Pregabalin
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Pregabalin is a GABA analogue that is FDA approved for the treatment of neuropathic pain associated with diabetic peripheral neuropathy (DPN), postherpetic neuralgia (PHN), adjunctive therapy for adult patients with partial onset seizures ,fibromyalgia, neuropathic pain associated with spinal cord injury. Common adverse reactions include dizziness, somnolence, dry mouth, edema, blurred vision, weight gain and abnormal thinking (primarily difficulty with concentration/attention).
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- LYRICA is indicated for:
- Management of neuropathic pain associated with diabetic peripheral neuropathy
- Management of postherpetic neuralgia
- Adjunctive therapy for adult patients with partial onset seizures
- Management of fibromyalgia
- Management of neuropathic pain associated with spinal cord injury
Dosage And Administration
- LYRICA is given orally with or without food.
- When discontinuing LYRICA, taper gradually over a minimum of 1 week.
Neuropathic Pain Associated with Diabetic Peripheral Neuropathy
- The maximum recommended dose of LYRICA is 100 mg three times a day (300 mg/day) in patients with creatinine clearance of at least 60 mL/min. Begin dosing at 50 mg three times a day (150 mg/day). The dose may be increased to 300 mg/day within 1 week based on efficacy and tolerability. Because LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function.
- Although LYRICA was also studied at 600 mg/day, there is no evidence that this dose confers additional significant benefit and this dose was less well tolerated. In view of the dose-dependent adverse reactions, treatment with doses above 300 mg/day is not recommended.
Postherpetic Neuralgia
- The recommended dose of LYRICA is 75 to 150 mg two times a day, or 50 to 100 mg three times a day (150 to 300 mg/day) in patients with creatinine clearance of at least 60 mL/min. Begin dosing at 75 mg two times a day, or 50 mg three times a day (150 mg/day). The dose may be increased to 300 mg/day within 1 week based on efficacy and tolerability. Because LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function.
- Patients who do not experience sufficient pain relief following 2 to 4 weeks of treatment with 300 mg/day, and who are able to tolerate LYRICA, may be treated with up to 300 mg two times a day, or 200 mg three times a day (600 mg/day). In view of the dose-dependent adverse reactions and the higher rate of treatment discontinuation due to adverse reactions, reserve dosing above 300 mg/day for those patients who have on-going pain and are tolerating 300 mg daily.
Adjunctive Therapy for Adult Patients with Partial Onset Seizures
- LYRICA at doses of 150 to 600 mg/day has been shown to be effective as adjunctive therapy in the treatment of partial onset seizures in adults. Both the efficacy and adverse event profiles of LYRICA have been shown to be dose-related. Administer the total daily dose in two or three divided doses. In general, it is recommended that patients be started on a total daily dose no greater than 150 mg/day (75 mg two times a day, or 50 mg three times a day). Based on individual patient response and tolerability, the dose may be increased to a maximum dose of 600 mg/day.
- Because LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function.
- The effect of dose escalation rate on the tolerability of LYRICA has not been formally studied.
- The efficacy of add-on LYRICA in patients taking gabapentin has not been evaluated in controlled trials. Consequently, dosing recommendations for the use of LYRICA with gabapentin cannot be offered.
Management of Fibromyalgia
- The recommended dose of LYRICA for fibromyalgia is 300 to 450 mg/day. Begin dosing at 75 mg two times a day (150 mg/day). The dose may be increased to 150 mg two times a day (300 mg/day) within 1 week based on efficacy and tolerability. Patients who do not experience sufficient benefit with 300 mg/day may be further increased to 225 mg two times a day (450 mg/day). Although LYRICA was also studied at 600 mg/day, there is no evidence that this dose confers additional benefit and this dose was less well tolerated. In view of the dose-dependent adverse reactions, treatment with doses above 450 mg/day is not recommended. Because LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function.
Neuropathic Pain Associated with Spinal Cord Injury
- The recommended dose range of LYRICA for the treatment of neuropathic pain associated with spinal cord injury is 150 to 600 mg/day. The recommended starting dose is 75 mg two times a day (150 mg/day). The dose may be increased to 150 mg two times a day (300 mg/day) within 1 week based on efficacy and tolerability. Patients who do not experience sufficient pain relief after 2 to 3 weeks of treatment with 150 mg two times a day and who tolerate LYRICA may be treated with up to 300 mg two times a day. Because LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function.
Patients with Renal Impairment
- In view of dose-dependent adverse reactions and since LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function. Base the dose adjustment in patients with renal impairment on creatinine clearance (CLcr), as indicated in Table 1. To use this dosing table, an estimate of the patient's CLcr in mL/min is needed. CLcr in mL/min may be estimated from serum creatinine (mg/dL) determination using the Cockcroft and Gault equation:
- Next, refer to the Dosage and Administration section to determine the recommended total daily dose based on indication, for a patient with normal renal function (CLcr ≥60 mL/min). Then refer to Table 1 to determine the corresponding renal adjusted dose.
- (For example: A patient initiating LYRICA therapy for postherpetic neuralgia with normal renal function (CLcr ≥60 mL/min), receives a total daily dose of 150 mg/day pregabalin. Therefore, a renal impaired patient with a CLcr of 50 mL/min would receive a total daily dose of 75 mg/day pregabalin administered in two or three divided doses.)
- For patients undergoing hemodialysis, adjust the pregabalin daily dose based on renal function. In addition to the daily dose adjustment, administer a supplemental dose immediately following every 4-hour hemodialysis treatment (see Table 1).
Oral Solution Concentration and Dispensing
- The oral solution is 20 mg pregabalin per milliliter (mL) and prescriptions should be written in milligrams (mg). The pharmacist will calculate the applicable dose in mL for dispensing (e.g., 150 mg equals 7.5 mL oral solution).
Dosage Forms And Strengths
- Capsules: 25 mg, 50 mg, 75 mg, 100 mg, 150 mg, 200 mg, 225 mg, and 300 mg
- Oral Solution: 20 mg/mL
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Pregabalin in adult patients.
Non–Guideline-Supported Use
Generalized anxiety disorder
- 450 mg per day[1]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Pregabalin in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Pregabalin in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Pregabalin in pediatric patients.
Contraindications
- LYRICA is contraindicated in patients with known hypersensitivity to pregabalin or any of its components. Angioedema and hypersensitivity reactions have occurred in patients receiving pregabalin therapy.
Warnings
Precautions
- Angioedema
- There have been postmarketing reports of angioedema in patients during initial and chronic treatment with LYRICA. Specific symptoms included swelling of the face, mouth (tongue, lips, and gums), and neck (throat and larynx). There were reports of life-threatening angioedema with respiratory compromise requiring emergency treatment. Discontinue LYRICA immediately in patients with these symptoms.
- Exercise caution when prescribing LYRICA to patients who have had a previous episode of angioedema. In addition, patients who are taking other drugs associated with angioedema (e.g., angiotensin converting enzyme inhibitors ACE-inhibitors) may be at increased risk of developing angioedema.
- Hypersensitivity
- Withdrawal of Antiepileptic Drugs (AEDs)
- As with all AEDs, withdraw LYRICA gradually to minimize the potential of increased seizure frequency in patients with seizure disorders. If LYRICA is discontinued, taper the drug gradually over a minimum of 1 week.
- Suicidal Behavior and Ideation
- Antiepileptic drugs (AEDs), including LYRICA, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Monitor patients treated with any AED for any indication for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
- Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
- The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
- The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5–100 years) in the clinical trials analyzed.
- Table 2 shows absolute and relative risk by indication for all evaluated AEDs.
- The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
- Anyone considering prescribing LYRICA or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
- Inform patients, their caregivers, and families that LYRICA and other AEDs increase the risk of suicidal thoughts and behavior and advise them of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Report behaviors of concern immediately to healthcare providers.
- Peripheral Edema
- LYRICA treatment may cause peripheral edema. In short-term trials of patients without clinically significant heart or peripheral vascular disease, there was no apparent association between peripheral edema and cardiovascular complications such as hypertension or congestive heart failure. Peripheral edema was not associated with laboratory changes suggestive of deterioration in renal or hepatic function.
- In controlled clinical trials the incidence of peripheral edema was 6% in the LYRICA group compared with 2% in the placebo group. In controlled clinical trials, 0.5% of LYRICA patients and 0.2% placebo patients withdrew due to peripheral edema.
- Higher frequencies of weight gain and peripheral edema were observed in patients taking both LYRICA and a thiazolidinedione antidiabetic agent compared to patients taking either drug alone. The majority of patients using thiazolidinedione antidiabetic agents in the overall safety database were participants in studies of pain associated with diabetic peripheral neuropathy. In this population, peripheral edema was reported in 3% (2/60) of patients who were using thiazolidinedione antidiabetic agents only, 8% (69/859) of patients who were treated with LYRICA only, and 19% (23/120) of patients who were on both LYRICA and thiazolidinedione antidiabetic agents. Similarly, weight gain was reported in 0% (0/60) of patients on thiazolidinediones only; 4% (35/859) of patients on LYRICA only; and 7.5% (9/120) of patients on both drugs.
- As the thiazolidinedione class of antidiabetic drugs can cause weight gain and/or fluid retention, possibly exacerbating or leading to heart failure, exercise caution when co-administering LYRICA and these agents.
- Because there are limited data on congestive heart failure patients with New York Heart Association (NYHA) Class III or IV cardiac status, exercise caution when using LYRICA in these patients.
- Dizziness and Somnolence
- LYRICA may cause dizziness and somnolence. Inform patients that LYRICA-related dizziness and somnolence may impair their ability to perform tasks such as driving or operating machinery.
- In the LYRICA controlled trials, dizziness was experienced by 30% of LYRICA-treated patients compared to 8% of placebo-treated patients; somnolence was experienced by 23% of LYRICA-treated patients compared to 8% of placebo-treated patients. Dizziness and somnolence generally began shortly after the initiation of LYRICA therapy and occurred more frequently at higher doses. Dizziness and somnolence were the adverse reactions most frequently leading to withdrawal (4% each) from controlled studies. In LYRICA-treated patients reporting these adverse reactions in short-term, controlled studies, dizziness persisted until the last dose in 30% and somnolence persisted until the last dose in 42% of patients.
- LYRICA treatment may cause weight gain. In LYRICA controlled clinical trials of up to 14 weeks, a gain of 7% or more over baseline weight was observed in 9% of LYRICA-treated patients and 2% of placebo-treated patients. Few patients treated with LYRICA (0.3%) withdrew from controlled trials due to weight gain. LYRICA associated weight gain was related to dose and duration of exposure, but did not appear to be associated with baseline BMI, gender, or age. Weight gain was not limited to patients with edema.
- Although weight gain was not associated with clinically important changes in blood pressure in short-term controlled studies, the long-term cardiovascular effects of LYRICA-associated weight gain are unknown.
- Among diabetic patients, LYRICA-treated patients gained an average of 1.6 kg (range: -16 to 16 kg), compared to an average 0.3 kg (range: -10 to 9 kg) weight gain in placebo patients. In a cohort of 333 diabetic patients who received LYRICA for at least 2 years, the average weight gain was 5.2 kg.
- While the effects of LYRICA-associated weight gain on glycemic control have not been systematically assessed, in controlled and longer-term open label clinical trials with diabetic patients, LYRICA treatment did not appear to be associated with loss of glycemic control (as measured by HbA1C).
- Abrupt or Rapid Discontinuation
- Tumorigenic Potential
- In standard preclinical in vivo lifetime carcinogenicity studies of LYRICA, an unexpectedly high incidence of hemangiosarcoma was identified in two different strains of mice. The clinical significance of this finding is unknown. Clinical experience during LYRICA's premarketing development provides no direct means to assess its potential for inducing tumors in humans.
- In clinical studies across various patient populations, comprising 6396 patient-years of exposure in patients >12 years of age, new or worsening-preexisting tumors were reported in 57 patients. Without knowledge of the background incidence and recurrence in similar populations not treated with LYRICA, it is impossible to know whether the incidence seen in these cohorts is or is not affected by treatment.
- Ophthalmological Effects
- In controlled studies, a higher proportion of patients treated with LYRICA reported blurred vision (7%) than did patients treated with placebo (2%), which resolved in a majority of cases with continued dosing. Less than 1% of patients discontinued LYRICA treatment due to vision-related events (primarily blurred vision).
- Prospectively planned ophthalmologic testing, including visual acuity testing, formal visual field testing and dilated funduscopic examination, was performed in over 3600 patients. In these patients, visual acuity was reduced in 7% of patients treated with LYRICA, and 5% of placebo-treated patients. Visual field changes were detected in 13% of LYRICA-treated, and 12% of placebo-treated patients. Funduscopic changes were observed in 2% of LYRICA-treated and 2% of placebo-treated patients.
- Although the clinical significance of the ophthalmologic findings is unknown, inform patients to notify their physician if changes in vision occur. If visual disturbance persists, consider further assessment. Consider more frequent assessment for patients who are already routinely monitored for ocular conditions.
- Creatine Kinase Elevations
- LYRICA treatment was associated with creatine kinase elevations. Mean changes in creatine kinase from baseline to the maximum value were 60 U/L for LYRICA-treated patients and 28 U/L for the placebo patients. In all controlled trials across multiple patient populations, 1.5% of patients on LYRICA and 0.7% of placebo patients had a value of creatine kinase at least three times the upper limit of normal. Three LYRICA treated subjects had events reported as rhabdomyolysis in premarketing clinical trials. The relationship between these myopathy events and LYRICA is not completely understood because the cases had documented factors that may have caused or contributed to these events. Instruct patients to promptly report unexplained muscle pain, tenderness, or weakness, particularly if these muscle symptoms are accompanied by malaise or fever. Discontinue treatment with LYRICA if myopathy is diagnosed or suspected or if markedly elevated creatine kinase levels occur.
- Decreased Platelet Count
- LYRICA treatment was associated with a decrease in platelet count. LYRICA-treated subjects experienced a mean maximal decrease in platelet count of 20 × 103/µL, compared to 11 × 103/µL in placebo patients. In the overall database of controlled trials, 2% of placebo patients and 3% of LYRICA patients experienced a potentially clinically significant decrease in platelets, defined as 20% below baseline value and <<<150 × 103/µL. A single LYRICA treated subject developed severe thrombocytopenia with a platelet count less than 20 × 103/ µL. In randomized controlled trials, LYRICA was not associated with an increase in bleeding-related adverse reactions.
- PR Interval Prolongation
- LYRICA treatment was associated with PR interval prolongation. In analyses of clinical trial ECG data, the mean PR interval increase was 3–6 msec at LYRICA doses ≥300 mg/day. This mean change difference was not associated with an increased risk of PR increase ≥25% from baseline, an increased percentage of subjects with on-treatment PR >200 msec, or an increased risk of adverse reactions of second or third degree AV block.
- Subgroup analyses did not identify an increased risk of PR prolongation in patients with baseline PR prolongation or in patients taking other PR prolonging medications. However, these analyses cannot be considered definitive because of the limited number of patients in these categories.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- In all controlled and uncontrolled trials across various patient populations during the premarketing development of LYRICA, more than 10,000 patients have received LYRICA. Approximately 5000 patients were treated for 6 months or more, over 3100 patients were treated for 1 year or longer, and over 1400 patients were treated for at least 2 years.
- Adverse Reactions Most Commonly Leading to Discontinuation in All Premarketing Controlled Clinical Studies
- In premarketing controlled trials of all populations combined, 14% of patients treated with LYRICA and 7% of patients treated with placebo discontinued prematurely due to adverse reactions. In the LYRICA treatment group, the adverse reactions most frequently leading to discontinuation were dizziness (4%) and somnolence (4%). In the placebo group, 1% of patients withdrew due to dizziness and <1% withdrew due to somnolence. Other adverse reactions that led to discontinuation from controlled trials more frequently in the LYRICA group compared to the placebo group were ataxia, confusion, asthenia, thinking abnormal, blurred vision, incoordination, and peripheral edema (1% each).
- Most Common Adverse Reactions in All Premarketing Controlled Clinical Studies
- In premarketing controlled trials of all patient populations combined, dizziness, somnolence, dry mouth, edema, blurred vision, weight gain, and "thinking abnormal" (primarily difficulty with concentration/attention) were more commonly reported by subjects treated with LYRICA than by subjects treated with placebo (≥5% and twice the rate of that seen in placebo).
- Controlled Studies with Neuropathic Pain Associated with Diabetic Peripheral Neuropathy
- Adverse Reactions Leading to Discontinuation
- In clinical trials in patients with neuropathic pain associated with diabetic peripheral neuropathy, 9% of patients treated with LYRICA and 4% of patients treated with placebo discontinued prematurely due to adverse reactions. In the LYRICA treatment group, the most common reasons for discontinuation due to adverse reactions were dizziness (3%) and somnolence (2%). In comparison, <1% of placebo patients withdrew due to dizziness and somnolence. Other reasons for discontinuation from the trials, occurring with greater frequency in the LYRICA group than in the placebo group, were asthenia, confusion, and peripheral edema. Each of these events led to withdrawal in approximately 1% of patients.
- Most Common Adverse Reactions
- Table 3 lists all adverse reactions, regardless of causality, occurring in ≥1% of patients with neuropathic pain associated with diabetic neuropathy in the combined LYRICA group for which the incidence was greater in this combined LYRICA group than in the placebo group. A majority of pregabalin-treated patients in clinical studies had adverse reactions with a maximum intensity of "mild" or "moderate".
- Controlled Studies in Postherpetic Neuralgia
- Adverse Reactions Leading to Discontinuation
- In clinical trials in patients with postherpetic neuralgia, 14% of patients treated with LYRICA and 7% of patients treated with placebo discontinued prematurely due to adverse reactions. In the LYRICA treatment group, the most common reasons for discontinuation due to adverse reactions were dizziness (4%) and somnolence (3%). In comparison, less than 1% of placebo patients withdrew due to dizziness and somnolence. Other reasons for discontinuation from the trials, occurring in greater frequency in the LYRICA group than in the placebo group, were confusion (2%), as well as peripheral edema, asthenia, ataxia, and abnormal gait (1% each).
- Most Common Adverse Reactions
- Table 4 lists all adverse reactions, regardless of causality, occurring in ≥ 1% of patients with neuropathic pain associated with postherpetic neuralgia in the combined LYRICA group for which the incidence was greater in this combined LYRICA group than in the placebo group. In addition, an event is included, even if the incidence in the all LYRICA group is not greater than in the placebo group, if the incidence of the event in the 600 mg/day group is more than twice that in the placebo group. A majority of pregabalin-treated patients in clinical studies had adverse reactions with a maximum intensity of "mild" or "moderate". Overall, 12.4% of all pregabalin-treated patients and 9.0% of all placebo-treated patients had at least one severe event while 8% of pregabalin-treated patients and 4.3% of placebo-treated patients had at least one severe treatment-related adverse event.
- Controlled Add-On Studies in Adjunctive Therapy for Adult Patients with Partial Onset Seizures
- Adverse Reactions Leading to Discontinuation
- Approximately 15% of patients receiving LYRICA and 6% of patients receiving placebo in add-on epilepsy trials discontinued prematurely due to adverse reactions. In the LYRICA treatment group, the adverse reactions most frequently leading to discontinuation were dizziness (6%), ataxia (4%), and somnolence (3%). In comparison, <1% of patients in the placebo group withdrew due to each of these events. Other adverse reactions that led to discontinuation of at least 1% of patients in the LYRICA group and at least twice as frequently compared to the placebo group were asthenia, diplopia, blurred vision, thinking abnormal, nausea, tremor, vertigo, headache, and confusion (which each led to withdrawal in 2% or less of patients).
- Most Common Adverse Reactions
- Table 5 lists all dose-related adverse reactions occurring in at least 2% of all LYRICA-treated patients. Dose-relatedness was defined as the incidence of the adverse event in the 600 mg/day group was at least 2% greater than the rate in both the placebo and 150 mg/day groups. In these studies, 758 patients received LYRICA and 294 patients received placebo for up to 12 weeks. Because patients were also treated with 1 to 3 other AEDs, it is not possible to determine whether the following adverse reactions can be ascribed to LYRICA alone, or the combination of LYRICA and other AEDs. A majority of pregabalin-treated patients in clinical studies had adverse reactions with a maximum intensity of "mild" or "moderate".
- Controlled Studies with Fibromyalgia
- Adverse Reactions Leading to Discontinuation
- In clinical trials of patients with fibromyalgia, 19% of patients treated with pregabalin (150–600 mg/day) and 10% of patients treated with placebo discontinued prematurely due to adverse reactions. In the pregabalin treatment group, the most common reasons for discontinuation due to adverse reactions were dizziness (6%) and somnolence (3%). In comparison, <1% of placebo-treated patients withdrew due to dizziness and somnolence. Other reasons for discontinuation from the trials, occurring with greater frequency in the pregabalin treatment group than in the placebo treatment group, were fatigue, headache, balance disorder, and weight increased. Each of these adverse reactions led to withdrawal in approximately 1% of patients.
- Most Common Adverse Reactions
- Table 6 lists all adverse reactions, regardless of causality, occurring in ≥2% of patients with fibromyalgia in the 'all pregabalin' treatment group for which the incidence was greater than in the placebo treatment group. A majority of pregabalin-treated patients in clinical studies experienced adverse reactions with a maximum intensity of "mild" or "moderate".
- Controlled Studies in Neuropathic Pain Associated with Spinal Cord Injury
- Adverse Reactions Leading to Discontinuation
- In clinical trials of patients with neuropathic pain associated with spinal cord injury, 13% of patients treated with pregabalin and 10% of patients treated with placebo discontinued prematurely due to adverse reactions. In the pregabalin treatment group, the most common reasons for discontinuation due to adverse reactions were somnolence (3%) and edema (2%). In comparison, none of the placebo-treated patients withdrew due to somnolence and edema. Other reasons for discontinuation from the trials, occurring with greater frequency in the pregabalin treatment group than in the placebo treatment group, were fatigue and balance disorder. Each of these adverse reactions led to withdrawal in less than 2% of patients.
- Most Common Adverse Reactions
- Table 7 lists all adverse reactions, regardless of causality, occurring in ≥2% of patients with neuropathic pain associated with spinal cord injury in the controlled trials. A majority of pregabalin-treated patients in clinical studies experienced adverse reactions with a maximum intensity of "mild" or "moderate".
- Other Adverse Reactions Observed During the Clinical Studies of LYRICA
- Following is a list of treatment-emergent adverse reactions reported by patients treated with LYRICA during all clinical trials. The listing does not include those events already listed in the previous tables or elsewhere in labeling, those events for which a drug cause was remote, those events which were so general as to be uninformative, and those events reported only once which did not have a substantial probability of being acutely life-threatening.
- Events are categorized by body system and listed in order of decreasing frequency according to the following definitions: frequent adverse reactions are those occurring on one or more occasions in at least 1/100 patients; infrequent adverse reactions are those occurring in 1/100 to 1/1000 patients; rare reactions are those occurring in fewer than 1/1000 patients.
Body as a Whole
- Frequent: Abdominal pain, Allergic reaction, Fever, Infrequent: Abscess, Cellulitis, Chills, Malaise, Neck rigidity, Overdose, Pelvic pain, Photosensitivity reaction, Rare: Anaphylactoid reaction, Ascites, Granuloma, Hangover effect, Intentional Injury, Retroperitoneal Fibrosis, Shock
Cardiovascular System
- Infrequent: Deep thrombophlebitis, Heart failure, Hypotension, Postural hypotension, Retinal vascular disorder, Syncope; Rare: ST Depressed, Ventricular Fibrillation
Digestive System
- Frequent: Gastroenteritis, Increased appetite; Infrequent: Cholecystitis, Cholelithiasis, Colitis, Dysphagia, Esophagitis, Gastritis, Gastrointestinal hemorrhage, Melena, Mouth ulceration, Pancreatitis, Rectal hemorrhage, Tongue edema; Rare: Aphthous stomatitis, Esophageal Ulcer, Periodontal abscess
Hemic and Lymphatic System
- Frequent: Ecchymosis; Infrequent: Anemia, Eosinophilia, Hypochromic anemia, Leukocytosis, Leukopenia, Lymphadenopathy, Thrombocytopenia; Rare: Myelofibrosis, Polycythemia, Prothrombin decreased, Purpura, Thrombocythemia
Metabolic and Nutritional Disorders
- Rare: Glucose Tolerance Decreased, Urate Crystalluria
Musculoskeletal System
- Frequent: Arthralgia, Leg cramps, Myalgia, Myasthenia; Infrequent: Arthrosis; Rare: Chondrodystrophy, Generalized Spasm
Nervous System
- Frequent: Anxiety, Depersonalization, Hypertonia, Hypoesthesia, Libido decreased, Nystagmus, Paresthesia, Sedation, Stupor, Twitching; Infrequent: Abnormal dreams, Agitation, Apathy, Aphasia, Circumoral paresthesia, Dysarthria, Hallucinations, Hostility, Hyperalgesia, Hyperesthesia, Hyperkinesia, Hypokinesia, Hypotonia, Libido increased, Myoclonus, Neuralgia, Rare: Addiction, Cerebellar syndrome, Cogwheel rigidity, Coma, Delirium, Delusions, Dysautonomia, Dyskinesia, Dystonia, Encephalopathy, Extrapyramidal syndrome, Guillain-Barré syndrome, Hypalgesia, Intracranial hypertension, Manic reaction, Paranoid reaction, Peripheral neuritis, Personality disorder, Psychotic depression, Schizophrenic reaction, Sleep disorder, Torticollis, Trismus
Respiratory System
- Rare: Apnea, Atelectasis, Bronchiolitis, Hiccup, Laryngismus, Lung edema, Lung fibrosis, Yawn
Skin and Appendages
- Frequent: Pruritus, Infrequent: Alopecia, Dry skin, Eczema, Hirsutism, Skin ulcer, Urticaria, Vesiculobullous rash; Rare: Angioedema, Exfoliative dermatitis, Lichenoid dermatitis, Melanosis, Nail Disorder, Petechial rash, Purpuric rash, Pustular rash, Skin atrophy, Skin necrosis, Skin nodule, Stevens-Johnson syndrome, Subcutaneous nodule
Special senses
- Frequent: Conjunctivitis, Diplopia, Otitis media, Tinnitus; Infrequent: Abnormality of accommodation, Blepharitis, Dry eyes, Eye hemorrhage, Hyperacusis, Photophobia, Retinal edema, Taste loss, Taste perversion; Rare: Anisocoria, Blindness, Corneal ulcer, Exophthalmos, Extraocular palsy, Iritis, Keratitis, Keratoconjunctivitis, Miosis, Mydriasis, Night blindness, Ophthalmoplegia, Optic atrophy, Papilledema, Parosmia, Ptosis, Uveitis
Urogenital System
- Frequent: Anorgasmia, Impotence, Urinary frequency, Urinary incontinence; Infrequent: Abnormal ejaculation, Albuminuria, Amenorrhea, Dysmenorrhea, Dysuria, Hematuria, Kidney calculus, Leukorrhea, Menorrhagia, Metrorrhagia, Nephritis, Oliguria, Urinary retention, Urine abnormality; Rare: Acute kidney failure, Balanitis, Bladder Neoplasm, Cervicitis, Dyspareunia, Epididymitis, Female lactation, Glomerulitis, Ovarian disorder, Pyelonephritis
Comparison of Gender and Race
- The overall adverse event profile of pregabalin was similar between women and men. There are insufficient data to support a statement regarding the distribution of adverse experience reports by race.
Nervous System Disorders
Gastrointestinal Disorders
Reproductive System and Breast Disorders
- Gynecomastia, Breast Enlargement
Postmarketing Experience
- The following adverse reactions have been identified during postapproval use of LYRICA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- In addition, there are post-marketing reports of events related to reduced lower gastrointestinal tract function (e.g., intestinal obstruction, paralytic ileus, constipation) when LYRICA was co-administered with medications that have the potential to produce constipation, such as opioid analgesics. There are also post-marketing reports of respiratory failure and coma in patients taking pregabalin and other CNS depressant medications.
Drug Interactions
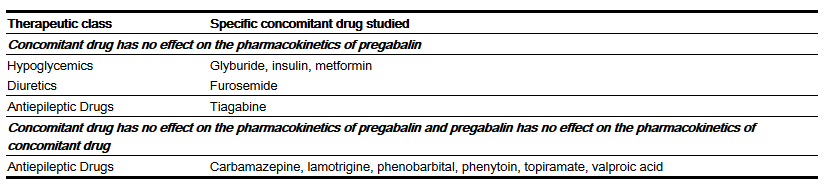
- Since LYRICA is predominantly excreted unchanged in the urine, undergoes negligible metabolism in humans (<2% of a dose recovered in urine as metabolites), and does not bind to plasma proteins, its pharmacokinetics are unlikely to be affected by other agents through metabolic interactions or protein binding displacement. In vitro and in vivo studies showed that LYRICA is unlikely to be involved in significant pharmacokinetic drug interactions. Specifically, there are no pharmacokinetic interactions between pregabalin and the following antiepileptic drugs: carbamazepine, valproic acid, lamotrigine, phenytoin, phenobarbital, and topiramate. Important pharmacokinetic interactions would also not be expected to occur between LYRICA and commonly used antiepileptic drugs.
- Pharmacodynamics
- Multiple oral doses of LYRICA were co-administered with oxycodone, lorazepam, or ethanol. Although no pharmacokinetic interactions were seen, additive effects on cognitive and gross motor functioning were seen when LYRICA was co-administered with these drugs. No clinically important effects on respiration were seen.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- Increased incidences of fetal structural abnormalities and other manifestations of developmental toxicity, including lethality, growth retardation, and nervous and reproductive system functional impairment, were observed in the offspring of rats and rabbits given pregabalin during pregnancy, at doses that produced plasma pregabalin exposures (AUC) ≥5 times human exposure at the maximum recommended dose (MRD) of 600 mg/day.
- When pregnant rats were given pregabalin (500, 1250, or 2500 mg/kg) orally throughout the period of organogenesis, incidences of specific skull alterations attributed to abnormally advanced ossification (premature fusion of the jugal and nasal sutures) were increased at ≥1250 mg/kg, and incidences of skeletal variations and retarded ossification were increased at all doses. Fetal body weights were decreased at the highest dose. The low dose in this study was associated with a plasma exposure (AUC) approximately 17 times human exposure at the MRD of 600 mg/day. A no-effect dose for rat embryo-fetal developmental toxicity was not established.
- When pregnant rabbits were given LYRICA (250, 500, or 1250 mg/kg) orally throughout the period of organogenesis, decreased fetal body weight and increased incidences of skeletal malformations, visceral variations, and retarded ossification were observed at the highest dose. The no-effect dose for developmental toxicity in rabbits (500 mg/kg) was associated with a plasma exposure approximately 16 times human exposure at the MRD.
- In a study in which female rats were dosed with LYRICA (50, 100, 250, 1250, or 2500 mg/kg) throughout gestation and lactation, offspring growth was reduced at ≥ 100 mg/kg and offspring survival was decreased at ≥250 mg/kg. The effect on offspring survival was pronounced at doses ≥1250 mg/kg, with 100% mortality in high-dose litters. When offspring were tested as adults, neurobehavioral abnormalities (decreased auditory startle responding) were observed at ≥250 mg/kg and reproductive impairment (decreased fertility and litter size) was seen at 1250 mg/kg. The no-effect dose for pre- and postnatal developmental toxicity in rats (50 mg/kg) produced a plasma exposure approximately 2 times human exposure at the MRD.
- There are no adequate and well-controlled studies in pregnant women. Use LYRICA during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- To provide information regarding the effects of in utero exposure to LYRICA, physicians are advised to recommend that pregnant patients taking LYRICA enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry. This can be done by calling the toll free number 1-888-233-2334, and must be done by patients themselves. Information on the registry can also be found at the website http://www.aedpregnancyregistry.org/.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Pregabalin in women who are pregnant.
Labor and Delivery
- The effects of LYRICA on labor and delivery in pregnant women are unknown. In the prenatal-postnatal study in rats, pregabalin prolonged gestation and induced dystocia at exposures ≥50 times the mean human exposure (AUC (0–24) of 123 µg∙hr/mL) at the maximum recommended clinical dose of 600 mg/day.
Nursing Mothers
- It is not known if pregabalin is excreted in human milk; it is, however, present in the milk of rats. Because many drugs are excreted in human milk, and because of the potential for tumorigenicity shown for pregabalin in animal studies, decide whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- The safety and efficacy of pregabalin in pediatric patients have not been established.
- In studies in which pregabalin (50 to 500 mg/kg) was orally administered to young rats from early in the postnatal period (Postnatal Day 7) through sexual maturity, neurobehavioral abnormalities (deficits in learning and memory, altered locomotor activity, decreased auditory startle responding and habituation) and reproductive impairment (delayed sexual maturation and decreased fertility in males and females) were observed at doses ≥50 mg/kg. The neurobehavioral changes of acoustic startle persisted at ≥250 mg/kg and locomotor activity and water maze performance at ≥500 mg/kg in animals tested after cessation of dosing and, thus, were considered to represent long-term effects. The low effect dose for developmental neurotoxicity and reproductive impairment in juvenile rats (50 mg/kg) was associated with a plasma pregabalin exposure (AUC) approximately equal to human exposure at the maximum recommended dose of 600 mg/day. A no-effect dose was not established.
Geriatic Use
- In controlled clinical studies of LYRICA in neuropathic pain associated with diabetic peripheral neuropathy, 246 patients were 65 to 74 years of age, and 73 patients were 75 years of age or older.
- In controlled clinical studies of LYRICA in neuropathic pain associated with postherpetic neuralgia, 282 patients were 65 to 74 years of age, and 379 patients were 75 years of age or older.
- In controlled clinical studies of LYRICA in epilepsy, there were only 10 patients 65 to 74 years of age, and 2 patients who were 75 years of age or older.
- No overall differences in safety and efficacy were observed between these patients and younger patients.
- In controlled clinical studies of LYRICA in fibromyalgia, 106 patients were 65 years of age or older. Although the adverse reaction profile was similar between the two age groups, the following neurological adverse reactions were more frequent in patients 65 years of age or older: dizziness, blurred vision, balance disorder, tremor, confusional state, coordination abnormal, and lethargy.
- LYRICA is known to be substantially excreted by the kidney, and the risk of toxic reactions to LYRICA may be greater in patients with impaired renal function. Because LYRICA is eliminated primarily by renal excretion, adjust the dose for elderly patients with renal impairment.
Gender
There is no FDA guidance on the use of Pregabalin with respect to specific gender populations.
Race
There is no FDA guidance on the use of Pregabalin with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Pregabalin in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Pregabalin in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Pregabalin in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Pregabalin in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Pregabalin in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Pregabalin in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- There is limited experience with overdose of LYRICA. The highest reported accidental overdose of LYRICA during the clinical development program was 8000 mg, and there were no notable clinical consequences.
Management
- There is no specific antidote for overdose with LYRICA. If indicated, elimination of unabsorbed drug may be attempted by emesis or gastric lavage; observe usual precautions to maintain the airway. General supportive care of the patient is indicated including monitoring of vital signs and observation of the clinical status of the patient. Contact a Certified Poison Control Center for up-to-date information on the management of overdose with LYRICA.
- Although hemodialysis has not been performed in the few known cases of overdose, it may be indicated by the patient's clinical state or in patients with significant renal impairment. Standard hemodialysis procedures result in significant clearance of pregabalin (approximately 50% in 4 hours).
Chronic Overdose
There is limited information regarding Chronic Overdose of Pregabalin in the drug label.
Pharmacology
| |
| |
Pregabalin
| |
| Systematic (IUPAC) name | |
| (S)-3-(aminomethyl)-5-methylhexanoic acid | |
| Identifiers | |
| CAS number | |
| ATC code | N03 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 159.23 g.mol-1 |
| SMILES | & |
| Synonyms | PD-144,723 |
| Pharmacokinetic data | |
| Bioavailability | ≥90% |
| Protein binding | Nil |
| Metabolism | Negligible |
| Half life | 5–6.5 hours |
| Excretion | Renal |
| Therapeutic considerations | |
| Pregnancy cat. | |
| Legal status |
Prescription Only (S4)(AU) POM (UK), Schedule V (U.S.) |
| Routes | oral |
Mechanism of Action
- LYRICA (pregabalin) binds with high affinity to the alpha2-delta site (an auxiliary subunit of voltage-gated calcium channels) in central nervous system tissues. Although the mechanism of action of pregabalin has not been fully elucidated, results with genetically modified mice and with compounds structurally related to pregabalin (such as gabapentin) suggest that binding to the alpha2-delta subunit may be involved in pregabalin's anti-nociceptive and antiseizure effects in animals. In animal models of nerve damage, pregabalin has been shown to reduce calcium-dependent release of pro-nociceptive neurotransmitters in the spinal cord, possibly by disrupting alpha2-delta containing-calcium channel trafficking and/or reducing calcium currents. Evidence from other animal models of nerve damage and persistent pain suggest the anti-nociceptive activities of pregabalin may also be mediated through interactions with descending noradrenergic and serotonergic pathways originating from the brainstem that modulate pain transmission in the spinal cord.
- While pregabalin is a structural derivative of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA), it does not bind directly to GABAA, GABAB, or benzodiazepine receptors, does not augment GABAA responses in cultured neurons, does not alter rat brain GABA concentration or have acute effects on GABA uptake or degradation. However, in cultured neurons prolonged application of pregabalin increases the density of GABA transporter protein and increases the rate of functional GABA transport. Pregabalin does not block sodium channels, is not active at opiate receptors, and does not alter cyclooxygenase enzyme activity. It is inactive at serotonin and dopamine receptors and does not inhibit dopamine, serotonin, or noradrenaline reuptake.
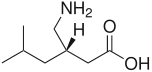
Structure
- Pregabalin is described chemically as (S)-3-(aminomethyl)-5-methylhexanoic acid. The molecular formula is C8H17NO2 and the molecular weight is 159.23. The chemical structure of pregabalin is:
- Pregabalin is a white to off-white, crystalline solid with a pKa1 of 4.2 and a pKa2 of 10.6. It is freely soluble in water and both basic and acidic aqueous solutions. The log of the partition coefficient (n-octanol/0.05M phosphate buffer) at pH 7.4 is – 1.35.
- LYRICA (pregabalin) Capsules are administered orally and are supplied as imprinted hard-shell capsules containing 25, 50, 75, 100, 150, 200, 225, and 300 mg of pregabalin, along with lactose monohydrate, cornstarch, and talc as inactive ingredients. The capsule shells contain gelatin and titanium dioxide. In addition, the orange capsule shells contain red iron oxide and the white capsule shells contain sodium lauryl sulfate and colloidal silicon dioxide. Colloidal silicon dioxide is a manufacturing aid that may or may not be present in the capsule shells. The imprinting ink contains shellac, black iron oxide, propylene glycol, and potassium hydroxide.
- LYRICA (pregabalin) oral solution, 20 mg/mL, is administered orally and is supplied as a clear, colorless solution contained in a 16 fluid ounce white HDPE bottle with a polyethylene-lined closure. The oral solution contains 20 mg/mL of pregabalin, along with methylparaben, propylparaben, monobasic sodium phosphate anhydrous, dibasic sodium phosphate anhydrous, sucralose, artificial strawberry #11545 and purified water as inactive ingredients.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Pregabalin in the drug label.
Pharmacokinetics
- Pregabalin is well absorbed after oral administration, is eliminated largely by renal excretion, and has an elimination half-life of about 6 hours.
- Absorption and Distribution
- Following oral administration of LYRICA capsules under fasting conditions, peak plasma concentrations occur within 1.5 hours. Pregabalin oral bioavailability is ≥90% and is independent of dose. Following single- (25 to 300 mg) and multiple- dose (75 to 900 mg/day) administration, maximum plasma concentrations (Cmax) and area under the plasma concentration-time curve (AUC) values increase linearly. Following repeated administration, steady state is achieved within 24 to 48 hours. Multiple-dose pharmacokinetics can be predicted from single-dose data.
- The rate of pregabalin absorption is decreased when given with food, resulting in a decrease in Cmax of approximately 25% to 30% and an increase in Tmax to approximately 3 hours. However, administration of pregabalin with food has no clinically relevant effect on the total absorption of pregabalin. Therefore, pregabalin can be taken with or without food.
- Pregabalin does not bind to plasma proteins. The apparent volume of distribution of pregabalin following oral administration is approximately 0.5 L/kg. Pregabalin is a substrate for system L transporter which is responsible for the transport of large amino acids across the blood brain barrier. Although there are no data in humans, pregabalin has been shown to cross the blood brain barrier in mice, rats, and monkeys. In addition, pregabalin has been shown to cross the placenta in rats and is present in the milk of lactating rats.
- Metabolism and Elimination
- Pregabalin undergoes negligible metabolism in humans. Following a dose of radiolabeled pregabalin, approximately 90% of the administered dose was recovered in the urine as unchanged pregabalin. The N-methylated derivative of pregabalin, the major metabolite of pregabalin found in urine, accounted for 0.9% of the dose. In preclinical studies, pregabalin (S-enantiomer) did not undergo racemization to the R-enantiomer in mice, rats, rabbits, or monkeys.
- Pregabalin is eliminated from the systemic circulation primarily by renal excretion as unchanged drug with a mean elimination half-life of 6.3 hours in subjects with normal renal function. Mean renal clearance was estimated to be 67.0 to 80.9 mL/min in young healthy subjects. Because pregabalin is not bound to plasma proteins this clearance rate indicates that renal tubular reabsorption is involved. Pregabalin elimination is nearly proportional to creatinine clearance (CLcr).
- Pharmacokinetics in Special Populations
- Race
- In population pharmacokinetic analyses of the clinical studies in various populations, the pharmacokinetics of LYRICA were not significantly affected by race (Caucasians, Blacks, and Hispanics).
- Gender
- Population pharmacokinetic analyses of the clinical studies showed that the relationship between daily dose and LYRICA drug exposure is similar between genders.
- Renal Impairment and Hemodialysis
- Pregabalin clearance is nearly proportional to creatinine clearance (CLcr). Dosage reduction in patients with renal dysfunction is necessary. Pregabalin is effectively removed from plasma by hemodialysis. Following a 4-hour hemodialysis treatment, plasma pregabalin concentrations are reduced by approximately 50%. For patients on hemodialysis, dosing must be modified.
- Elderly
- Pregabalin oral clearance tended to decrease with increasing age. This decrease in pregabalin oral clearance is consistent with age-related decreases in CLcr. Reduction of pregabalin dose may be required in patients who have age-related compromised renal function.
- Pediatric Pharmacokinetics
- Pharmacokinetics of pregabalin have not been adequately studied in pediatric patients.
- Drug Interactions
- In Vitro Studies
- Pregabalin, at concentrations that were, in general, 10-times those attained in clinical trials, does not inhibit human CYP1A2, CYP2A6, CYP2C9, CYP2C19, CYP2D6, CYP2E1, and CYP3A4 enzyme systems. In vitro drug interaction studies demonstrate that pregabalin does not induce CYP1A2 or CYP3A4 activity. Therefore, an increase in the metabolism of coadministered CYP1A2 substrates (e.g. theophylline, caffeine) or CYP 3A4 substrates (e.g., midazolam, testosterone) is not anticipated.
- In Vitro Studies
- In Vivo Studies
- The drug interaction studies described in this section were conducted in healthy adults, and across various patient populations.
- In Vivo Studies
- Gabapentin
- The pharmacokinetic interactions of pregabalin and gabapentin were investigated in 12 healthy subjects following concomitant single-dose administration of 100-mg pregabalin and 300-mg gabapentin and in 18 healthy subjects following concomitant multiple-dose administration of 200-mg pregabalin every 8 hours and 400-mg gabapentin every 8 hours. Gabapentin pharmacokinetics following single- and multiple-dose administration were unaltered by pregabalin coadministration. The extent of pregabalin absorption was unaffected by gabapentin coadministration, although there was a small reduction in rate of absorption.
- Pregabalin coadministration (200 mg three times a day) had no effect on the steady-state pharmacokinetics of norethindrone and ethinyl estradiol (1 mg/35 µg, respectively) in healthy subjects.
- Multiple-dose administration of pregabalin (300 mg twice a day) in healthy subjects had no effect on the rate and extent of lorazepam single-dose pharmacokinetics and single-dose administration of lorazepam (1 mg) had no effect on the steady-state pharmacokinetics of pregabalin.
- Multiple-dose administration of pregabalin (300 mg twice a day) in healthy subjects had no effect on the rate and extent of oxycodone single-dose pharmacokinetics. Single-dose administration of oxycodone (10 mg) had no effect on the steady-state pharmacokinetics of pregabalin.
- Ethanol
- Multiple-dose administration of pregabalin (300 mg twice a day) in healthy subjects had no effect on the rate and extent of ethanol single-dose pharmacokinetics and single-dose administration of ethanol (0.7 g/kg) had no effect on the steady-state pharmacokinetics of pregabalin.
- Steady-state trough plasma concentrations of phenytoin, carbamazepine and carbamazepine 10,11 epoxide, valproic acid, and lamotrigine were not affected by concomitant pregabalin (200 mg three times a day) administration.
- Population pharmacokinetic analyses in patients treated with pregabalin and various concomitant medications suggest the following:
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenesis
- A dose-dependent increase in the incidence of malignant vascular tumors (hemangiosarcomas) was observed in two strains of mice (B6C3F1 and CD-1) given pregabalin (200, 1000, or 5000 mg/kg) in the diet for two years. Plasma pregabalin exposure (AUC) in mice receiving the lowest dose that increased hemangiosarcomas was approximately equal to the human exposure at the maximum recommended dose (MRD) of 600 mg/day. A no-effect dose for induction of hemangiosarcomas in mice was not established. No evidence of carcinogenicity was seen in two studies in Wistar rats following dietary administration of pregabalin for two years at doses (50, 150, or 450 mg/kg in males and 100, 300, or 900 mg/kg in females) that were associated with plasma exposures in males and females up to approximately 14 and 24 times, respectively, human exposure at the MRD.
- Mutagenesis
- Pregabalin was not mutagenic in bacteria or in mammalian cells in vitro, was not clastogenic in mammalian systems in vitro and in vivo, and did not induce unscheduled DNA synthesis in mouse or rat hepatocytes.
- Impairment of Fertility
- In fertility studies in which male rats were orally administered pregabalin (50 to 2500 mg/kg) prior to and during mating with untreated females, a number of adverse reproductive and developmental effects were observed. These included decreased sperm counts and sperm motility, increased sperm abnormalities, reduced fertility, increased preimplantation embryo loss, decreased litter size, decreased fetal body weights, and an increased incidence of fetal abnormalities.
- Effects on sperm and fertility parameters were reversible in studies of this duration (3–4 months). The no-effect dose for male reproductive toxicity in these studies (100 mg/kg) was associated with a plasma pregabalin exposure (AUC) approximately 3 times human exposure at the maximum recommended dose (MRD) of 600 mg/day.
- In addition, adverse reactions on reproductive organ (testes, epididymides) histopathology were observed in male rats exposed to pregabalin (500 to 1250 mg/kg) in general toxicology studies of four weeks or greater duration. The no-effect dose for male reproductive organ histopathology in rats (250 mg/kg) was associated with a plasma exposure approximately 8 times human exposure at the MRD.
- In a fertility study in which female rats were given pregabalin (500, 1250, or 2500 mg/kg) orally prior to and during mating and early gestation, disrupted estrous cyclicity and an increased number of days to mating were seen at all doses, and embryolethality occurred at the highest dose. The low dose in this study produced a plasma exposure approximately 9 times that in humans receiving the MRD. A no-effect dose for female reproductive toxicity in rats was not established.
- Human Data
- In a double-blind, placebo-controlled clinical trial to assess the effect of pregabalin on sperm motility, 30 healthy male subjects were exposed to pregabalin at a dose of 600 mg/day. After 3 months of treatment (one complete sperm cycle), the difference between placebo- and pregabalin-treated subjects in mean percent sperm with normal motility was <4% and neither group had a mean change from baseline of more than 2%. Effects on other male reproductive parameters in humans have not been adequately studied.
Animal Toxicology and/or Pharmacology
- Dermatopathy
- Skin lesions ranging from erythema to necrosis were seen in repeated-dose toxicology studies in both rats and monkeys. The etiology of these skin lesions is unknown. At the maximum recommended human dose (MRD) of 600 mg/day, there is a 2-fold safety margin for the dermatological lesions. The more severe dermatopathies involving necrosis were associated with pregabalin exposures (as expressed by plasma AUCs) of approximately 3 to 8 times those achieved in humans given the MRD. No increase in incidence of skin lesions was observed in clinical studies.
- Ocular Lesions
- Ocular lesions (characterized by retinal atrophy [including loss of photoreceptor cells] and/or corneal inflammation/mineralization) were observed in two lifetime carcinogenicity studies in Wistar rats. These findings were observed at plasma pregabalin exposures (AUC) ≥2 times those achieved in humans given the maximum recommended dose of 600 mg/day. A no-effect dose for ocular lesions was not established. Similar lesions were not observed in lifetime carcinogenicity studies in two strains of mice or in monkeys treated for 1 year.
Clinical Studies
Neuropathic Pain Associated with Diabetic Peripheral Neuropathy
- The efficacy of the maximum recommended dose of LYRICA for the management of neuropathic pain associated with diabetic peripheral neuropathy was established in three double-blind, placebo-controlled, multicenter studies with three times a day dosing, two of which studied the maximum recommended dose. Patients were enrolled with either Type 1 or Type 2 diabetes mellitus and a diagnosis of painful distal symmetrical sensorimotor polyneuropathy for 1 to 5 years. A total of 89% of patients completed Studies DPN 1 and DPN 2. The patients had a minimum mean baseline pain score of ≥4 on an 11-point numerical pain rating scale ranging from 0 (no pain) to 10 (worst possible pain). The baseline mean pain scores across the two studies ranged from 6.1 to 6.7. Patients were permitted up to 4 grams of acetaminophen per day as needed for pain, in addition to pregabalin. Patients recorded their pain daily in a diary.
- Study DPN 1: This 5-week study compared LYRICA 25, 100, or 200 mg three times a day with placebo. Treatment with LYRICA 100 and 200 mg three times a day statistically significantly improved the endpoint mean pain score and increased the proportion of patients with at least a 50% reduction in pain score from baseline. There was no evidence of a greater effect on pain scores of the 200 mg three times a day dose than the 100 mg three times a day dose, but there was evidence of dose dependent adverse reactions. For a range of levels of improvement in pain intensity from baseline to study endpoint, Figure 1 shows the fraction of patients achieving that level of improvement. The figure is cumulative, so that patients whose change from baseline is, for example, 50%, are also included at every level of improvement below 50%. Patients who did not complete the study were assigned 0% improvement. Some patients experienced a decrease in pain as early as Week 1, which persisted throughout the study.
- Figure 1: Patients Achieving Various Levels of Improvement in Pain Intensity – Study DPN 1
- Study DPN 2: This 8-week study compared LYRICA 100 mg three times a day with placebo. Treatment with LYRICA 100 mg three times a day statistically significantly improved the endpoint mean pain score and increased the proportion of patients with at least a 50% reduction in pain score from baseline. For various levels of improvement in pain intensity from baseline to study endpoint, Figure 2 shows the fraction of patients achieving that level of improvement. The figure is cumulative, so that patients whose change from baseline is, for example, 50%, are also included at every level of improvement below 50%. Patients who did not complete the study were assigned 0% improvement. Some patients experienced a decrease in pain as early as Week 1, which persisted throughout the study.
- Figure 2: Patients Achieving Various Levels of Improvement in Pain Intensity–Study DPN 2
Postherpetic Neuralgia
- The efficacy of LYRICA for the management of postherpetic neuralgia was established in three double-blind, placebo-controlled, multicenter studies. These studies enrolled patients with neuralgia persisting for at least 3 months following healing of herpes zoster rash and a minimum baseline score of ≥4 on an 11-point numerical pain rating scale ranging from 0 (no pain) to 10 (worst possible pain). Seventy-three percent of patients completed the studies. The baseline mean pain scores across the 3 studies ranged from 6 to 7. Patients were permitted up to 4 grams of acetaminophen per day as needed for pain, in addition to pregabalin. Patients recorded their pain daily in a diary.
- Study PHN 1: This 13-week study compared LYRICA 75, 150, and 300 mg twice daily with placebo. Patients with creatinine clearance (CLcr) between 30 to 60 mL/min were randomized to 75 mg, 150 mg, or placebo twice daily. Patients with creatinine clearance greater than 60 mL/min were randomized to 75 mg, 150 mg, 300 mg or placebo twice daily. In patients with creatinine clearance greater than 60 mL/min treatment with all doses of LYRICA statistically significantly improved the endpoint mean pain score and increased the proportion of patients with at least a 50% reduction in pain score from baseline. Despite differences in dosing based on renal function, patients with creatinine clearance between 30 to 60 mL/min tolerated LYRICA less well than patients with creatinine clearance greater than 60 mL/min as evidenced by higher rates of discontinuation due to adverse reactions. For various levels of improvement in pain intensity from baseline to study endpoint, Figure 3 shows the fraction of patients achieving that level of improvement. The figure is cumulative, so that patients whose change from baseline is, for example, 50%, are also included at every level of improvement below 50%. Patients who did not complete the study were assigned 0% improvement. Some patients experienced a decrease in pain as early as Week 1, which persisted throughout the study.
- Figure 3: Patients Achieving Various Levels of Improvement in Pain Intensity– Study PHN 1
- Study PHN 2: This 8-week study compared LYRICA 100 or 200 mg three times a day with placebo, with doses assigned based on creatinine clearance. Patients with creatinine clearance between 30 to 60 mL/min were treated with 100 mg three times a day, and patients with creatinine clearance greater than 60 mL/min were treated with 200 mg three times daily. Treatment with LYRICA statistically significantly improved the endpoint mean pain score and increased the proportion of patients with at least a 50% reduction in pain score from baseline. For various levels of improvement in pain intensity from baseline to study endpoint, Figure 4 shows the fraction of patients achieving those levels of improvement. The figure is cumulative, so that patients whose change from baseline is, for example, 50%, are also included at every level of improvement below 50%. Patients who did not complete the study were assigned 0% improvement. Some patients experienced a decrease in pain as early as Week 1, which persisted throughout the study.
- Figure 4: Patients Achieving Various Levels of Improvement in Pain Intensity – Study PHN 2
- Study PHN 3: This 8-week study compared LYRICA 50 or 100 mg three times a day with placebo with doses assigned regardless of creatinine clearance. Treatment with LYRICA 50 and 100 mg three times a day statistically significantly improved the endpoint mean pain score and increased the proportion of patients with at least a 50% reduction in pain score from baseline. Patients with creatinine clearance between 30 to 60 mL/min tolerated LYRICA less well than patients with creatinine clearance greater than 60 mL/min as evidenced by markedly higher rates of discontinuation due to adverse reactions. For various levels of improvement in pain intensity from baseline to study endpoint, Figure 5 shows the fraction of patients achieving that level of improvement. The figure is cumulative, so that patients whose change from baseline is, for example, 50%, are also included at every level of improvement below 50%. Patients who did not complete the study were assigned 0% improvement. Some patients experienced a decrease in pain as early as Week 1, which persisted throughout the study.
- Figure 5: Patients Achieving Various Levels of Improvement in Pain Intensity– Study PHN 3
Adjunctive Therapy for Adult Patients with Partial Onset Seizures
- The efficacy of LYRICA as adjunctive therapy in partial onset seizures was established in three 12-week, randomized, double-blind, placebo-controlled, multicenter studies in adult patients. Patients were enrolled who had partial onset seizures with or without secondary generalization and were not adequately controlled with 1 to 3 concomitant antiepileptic drugs (AEDs). Patients taking gabapentin were required to discontinue gabapentin treatment 1 week prior to entering baseline. During an 8-week baseline period, patients had to experience at least 6 partial onset seizures with no seizure-free period exceeding 4 weeks. The mean duration of epilepsy was 25 years in these 3 studies and the mean and median baseline seizure frequencies were 22.5 and 10 seizures per month, respectively. Approximately half of the patients were taking 2 concurrent AEDs at baseline. Among the LYRICA-treated patients, 80% completed the double-blind phase of the studies.
- Table 8 shows median baseline seizure rates and median percent reduction in seizure frequency by dose.
- In the first study (E1), there was evidence of a dose-response relationship for total daily doses of Lyrica between 150 and 600 mg/day; a dose of 50 mg/day was not effective. In the first study (E1), each daily dose was divided into two equal doses (twice a day dosing). In the second study (E2), each daily dose was divided into three equal doses (three times a day dosing). In the third study (E3), the same total daily dose was divided into two equal doses for one group (twice a day dosing) and three equal doses for another group (three times a day dosing). While the three times a day dosing group in Study E3 performed numerically better than the twice a day dosing group, this difference was small and not statistically significant.
- A secondary outcome measure included the responder rate (proportion of patients with ≥50% reduction from baseline in partial seizure frequency). The following figure displays responder rate by dose for two of the studies.
- Subset evaluations of the antiseizure efficacy of LYRICA showed no clinically important differences as a function of age, gender, or race.
Management of Fibromyalgia
- The efficacy of LYRICA for management of fibromyalgia was established in one 14-week, double-blind, placebo-controlled, multicenter study (F1) and one six-month, randomized withdrawal study (F2). Studies F1 and F2 enrolled patients with a diagnosis of fibromyalgia using the American College of Rheumatology (ACR) criteria (history of widespread pain for 3 months, and pain present at 11 or more of the 18 specific tender point sites). The studies showed a reduction in pain by visual analog scale. In addition, improvement was demonstrated based on a patient global assessment (PGIC), and on the Fibromyalgia Impact Questionnaire (FIQ).
- Study F1: This 14-week study compared LYRICA total daily doses of 300 mg, 450 mg and 600 mg with placebo. Patients were enrolled with a minimum mean baseline pain score of greater than or equal to 4 on an 11-point numeric pain rating scale and a score of greater than or equal to 40 mm on the 100 mm pain visual analog scale (VAS). The baseline mean pain score in this trial was 6.7. Responders to placebo in an initial one-week run-in phase were not randomized into subsequent phases of the study. A total of 64% of patients randomized to LYRICA completed the study. There was no evidence of a greater effect on pain scores of the 600 mg daily dose than the 450 mg daily dose, but there was evidence of dose-dependent adverse reactions. Some patients experienced a decrease in pain as early as Week 1, which persisted throughout the study. The results are summarized in Figure 8 and Table 9.
- For various levels of improvement in pain intensity from baseline to study endpoint, Figure 8 shows the fraction of patients achieving that level of improvement. The figure is cumulative. Patients who did not complete the study were assigned 0% improvement. Some patients experienced a decrease in pain as early as Week 1, which persisted throughout the study.
- Figure 8: Patients Achieving Various Levels of Improvement in Pain Intensity – Fibromyalgia Study F1
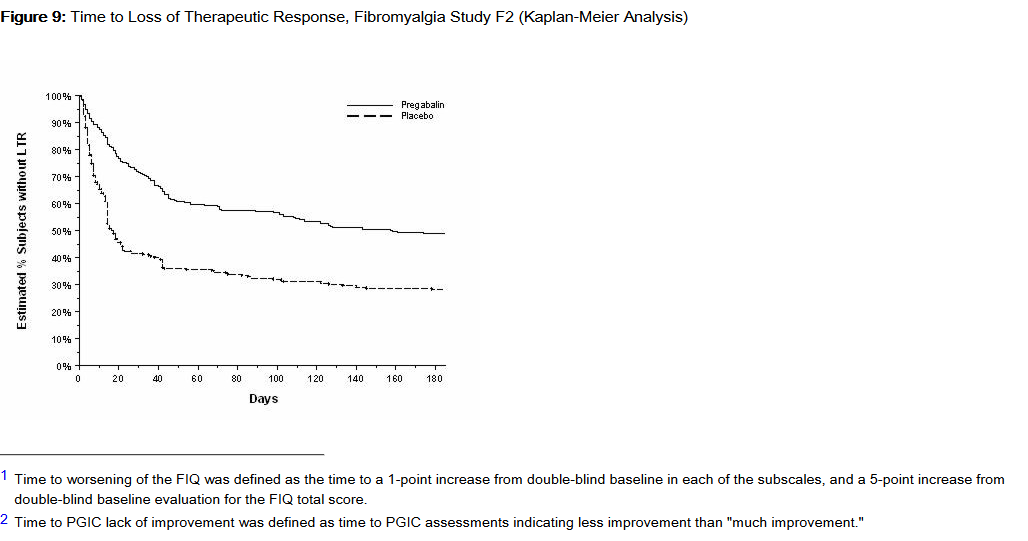
- Study F2: This randomized withdrawal study compared LYRICA with placebo. Patients were titrated during a 6-week open-label dose optimization phase to a total daily dose of 300 mg, 450 mg, or 600 mg. Patients were considered to be responders if they had both: 1) at least a 50% reduction in pain (VAS) and, 2) rated their overall improvement on the PGIC as "much improved" or "very much improved." Those who responded to treatment were then randomized in the double-blind treatment phase to either the dose achieved in the open-label phase or to placebo. Patients were treated for up to 6 months following randomization. Efficacy was assessed by time to loss of therapeutic response, defined as 1) less than 30% reduction in pain (VAS) from open-label baseline during two consecutive visits of the double-blind phase, or 2) worsening of FM symptoms necessitating an alternative treatment. Fifty-four percent of patients were able to titrate to an effective and tolerable dose of LYRICA during the 6-week open-label phase. Of the patients entering the randomized treatment phase assigned to remain on LYRICA, 38% of patients completed 26 weeks of treatment versus 19% of placebo-treated patients.
- When considering return of pain or withdrawal due to adverse events as loss of response (LTR), treatment with LYRICA resulted in a longer time to loss of therapeutic response than treatment with placebo. Fifty-three percent of the pregabalin-treated subjects compared to 33% of placebo patients remained on study drug and maintained a therapeutic response to Week 26 of the study. Treatment with LYRICA also resulted in a longer time to loss of response based on the FIQ1, and longer time to loss of overall assessment of patient status, as measured by the PGIC2.
- Figure 9: Time to Loss of Therapeutic Response, Fibromyalgia Study F2 (Kaplan-Meier Analysis)
Management of Neuropathic Pain Associated with Spinal Cord Injury
- The efficacy of LYRICA for the management of neuropathic pain associated with spinal cord injury was established in two double-blind, placebo-controlled, multicenter studies. Patients were enrolled with neuropathic pain associated with spinal cord injury that persisted continuously for at least three months or with relapses and remissions for at least six months. A total of 63% of patients completed study 1 and 84% completed study 2. The patients had a minimum mean baseline pain score of ≥4 on an 11-point numerical pain rating scale ranging from 0 (no pain) to 10 (worst possible pain). The baseline mean pain scores across the two studies ranged from 6.5 to 6.7.
- Patients were allowed to take opioids, non-opioid analgesics, antiepileptic drugs, muscle relaxants, and antidepressant drugs if the dose was stable for 30 days prior to screening. Patients were allowed to take acetaminophen and nonsteroidal anti-inflammatory drugs during the studies.
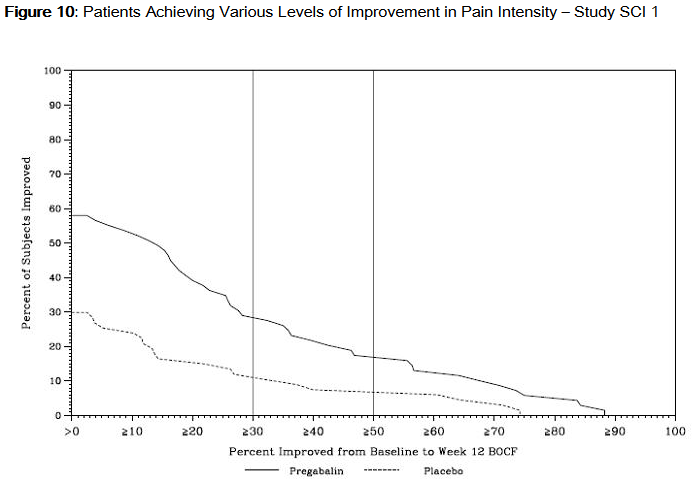
- Study SCI 1: This 12-week, randomized, double-blind, parallel-group, multicenter, flexible dose (150–600 mg/day) study compared pregabalin with placebo. The 12-week study consisted of a 3-week dose adjustment phase and a 9-week dose maintenance phase. Treatment with LYRICA 150–600 mg/day statistically significantly improved the endpoint weekly mean pain score, and increased the proportion of patients with at least a 30% and 50% reduction in pain score from baseline. The fraction of patients achieving various levels of improvement in pain intensity from baseline to Week 12 is presented in Figure 10. Some patients experienced a decrease in pain as early as week 1, which persisted throughout the study.
- Figure 10: Patients Achieving Various Levels of Improvement in Pain Intensity – Study SCI 1
- Study SCI 2: This 16-week, randomized, double-blind, placebo-controlled, parallel-group, multicenter, flexible dose (150–600 mg/day, in increments of 150 mg) study compared the efficacy, safety and tolerability of pregabalin with placebo. The 16-week study consisted of a 4-week dose adjustment phase and a 12-week dose maintenance phase. Treatment with LYRICA statistically significantly improved the endpoint weekly mean pain score, and increased the proportion of patients with at least a 30% and 50% reduction in pain score from baseline. The fraction of patients achieving various levels of improvement in pain intensity from baseline to Week 16 is presented in Figure 11. Some patients experienced a decrease in pain as early as week 1, which persisted throughout the study.
- Figure 11: Patients Achieving Various Levels of Improvement in Pain Intensity – Study SCI 2
How Supplied
- 25 mg capsules:
- White, hard-gelatin capsule printed with black ink "Pfizer" on the cap, "PGN 25" on the body; available in:
- Bottles of 90: NDC 0071-1012-68
- 50 mg capsules:
- White, hard-gelatin capsule printed with black ink "Pfizer" on the cap, "PGN 50" and an ink band on the body, available in:
- Bottles of 90: NDC 0071-1013-68
- Unit-Dose Blister Packages of 100: NDC 0071-1013-41
- 75 mg capsules:
- White/orange hard gelatin capsule printed with black ink "Pfizer" on the cap, "PGN 75" on the body; available in:
- Bottles of 90: NDC 0071-1014-68
- Unit-Dose Blister Packages of 100: NDC 0071-1014-41
- 100 mg capsules:
- Orange, hard-gelatin capsule printed with black ink "Pfizer" on the cap, "PGN 100" on the body, available in:
- Bottles of 90: NDC 0071-1015-68
- Unit-Dose Blister Packages of 100: NDC 0071-1015-41
- 150 mg capsules:
- White hard gelatin capsule printed with black ink "Pfizer" on the cap, "PGN 150" on the body, available in:
- Bottles of 90: NDC 0071-1016-68
- Unit-Dose Blister Packages of 100: NDC 0071-1016-41
- 200 mg capsules:
- Light orange hard gelatin capsule printed with black ink "Pfizer" on the cap, "PGN 200" on the body, available in:
- Bottles of 90: NDC 0071-1017-68
- 225 mg capsules:
- White/light orange hard gelatin capsule printed with black ink "Pfizer" on the cap, "PGN 225" on the body; available in:
- Bottles of 90: NDC 0071-1019-68
- 300 mg capsules:
- White/orange hard gelatin capsule printed with black ink "Pfizer" on the cap, "PGN 300" on the body, available in:
- Bottles of 90: NDC 0071-1018-68
- 20 mg/mL oral solution:
- 16 fluid ounce white high density polyethylene (HDPE) bottle with a polyethylene-lined closure:
- 16 fluid ounce bottle NDC 0071-1020-01
- Storage and Handling
- Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Storage
There is limited information regarding Pregabalin Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Pregabalin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Pregabalin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Medication Guide
- Inform patients of the availability of a Medication Guide, and instruct them to read the Medication Guide prior to taking LYRICA. Instruct patients to take LYRICA only as prescribed.
- Angioedema
- Advise patients that LYRICA may cause angioedema, with swelling of the face, mouth (lip, gum, tongue) and neck (larynx and pharynx) that can lead to life-threatening respiratory compromise. Instruct patients to discontinue LYRICA and immediately seek medical care if they experience these symptoms.
- Hypersensitivity
- Advise patients that LYRICA has been associated with hypersensitivity reactions such as wheezing, dyspnea, rash, hives, and blisters. Instruct patients to discontinue LYRICA and immediately seek medical care if they experience these symptoms.
- Suicidal Thinking and Behavior
- Patients, their caregivers, and families should be counseled that AEDs, including LYRICA, may increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Report behaviors of concern immediately to healthcare providers.
- Dizziness and Somnolence
- Counsel patients that LYRICA may cause dizziness, somnolence, blurred vision and other CNS signs and symptoms. Accordingly, advise patients not to drive, operate complex machinery, or engage in other hazardous activities until they have gained sufficient experience on LYRICA to gauge whether or not it affects their mental, visual, and/or motor performance adversely.
- Weight Gain and Edema
- Counsel patients that LYRICA may cause edema and weight gain. Advise patients that concomitant treatment with LYRICA and a thiazolidinedione antidiabetic agent may lead to an additive effect on edema and weight gain. For patients with preexisting cardiac conditions, this may increase the risk of heart failure.
- Abrupt or Rapid Discontinuation
- Advise patients to take LYRICA as prescribed. Abrupt or rapid discontinuation may result in insomnia, nausea, headache, anxiety, hyperhidrosis, or diarrhea.
- Ophthalmological Effects
- Counsel patients that LYRICA may cause visual disturbances. Inform patients that if changes in vision occur, they should notify their physician.
- Creatine Kinase Elevations
- CNS Depressants
- Inform patients who require concomitant treatment with central nervous system depressants such as opiates or benzodiazepines that they may experience additive CNS side effects, such as somnolence.
- Alcohol
- Tell patients to avoid consuming alcohol while taking LYRICA, as LYRICA may potentiate the impairment of motor skills and sedating effects of alcohol.
- Use in Pregnancy
- Instruct patients to notify their physician if they become pregnant or intend to become pregnant during therapy, and to notify their physician if they are breast feeding or intend to breast feed during therapy.
- Encourage patients to enroll in the NAAED Pregnancy Registry if they become pregnant. This registry is collecting information about the safety of antiepileptic drugs during pregnancy. To enroll, patients can call the toll free number 1-888-233-2334.
- Male Fertility
- Inform men being treated with LYRICA who plan to father a child of the potential risk of male-mediated teratogenicity. In preclinical studies in rats, pregabalin was associated with an increased risk of male-mediated teratogenicity. The clinical significance of this finding is uncertain.
- Dermatopathy
- Instruct diabetic patients to pay particular attention to skin integrity while being treated with LYRICA. Some animals treated with pregabalin developed skin ulcerations, although no increased incidence of skin lesions associated with LYRICA was observed in clinical trials.
MEDICATION GUIDE
LYRICA (LEER-i-kah)
(pregabalin)
- Capsules and Oral Solution, CV
- Read this Medication Guide before you start taking LYRICA and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment. If you have any questions about LYRICA, ask your healthcare provider or pharmacist.
- What is the most important information I should know about LYRICA?
- LYRICA may cause serious side effects including:
- Serious, even life-threatening, allergic reactions
- Suicidal thoughts or actions
- Swelling of your hands, legs and feet
- Dizziness and sleepiness
- These serious side effects are described below:
- Serious, even life-threatening, allergic reactions.
- Stop taking LYRICA and call your healthcare provider right away if you have any of these signs of a serious allergic reaction:
- swelling of your face, mouth, lips, gums, tongue, throat or neck
- trouble breathing
- rash, hives (raised bumps) or blisters
- Serious, even life-threatening, allergic reactions.
- Like other antiepileptic drugs, LYRICA may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
- Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
- If you have suicidal thoughts or actions, do not stop LYRICA without first talking to a healthcare provider.
- Stopping LYRICA suddenly can cause serious problems.
- Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
- How can I watch for early symptoms of suicidal thoughts and actions?
- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
- Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
- Swelling of your hands, legs and feet. This swelling can be a serious problem for people with heart problems.
- Dizziness and sleepiness.
- Do not drive a car, work with machines, or do other dangerous activities until you know how LYRICA affects you. Ask your healthcare provider about when it will be okay to do these activities.
- Like other antiepileptic drugs, LYRICA may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
- What is LYRICA?
- LYRICA is a prescription medicine used in adults, 18 years and older, to treat:
- pain from damaged nerves (neuropathic pain) that happens with diabetes
- pain from damaged nerves (neuropathic pain) that follows healing of shingles
- partial seizures when taken together with other seizure medicines
- fibromyalgia (pain all over your body)
- pain from damaged nerves (neuropathic pain) that follows spinal cord injury
- LYRICA has not been studied in children under 18 years of age.
- LYRICA is a prescription medicine used in adults, 18 years and older, to treat:
- Who Should Not Take LYRICA?
- Do not take LYRICA if you are allergic to pregabalin or any of the ingredients in LYRICA.
- See "What is the most important information I should know about LYRICA?" for the signs of an allergic reaction.
- See the end of this leaflet for a complete list of ingredients in LYRICA.
- Do not take LYRICA if you are allergic to pregabalin or any of the ingredients in LYRICA.
- What should I tell my healthcare provider before taking LYRICA?
- Before taking LYRICA, tell your healthcare provider about all your medical conditions, including if you:
- have or have had depression, mood problems or suicidal thoughts or behavior
- have kidney problems or get kidney dialysis
- have heart problems including heart failure
- have a bleeding problem or a low blood platelet count
- have abused prescription medicines, street drugs, or alcohol in the past
- have ever had swelling of your face, mouth, tongue, lips, gums, neck, or throat (angioedema)
- plan to father a child. Animal studies have shown that pregabalin, the active ingredient in LYRICA, made male animals less fertile and caused sperm to change. Also, in animal studies, birth defects were seen in the offspring (babies) of male animals treated with pregabalin. It is not known if these problems can happen in people who take LYRICA.
- are pregnant or plan to become pregnant. It is not known if LYRICA will harm your unborn baby. You and your healthcare provider will have to decide if you should take LYRICA while you are pregnant. If you become pregnant while taking LYRICA, talk to your healthcare provider about registering with the North American Antiepileptic Drug Pregnancy Registry. You can enroll in this registry by calling 1-888-233-2334. The purpose of this registry is to collect information about the safety of antiepileptic drugs during pregnancy.
- are breastfeeding. It is not known if LYRICA passes into breast milk and if it can harm your baby. You and your healthcare provider should discuss whether you should take LYRICA or breast-feed, but you should not do both.
- Before taking LYRICA, tell your healthcare provider about all your medical conditions, including if you:
- Tell your healthcare provider about all the medicines you take including prescription and non-prescription medicines, vitamins or herbal supplements. LYRICA and other medicines may affect each other causing side effects. Especially tell your healthcare provider if you take:
- angiotensin converting enzyme (ACE) inhibitors, which are used to treat many conditions, including high blood pressure. You may have a higher chance for swelling and hives if these medicines are taken with LYRICA. See "What is the most important information I should know about LYRICA?"
- Avandia (rosiglitazone), Avandamet (contains rosiglitazone and metformin), or Actos (pioglitazone) for diabetes. You may have a higher chance of weight gain or swelling of your hands or feet if these medicines are taken with LYRICA. See "What are the possible side effects of LYRICA."
- any narcotic pain medicine (such as oxycodone), tranquilizers or medicines for anxiety (such as lorazepam). You may have a higher chance for dizziness and sleepiness if these medicines are taken with LYRICA.
- any medicines that make you sleepy
- Know the medicines you take. Keep a list of them with you to show your healthcare provider and pharmacist each time you get a new medicine. Do not start a new medicine without talking with your healthcare provider.
- Tell your healthcare provider about all the medicines you take including prescription and non-prescription medicines, vitamins or herbal supplements. LYRICA and other medicines may affect each other causing side effects. Especially tell your healthcare provider if you take:
- How should I take LYRICA?
- Take LYRICA exactly as prescribed. Your healthcare provider will tell you how much LYRICA to take and when to take it. Take LYRICA at the same times each day.
- LYRICA may be taken with or without food.
- Your healthcare provider may change your dose. Do not change your dose without talking to your healthcare provider.
- Do not stop taking LYRICA without talking to your healthcare provider. If you stop taking LYRICA suddenly you may have headaches, nausea, diarrhea, trouble sleeping, increased sweating, or you may feel anxious. If you have epilepsy and you stop taking LYRICA suddenly, you may have seizures more often. Talk with your healthcare provider about how to stop LYRICA slowly.
- If you miss a dose, take it as soon as you remember. If it is almost time for your next dose, just skip the missed dose. Take the next dose at your regular time. Do not take two doses at the same time.
- If you take too much LYRICA, call your healthcare provider or poison control center, or go to the nearest emergency room right away.
- Take LYRICA exactly as prescribed. Your healthcare provider will tell you how much LYRICA to take and when to take it. Take LYRICA at the same times each day.
- What should I avoid while taking LYRICA?
- Do not drive a car, work with machines, or do other dangerous activities until you know how LYRICA affects you.
- Do not drink alcohol while taking LYRICA. LYRICA and alcohol can affect each other and increase side effects such as sleepiness and dizziness.
- What are the possible side effects of LYRICA?
- LYRICA may cause serious side effects, including:
- See "What is the most important information I should know about LYRICA?"
- muscle problems, muscle pain, soreness, or weakness. If you have these symptoms, especially if you feel sick and have a fever, tell your healthcare provider right away.
- problems with your eyesight, including blurry vision. Call your healthcare provider if you have any changes in your eyesight.
- weight gain. If you have diabetes, weight gain may affect the management of your diabetes. Weight gain can also be a serious problem for people with heart problems.
- feeling "high"
- The most common side effects of LYRICA are:
- dizziness
- blurry vision
- weight gain
- sleepiness
- trouble concentrating
- swelling of hands and feet
- dry mouth
- LYRICA caused skin sores in animal studies. Skin sores did not happen in studies in people. If you have diabetes, you should pay attention to your skin while taking LYRICA and tell your healthcare provider about any sores or skin problems.
- Tell your healthcare provider about any side effect that bothers you or that does not go away.
- These are not all the possible side effects of LYRICA. For more information, ask your healthcare provider or pharmacist.
- Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
- LYRICA may cause serious side effects, including:
- How should I store LYRICA?
- Store LYRICA capsules and oral solution at room temperature, 59°F to 86°F (15°C to 30°C) in its original package.
- Safely throw away any LYRICA that is out of date or no longer needed.
- Keep LYRICA and all medicines out of the reach of children.
- Store LYRICA capsules and oral solution at room temperature, 59°F to 86°F (15°C to 30°C) in its original package.
- General information about LYRICA
- Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use LYRICA for a condition for which it was not prescribed. Do not give LYRICA to other people, even if they have the same symptoms you have. It may harm them.
- This Medication Guide summarizes the most important information about LYRICA. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about LYRICA that is written for health professionals.
- You can also visit the LYRICA website at www.LYRICA.com or call 1-866-459-7422 (1-866-4LYRICA).
- What are the ingredients In LYRICA?
- Active ingredient: pregabalin
- Inactive ingredients:
- LYRICA capsules: lactose monohydrate, cornstarch, talc
- Capsule shell: gelatin and titanium dioxide; Orange capsule shell: red iron oxide; White capsule shell: sodium lauryl sulfate, colloidal silicon dioxide. Colloidal silicon dioxide is a manufacturing aid that may or may not be present in the capsule shells.
- Imprinting ink: shellac, black iron oxide, propylene glycol, potassium hydroxide.
- LYRICA oral solution: methylparaben, propylparaben, monobasic sodium phosphate anhydrous, dibasic sodium phosphate anhydrous, sucralose, artificial strawberry #11545 and purified water.
- This Medication Guide has been approved by the U.S. Food and Drug Administration.
Precautions with Alcohol
- Avoid consuming alcohol while taking LYRICA, as LYRICA may potentiate the impairment of motor skills and sedating effects of alcohol.
Brand Names
- LYRICA®[2]
Look-Alike Drug Names
- Lyrica® — Lopressor®[3]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Feltner D, Wittchen HU, Kavoussi R, Brock J, Baldinetti F, Pande AC (2008). "Long-term efficacy of pregabalin in generalized anxiety disorder". Int Clin Psychopharmacol. 23 (1): 18–28. doi:10.1097/YIC.0b013e3282f0f0d7. PMID 18090504.
- ↑ "LYRICA (pregabalin) capsule LYRICA (pregabalin) solution".
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Pregabalin
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin25.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin26.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin27.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin28.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin29.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin30.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin31.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin32.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin33.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin34.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin35.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin36.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin38.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin39.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin40.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin42.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin43.png
}}