Pulmonic regurgitation pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
The pathophysiologic mechanism of [[pulmonic regurgitation]] includes [[right ventricular overload]] resulting in right ventricular remodeling and progressive decline in function. The rate of decline in right ventricular [[systolic function]] is affected by associated conditions such as peripheral [[pulmonary artery stenosis]] and [[pulmonary hypertension]] which further increase the severity of [[pulmonary regurgitation]]. | The pathophysiologic mechanism of [[pulmonic regurgitation]] includes [[right ventricular overload]] resulting in the right [[ventricular remodeling]] and progressive decline in function. The rate of decline in right ventricular [[systole|systolic function]] is affected by associated conditions such as peripheral [[pulmonary artery stenosis]] and [[pulmonary hypertension]] which further increase the severity of [[pulmonary regurgitation]]. | ||
==Pathophysiology== | ==Pathophysiology== | ||
The pulmonic regurgitation usually occurs by one of the following mechanisms:<ref>{{cite book | last = Khavandi | first = Ali | title = Essential revision notes for the cardiology KBA | publisher = Oxford University Press | location = Oxford | year = 2014 | isbn = 978-0199654901 }} </ref> | ===Anatomy of and physiology of [[pulmonic valve]]=== | ||
===Pathogenesis=== | |||
The pulmonic regurgitation usually occurs by one of the following mechanisms:<ref>{{cite book | last = Khavandi | first = Ali | title = Essential revision notes for the cardiology KBA | publisher = Oxford University Press | location = Oxford | year = 2014 | isbn = 978-0199654901 }} </ref><ref>{{cite book | last = Khavandi | first = Ali | title = Essential revision notes for the cardiology KBA | publisher = Oxford University Press | location = Oxford | year = 2014 | isbn = 978-0199654901 }}</ref> | |||
===Acquired alteration in the valvular leaflet morphology<ref name="CurtissMiller1983">{{cite journal|last1=Curtiss|first1=E I|last2=Miller|first2=T R|last3=Shapiro|first3=L S|title=Pulmonic regurgitation due to valvular tophi.|journal=Circulation|volume=67|issue=3|year=1983|pages=699–701|issn=0009-7322|doi=10.1161/01.CIR.67.3.699}}</ref>=== | ====Acquired alteration in the valvular leaflet morphology<ref name="CurtissMiller1983">{{cite journal|last1=Curtiss|first1=E I|last2=Miller|first2=T R|last3=Shapiro|first3=L S|title=Pulmonic regurgitation due to valvular tophi.|journal=Circulation|volume=67|issue=3|year=1983|pages=699–701|issn=0009-7322|doi=10.1161/01.CIR.67.3.699}}</ref>==== | ||
*The development of [[pulmonic regurgitation]] due to [[tophus]] valvular vegetations has been reported in a case. The patient reported had long-standing cyanotic [[congenital heart disease]] and developed [[hyperuricemia]] secondary to [[polycythemia]]. The possible mechanism of development of the [[ | *The development of [[pulmonic regurgitation]] due to [[tophus]] valvular vegetations has been reported in a case. The patient reported had long-standing cyanotic [[congenital heart disease]] and developed [[hyperuricemia]] secondary to [[polycythemia]]. The possible mechanism of development of the vegetations involved hemodynamic [[valve|valvular]] trauma in the setting of sustained [[hyperuricemia]] and subsequent [[dystrophic calcification]] at primary [[tophus]] lesion. | ||
====Idiopathic dilatation of the pulmonary artery (IDPA)<ref name="pmid28228295">{{cite journal |vauthors=Malviya A, Jha PK, Kalita JP, Saikia MK, Mishra A |title=Idiopathic dilatation of pulmonary artery: A review |journal=Indian Heart J |volume=69 |issue=1 |pages=119–124 |date=2017 |pmid=28228295 |pmc=5319124 |doi=10.1016/j.ihj.2016.07.009 |url=}}</ref><ref name="pmid27891002">{{cite journal |vauthors=Sharma RK, Talwar D, Gupta SK, Bansal S |title=Idiopathic dilatation of pulmonary artery |journal=Lung India |volume=33 |issue=6 |pages=675–677 |date=2016 |pmid=27891002 |pmc=5112830 |doi=10.4103/0970-2113.192869 |url=}}</ref><ref name="SegallRitter1950">{{cite journal|last1=Segall|first1=S.|last2=Ritter|first2=I. I.|last3=Hwang|first3=W.|title=A Case of Marked Dilatation of the Pulmonary Arterial Tree Associated with Mitral Stenosis|journal=Circulation|volume=1|issue=4|year=1950|pages=777–781|issn=0009-7322|doi=10.1161/01.CIR.1.4.777}}</ref>==== | |||
===Idiopathic dilatation of the pulmonary artery (IDPA)<ref name="pmid28228295">{{cite journal |vauthors=Malviya A, Jha PK, Kalita JP, Saikia MK, Mishra A |title=Idiopathic dilatation of pulmonary artery: A review |journal=Indian Heart J |volume=69 |issue=1 |pages=119–124 |date=2017 |pmid=28228295 |pmc=5319124 |doi=10.1016/j.ihj.2016.07.009 |url=}}</ref><ref name="pmid27891002">{{cite journal |vauthors=Sharma RK, Talwar D, Gupta SK, Bansal S |title=Idiopathic dilatation of pulmonary artery |journal=Lung India |volume=33 |issue=6 |pages=675–677 |date=2016 |pmid=27891002 |pmc=5112830 |doi=10.4103/0970-2113.192869 |url=}}</ref><ref name="SegallRitter1950">{{cite journal|last1=Segall|first1=S.|last2=Ritter|first2=I. I.|last3=Hwang|first3=W.|title=A Case of Marked Dilatation of the Pulmonary Arterial Tree Associated with Mitral Stenosis|journal=Circulation|volume=1|issue=4|year=1950|pages=777–781|issn=0009-7322|doi=10.1161/01.CIR.1.4.777}}</ref>=== | |||
*The exact pathogenesis of dilatation of the [[pulmonary artery]] is not fully understood. The demonstration of the [[disease]] among [[child|pediatric population]] signals the [[congenital]] nature of the [[etiology]]. Main [[pulmonary artery]] and the origin of its right and left main pulmonary arteries are majorly affected. It is thought that [[pulmonary artery]] dilatation is mediated by the unequal division of truncus arteriosus communis. Other proposed mechanisms include maldevelopment of the whole [[pulmonary tree]] and the association of hypoplastic [[aorta]] with dilated. | *The exact pathogenesis of dilatation of the [[pulmonary artery]] is not fully understood. The demonstration of the [[disease]] among [[child|pediatric population]] signals the [[congenital]] nature of the [[etiology]]. Main [[pulmonary artery]] and the origin of its right and left main pulmonary arteries are majorly affected. It is thought that [[pulmonary artery]] dilatation is mediated by the unequal division of truncus arteriosus communis. Other proposed mechanisms include maldevelopment of the whole [[pulmonary tree]] and the association of hypoplastic [[aorta]] with dilated. | ||
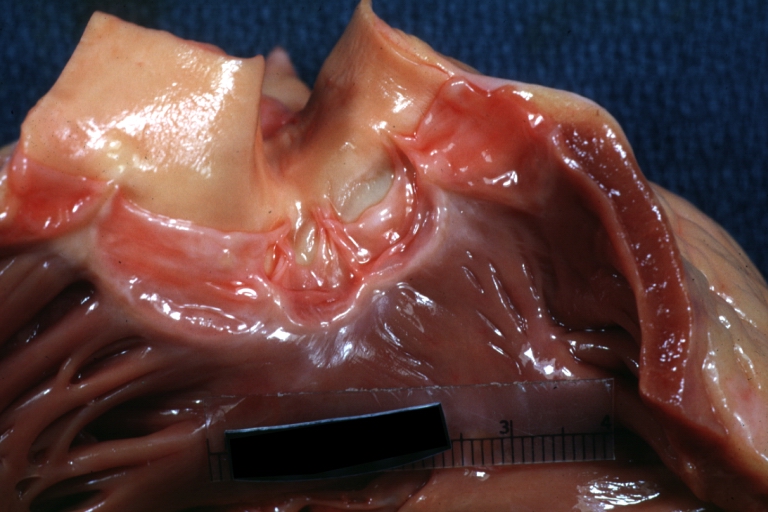
=== | [[Image:Quadricuspid pulmonary valve.jpg|thumb|left|Quadricuspid pulmonary valve (one of the congenital causes of [[PR]] - Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology http://www.peir.net]] | ||
*It is thought that the development of [[pulmonary artery]] aneurysm is mediated by either the congenital weakness or cystic [[tunica media|medial]] degeneration of the [[pulmonary artery]] walls. An association between cystic [[tunica media|medial]] degeneration and increased hemodynamic forces then leads to [[aneurysm]] formation. Pulmonary artery [[aneurysms]] have been associated with structural cardiac and vascular abnormalities, [[vasculitis]], and [[infection]] (such as [[syphilis]]. | ====Congenital absence or malformation of the valve<ref name="BouzasKilner2005">{{cite journal|last1=Bouzas|first1=Beatriz|last2=Kilner|first2=Philip J.|last3=Gatzoulis|first3=Michael A.|title=Pulmonary regurgitation: not a benign lesion|journal=European Heart Journal|volume=26|issue=5|year=2005|pages=433–439|issn=0195-668X|doi=10.1093/eurheartj/ehi091}}</ref><ref name="pmid28228295">{{cite journal |vauthors=Malviya A, Jha PK, Kalita JP, Saikia MK, Mishra A |title=Idiopathic dilatation of pulmonary artery: A review |journal=Indian Heart J |volume=69 |issue=1 |pages=119–124 |date=2017 |pmid=28228295 |pmc=5319124 |doi=10.1016/j.ihj.2016.07.009 |url=}}</ref><ref name="pmid27891002">{{cite journal |vauthors=Sharma RK, Talwar D, Gupta SK, Bansal S |title=Idiopathic dilatation of pulmonary artery |journal=Lung India |volume=33 |issue=6 |pages=675–677 |date=2016 |pmid=27891002 |pmc=5112830 |doi=10.4103/0970-2113.192869 |url=}}</ref><ref name="pmid16181901">{{cite journal |vauthors=Deb SJ, Zehr KJ, Shields RC |title=Idiopathic pulmonary artery aneurysm |journal=Ann. Thorac. Surg. |volume=80 |issue=4 |pages=1500–2 |date=October 2005 |pmid=16181901 |doi=10.1016/j.athoracsur.2004.04.011 |url=}}</ref>==== | ||
*Absent [[pulmonary valve]] syndrome (APVS) is rare and involves developmental abnormality and [[dysplasia]] or absolute absence of [[pulmonary valve]] cusps. A variable degree of dilatation/[[aneurysm]] of the main [[pulmonary artery]] always accompanies the disorder. | |||
*It is thought that the development of [[pulmonary artery]] aneurysm is mediated by either the congenital weakness or cystic [[tunica media|medial]] degeneration of the [[pulmonary artery]] walls. An association between cystic [[tunica media|medial]] degeneration and increased hemodynamic forces then leads to [[aneurysm]] formation. Pulmonary artery [[aneurysms]] have been associated with structural cardiac and vascular abnormalities, [[vasculitis]], and [[infection]] (such as [[syphilis]]). | |||
*The pathogenesis of Fallot type (APVS) involves either [[agenesis]] of [[ductus arteriosus]] or post pulmonary stenotic dilatation due to increased [[stroke volume]]. | |||
*Quuadricuspid [[pulmonary valve]] is rare but may cause [[PR]]. Thick [[valve|valvular]] leaflets with decreased mobility without complete closure during [[diastole]] may lead to the development of [[PR]].<ref name="pmid12094521">{{cite journal |vauthors=Kotani A, Nakagawa K, Yamamoto T, Hirano Y, Kimura H, Yamada S, Ikawa H, Ishikawa K |title=[Quadricuspid pulmonary valve with valvular stenosis and regurgitation identified by transthoracic echocardiography: a case report] |language=Japanese |journal=J Cardiol |volume=39 |issue=6 |pages=313–9 |date=June 2002 |pmid=12094521 |doi= |url=}}</ref> | |||
= | ====Increasing regurgitation causing [[right ventricle|right ventricular]] volume overload<ref name="pmid26430501">{{cite journal| author=Bigdelian H, Mardani D, Sedighi M| title=The Effect of Pulmonary Valve Replacement (PVR) Surgery on Hemodynamics of Patients Who Underwent Repair of Tetralogy of Fallot (TOF). | journal=J Cardiovasc Thorac Res | year= 2015 | volume= 7 | issue= 3 | pages= 122-5 | pmid=26430501 | doi=10.15171/jcvtr.2015.26 | pmc=4586599 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26430501 }} </ref>==== | ||
===Increasing regurgitation causing [[right ventricle|right ventricular]] volume overload<ref name="pmid26430501">{{cite journal| author=Bigdelian H, Mardani D, Sedighi M| title=The Effect of Pulmonary Valve Replacement (PVR) Surgery on Hemodynamics of Patients Who Underwent Repair of Tetralogy of Fallot (TOF). | journal=J Cardiovasc Thorac Res | year= 2015 | volume= 7 | issue= 3 | pages= 122-5 | pmid=26430501 | doi=10.15171/jcvtr.2015.26 | pmc=4586599 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26430501 }} </ref>=== | * Patients with [[pulmonic regurgitation]] develop chronic [[right ventricle|right ventricular]] overload resulting in right [[Ventricular remodeling|ventricular remodeling]] and progressive decline in function. The rate of decline in right ventricular [[systole|systolic function]] is affected by associated conditions such as peripheral [[pulmonary artery stenosis]] and [[pulmonary hypertension]] which further increase the severity of pulmonary regurgitation. Among patients with increased [[pulmonary artery pressure]] from dysfunction of [[left ventricle]] or residual [[pulmonary artery stenosis]] increases the severity of [[pulmonary regurgitation]]. Progressive dilation of the [[right ventricle]] results in functional [[tricuspid regurgitation]] and increases the risk of developing [[arrhythmias]]. | ||
* Patients with [[pulmonic regurgitation]] develop chronic [[right ventricular | |||
*The [[Diastolic blood pressure|diastolic pressure]] difference between [[right ventricle]] and [[pulmonary artery]] is usually very small and steers the pulmonic valve regurgitation. The right ventricular stiffness due to [[right ventricular hypertrophy]] (such as in [[Tetralogy of Fallot]]) and [[fibrosis]], increases the ventricular [[diastolic pressure]], decreasing the gradient thus causing regurge. A slight increase in the intrathoracic pressure (such as among [[ventilated]] patients) can accentuate the pulmonary regurgitation considerably.<ref name="pmid17569817">{{cite journal| author=Chaturvedi RR, Redington AN| title=Pulmonary regurgitation in congenital heart disease. | journal=Heart | year= 2007 | volume= 93 | issue= 7 | pages= 880-9 | pmid=17569817 | doi=10.1136/hrt.2005.075234 | pmc=1994453 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17569817 }} </ref> | *The [[Diastolic blood pressure|diastolic pressure]] difference between [[right ventricle]] and [[pulmonary artery]] is usually very small and steers the pulmonic valve regurgitation. The right ventricular stiffness due to [[right ventricular hypertrophy]] (such as in [[Tetralogy of Fallot]]) and [[fibrosis]], increases the ventricular [[diastolic pressure]], decreasing the gradient thus causing regurge. A slight increase in the intrathoracic pressure (such as among [[ventilated]] patients) can accentuate the pulmonary regurgitation considerably.<ref name="pmid17569817">{{cite journal| author=Chaturvedi RR, Redington AN| title=Pulmonary regurgitation in congenital heart disease. | journal=Heart | year= 2007 | volume= 93 | issue= 7 | pages= 880-9 | pmid=17569817 | doi=10.1136/hrt.2005.075234 | pmc=1994453 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17569817 }} </ref> | ||
*The severity of [[regurgitant jet]] is dependent on:<ref name="pmid26430501">{{cite journal| author=Bigdelian H, Mardani D, Sedighi M| title=The Effect of Pulmonary Valve Replacement (PVR) Surgery on Hemodynamics of Patients Who Underwent Repair of Tetralogy of Fallot (TOF). | journal=J Cardiovasc Thorac Res | year= 2015 | volume= 7 | issue= 3 | pages= 122-5 | pmid=26430501 | doi=10.15171/jcvtr.2015.26 | pmc=4586599 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26430501 }} </ref> | *The severity of [[regurgitant jet]] is dependent on:<ref name="pmid26430501">{{cite journal| author=Bigdelian H, Mardani D, Sedighi M| title=The Effect of Pulmonary Valve Replacement (PVR) Surgery on Hemodynamics of Patients Who Underwent Repair of Tetralogy of Fallot (TOF). | journal=J Cardiovasc Thorac Res | year= 2015 | volume= 7 | issue= 3 | pages= 122-5 | pmid=26430501 | doi=10.15171/jcvtr.2015.26 | pmc=4586599 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26430501 }} </ref> | ||
| Line 29: | Line 31: | ||
**[[Right ventricle]] [[diastolic]] [[compliance]] | **[[Right ventricle]] [[diastolic]] [[compliance]] | ||
**Duration of [[right ventricular]] [[diastole]] | **Duration of [[right ventricular]] [[diastole]] | ||
==== | |||
===Genetics=== | |||
*25% cases of absent [[pulmonary valve]] syndrome (APVS) are associated with [[Chromosome abnormality|chromosomal anomalies]] such as [[Trisomy 21]], [[Trisomy 13]], [[chromosome]] 6 and 7 deletions.<ref name="pmid24843213">{{cite journal |vauthors=Grewal DS, Chamoli SC, Saxena S |title=Absent pulmonary valve syndrome - Antenatal diagnosis |journal=Med J Armed Forces India |volume=70 |issue=2 |pages=198–200 |date=April 2014 |pmid=24843213 |pmc=4017172 |doi=10.1016/j.mjafi.2013.07.002 |url=}}</ref> | |||
*22q11 microdeletion has been shown to be associated with 25% cases of APVS.<ref name="pmid15386602">{{cite journal |vauthors=Volpe P, Paladini D, Marasini M, Buonadonna AL, Russo MG, Caruso G, Marzullo A, Arciprete P, Martinelli P, Gentile M |title=Characteristics, associations and outcome of absent pulmonary valve syndrome in the fetus |journal=Ultrasound Obstet Gynecol |volume=24 |issue=6 |pages=623–8 |date=November 2004 |pmid=15386602 |doi=10.1002/uog.1729 |url=}}</ref> | |||
===Associated conditions=== | |||
Isolated [[PR]] is uncommon and is usually demonstrated with other [[valve|valvular]] abnormalities or in certain conditions. The most important conditions/[[diseases]] associated with [[PR]] include: | |||
*[[TOF]]: Surgical repair of [[pulmonic stenosis]] associated with [[TOF]] may lead to [[PR]]. Post [[TOF]] repair, [[PR]] is a common complication. | |||
*[[Marfan syndrome]] | |||
| | *[[Rheumatic heart disease]] | ||
*[[Syphilis]] | |||
*[[Carcinoid syndrome|Carcinoid heart disease]] | |||
* | ===Gross pathology=== | ||
* | *On gross pathology vegetative lesions on the [[pulmonic valve]] leaflets may be observed in a [[patient]] with [[acquired]] alteration in the [[valve|valvular]] leaflet [[morphology]].<ref name="CurtissMiller1983">{{cite journal|last1=Curtiss|first1=E I|last2=Miller|first2=T R|last3=Shapiro|first3=L S|title=Pulmonic regurgitation due to valvular tophi.|journal=Circulation|volume=67|issue=3|year=1983|pages=699–701|issn=0009-7322|doi=10.1161/01.CIR.67.3.699}}</ref> | ||
===Microscopic pathology=== | |||
* | *In polarized light microscopy of the material taken from the [[pulmonic valve]], [[Gout diagnostic study of choice|negatively birefringent crystals]] may be observed in [[acquired]] alteration in the [[valve|valvular]] leaflet [[morphology]].<ref name="CurtissMiller1983">{{cite journal|last1=Curtiss|first1=E I|last2=Miller|first2=T R|last3=Shapiro|first3=L S|title=Pulmonic regurgitation due to valvular tophi.|journal=Circulation|volume=67|issue=3|year=1983|pages=699–701|issn=0009-7322|doi=10.1161/01.CIR.67.3.699}}</ref> | ||
* | |||
* | |||
|} | |||
==References== | ==References== | ||
{{Reflist}} | {{Reflist|2}} | ||
==See Also== | ==See Also== | ||
Revision as of 20:13, 3 August 2020
|
Pulmonic regurgitation Microchapters |
|
Diagnosis |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Aravind Kuchkuntla, M.B.B.S[2], Aysha Anwar, M.B.B.S[3]
Overview
The pathophysiologic mechanism of pulmonic regurgitation includes right ventricular overload resulting in the right ventricular remodeling and progressive decline in function. The rate of decline in right ventricular systolic function is affected by associated conditions such as peripheral pulmonary artery stenosis and pulmonary hypertension which further increase the severity of pulmonary regurgitation.
Pathophysiology
Anatomy of and physiology of pulmonic valve
Pathogenesis
The pulmonic regurgitation usually occurs by one of the following mechanisms:[1][2]
Acquired alteration in the valvular leaflet morphology[3]
- The development of pulmonic regurgitation due to tophus valvular vegetations has been reported in a case. The patient reported had long-standing cyanotic congenital heart disease and developed hyperuricemia secondary to polycythemia. The possible mechanism of development of the vegetations involved hemodynamic valvular trauma in the setting of sustained hyperuricemia and subsequent dystrophic calcification at primary tophus lesion.
Idiopathic dilatation of the pulmonary artery (IDPA)[4][5][6]
- The exact pathogenesis of dilatation of the pulmonary artery is not fully understood. The demonstration of the disease among pediatric population signals the congenital nature of the etiology. Main pulmonary artery and the origin of its right and left main pulmonary arteries are majorly affected. It is thought that pulmonary artery dilatation is mediated by the unequal division of truncus arteriosus communis. Other proposed mechanisms include maldevelopment of the whole pulmonary tree and the association of hypoplastic aorta with dilated.
Congenital absence or malformation of the valve[7][4][5][8]
- Absent pulmonary valve syndrome (APVS) is rare and involves developmental abnormality and dysplasia or absolute absence of pulmonary valve cusps. A variable degree of dilatation/aneurysm of the main pulmonary artery always accompanies the disorder.
- It is thought that the development of pulmonary artery aneurysm is mediated by either the congenital weakness or cystic medial degeneration of the pulmonary artery walls. An association between cystic medial degeneration and increased hemodynamic forces then leads to aneurysm formation. Pulmonary artery aneurysms have been associated with structural cardiac and vascular abnormalities, vasculitis, and infection (such as syphilis).
- The pathogenesis of Fallot type (APVS) involves either agenesis of ductus arteriosus or post pulmonary stenotic dilatation due to increased stroke volume.
- Quuadricuspid pulmonary valve is rare but may cause PR. Thick valvular leaflets with decreased mobility without complete closure during diastole may lead to the development of PR.[9]
Increasing regurgitation causing right ventricular volume overload[10]
- Patients with pulmonic regurgitation develop chronic right ventricular overload resulting in right ventricular remodeling and progressive decline in function. The rate of decline in right ventricular systolic function is affected by associated conditions such as peripheral pulmonary artery stenosis and pulmonary hypertension which further increase the severity of pulmonary regurgitation. Among patients with increased pulmonary artery pressure from dysfunction of left ventricle or residual pulmonary artery stenosis increases the severity of pulmonary regurgitation. Progressive dilation of the right ventricle results in functional tricuspid regurgitation and increases the risk of developing arrhythmias.
- The diastolic pressure difference between right ventricle and pulmonary artery is usually very small and steers the pulmonic valve regurgitation. The right ventricular stiffness due to right ventricular hypertrophy (such as in Tetralogy of Fallot) and fibrosis, increases the ventricular diastolic pressure, decreasing the gradient thus causing regurge. A slight increase in the intrathoracic pressure (such as among ventilated patients) can accentuate the pulmonary regurgitation considerably.[11]
- The severity of regurgitant jet is dependent on:[10]
- Size of the regurgitant orifice
- Afterload of the right ventricle
- Right ventricle diastolic compliance
- Duration of right ventricular diastole
Genetics
- 25% cases of absent pulmonary valve syndrome (APVS) are associated with chromosomal anomalies such as Trisomy 21, Trisomy 13, chromosome 6 and 7 deletions.[12]
- 22q11 microdeletion has been shown to be associated with 25% cases of APVS.[13]
Associated conditions
Isolated PR is uncommon and is usually demonstrated with other valvular abnormalities or in certain conditions. The most important conditions/diseases associated with PR include:
- TOF: Surgical repair of pulmonic stenosis associated with TOF may lead to PR. Post TOF repair, PR is a common complication.
- Marfan syndrome
- Rheumatic heart disease
- Syphilis
- Carcinoid heart disease
Gross pathology
- On gross pathology vegetative lesions on the pulmonic valve leaflets may be observed in a patient with acquired alteration in the valvular leaflet morphology.[3]
Microscopic pathology
- In polarized light microscopy of the material taken from the pulmonic valve, negatively birefringent crystals may be observed in acquired alteration in the valvular leaflet morphology.[3]
References
- ↑ Khavandi, Ali (2014). Essential revision notes for the cardiology KBA. Oxford: Oxford University Press. ISBN 978-0199654901.
- ↑ Khavandi, Ali (2014). Essential revision notes for the cardiology KBA. Oxford: Oxford University Press. ISBN 978-0199654901.
- ↑ 3.0 3.1 3.2 Curtiss, E I; Miller, T R; Shapiro, L S (1983). "Pulmonic regurgitation due to valvular tophi". Circulation. 67 (3): 699–701. doi:10.1161/01.CIR.67.3.699. ISSN 0009-7322.
- ↑ 4.0 4.1 Malviya A, Jha PK, Kalita JP, Saikia MK, Mishra A (2017). "Idiopathic dilatation of pulmonary artery: A review". Indian Heart J. 69 (1): 119–124. doi:10.1016/j.ihj.2016.07.009. PMC 5319124. PMID 28228295.
- ↑ 5.0 5.1 Sharma RK, Talwar D, Gupta SK, Bansal S (2016). "Idiopathic dilatation of pulmonary artery". Lung India. 33 (6): 675–677. doi:10.4103/0970-2113.192869. PMC 5112830. PMID 27891002.
- ↑ Segall, S.; Ritter, I. I.; Hwang, W. (1950). "A Case of Marked Dilatation of the Pulmonary Arterial Tree Associated with Mitral Stenosis". Circulation. 1 (4): 777–781. doi:10.1161/01.CIR.1.4.777. ISSN 0009-7322.
- ↑ Bouzas, Beatriz; Kilner, Philip J.; Gatzoulis, Michael A. (2005). "Pulmonary regurgitation: not a benign lesion". European Heart Journal. 26 (5): 433–439. doi:10.1093/eurheartj/ehi091. ISSN 0195-668X.
- ↑ Deb SJ, Zehr KJ, Shields RC (October 2005). "Idiopathic pulmonary artery aneurysm". Ann. Thorac. Surg. 80 (4): 1500–2. doi:10.1016/j.athoracsur.2004.04.011. PMID 16181901.
- ↑ Kotani A, Nakagawa K, Yamamoto T, Hirano Y, Kimura H, Yamada S, Ikawa H, Ishikawa K (June 2002). "[Quadricuspid pulmonary valve with valvular stenosis and regurgitation identified by transthoracic echocardiography: a case report]". J Cardiol (in Japanese). 39 (6): 313–9. PMID 12094521.
- ↑ 10.0 10.1 Bigdelian H, Mardani D, Sedighi M (2015). "The Effect of Pulmonary Valve Replacement (PVR) Surgery on Hemodynamics of Patients Who Underwent Repair of Tetralogy of Fallot (TOF)". J Cardiovasc Thorac Res. 7 (3): 122–5. doi:10.15171/jcvtr.2015.26. PMC 4586599. PMID 26430501.
- ↑ Chaturvedi RR, Redington AN (2007). "Pulmonary regurgitation in congenital heart disease". Heart. 93 (7): 880–9. doi:10.1136/hrt.2005.075234. PMC 1994453. PMID 17569817.
- ↑ Grewal DS, Chamoli SC, Saxena S (April 2014). "Absent pulmonary valve syndrome - Antenatal diagnosis". Med J Armed Forces India. 70 (2): 198–200. doi:10.1016/j.mjafi.2013.07.002. PMC 4017172. PMID 24843213.
- ↑ Volpe P, Paladini D, Marasini M, Buonadonna AL, Russo MG, Caruso G, Marzullo A, Arciprete P, Martinelli P, Gentile M (November 2004). "Characteristics, associations and outcome of absent pulmonary valve syndrome in the fetus". Ultrasound Obstet Gynecol. 24 (6): 623–8. doi:10.1002/uog.1729. PMID 15386602.