Systole (medicine)
Template:WikiDoc Cardiology News Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
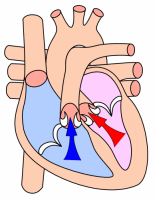
Systole is the contraction of heart chambers, driving blood out of the chambers. The chamber most often discussed is the left ventricle. However, all four chambers of the heart undergo systole and diastole in a timed fashion so that blood is propelled forward through the cardiovascular system.
Types
Electrical vs. mechanical
Electrical systole is the electrical activity that stimulates the myocardium of the chambers of the heart to create an action potential to have the muscles contract. This is soon followed by Mechanical systole, which is the mechanical contraction of the heart.
Atrial
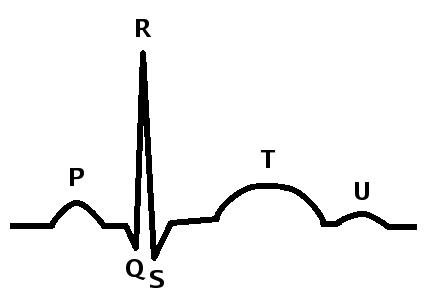
Atrial systole is the contraction of the myocardium of the left and right atria. Electrical systole of the atria begins with the onset of the P wave on the ECG.
Atrial systole, which normally occurs in the late portion of ventricular diastole, causes increased pressure in the atrium and added blood flow into the ventricles. This added blood flow is known as atrial kick, and is absent if there is loss of normal electrical conduction in the heart, such as during atrial fibrillation, atrial flutter, and complete heart block. Aortic and pulmonary valves are closed. Mitral and tricuspid valves are open due to the increased pressure in the atria.
Ventricular
Ventricular systole is the contraction of the myocardium of the left and right ventricles. Electrical systole of the ventricles begins at the beginning of the QRS complex on the EKG.
At the beginning of ventricular systole, the pressure in the left ventricle increases. This soon eclipses the pressure in the left atrium, closing the mitral valve. The pressure in the left ventricle continues to rise, until the pressure in the ventricle is greater than the pressure in the aorta. This causes the aortic valve to open, allowing the blood to eject into the aorta, to perfuse the end organs of the body.
Physiological mechanism
Systole (or contraction of the heart) is initiated by the electrical cells of the sinoatrial node, which is the heart's natural pacemaker. These cells are activated spontaneously by depolarization of their membranes beyond a certain threshold for excitation. At this point, voltage-gated calcium channels on the cell membrane open and allow calcium ions to pass through, into the sarcoplasm, or interior, of the muscle cell. Some calcium ions bind to receptors on the sarcoplasmic reticulum causing an influx of calcium ions into the sarcoplasm. The calcium ions bind to the troponin, causing a conformation change, breaking the bond between the protein tropomyosin, to which the troponin is attached, and the myosin binding sites. This allows the myosin heads to bind to the myosin binding sites on the actin protein filament and contraction results as the myosin heads draw the actin filaments along, are bound by ATP, causing them to release the actin, and return to their original position, breaking down the ATP into ADP and a phosphate group. The action potential spreads via the passage of sodium ions through the gap junctions that connect the sarcoplasm of adjacent myocardial cells.
Norepinephrine (noradrenaline) is released by the terminal boutons of depolarized sympathetic fibres, at the sinoatrial and atrioventricular nodes.
Norepinephrine diffuses across the synaptic cleft binds to the β1-adrenoreceptors – G-protein linked receptors, consisting of seven transmembrane domains – shifting their equilibrium towards the active state. The receptor changes its conformation and mechanically activates the G-protein which is released. The G-protein is involved in the production of cyclic adenyl monophosphate (cAMP) from adenyl triphosphate (ATP) and this in turn activates the protein kinase (β-adrenoreceptor kinase). β-adrenoreceptor kinase phosphorylates the calcium ion channels in the sarcolemma, so that calcium ion influx is increased when they are activated by the appropriate transmembrane voltage. This will of course, cause more of the calcium receptors in the sarcoplasmic reticulum to be activated, creating a larger flow of calcium ions into the sarcoplasm. More troponin will be bound and more myosin binding sites cleared [of tropomyosin] so that more myosin heads can be recruited for the contraction and a greater force and speed of contraction results.
(Phosphodiesterase catalyses the decomposition of cAMP to AMP so that it is no longer able to activate the protein kinase. AMP will of course, go on to be phosphorylated to ATP and may be recycled.)
Noradrenaline also affects the atrioventricular node, reducing the delay before continuing conduction of the action potential via the bundle of His.