Dilated cardiomyopathy natural history, complications and prognosis
|
Dilated cardiomyopathy Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Dilated cardiomyopathy natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Dilated cardiomyopathy natural history, complications and prognosis |
|
FDA on Dilated cardiomyopathy natural history, complications and prognosis |
|
CDC on Dilated cardiomyopathy natural history, complications and prognosis |
|
Dilated cardiomyopathy natural history, complications and prognosis in the news |
|
Blogs on Dilated cardiomyopathy natural history, complications and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Abdelrahman Ibrahim Abushouk, MD[2]
Overview
The natural history of dilated cardiomyopathy has significantly improved following the advances in medical therapy and introduction of cardiac resynchronization and implantable defibrillators. However, patients with DCM are still prone to complications as heart failure, arrhythmias, arterial embolism and sudden cardiac death. There are several prognostic indicators when evaluating dilated cardiomyopathy, the most important one being ejection fraction. Complications as a result of dilated cardiomyopathy include heart failure, aortic and mitral valve regurgitation, emboli, edema, arrhythmias and sudden cardiac arrest.
Natural History, Complications, and Prognosis
Natural History
- Dilated cardiomyopathy is the final common pathway for different etiologic mechanisms.
- During the initial visit of a patient with DCM, the clinician should in fact consider all the potentially reversible causes of left ventricular dysfunction, likely to benefit from specific therapeutic intervention.
- The onset of DCM can be at times indistinguishable from other conditions which can be specifically recovered by correcting the underlying problem.[1]
- The natural history of DCM has thus significantly changed in the last few years, particularly after the introduction and utilization of ACE-inhibitors, betablockers, anti-aldosterone drugs and nonpharmacological treatments, such as cardiac resynchronization (CRT) and implantable defibrillator (ICD).[2]
- However, still about 2% of patients with DCM died of sudden cardiac death after the diagnosis and the risk of other complications as heart failure, arterial infarctions, and valvular insufficiency remains high.[3]
Complications
The following complications may occur in patients with dilated cardiomyopathy.[3]
- Heart failure: may occur as the end result of DCM pathogenesis.
- Heart valve regurgitation
- Arrhythmias: as conduction delays, bundle branch blocks, and tachyarrhythmias.
- Edema: Central (pulmonary congestion and hepatomegaly) and peripheral (pedal).
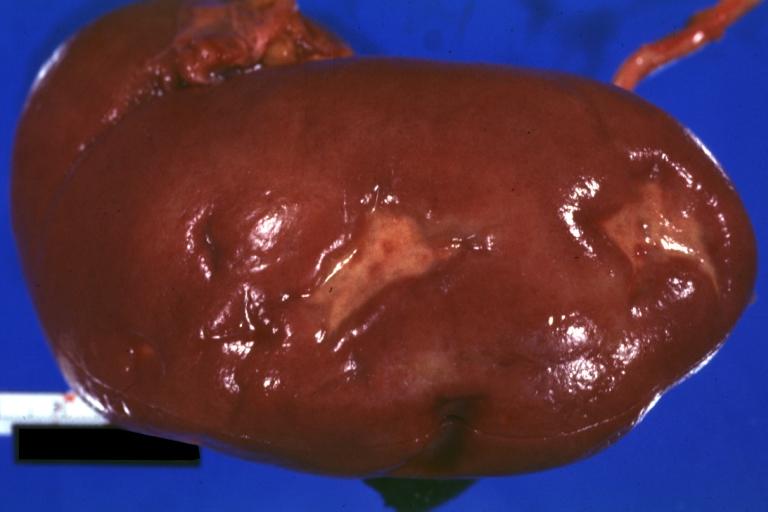
- Embolism: causing arterial infarcts as renal infarcts and stroke.
- Sudden cardiac arrest: may occur in 2% of patients with DCM.
-
Kidney: Infarct Remote: Gross external view with capsule removed two old and very typical infarct scars 27 year old person with dilated cardiomyopathy
-
Brain: Infarct: Healing large MCA and PICA probably embolic 64 year old female chronic obstructive pulmonary disease and cardiomyopathy with atrial fibrillation
Prognosis
There are many prognostic factors which can be evaluated in a patient with dilated cardiomyopathy. The most important prognostic indicator is a decreased ejection fraction, in addition increased left ventricular size and right ventricular dilation are independent indicators of a poor prognosis. As is in most types of heart failure a poor NYHA functional class and increased PASP (>35mmHg) are also poor prognostic indicators. Other findings that infer a poor prognosis are as follows: Maximal O2 uptake of < 12mL/kg / minute on exercise testing, LBBB (left bundle branch block), non sustained ventricular tachycardia, syncope, hyponatremia with a serum sodium less than 135, elevated norepinephrine, ANP (atrial natriuretic peptide) and renin levels (not routinely measured in clinical practice), elevated PCWP (pulmonary capillary wedge pressure) > 18mmHg and low cardiac index < 2.5L/min/m^2.[4][5]
References
- ↑ Di Lenarda A, Pinamonti B, Mestroni L, Salvi A, Sabbadini G, Gregori D; et al. (2004). "[How the natural history of dilated cardiomyopathy has changed. Review of the Registry of Myocardial Diseases of Trieste]". Ital Heart J Suppl. 5 (4): 253–66. PMID 15185463.
- ↑ Merlo M, Gentile P, Naso P, Sinagra G (2017). "The natural history of dilated cardiomyopathy: how has it changed?". J Cardiovasc Med (Hagerstown). 18 Suppl 1: e161–e165. doi:10.2459/JCM.0000000000000459. PMID 27828827.
- ↑ 3.0 3.1 Zecchin M, Merlo M, Pivetta A, Barbati G, Lutman C, Gregori D; et al. (2012). "How can optimization of medical treatment avoid unnecessary implantable cardioverter-defibrillator implantations in patients with idiopathic dilated cardiomyopathy presenting with "SCD-HeFT criteria?"". Am J Cardiol. 109 (5): 729–35. doi:10.1016/j.amjcard.2011.10.033. PMID 22176998.
- ↑ Castelli G, Fornaro A, Ciaccheri M, Dolara A, Troiani V, Tomberli B; et al. (2013). "Improving survival rates of patients with idiopathic dilated cardiomyopathy in Tuscany over 3 decades: impact of evidence-based management". Circ Heart Fail. 6 (5): 913–21. doi:10.1161/CIRCHEARTFAILURE.112.000120. PMID 23888044.
- ↑ Hagar A, Pu XB, Chen SJ, Shah JP, Chen M (2019). "Clinical characteristics, treatment and prognosis of patients with idiopathic dilated cardiomyopathy: a tertiary center experience". J Geriatr Cardiol. 16 (4): 320–328. doi:10.11909/j.issn.1671-5411.2019.04.004. PMC 6503477 Check
|pmc=value (help). PMID 31105752.