levine EMB agar inoculated with stool will show black colonies with greenish-black metallic sheen. This is diagnosic of E. coli. The organism is lysine positive, and grows on TSI slant with a (A/A/g+/H2S-) profile. IMViC is ++-- for E. coli as it is indol positive (red ring) and methyl red positive (bright red), but Voges–Proskauer (VP) negative (no change - colorless) and citrate negative (no change-green color). Serology is done using the SSS-Coagglutination test.
Enterohaemorrhagic E. coli O157:H7 - It is isolated either from urine or, more commonly, stool. There exist three protocols for diagnosis:
- Diagnosis is made in the manner similar to the diagnostic protocol of EPEC and ETEC. Sorbitol-MacConkey agar, a modified MacConkey agar which has sorbitol instead of lactose, is used and the EHEC produce colorless colonie due to is inability to utilize sorbitol. TSI slant and IMViC are then performed. Serology detects O157:H7 antigens.
- Gram stain demonstrating gram negative rods with no particular arrangement.
- Two bottles of verocells are used. One is inoculated with equal portions of stool extract and antitoxin, while the other containing only stool extract. If the first bottle shows neutralization (no cytopathic effects) while the second doesn't; the test is considered positive. This is based on the fact that the toxin produced by this strain is neutralized in the presence of its specific antibody, meaning that it will not be able to exert its effects on cells.
Antibiotic Therapy and Resistance
Bacterial infections are usually treated with antibiotics. However, the antibiotic sensitivities of different strains of E. coli vary widely. As a Gram-negative organism, E. coli is resistant to many antibiotics that are effective against Gram-positive organisms. Antibiotics which may be used to treat E. coli infection include amoxicillin as well as other semi-synthetic penicillins, many cephalosporins, carbapenems, aztreonam, trimethoprim-sulfamethoxazole, ciprofloxacin, nitrofurantoin, and aminoglycosides.
Antibiotic resistance is a growing problem. A part of it is due to the overuse of antibiotics in humans, but the use of antibiotics as growth promoters in the food of animals is also a contributing factor. A study published in the journal Science in August 2007 found that the rate of adaptative mutations in E. coli is on the order of 10–5 per genome per generation, which is 1,000 times as high as previous estimates. This finding is very significant for the study and management of bacterial antibiotic resistance.[36][37]
Antibiotic-resistant E. coli may also pass on the genes responsible for antibiotic resistance to other species of bacteria, such as Staphylococcus aureus. E. coli often carry multidrug resistant plasmids and when under stress, it can readily transfer those plasmids to other species. E. coli is a frequent member of biofilms, where many species of bacteria exist in close proximity to each other. This mixing of species allows E. coli strains that are piliated to accept and transfer plasmids from and to other bacteria. Thus, E. coli and the other enterobacteria are important reservoirs of transferable antibiotic resistance.[38]
Beta-lactamase strains
Resistance to beta-lactam antibiotics has become a particular problem in the recent decades, as strains of bacteria that produce extended-spectrum beta-lactamases have become more common. The beta-lactamase makes many, if not all, of the penicillins and cephalosporins ineffective as therapeutic measures. Extended-spectrum beta-lactamase–producing E. coli are highly resistant to an array of antibiotics and infections caused by these strains are difficult to treat. In many instances, only two oral antibiotics and a very limited group of intravenous antibiotics remain effective.[39]
Increased concern about the prevalence of this form of "superbug" in the United Kingdom has led to calls for further monitoring and a UK-wide strategy to deal with infections and the deaths. Susceptibility testing should guide treatment in all infections in which the organism can be isolated for culture.[40]
Phage therapy
Phage therapy involves the use of viruses that specifically target pathogenic bacteria. It has been developed over the last 80 years, primarily in the former Soviet Union, where it was used to prevent diarrhea caused by E. coli. Presently, phage therapy for humans is available only at the Phage Therapy Center in the Republic of Georgia and Poland. However, on January 2 2007, the United States Food and Drug Administration (FDA) gave Omnilytics (a biotech company focused on developing solutions for infectious disease and pest control) the approval to apply its E. coli O157:H7 killing phage in a mist, spray, or wash on live cattle bred for harvest.[41][42] [43]
Vaccination
Researchers have actively been working to develop safe, effective vaccines to lower the worldwide incidence of E. coli infection. In March, 2006, a vaccine, eliciting an immune response against the E. coli O157:H7 O-specific polysaccharide conjugated to recombinant exotoxin A of Pseudomonas aeruginosa (O157-rEPA), was reported to be safe in children two to five years old. Previous work had already indicated its safety in adults. A phase III clinical trial to verify the large-scale efficacy of the treatment is planned.[44][45]
In January 2007 the Canadian bio-pharmaceutical company Bioniche announced the development of a cattle vaccine which reduces the number of E. coli O157:H7 shed in manure to about 1000 pathogenic bacteria per gram of manure.[46][47][48]
Role in Biotechnology
File:E coli metabolic network.png
Because of its long history of laboratory culture and ease of manipulation, E. coli also plays an important role in modern biological engineering and industrial microbiology. The work of Stanley Norman Cohen and Herbert Boyer on E. coli, using plasmids and restriction enzymes to create recombinant DNA, has become a foundation.[49] [50]
E. coli is considered a very versatile host for the production of heterologous proteins. Researchers can introduce genes into the microbes using plasmids, allowing for the mass production of proteins used in the industrial fermentation processes. Genetic systems have also been developed which allow the production of recombinant proteins using E. coli. One of the first useful applications of recombinant DNA technology was the manipulation of E. coli to produce human insulin. Modified E. coli have been used in vaccine development, bioremediation, and production of immobilised enzymes. E. coli cannot, however, be used to produce some of the more large, complex proteins which contain multiple disulfide bonds and, in particular, unpaired thiols, or proteins that also require post-translational modification for activity.[49][51][52]
Model organism
E. coli is frequently used as a model organism in microbiology studies. Cultivated strains (e.g. E. coli K12) are well-adapted to the laboratory environment, and, unlike wild type strains, have lost their ability to thrive in the intestine. Many lab strains lose their ability to form biofilms.[53][54] These features protect wild type strains from antibodies and other chemical attacks, but require a large expenditure of energy and material resources.
In 1946, Joshua Lederberg and Edward Tatum first described the phenomenon known as bacterial conjugation using E. coli as a model bacterium,[55] and it remains the primary model to study conjugation. E. coli was an integral part of the first experiments to understand phage genetics,[56] and early researchers, such as Seymour Benzer, used E. coli and phage T4 to understand the topography of gene structure.[57] Prior to Benzer's research, it was not known whether the gene was a linear structure, or if it had a branching pattern.
See also
References
- ↑ "Escherichia coli O157:H7". CDC Division of Bacterial and Mycotic Diseases. Retrieved 2007-01-25.
- ↑ Vogt, R.L. (2005). "Escherichia coli O157:H7 outbreak associated with consumption of ground beef, June-July 2002". Public Health Reports. 2: 174–178. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) PMID 15842119. - ↑ Bentley, R, Meganathan, R., Biosynthesis of Vitamin K (menaquinone) in Bacteria, Bacteriological Reviews, 1982, 46(3):241-280. Review.
- ↑ 4.0 4.1 Hudault, S.; J. Guignot and A.L. Servin (July 2001). "Escherichia coli strains colonizing the gastrointestinal tract protect germfree mice against Salmonella typhimurium infection." Gut 49:47-55. PMID 11413110.
- ↑ Reid, G.; J. Howard and B.S. Gan (September 2001). "Can bacterial interference prevent infection?" Trends in Microbiology 9(9):424-428. PMID 11553454.
- ↑ 6.0 6.1 Feng P, Weagant S, Grant, M (2002-09-01). "Enumeration of Escherichia coli and the Coliform Bacteria". Bacteriological Analytical Manual (8th ed.). FDA/Center for Food Safety & Applied Nutrition. Retrieved 2007-01-25.
- ↑ Thompson, Andrea (June 4, 2007). "E. coli Thrives in Beach Sands". Live Science. Retrieved 2007-12-03.
- ↑ "Escherichia". Taxonomy Browser. NCBI. Retrieved 2007-11-30.
- ↑ Madigan MT, Martinko JM (2006). Brock Biology of microorganisms (11th ed. ed.). Pearson. ISBN 0-13-196893-9.
- ↑ Fotadar U, Zaveloff P, Terracio L (2005). "Growth of Escherichia coli at elevated temperatures". J. Basic Microbiol. 45 (5): 403–4. PMID 16187264.
- ↑ Ingledew WJ, Poole RK (1984). "The respiratory chains of Escherichia coli". Microbiol. Rev. 48 (3): 222&ndash, 71. PMID 6387427.
- ↑ Darnton NC, Turner L, Rojevsky S, Berg HC, On torque and tumbling in swimming Escherichia coli. J Bacteriol. 2007 Mar;189(5):1756-64. Epub 2006 Dec 22.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 Todar, K. "Pathogenic E. coli". Online Textbook of Bacteriology. University of Wisconsin-Madison Department of Bacteriology. Retrieved 2007-11-30.
- ↑ 14.0 14.1 Evans Jr., Doyle J. "Escherichia Coli". Medical Microbiology, 4th edition. The University of Texas Medical Branch at Galveston. Retrieved 2007-12-02. Unknown parameter
|coauthors=ignored (help) - ↑ Tauschek M, Gorrell R, Robins-Browne RM,. "Identification of a protein secretory pathway for the secretion of heat-labile enterotoxin by an enterotoxigenic strain of Escherichia coli". PNAS. 99: 7066–7071.
- ↑ "Gene Sequence Of Deadly E. Coli Reveals Surprisingly Dynamic Genome". Science Daily. 2001-01-25. Retrieved 2007-02-08.
- ↑ Rolhion N, Darfeuille-Michaud A (2007). "Adherent-invasive Escherichia coli in inflammatory bowel disease". Inflamm. Bowel Dis. 13 (10): 1277–83. doi:10.1002/ibd.20176. PMID 17476674.
- ↑ Baumgart M, Dogan B, Rishniw M; et al. (2007). "Culture independent analysis of ileal mucosa reveals a selective increase in invasive Escherichia coli of novel phylogeny relative to depletion of Clostridiales in Crohn's disease involving the ileum". ISME J. 1 (5): 403–18. doi:10.1038/ismej.2007.52. PMID 18043660.
- ↑ 19.0 19.1 19.2 "Retail Establishments; Annex 3 - Hazard Analysis". Managing Food Safety: A Manual for the Voluntary Use of HACCP Principles for Operators of Food Service and Retail Establishments. U.S. Department of Health and Human Services Food and Drug Administration Center for Food Safety and Applied Nutrition. April 2006. Retrieved 2007-12-02.
- ↑ Gehlbach, S.H. (1973). "Spread of disease by fecal-oral route in day nurseries". Health Service Reports. 88 (4): 320–322. PMID 4574421. Unknown parameter
|coauthors=ignored (help); Unknown parameter|month=ignored (help) - ↑ 21.0 21.1 Sabin Russell (Friday, October 13, 2006). "Spinach E. coli linked to cattle; Manure on pasture had same strain as bacteria in outbreak". San Francisco Chronicle. Retrieved 2007-12-02. Check date values in:
|date=(help) - ↑ Heaton, J.C. (2007). "Microbial contamination of fruit and vegetables and the behaviour of enteropathogens in the phyllosphere: a review". Journal of Applied Microbiology. doi:10.1111/j.1365-2672.2007.03587.x. PMID 17927745. Unknown parameter
|coauthors=ignored (help); Unknown parameter|month=ignored (help) - ↑ Thomas R. DeGregori (2007-08-17). "CGFI: Maddening Media Misinformation on Biotech and Industrial Agriculture". Retrieved 2007-12-08.
- ↑ Chalmers, R.M. (2000). "Waterborne Escherichia coli O157". Society for Applied Microbiology Symposium Series (29): 124S–132S. PMID 10880187. Unknown parameter
|coauthors=ignored (help) - ↑ Bach, S.J. (2002). "Transmission and control of Escherichia coli O157:H7". Canadian Journal of Animal Science. 82: 475–490. Unknown parameter
|coauthors=ignored (help) - ↑ Institute of Medicine of the National Academies (2002). Escherichia coli O157:H7 in Ground Beef: Review of a Draft Risk Assessment. Washington, D.C.: The National Academies Press. ISBN 0-309-08627-2.
- ↑ Heuvelink, A.E. (2002). "Escherichia coli O157 infection associated with a petting zoo". Epidemiology and Infection. 129 (2): 295–302. PMID 12403105. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Rahn, K. (1998). "Follow-up study of verocytotoxigenic Escherichia coli infection in dairy farm families". Journal of Infectious Disease. 177 (4): 1139–1140. PMID 9535003. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Trevena, W.B. (1999). "Transmission of Vero cytotoxin producing Escherichia coli O157 infection from farm animals to humans in Cornwall and west Devon". Community Disease and Public Health. 2 (4): 263–268. PMID 10598383. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Szalanski A, Owens C, McKay T, Steelman C (2004). "Detection of Campylobacter and Escherichia coli O157:H7 from filth flies by polymerase chain reaction". Med Vet Entomol. 18 (3): 241–6. PMID 15347391.
- ↑ Sela S, Nestel D, Pinto R, Nemny-Lavy E, Bar-Joseph M (2005). "Mediterranean fruit fly as a potential vector of bacterial pathogens". Appl Environ Microbiol. 71 (7): 4052–6. PMID 16000820.
- ↑ Alam M, Zurek L (2004). "Association of Escherichia coli O157:H7 with houseflies on a cattle farm". Appl Environ Microbiol. 70 (12): 7578–80. PMID 15574966.
- ↑ Varma, J.K. (2003). "An outbreak of Escherichia coli O157 infection following exposure to a contaminated building". JAMA. 290 (20): 2709–2712. PMID 14645313. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Justice S, Hunstad D, Seed P, Hultgren S (2006). "Filamentation by Escherichia coli subverts innate defenses during urinary tract infection". Proc Natl Acad Sci U S A. 103 (52): 19884–9. PMID 17172451.
- ↑ Ehrlich G, Hu F, Shen K, Stoodley P, Post J (2005). "Bacterial plurality as a general mechanism driving persistence in chronic infections". Clin Orthop Relat Res: 20–4. PMID 16056021. Unknown parameter
|month=ignored (help) - ↑ Johnson J, Kuskowski M, Menard M, Gajewski A, Xercavins M, Garau J (2006). "Similarity between human and chicken Escherichia coli isolates in relation to ciprofloxacin resistance status". J Infect Dis. 194 (1): 71–8. PMID 16741884.
- ↑ "Adaptive Mutations in Bacteria: High Rate and Small Effects". Science Magazine. 10 August 2007. Unknown parameter
|accessdaymonth=ignored (help); Unknown parameter|accessyear=ignored (|access-date=suggested) (help); Check date values in:|date=(help) - ↑ Salyers AA, Gupta A, Wang Y (2004). "Human intestinal bacteria as reservoirs for antibiotic resistance genes". Trends Microbiol. 12 (9): 412–6. PMID 15337162.
- ↑ Paterson DL, Bonomo RA (2005). "Extended-spectrum beta-lactamases: a clinical update". Clin. Microbiol. Rev. 18 (4): 657–86. PMID 16223952.
- ↑ "HPA Press Statement: Infections caused by ESBL-producing E. coli".
- ↑ "Medical conditions treated with phage therapy". Phage Therapy Center.
- ↑ "Therapeutic use of bacteriophages in bacterial infections". Polish Academy of Sciences.
- ↑ "OmniLytics Announces USDA/FSIS Approval for Bacteriophage Treatment of E. coli O157:H7 on Livestock". OmniLytics.
- ↑ Girard M, Steele D, Chaignat C, Kieny M (2006). "A review of vaccine research and development: human enteric infections". Vaccine. 24 (15): 2732–50. PMID 16483695.
- ↑ Ahmed A, Li J, Shiloach Y, Robbins J, Szu S (2006). "Safety and immunogenicity of Escherichia coli O157 O-specific polysaccharide conjugate vaccine in 2-5-year-old children". J Infect Dis. 193 (4): 515–21. PMID 16425130.
- ↑ Pearson H (2007). "The dark side of E. coli". Nature. 445 (7123): 8–9. PMID 17203031.
- ↑ "New cattle vaccine controls E. coli infections". Canada AM. 2007-01-11. Retrieved 2007-02-08.
- ↑ "Canadian Research Collaboration Produces World's First Food Safety Vaccine: Against E. coli O157:H7" (Press release). Bioniche Life Sciences Inc. 2007-01-10. Retrieved 2007-02-08. Check date values in:
|date=(help) - ↑ 49.0 49.1 Lee SY (1996). "High cell-density culture of Escherichia coli". Trends Biotechnol. 14 (3): 98–105. doi:10.1016/0167-7799(96)80930-9. PMID 8867291.
- ↑ "Special Report: The birth of biotechnology", Nature 421, 456-457 (23 January 2003)
- ↑ Cornelis P (2000). "Expressing genes in different Escherichia coli compartments". Curr. Opin. Biotechnol. 11 (5): 450–4. doi:10.1016/S0958-1669(00)00131-2. PMID 11024362.
- ↑ Tof, Ilanit (1994). "Recombinant DNA Technology in the Synthesis of Human Insulin". Little Tree Pty. Ltd. Retrieved 2007-11-30.
- ↑ Fux CA, Shirtliff M, Stoodley P, Costerton JW (2005). "Can laboratory reference strains mirror "real-world" pathogenesis?". Trends Microbiol. 13 (2): 58–63. doi:10.1016/j.tim.2004.11.001. PMID 15680764.
- ↑ Vidal O, Longin R, Prigent-Combaret C, Dorel C, Hooreman M, Lejeune P (1998). "Isolation of an Escherichia coli K-12 mutant strain able to form biofilms on inert surfaces: involvement of a new ompR allele that increases curli expression". J. Bacteriol. 180 (9): 2442–9. PMID 9573197.
- ↑ Lederberg, Joshua (1946). "Gene recombination in E. coli" (PDF). Nature. 158: 558. Unknown parameter
|coauthors=ignored (help); Unknown parameter|month=ignored (help) Source: National Library of Medicine - The Joshua Lederberg Papers - ↑ "The Phage Course - Origins". Cold Spring Harbor Laboratory. 2006. Retrieved 2007-12-03.
- ↑ Benzer, Seymour (1961). "On the topography of the genetic fine structure". PNAS. 47 (3): 403–415. Unknown parameter
|month=ignored (help)
General
- E.coli Food poisoning can be long-term problem - Yahoo News
- E. coli statistics
- Spinach and E. coli Outbreak - U.S. FDA
- E. coli Outbreak From Fresh Spinach - U.S. CDC
Databases
- EcoCyc: Encyclopedia of E. coli genes and metabolism
- Uropathogenic Escherichia coli (UPEC)
- Genome information on diarrheagenic E.coli and evolutionarily related organisms is available from the NIAID Enteropathogen Resource Integration Center (ERIC)
- EcoliHub
- The community annotation system for E. coli K-12 and its phages and plamids can be found at EcoliWiki
- The structure of the O-antigens that form the basis of the serological classification of E. coli
an:Escherichia coli bg:Escherichia coli ca:Escheríchia coli cs:Escherichia coli da:Escherichia coli de:Escherichia coli et:Soolekepike hr:Escherichia coli id:Escherichia coli it:Escherichia coli he:Escherichia coli kn:ಎಸ್ಚರೀಶಿಯ ಕೋಲಿ nl:Escherichia coli no:Escherichia coli nn:Escherichia coli oc:Escherichia coli simple:Escherichia coli sl:Escherichia coli sr:Ешерихија коли fi:Escherichia coli sv:Escherichia coli th:อีโคไล chr:Escherichia coli uk:Кишкова паличка