Smallpox
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Michael Maddaleni, B.S.{{#meta: itemprop="medicalWebPageAudiences" content="patient"}}{{#meta: itemprop="medicalWebPageSpecialities" content="cardiology"}}{{#meta: itemprop="medicalWebPageInfoTypes" content="symptoms,diagnosis,treatment,causes,prognosis,complications"}} [[Natural Progression::{{{naturalProgression}}}| ]] Classification Classic::Classification Atypical::
Overview
|
Smallpox Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Smallpox On the Web |
|
American Roentgen Ray Society Images of Smallpox |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [3]
Overview
Smallpox is a contagious disease unique to humans.[1] Smallpox is caused by either of two virus variants named Variola major and Variola minor. The deadlier form, V. major, has a mortality rate of 30–35%, while V. minor causes a milder form of disease called alastrim and kills ~1% of its victims.[2][1] Long-term side-effects for survivors include the characteristic skin scars. Occasional side effects include blindness due to corneal ulcerations and infertility in male survivors.
Historical Perspective
Up until 1977, when it became the only human infectious disease to have been completely eradicated, smallpox had had great impact in human history. The disease is estimated to be at least 16,000 years old and played a major role in the history of Europe, Asia, North America, and Africa. The first clinical evidence of the disease was found in an Egyptian mummy, Ramses V. Smallpox has also been used as a weapon throughout history. The most recent example was the weaponization of smallpox during World War II. After successful vaccination campaigns in the 19th and 20th centuries, the WHO certified the eradication of smallpox in 1980.[3]
Eradication
Smallpox was declared eradicated in 1980 by the WHO. The eradication of smallpox required a global effort. Since every country was susceptible of the devastating disease, eradicating this infection was expensive and took many years.
Post-Eradication
After the reported death by smallpox accident in 1978, all known stocks of the virus were destroyed. Today only the United States CDC and Russian State Research Center of Virology and Biotechnology VECTOR have the virus in their laboratories for research purposes.
Pathophysiology
Smallpox virus may be transmitted from contaminated surfaces or aerosolized particles. It is capable of inducing harm by evading the host's immune system and replicating inside host's cells. The virus may cause 3 forms of the disease: 1) ordinary; 2) flat-type; or 3) hemorrhagic smallpox. It infects different cells of the body, being known by it's characteristic lesions on the skin.
Causes
Smallpox is caused by the variola virus, a dsDNA virus of the Poxviridae family. There are two forms of this virus with different virulences, evidenced on the discrepancy in respective death rates. The virus survives in the cold and aerosoled environments, what explains its oral transmission among humans, which are it's only host species. Unlike other DNA viruses, it replicates within the cytoplasm, to which it shows tropism.
Differentiating Smallpox from other Diseases
Prior to its eradication, smallpox would need to be differentiated from other diseases that cause a vesicular rash and a fever including chickenpox (which was often mistaken for smallpox), herpes zoster and erythema multiforme.[4]
Epidemiology and Demographics
The true incidence of smallpox, before declared eradicated in 1980 by the WHO, wasn't possible to specify due to the lack of new case reports from countries, particularly endemic regions, in which the reported numbers are stipulated to be 1-2% of the reality. Children and young adults were the most affected, especially in regions with low level of immunity. There is no evidence of gender or race difference in the incidence of the disease. Developing countries had a higher incidence of the disease.[5]
Risk Factors
People who work in laboratories with the virus, or live in areas which have been target of bioterrorism, are at risk of contracting smallpox. Before eradication, risk factors included: physical contact with a patient with the disease, contact with contaminated body fluids, and exposure to contaminated aerosolized particles.[4]
Natural History, Complications and Prognosis
The natural history and outcome of smallpox depend on the form of disease. The common progress will start with flu-like symptoms followed by a skin rash that generally progresses in a typical fashion, leading to the formation of scabs that will fall off, leaving a scar. The complications may include respiratory conditions, from bronchitis to pneumonia, but may also involve the joints, bones and/or eyes. The overall fatality rate for the variola major form was about 30%.
Diagnosis
Diagnostic Criteria
The diagnosis of smallpox is guided by an algorithm, elaborated by the CDC, that follows certain major and minor criteria.
History and Symptoms
Symptoms of smallpox progress in a typical fashion and some of its common symptoms may include high fever, rash (initially in the oral mucosa, followed by the skin), malaise, fatigue, muscle pain and vomiting.
Physical Examination
Depending on the stage of the disease, physical findings may include: high fever, tachycardia secondary to the fever, rash of the oral mucosa, skin rash with typical progression, ophthalmological changes, abdominal pain, and altered mental status.
Laboratory Findings
The polymerase chain reaction test and the growth of the virus in specific cell cultures allow the identification of the smallpox virus.
Treatment
Medical Therapy
There is no antiviral treatment for smallpox. In case of disease, it is only possible to manage the wellbeing of the patient, hydrate and administer certain drugs to decrease the fever or pain and to treat concomitant bacterial and/or viral infections.
Primary Prevention
Primary prevention of smallpox consists in the administration of the vaccinia vaccine, which attenuates or suppresses the manifestations of the disease, if administrated soon after infection has occurred. In the absence of an outbreak, the vaccine is only administered to clinical and/or laboratory workers dealing with the virus in specialized laboratories. It has several adverse effects, particularly in immunosuppressed individuals, those with heart conditions or allergies, for whom its administration must be guided by specific rules.
Outbreak Prevention
The CDC has elaborated a series of measures to protect the citizens in case of a smallpox outbreak.[4]
Cost-Effectiveness of Therapy
The efforts made for the eradication of smallpox were cost-effective, since the disease was successfully eradicated in 1980.
Future or Investigational Therapies
Even though it has been eradicated, there are undergoing studies to find an antiviral drug against smallpox virus due to the potential of an outbreak, and/or use as use in bioterrorism.
References
- ↑ 1.0 1.1 Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. pp. 525&ndash, 8. ISBN 0838585299.
- ↑ Behbehani AM (1983). "The smallpox story: life and death of an old disease". Microbiol Rev. 47 (4): 455–509. PMID 6319980.
- ↑ De Cock KM (2001). "(Book Review) The Eradication of Smallpox: Edward Jenner and The First and Only Eradication of a Human Infectious Disease". Nature Medicine. 7: 15&ndash, 6.
- ↑ 4.0 4.1 4.2 "Smallpox disease overview".
- ↑ "The epidemiology of smallpox" (PDF).
Historical Perspective
|
Smallpox Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Smallpox On the Web |
|
American Roentgen Ray Society Images of Smallpox |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [4]
Overview
Smallpox is estimated to be at least 16,000 years old, and up until 1977, when it became the only human infectious disease to have been completely eradicated, smallpox played a major role in human history. The first clinical evidence of the disease was found in an Egyptian mummy, Ramses V. Smallpox has also been used as a weapon throughout history. The most recent example was the weaponization of smallpox during World War II. After successful vaccination campaigns in the 19th and 20th centuries, the WHO certified the eradication of smallpox in 1980.[1]
Historical Perspective
Impact on Historical Figures and History
Famous victims of this disease include Date Masamune of Japan (who lost an eye to the disease), Ramses V,[2] the Shunzhi Emperor and Tongzhi Emperor of China (official history), Mary II of England, Maximilian III Joseph, Elector of Bavaria and Peter II of Russia. Guru Har Krishan 8th Guru of the Sikhs in 1664, Peter III of Russia in 1744 and Abraham Lincoln in 1863.[3] Joseph Stalin, who was badly scarred by the disease early in life, often had photographs retouched to make his pockmarks less apparent.
Families prominent in history often had several people fall victim to the disease. For example, several relatives of Henry VIII survived the disease but were scarred by it. These include his sister Margaret, Queen of Scotland, his fourth wife, Anne of Cleves, and his daughter, Elizabeth I of England in 1562. His son and heir Edward VI died very shortly after apparently recovering from the disease. Some scholars assert that his death may have been due to complications from smallpox. A more distant relative Mary Queen of Scots contracted the disease as a child but had no visible scarring. Deaths from smallpox often impacted dynastic succession. Louis XV of France succeeded his great-grandfather through a series of deaths of smallpox or measles among those earlier in the succession line and himself died of the disease in 1774.
Outbreak in North America
Between 1775 and 1782, a smallpox epidemic raged across much of North America, killing more than 130,000 people. Among other places it affected:
- The town of Boston during the British occupation and the American siege of 1775
- The American invasion of Quebec, 1775
- Smallpox ravaged the populations of escaped slaves who fled to the British lines in the South during the american revolutionary war
- New Orleans, 1778
- Tens of thousands of people died throughout Mexico beginning in 1779
- It swept through the Pueblos of New Mexico beginning in 1780
- It probably travelled among the people of the Great Plains
- It showed up in the interior trading posts of the Hudson's Bay Company in 1782
Outbreak in Europe
The 1972 outbreak of smallpox in Yugoslavia was the last major outbreak of smallpox in Europe. It was centred in Kosovo and Belgrade, Serbia (both then part of SFR Yugoslavia. A Muslim pilgrim had contracted the smallpox virus in the Middle East. Upon returning to his home in Kosovo, he started the epidemic in which 175 people were infected, 35 of whom died. The epidemic was efficiently and ruthlessly contained by enforced quarantine and mass vaccination.
Background
By 1972, vaccination for smallpox had long been widely available and the disease was considered to be eradicated in Europe. The population of Yugoslavia had been regularly vaccinated against smallpox for 50 years, and the last case was reported in 1930. This was the major cause for the initial slow reaction by doctors, who did not promptly recognize the symptoms of the disease.
The outbreak
In early 1972, a 38-year-old Muslim clergyman from Damnjan near Đakovica, Kosovo, undertook the pilgrimage to Mecca. He also visited holy sites in Iraq, where there were known cases of smallpox. He returned home on February 15. The following morning he felt achy and tired, but attributed this to the long bus journey. He soon realised that he had some kind of infection, but, after feeling feverish for a couple of days and developing a rash, he recovered - probably because he had been vaccinated two months earlier.
On March 3, Latif Musa, a thirty-year-old schoolteacher, who had just arrived in Djakovica to enroll at the local higher institute of education, fell ill. He had no known direct contacts with the clergyman, so he might have been infected by one of the clergyman's friends or relatives who visited him during his illness, or by passing the clergyman in the street.
When Musa visited the local medical center two days later, the doctors tried to treat his fever with penicillin (smallpox is a virus, so this was ineffective). His condition didn't improve, and after a couple of days his brother took him to the hospital in Čačak, 150 km to the north in Serbia. The doctors there could not help him, so he was transferred by ambulance to the central hospital in Belgrade.
On March 9, Musa was shown to medical students and staff as a case of an atypical reaction to penicillin, which was a plausible explanation for his condition. On the following day, Musa suffered massive internal bleeding and, despite efforts to save his life, died in the evening.
The cause of death was listed as "reaction to penicillin". In fact he had contracted black pox, a highly contagious form of smallpox. Before his death, Musa directly infected 38 people (including nine doctors and nurses), eight of whom would consequently die.
Reaction
By March 22, medical authorities realised that Musa had died of smallpox. The government's reaction was swift. Martial law was declared. Measures included blockades of villages and neighbourhoods, roadblocks, prohibition of public meetings, closure of borders and prohibition of all non-essential travel. Hotels were requisitioned for quarantines in which 10,000 people who may have been in contact with the virus were held under guard by the army. The authorities undertook a massive revaccination of the population, helped by the World Health Organization. Donald Henderson, the world's foremost authority on smallpox, was flown in to help the effort.
Within two weeks, almost the entire population had been revaccinated. By mid-May the spread of the disease was stopped and the country returned to normal life. During the epidemic, 175 people contracted smallpox and 35 of them died.
Legacy
The Yugoslav government received international praise for the successful containment of the epidemic, which was also one of the finest hours for Donald Henderson and the WHO, as well as one of crucial steps in the eradication of smallpox.
Two months of martial law, the fear and the helplessness during of the epidemic left a lasting mark on an entire generation. Another, more tangible mark, was left in the shape of the small scars on millions of arms, left by the vaccination.
Timeline
- February 15 1972 - A clergyman returns from pilgrimage to Mecca infected with the smallpox virus.
- February 16 - The clergyman feels unwell.
- February 21 - Ljatif Muzza, a thirty-year old school teacher, arrives in Djakovica to continue his studies.
- March 3 - Muzza falls ill with a highly contagious form of smallpox.
- Between March 3 and March 9 Muzza is misdiagnosed and moved to hospitals in Čačak and then Belgrade. During this time, he directly infects 38 people.
- March 9 - Muzza is shown to medical students in the Belgrade hospital as a case of reaction to penicillin.
- March 10 - Muzza develops massive internal bleeding and dies.
- March 22 - Doctors correctly diagnose the cause of Muzza's death and government begins measures to contain the epidemic.
- Early April - Mass revaccination begins. Donald Henderson arrives.
- Late May - The epidemic is over. 175 people were infected, 35 died.
Inoculation

By that time, a preventive treatment for smallpox had finally arrived. It was a process called inoculation, also known as insufflation or variolation. Inoculation was not a sudden innovation, as it is known to have been practiced in India as early as 1000 BC.[5] The Indians rubbed pus into the skin lesions. The Chinese blew powdered smallpox scabs up the noses of the healthy after discovery, by a Buddhist nun, that this inoculated non-immune people. The patients would then develop a mild case of the disease and from then on were immune to it. This technique is known as variolation and although variolation had a 0.5-2% mortality rate, this was considerably less than the 20-30% mortality rate of the disease itself. The process spread to Turkey where Lady Mary Wortley Montagu, wife of the British ambassador, learned of it from Emmanuel Timoni (ca. 1670–1718), a doctor affiliated with the British Embassy in Istanbul. She had the procedure performed on her son and daughter, aged 5 and 4 respectively. They both recovered quickly and the procedure was hailed as a success and reported to the Royal Society in England. Timoni, from the University of Padova, Italy and a member of the Royal Society of London since 1703, published “an account, or history, of the procuring the smallpox by incision” in December 1713 in the Philosophical Transactions. His work was published again in 1714 in Leipzig and was followed by those of Pylarino (1715), Leduc (1722), and Maitland (1722).
In 1721, an epidemic of smallpox hit London and left the British Royal Family in fear. Reading of Lady Wortley Montagu’s efforts, they wanted to use inoculation on themselves. Doctors told them that it was a dangerous procedure, so they decided to try it on other people first. The test subjects they used were condemned prisoners. The doctors inoculated the prisoners and all of them recovered in a couple of weeks. So assured, the British royal family inoculated themselves and reassured the English people that it was safe.
But inoculation still had its critics. Prominent among them were religious preachers who claimed that smallpox was God’s way of punishing people and that inoculation was a tool of Satan. This resistance only encouraged Montagu and the others to work even harder. By 1723 inoculations were extremely common in England, but even scientific opposition (such as the Fellow of the Royal College of Physicians Pierce Dod) continued for some time.
In 1721, Onesimus was the slave of a Boston preacher when smallpox came to Boston via a ship arriving from Barbados.[6] His owner, Cotton Mather asked his slave if he ever had smallpox. Onesimus said, “Yes and no,” and explained a technique from his homeland in Africa, thought to be in Sudan. He explained that pus from an infected person was deliberately rubbed into a scratch or cut of a non-infected person, and when successful, the person had immunity. This remedy from an African slave was the precursor to inoculations. Cotton Mather, the son of a former Harvard University dean, was waging a campaign of his own to promote the process, although religious resistance to inoculation was very strong. At one point, Cotton Mather was in danger from a crowd that wanted to hang him. After six patients died from the procedure, he was called a murderer. But, when the population of Boston returned after the end of a smallpox epidemic in 1722, he was an instant hero. Out of the population of Boston, 7% had died from smallpox. Out of the 300 people that chose to inoculate themselves, only 2% died. In 1750, the English magazine, Gentleman's Magazine, reprinted a 1725 pamphlet that argued in support of smallpox inoculations. By 1774, it was considered odd not to choose inoculation. Onesimus was later freed by Mather, not for his knowledge and help in combating smallpox, but because Mather considered him to be disobedient.
Even though inoculation was a powerful method of controlling smallpox, it was far from perfect. Inoculation caused a mild case of smallpox which resulted in death in about 2% of the cases. It was also difficult to administer. Sick patients had to be locked away to prevent them from transmitting the disease to others. Thus George Washington initially hesitated to have his Revolutionary War troops inoculated during a smallpox outbreak in February 1777, writing, “should We inoculate generally, the Enemy, knowing it, will certainly take Advantage of our Situation;” but the virulence of the outbreak soon prompted him to order inoculation for all troops and recruits who had not had the disease.[7]
In 1796, a young boy in England was inoculated by Edward Jenner. The boy suffered from the disease for an entire month and recovered completely.
Weaponization of Smallpox
In World War II, scientists from the United Kingdom and the United States were involved in research into producing a biological weapon from smallpox. Plans of large scale production were never carried through as they considered that the weapon would not be very effective due to the wide-scale availability of a vaccine.[8]
The first smallpox weapons factory in the Soviet Union was established in 1947 in the city of Zagorsk, close to Moscow [9]. It was produced by injecting small amounts of the virus into chicken eggs. An especially virulent strain (codenamed India-1967 or India-1) was brought from India in 1967 by a special Soviet medical team that was sent to India to help to eradicate the virus. The pathogen was manufactured and stockpiled in large quantities throughout the 1970s and 1980s.
An outbreak of weaponized smallpox occurred during its testing in the 1970s. General Prof. Peter Burgasov, former Chief Sanitary Physician of the Soviet Army, and a senior researcher within the Soviet program of biological weapons described this incident:
- “On Vozrozhdeniya Island in the Aral Sea, the strongest recipes of smallpox were tested. Suddenly I was informed that there were mysterious cases of mortalities in Aralsk. A research ship of the Aral fleet came 15 km away from the island (it was forbidden to come any closer than 40 km). The lab technician of this ship took samples of plankton twice a day from the top deck. The smallpox formulation— 400 gr. of which was exploded on the island—”got her” and she became infected. After returning home to Aralsk, she infected several people including children. All of them died. I suspected the reason for this and called the Chief of General Staff of Ministry of Defense and requested to forbid the stop of the Alma-Ata—Moscow train in Aralsk. As a result, the epidemic around the country was prevented. I called Andropov, who at that time was Chief of KGB, and informed him of the exclusive recipe of smallpox obtained on Vozrazhdenie Island.” [10][11]
A production line to manufacture smallpox on an industrial scale was launched in the Vector Institute in 1990.[9] The development of genetically altered strains of smallpox was presumably conducted in the Institute under leadership of Dr. Sergei Netyosov in the middle of the 1990s, according to Kenneth Alibek, although this has never been proven due to the classified nature of the program[9]
References
- ↑ De Cock KM (2001). "(Book Review) The Eradication of Smallpox: Edward Jenner and The First and Only Eradication of a Human Infectious Disease". Nature Medicine. 7: 15&ndash, 6.
- ↑ Koplow, David (2003). Smallpox: The Fight to Eradicate a Global Scourge. Berkeley and Los Angeles, CA: University of California Press. ISBN 0-520-23732-3.
- ↑ "President Abraham Lincoln: Health & Medical History". 2007-03-24. Retrieved 2007-06-18.
- ↑ "Wikimedia Commons".
- ↑ Bourzac K (2002). "Smallpox: Historical Review of a Potential Bioterrorist Tool". Journal of Young Investigators. 6 (3): –.
- ↑ "BLACK HISTORY MONTH II: Why Wasn't I Taught That? (B. Willoughby)". Tolerance in the News. Retrieved 2006-09-23.
- ↑ Grizzard FE, Washington G, Chase PD, Twohig D (1985). George Washington to Major General Horatio Gates, 5–6 February 1777. In: The papers of George Washington. 8. Charlottesville: University Press of Virginia. ISBN 0-8139-1787-5.
- ↑ http://www.viewzone.com/smallpox.html
- ↑ 9.0 9.1 9.2 Alibek K, Handelman S (1999). Biohazard: The Chilling True Story of the Largest Covert Biological Weapons Program in the World—Told from Inside by the Man Who Ran It. New York: Delta. ISBN 0-385-33496-6.
- ↑ Shoham D, Wolfson Z (2004). "The Russian biological weapons program: vanished or disappeared?". Crit. Rev. Microbiol. 30 (4): 241–61. PMID 15646399.
- ↑ "Smallpox - not a bad weapon". Interview with General Burgasov (in Russian). Moscow News. Retrieved 2007-06-18.
Pathophysiology
|
Smallpox Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Smallpox On the Web |
|
American Roentgen Ray Society Images of Smallpox |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [5]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [6]
Overview
Smallpox virus may be transmitted from contaminated surfaces or aerosolized particles. It is capable of inducing harm by evading the host's immune system and replicating inside host's cells. The virus may cause 3 forms of the disease: 1) ordinary; 2) flat-type; or 3) hemorrhagic smallpox. It infects different cells of the body, being known by it's propensity to cause characteristic pock like lesions on the skin.
Transmission
Smallpox virus is transmitted by:[1]
- Physical contact
- Contact with infected body fluids
- Contact with infected objects
- Air through aerosolized particles
Genetics
Smallpox pathogenicity is due to its ability to evade the host's immune system. Most proteins responsible for the pathogenesis of the virus are located at the terminal DNA regions of the virus.
Genetic comparisons of the smallpox virus with the vaccinia virus allowed to observe certain genetic changes that may be responsible for the virulence of the smallpox virus. However, without studying the gene transcripts, it is not possible to draw objective conclusions.[2]
Pathogenesis
The smallpox virus commonly enters the body through the upper respiratory tract, invading the oropharyngeal and respiratory mucosa.[3] Other possible ports of entry include: skin, conjunctiva as well as through the placenta.[4] Although the viral scabs may contain life viruses, they are commonly contained within thickened material, which limits transmission.
Once in the respiratory mucosa, the infection commonly progresses as:[5][4][6]
- Asymptomatic respiratory mucosa infection
- Viral replication within respiratory epithelium
- Transient primary asymptomatic viraemia
- Virus enters macrophages and spreads to lymph nodes and reticuloendothelial system, where it replicates during 4 - 14 days
- Exuberant secondary viraemia, leading to symptom onset
During secondary viraemia the virus infects mucous cells of the pharynx and mouth, and endothelium of the capillaries of the dermis, causing skin lesions. Other organs with high viral loads include:[6]
Before development of the rash, the first lesions appear on the oropharyngeal mucosa, at which time the virus is released through the mucosal secretions, making that patient infectious.
Skin lesions develop due to migration of macrophages to the infected areas of the dermis, leading to edema and necrosis. With the influx of more polymorphonuclear cells, skin pustules will develop.[5]
The immune system responds to the viremia with activation of lymphocytes T and B and concomitant production of:[6]
- Neutralizing antibodies, during first week of disease, remaining for many years
- Hemagglutination-inhibition antibodies, by the 16th day of infection, beginning to decrease after 1 year
- Complement-fixation antibodies, by the 18th day of infection, beginning to decrease after 1 year
- Memory T cells, remaining for 50 years
Death by smallpox was commonly due to toxemia, following:[5]
Gross Pathology
Depending on the status of the patient's immune system, there are 3 forms of smallpox:[7]
Ordinary Smallpox
Ordinary smallpox is characterized by the following progression of lesions:[8]
- Initial hypopigmented macules, which appear first in the mouth
- Macules progress into papules and subsequently to vesicles
- Vesicles become pustules
- At the 14th day, pustules loose liquid content and become crusted
- At the 3rd week, most crusts will separate (palms and soles last)
This form of smallpox is typical of an immunocompetent patient, in whom the immune system is able to inhibit viral replication.
Flat-type Smallpox
Flat-type smallpox is characterized by the following progression of lesions:[9]
- Delayed appearance of macules
- Slow progression of the lesions, usually with flat and soft appearance
- Possible slough of skin sections
Most cases are fatal with presence of severe toxemia. This form of smallpox is typical of patients with weak cellular immune response to the virus.
Hemorrhagic-type smallpox
Hemorrhagic-type smallpox is characterized by the following progression of lesions:[10]
- Skin petechiae
- Mucous membrane and conjunctival bleeding
- Subcutaneous hemorrhage gives skin and conjunctivae deep red appearance
- Organ bleeding
- Early death by multi organ failure, usually before appearance of maculae.
This rare form of smallpox is typical of patients with severely compromised immune response, in which there is intense viral replication in the bone marrow and spleen. It is also associated with intense toxemia.
Microscopic Pathology
The typical skin vesicles observed in smallpox occur following:[11]
- Viral infection of the epidermal cell
- Cells in malpighian layer entering balloon degeneration, from formation of vacuoles
- Cytoplasmic enlargement leading to loss of nuclear material
- Destruction of upper and middle layers of stratum spinosum
- Formation of vesicles, with high viral index
On the other hand, in the infected mucous surfaces, the viral proliferation and absence of the stratum corneum, lead to the formation of ulcers. These ultimately lead to the release of greater loads of virus into the oropharynx.[12]
Histopathology
Poxviruses are characterized by cytoplasmic inclusions, however, these do not identify specifically the smallpox virus on a biopsy. There are 2 types of inclusion bodies:[13]
A-type
Typical of some viruses of the:
- Genus Orthopoxvirus:
- Cowpox virus
- Ectromelia virus
- Genus Avipoxvirus
B-type, or Guarnieri bodies
- In areas of active viral replication
- Present in infections by all poxviruses
- Appear as basophilic bodies near the nucleus on hematoxylin and eosin-stained samples
- Evident at epithelial cells underlying vesicles and pustules
Gallery
-
Hematoxylin and eosin (H&E)-stained tissue sample, reveals some of the histopathologic changes found in a human skin tissue sample from the site of a smallpox lesion. Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]
-
hematoxylin and eosin (H&E)-stained tissue sample, reveals some of the histopathologic changes found in a human skin tissue sample from the site of a smallpox lesion. Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]
-
This is a chickenpox scab (left), and smallpox scab (right) viewed in profile as a demonstration in comparative morphology. Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]
-
This image depicts three mounted chickenpox scabs seen from the side revealing the superficiality of these scabs when morphologically compared to a smallpox scab.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]
-
Viewed from above, this image depicts a smallpox scab (left), and chickenpox scab (right) as a demonstration in comparative morphology. Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]
-
Cytoarchitectural pathologic changes found in a sample of skin tissue from a eczema vaccinatum lesion, which had manifested itself after this patient had received a smallpox vaccination.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]
-
Cytoarchitectural pathologic changes found in a sample of skin tissue from a eczema vaccinatum lesion, which had manifested itself after this patient had received a smallpox vaccination.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]
References
- ↑ "Smallpox disease overview".
- ↑ Massung RF, Liu LI, Qi J, Knight JC, Yuran TE, Kerlavage AR; et al. (1994). "Analysis of the complete genome of smallpox variola major virus strain Bangladesh-1975". Virology. 201 (2): 215–40. doi:10.1006/viro.1994.1288. PMID 8184534.
- ↑ Cecil, Russell (2012). Goldman's Cecil medicine. Philadelphia: Elsevier/Saunders. ISBN 1437716040.
- ↑ 4.0 4.1 "Smallpox and its Eradication" (PDF).
- ↑ 5.0 5.1 5.2 Moore, Zack S; Seward, Jane F; Lane, J Michael (2006). "Smallpox". The Lancet. 367 (9508): 425–435. doi:10.1016/S0140-6736(06)68143-9. ISSN 0140-6736.
- ↑ 6.0 6.1 6.2 Breman, Joel G.; Henderson, D.A. (2002). "Diagnosis and Management of Smallpox". New England Journal of Medicine. 346 (17): 1300–1308. doi:10.1056/NEJMra020025. ISSN 0028-4793.
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 0443068399.
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 0443068399.
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 0443068399.
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 0443068399.
- ↑ Cecil, Russell (2012). Goldman's Cecil medicine. Philadelphia: Elsevier/Saunders. ISBN 1437716040.
- ↑ Cecil, Russell (2012). Goldman's Cecil medicine. Philadelphia: Elsevier/Saunders. ISBN 1437716040.
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 0443068399.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 14.6 "Public Health Image Library (PHIL), Centers for Disease Control and Prevention".
Epidemiology and Demographics
|
Smallpox Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Smallpox On the Web |
|
American Roentgen Ray Society Images of Smallpox |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [7]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [8]
Overview
Smallpox was declared eradicated in 1980 by the WHO. The true incidence of smallpox before its eradication is difficult to estimate due to poor reporting from endemic regions, which may have reported only 1-2% of the cases. Children and young adults were the most often affected, especially in regions with low levels of immunity. There is no evidence of gender or race differences in the incidence of the disease. Developing countries had a higher incidence of the disease.[1]
Incidence
The number of new cases, reported to the international health authorities, was often inaccurate. The data obtained from non-endemic countries, with good health services, was probably the most accurate. Yet, according to the Intensified Smallpox Eradication Programme, the reported incidence amounted only to 1-2% of the actual number of cases, which made it impossible to obtain an accurate estimate of the incidence.[1]
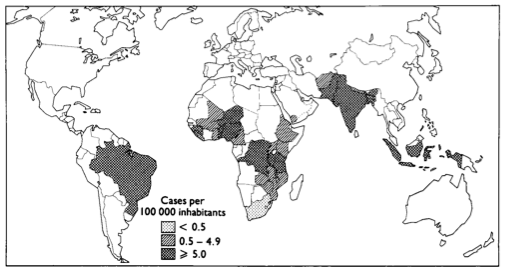
In endemic regions there were periods called epidemic years in which the incidence was much higher. In order to try to justify this discrepancy, several possibilities were evoked, such as:[1]
- Viability of the virus
- Changes in susceptibility of the host
- Social factors, such as dispersion of the population
- Seasonal variation in incidence in relation to eradication
Age
The age adjusted incidence of the disease may vary depending upon the level of acquired immunity in the population. When populations were exposed to the disease for the first time, all ages would be affected. In endemic regions, where there was some previous level of immunity, children and young adults were the most severely affected.[2][1][3]
Gender
Smallpox affected males and females equally.[1][3]
Race
The incidence of smallpox did not differ according to the race.[1][3]
Developed Countries
Developed countries, due to a better and established health system, had lower incidence of smallpox and better reports of new cases to international organizations.[1]
Developing Countries
In developing countries where healthcare facilities are sometimes not trusted by the population, cases were sometimes not reported to public health authorities. Also, vaccination was not sanctioned by some religious beliefs. Taken together, these factors might explain at least in part the higher incidence of smallpox in developing countries.[1]
References
Risk Factors
|
Smallpox Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Smallpox On the Web |
|
American Roentgen Ray Society Images of Smallpox |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [9]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [10]
Overview
People who work in laboratories with the virus are at risk of contracting smallpox. Before its eradication, risk factors for developing smallpox included: physical contact with a patient with the disease, contact with contaminated body fluids, and exposure to contaminated aerosolized particles.[1]
Risk Factors
Prior to Eradication
- Physical contact with someone with smallpox
- Direct contact with infected bodily fluids
- Direct contact with contaminated surfaces
- Exposure to aerosolized particles from someone with smallpox
Present
- Laboratory work with the virus
References
Causes
|
Smallpox Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Smallpox On the Web |
|
American Roentgen Ray Society Images of Smallpox |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [11]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [12]
Overview
Smallpox is caused by the variola virus, a dsDNA virus of the Poxviridae family. There are two forms of this virus with different virulences, as evidenced by their respective death rates. The virus survives in the cold and aerosoled environments, which explains its oral transmission among humans. Humans are the viruses only host which likely facilitated its eradication. Unlike other DNA viruses, smallpox replicates within the cytoplasm, to which it shows tropism.
Taxonomy
Viruses; dsDNA; Poxviridae; Chordopoxvirinae; Orthopoxvirus; Variola vera
Biology
Variola virus, also known as smallpox virus, is an orthopoxvirus, from the family Poxviridae, the largest viruses to infect humans. It is a 200-400 nm dsDNA virus, lacking icosahedral symmetry. The other viruses of the family Poxviridae include:[1]
The viral structure includes:[2][3][4]
- 1 Outer membrane
- 2 lateral bodies
- 1 dsDNA molecule in its core, containing 186,999 base pairs
Variola virus genes are similar to the ones of vaccinia virus. Since there is cross-protection between poxviruses, it was possible to use the second as a vaccine for smallpox virus.[5]
There are 2 forms of variola virus:
- Variola major
- Variola minor
Both strains of the virus share a large amount of genome, yet they differ clinically. This leads to the assumption that the difference in virulence resides in alternate gene expression.[1][6]
Poxviruses survive in cold and dry environments being able to survive in the aerosoled form, and are killed by hospital disinfectants and UV light.[1][6][7][8]
Unlike other DNA viruses, poxviruses replicate within the cytoplasm of the host cell. In order to replicate, poxviruses produce a variety of specialized proteins, not produced by other DNA viruses, the most important of which is a viral-associated DNA-dependent RNA polymerase.
Origin
The date of the origin of the smallpox virus is not settled. It most likely evolved from a rodent virus between 68,000 and 16,000 years ago.[9][10] This broad range of dates is due to the different records used to calibrate the molecular clock. It appears that the smallpox virus derived from a remote zoonosis from another animal host, that is today extinct.[11]
Tropism
Little is known about the mechanism responsible for host species tropism of smallpox virus. The virus is known to bind mammalian cells unspecifically. There appears to be no particular extracellular receptors involved in viral internalization and initial transcription. However, intracellular availability of trans-acting factors and viral capacity to block host cells antiviral response, such as the interferon pathway, are though to be important intracellular factors, determining viral tropism. The overall immune response by the host towards the virus, will be the key determinant of the infection's outcome and potential transmission to other hosts.[11]
Natural reservoir
Humans are the only known natural reservoir of the smallpox virus.[12]
References
- ↑ 1.0 1.1 1.2 Moore, Zack S; Seward, Jane F; Lane, J Michael (2006). "Smallpox". The Lancet. 367 (9508): 425–435. doi:10.1016/S0140-6736(06)68143-9. ISSN 0140-6736.
- ↑ Fields, Bernard (2007). Fields virology. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 0781760607.
- ↑ Massung RF, Liu LI, Qi J, Knight JC, Yuran TE, Kerlavage AR; et al. (1994). "Analysis of the complete genome of smallpox variola major virus strain Bangladesh-1975". Virology. 201 (2): 215–40. doi:10.1006/viro.1994.1288. PMID 8184534.
- ↑ Massung RF, Loparev VN, Knight JC, Totmenin AV, Chizhikov VE, Parsons JM; et al. (1996). "Terminal region sequence variations in variola virus DNA". Virology. 221 (2): 291–300. doi:10.1006/viro.1996.0378. PMID 8661439.
- ↑ Shchelkunov, Sergei N.; Resenchuk, Sergei M.; Totmenin, Alexei V.; Blinov, Vladimir M.; Marennikova, Svetlana S.; Sandakhchiev, Lev S. (1993). "Comparison of the genetic maps of variola and vaccinia viruses". FEBS Letters. 327 (3): 321–324. doi:10.1016/0014-5793(93)81013-P. ISSN 0014-5793.
- ↑ 6.0 6.1 "Smallpox and its Eradication" (PDF).
- ↑ Thomas G (1974). "Air sampling of smallpox virus". J Hyg (Lond). 73 (1): 1–7. PMC 2130554. PMID 4371586.
- ↑ HARPER GJ (1961). "Airborne micro-organisms: survival tests with four viruses". J Hyg (Lond). 59: 479–86. PMC 2134455. PMID 13904777.
- ↑ Esposito, J. J. (2006). "Genome Sequence Diversity and Clues to the Evolution of Variola (Smallpox) Virus". Science. 313 (5788): 807–812. doi:10.1126/science.1125134. ISSN 0036-8075.
- ↑ Li, Y.; Carroll, D. S.; Gardner, S. N.; Walsh, M. C.; Vitalis, E. A.; Damon, I. K. (2007). "On the origin of smallpox: Correlating variola phylogenics with historical smallpox records". Proceedings of the National Academy of Sciences. 104 (40): 15787–15792. doi:10.1073/pnas.0609268104. ISSN 0027-8424.
- ↑ 11.0 11.1 McFadden, Grant (2005). "Poxvirus tropism". Nature Reviews Microbiology. 3 (3): 201–213. doi:10.1038/nrmicro1099. ISSN 1740-1526.
- ↑ "Smallpox disease overview".
Differential Diagnosis
|
Smallpox Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Smallpox On the Web |
|
American Roentgen Ray Society Images of Smallpox |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [13]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [14]
Overview
Prior to its eradication, smallpox would need to be differentiated from other diseases that cause a vesicular rash and a fever including chickenpox (which was often mistaken for smallpox), herpes zoster and erythema multiforme.[1]
Differentiating Smallpox from other Diseases
Different rash-like conditions may be misdiagnosed with smallpox, particularly during the initial maculopapular phase, including:[2]
| Disease | Findings |
|---|---|
| Insect bites | In an insect bite, the insect injects formic acid, which can cause an immediate skin reaction often resulting in a rash and swelling in the injured area, often with formation of vesicles |
| Kawasaki disease | Commonly presents with high and persistent fever, red mucous membranes in mouth, "strawberry tongue", swollen lymph nodes and skin rash in early disease, with peeling off of the skin of the hands, feet and genital area |
| Monkeypox | Presentation is similar to smallpox, although it is often a milder form, with fever, headache, myalgia, back pain, swollen lymph nodes, a general feeling of discomfort, and exhaustion. Within 1 to 3 days (sometimes longer) after the appearance of fever, the patient develops a papular rash, often first on the face. The lesions usually develop through several stages before crusting and falling off. |
| Rubella | Commonly presents with a facial rash which then spreads to the trunk and limbs, fading after 3 days, low grade fever, swollen glands, joint pains, headache and conjunctivitis. The rash disappears after a few days with no staining or peeling of the skin. Forchheimer's sign occurs in 20% of cases, and is characterized by small, red papules on the area of the soft palate |
| Coxsackievirus | The most commonly caused disease is the Coxsackie A disease, presenting as hand, foot and mouth disease. It may be asymptomatic or cause mild symptoms, or it may produce fever and painful blisters in the mouth (herpangina), on the palms and fingers of the hand, or on the soles of the feet. There can also be blisters in the throat or above the tonsils. Adults can also be affected. The rash, which can appear several days after high temperature and painful sore throat, can be itchy and painful, especially on the hands/fingers and bottom of feet. |
| Acne | Typical of teenagers, usually appears on the face and upper neck, but the chest, back and shoulders may have acne as well. The upper arms can also have acne, but lesions found there are often keratosis pilaris, not acne. The typical acne lesions are comedones and inflammatory papules, pustules, and nodules. Some of the large nodules were previously called "cysts" |
| Syphilis | Commonly presents with gneralized systemic symptoms such as malaise, fatigue, headache and fever. Skin eruptions may be subtle and asymptomatic Classically described as 1) non-pruritic bilateral symmetrical mucocutaneous rash; 2) non-tender regional lymphadenopathy; 3) condylomata lata; and 4) patchy alopecia |
| Molluscum contagiosum | Lesions are commonly flesh-colored, dome-shaped, and pearly in appearance. They are often 1-5 millimeters in diameter, with a dimpled center. Generally not painful, but they may itch or become irritated. Picking or scratching the lesions may lead to further infection or scarring. In about 10% of the cases, eczema develops around the lesions. They may occasionally be complicated by secondary bacterial infections |
| Measles | Commonly presents with high fever, coryza and conjunctivitis, with observation of oral mucosal lesions (Koplik's spots), followed by widespread skin rash |
| Atypical measles | Symptoms commonly begin about 7-14 days after infection and present as fever, cough, coryza and conjunctivitis. Observation of Koplik's spots is also a characteristic finding in measles |
| Mononucleosis | Common symptoms include low-grade fever without chills, sore throat, white patches on tonsils and back of the throat, muscle weakness and sometime extreme fatigue, tender lymphadenopathy, petechial hemorrhage and skin rash |
| Erythema toxicum | Common rash in infants, with clustered and vesicular appearance |
| Rat-bite fever | Commonly presents with fever, chills, open sore at the site of the bite and rash, which may show red or purple plaques. |
| Parvovirus B19 | The rash of fifth disease is typically described as "slapped cheeks," with erythema across the cheeks and sparing the nasolabial folds, forehead, and mouth |
| Cytomegalovirus | Common symptoms include sore throat, swollen lymph nodes, fever, headache, fatigue, weakness, muscle pain and loss of appetite |
| Scarlet fever | Commonly includes fever, punctate red macules on the hard and soft palate and uvula (Forchheimer's spots), bright red tongue with a "strawberry" appearance, sore throat and headache and lymphadenopathy |
| Rocky Mountain spotted fever | Symptoms may include maculopapular rash, petechial rash, abdominal pain and joint pain |
| Stevens-Johnson syndrome | Symptoms may include fever, sore throat and fatigue. Commonly presents ulcers and other lesions in the mucous membranes, almost always in the mouth and lips but also in the genital and anal regions. Those in the mouth are usually extremely painful and reduce the patient's ability to eat or drink. Conjunctivitis of the eyes occurs in about 30% of children. A rash of round lesions about an inch across, may arise on the face, trunk, arms and legs, and soles of the feet, but usually not on the scalp. |
| Varicella-zoster virus | Commonly starts as a painful rash on one side of the face or body. The rash forms blisters that typically scab over in 7-10 days and clears up within 2-4 weeks. |
| Chickenpox | Commonly starts with conjunctival and catarrhal symptoms and then characteristic spots appearing in two or three waves, mainly on the body and head, rather than the hands, becoming itchy raw pox (small open sores which heal mostly without scarring). Touching the fluid from a chickenpox blister can also spread the disease. |
| Meningococcemia | Commonly presents with rash, petechiae, headache, confusion, and stiff neck, high fever, mental status changes, nausea and vomiting. |
| Rickettsialpox | First symptom is commonly a bump formed by a mite-bite, eventually resulting in a black, crusty scab. Many of the symptoms are flu-like including fever, chills, weakness and muscle pain but the most distinctive symptom is the rash that breaks out, spanning the person's entire body. |
| Meningitis | Commonly presents with headache, nuchal rigidity, fever, petechiae and altered mental status. |
| Impetigo | Commonly presents with pimple-like lesions surrounded by erythematous skin. Lesions are pustules, filled with pus, which then break down over 4-6 days and form a thick crust. It's often associated with insect bites, cuts, and other forms of trauma to the skin |
References
- ↑ "Smallpox disease overview".
- ↑ Moore, Zack S; Seward, Jane F; Lane, J Michael (2006). "Smallpox". The Lancet. 367 (9508): 425–435. doi:10.1016/S0140-6736(06)68143-9. ISSN 0140-6736.
Natural History, Complications & Prognosis
Complications
Complications of smallpox arise most commonly in the respiratory system and range from simple bronchitis to fatal pneumonia. Respiratory complications tend to develop on about the eighth day of the illness and can be either viral or bacterial in origin. Secondary bacterial infection of the skin is a relatively uncommon complication of smallpox. When this occurs, the fever usually remains elevated.
Other complications include encephalitis (1 in 500 patients), which is more common in adults and may cause temporary disability; permanent pitted scars, most notably on the face; and complications involving the eyes (2% of all cases). Pustules can form on the eyelid, conjunctiva, and cornea, leading to complications such as conjunctivitis, keratitis, corneal ulcer, iritis, iridocylcitis, and optic atrophy. Blindness results in approximately 35% to 40% of eyes affected with keratitis and corneal ulcer. Hemorrhagic smallpox can cause subconjunctival and retinal hemorrhages. In 2% to 5% of young children with smallpox, virions reach the joints and bone, causing osteomyelitis variolosa. Lesions are symmetrical, most common in the elbows, tibia, and fibula, and characteristically cause separation of an epiphysis and marked periosteal reactions. Swollen joints limit movement, and arthritis may lead to limb deformities, ankylosis, malformed bones, flail joints, and stubby fingers.
Prognosis
The overall case-fatality rate for ordinary-type smallpox is about 30%, but varies by pock distribution: ordinary type-confluent is fatal about 50–75% of the time, ordinary-type semi-confluent about 25–50% of the time, in cases where the rash is discrete the case-fatality rate is less than 10%. The overall fatality rate for children younger than 1 year of age is 40%–50%.
Hemorrhagic and flat types have the highest fatality rates. The fatality rate for flat-type is 90% or greater and nearly 100% is observed in cases of hemorrhagic smallpox. The case-fatality rate for variola minor is 1% or less. There is no evidence of chronic or recurrent infection with variola virus.
In fatal cases of ordinary smallpox, death usually occurs between the tenth and sixteenth days of the illness. The cause of death from smallpox is not clear, but the infection is now known to involve multiple organs. Circulating immune complexes, overwhelming viremia, or an uncontrolled immune response may be contributing factors. In early hemorrhagic smallpox, death occurs suddenly about six days after the fever develops. Cause of death in hemorrhagic cases involved heart failure, sometimes accompanied by pulmonary edema. In late hemorrhagic cases, high and sustained viremia, severe platelet loss and poor immune response were often cited as causes of death. In flat smallpox modes of death are similar to those in burns, with loss of fluid, protein and electrolytes beyond the capacity of the body to replace or acquire, and fulminating sepsis.
Diagnosis
{{#ask:Used To Diagnose::Smallpox |?Sort Order |format=list |headers=hide |link=none |sep= | |template=MedicalTestQuery |sort=Sort Order }}
Treatment
{{#ask:Used To Treat::Smallpox |?Sort Order |format=list |headers=hide |link=none |sep= | |template=MedicalTreatmentQuery |sort=Sort Order }} {{#ask:Prevents::Smallpox |?Sort Order |intro= | |format=list |headers=hide |link=none |sep= | |template=MedicalTreatmentQuery2 |sort=Sort Order }}
- Pages with reference errors
- Pages using duplicate arguments in template calls
- CS1 maint: Extra text: authors list
- CS1 maint: Extra text
- CS1 maint: Multiple names: authors list
- CS1 maint: Unrecognized language
- CS1 maint: Explicit use of et al.
- CS1 maint: PMC format
- Disease
- Pediatrics
- Smallpox
- Viral diseases
- Poxviruses
- Needs overview
- Needs content
- Infectious disease
![Hematoxylin and eosin (H&E)-stained tissue sample, reveals some of the histopathologic changes found in a human skin tissue sample from the site of a smallpox lesion. Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]](/images/8/8f/Smallpox-1.jpg)
![hematoxylin and eosin (H&E)-stained tissue sample, reveals some of the histopathologic changes found in a human skin tissue sample from the site of a smallpox lesion. Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]](/images/0/0b/Smallpox-2.jpg)
![This is a chickenpox scab (left), and smallpox scab (right) viewed in profile as a demonstration in comparative morphology. Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]](/images/3/30/Smallpox-5.jpg)
![This image depicts three mounted chickenpox scabs seen from the side revealing the superficiality of these scabs when morphologically compared to a smallpox scab.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]](/images/3/3c/Smallpox-7.jpg)
![Viewed from above, this image depicts a smallpox scab (left), and chickenpox scab (right) as a demonstration in comparative morphology. Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]](/images/e/e9/Smallpox-9.jpg)
![Cytoarchitectural pathologic changes found in a sample of skin tissue from a eczema vaccinatum lesion, which had manifested itself after this patient had received a smallpox vaccination.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]](/images/8/8a/Smallpox-74.jpg)
![Cytoarchitectural pathologic changes found in a sample of skin tissue from a eczema vaccinatum lesion, which had manifested itself after this patient had received a smallpox vaccination.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[14]](/images/6/61/Smallpox-76.jpg)