Multifocal atrial tachycardia: Difference between revisions
Sara Mohsin (talk | contribs) |
Sara Mohsin (talk | contribs) No edit summary |
||
| (27 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Multifocal atrial tachycardia}} | ||
{{CMG}} '''Associate Editor-In-Chief:''' {{S.M.}}, {{CZ}}, {{HK}} | |||
{{CMG}} | |||
{{SK}} MAT, Chaotic atrial tachycardia, Supraventricular tachycardia | {{SK}} MAT, Chaotic atrial tachycardia, Supraventricular tachycardia | ||
| Line 270: | Line 255: | ||
*[[Multifocal atrial tachycardia (MAT)|MAT]] is difficult to [[Treatments|treat]] in [[infancy]] but it [[Resolving power|resolves]] [[Frequentist|frequently]] and spontaneously within the first [[year]] of [[life]].<ref name="pmid6737948">{{cite journal| author=Toussaint R, Hofstetter R, von Bernuth G| title=[Multifocal atrial tachycardia in infancy]. | journal=Klin Padiatr | year= 1984 | volume= 196 | issue= 2 | pages= 118-20 | pmid=6737948 | doi=10.1055/s-2007-1025591 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6737948 }} </ref> | *[[Multifocal atrial tachycardia (MAT)|MAT]] is difficult to [[Treatments|treat]] in [[infancy]] but it [[Resolving power|resolves]] [[Frequentist|frequently]] and spontaneously within the first [[year]] of [[life]].<ref name="pmid6737948">{{cite journal| author=Toussaint R, Hofstetter R, von Bernuth G| title=[Multifocal atrial tachycardia in infancy]. | journal=Klin Padiatr | year= 1984 | volume= 196 | issue= 2 | pages= 118-20 | pmid=6737948 | doi=10.1055/s-2007-1025591 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6737948 }} </ref> | ||
==Natural history, Complications | ==Natural history, Complications and Prognosis== | ||
*[[Multifocal atrial tachycardia (MAT)|Multifocal atrial tachycardia]] is considered to be a [[Relatively compact|relatively]] [[benign]] [[Cardiac arrhythmia|arrhythmia]] with [[Likelihood|likely]] good [[outcome]] in the absence of a severe [[Underlying representation|underlying]] [[illness]]. | *[[Multifocal atrial tachycardia (MAT)|Multifocal atrial tachycardia]] is considered to be a [[Relatively compact|relatively]] [[benign]] [[Cardiac arrhythmia|arrhythmia]] with [[Likelihood|likely]] good [[outcome]] in the absence of a severe [[Underlying representation|underlying]] [[illness]]. | ||
*[[Multifocal atrial tachycardia (MAT)|MAT]] can be [[WellPoint|well]] [[Control|controlled]] if [[Treatments|treated]] with [[Appropriate Use Criteria|appropriate]] [[drugs]] along with a suggested long follow-up [[period]]. | *[[Multifocal atrial tachycardia (MAT)|MAT]] can be [[WellPoint|well]] [[Control|controlled]] if [[Treatments|treated]] with [[Appropriate Use Criteria|appropriate]] [[drugs]] along with a suggested long follow-up [[period]]. | ||
| Line 334: | Line 319: | ||
|} | |} | ||
==History and Symptoms== | ===History and Symptoms=== | ||
*Mostly [[patients]] with [[Multifocal atrial tachycardia (MAT)|multifocal atrial tachycardia]] are [[asymptomatic]]. | *Mostly [[patients]] with [[Multifocal atrial tachycardia (MAT)|multifocal atrial tachycardia]] are [[asymptomatic]]. | ||
*[[Multifocal atrial tachycardia (MAT)|MAT]] is often [[Incidental finding|incidentally found]] during the routine [[electrocardiogram]]. | *[[Multifocal atrial tachycardia (MAT)|MAT]] is often [[Incidental finding|incidentally found]] during the routine [[electrocardiogram]]. | ||
| Line 358: | Line 343: | ||
** May progress to [[atrial fibrillation]] | ** May progress to [[atrial fibrillation]] | ||
==Physical Examination== | ===Physical Examination=== | ||
*[[Physical examination]] findings of [[patients]] with [[Multifocal atrial tachycardia (MAT)|multifocal atrial tachycardia]] include: | *[[Physical examination]] findings of [[patients]] with [[Multifocal atrial tachycardia (MAT)|multifocal atrial tachycardia]] include: | ||
**[[Elevated heart rate]] usually greater than 100 [[Beats per minute|bpm]] | **[[Elevated heart rate]] usually greater than 100 [[Beats per minute|bpm]] | ||
| Line 394: | Line 379: | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Non-dihydropyridine calcium channel blocker|Non-dihydropyridine calcium channel blockers]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Non-dihydropyridine calcium channel blocker|Non-dihydropyridine calcium channel blockers]]''' | ||
|Once electrolyte abnormalities have been corrected, possible treatment options include non-dihydropyridine calcium channel blockers | | | ||
* Once all the [[electrolyte abnormalities]] have been [[Corrective|corrected]], [[Possibility theory|possible]] [[Treatments|treatment]] options include [[Non-dihydropyridine calcium channel blocker|non-dihydropyridine calcium channel blockers]]. | |||
* If the [[Multifocal atrial tachycardia (MAT)|MAT]] [[patient]] has an [[Underlying representation|underlying]] [[pulmonary disease]], the [[First-line treatment|first-line agent]] is a [[non-dihydropyridine calcium channel blocker]] such as [[verapamil]] or [[diltiazem]]. | |||
* These [[drugs]] [[Suppression (eye)|suppress]] the [[atrial]] [[rate]] and decrease [[Conduction System|conduction]] through the [[atrioventricular node]] thus, [[Slow|slowing]] the [[ventricular]] [[rate]], with an [[average]] [[reduction]] in the [[ventricular]] [[rate]] of 31 [[beats per minute]] and reversion of 43% of the [[Multifocal atrial tachycardia (MAT)|MAT]] [[patients]] to [[normal sinus rhythm]]. | |||
*[[Calcium channel blockers]] ([[Calcium channel blocker|CCB]]) should be [[Usage analysis|used]] with caution in [[patients]] with preexisting [[heart failure]] or [[hypotension]] due to negative [[inotropic]] [[Effect size|effects]] and peripheral [[vasodilation]]. | |||
*[[Calcium channel blocker|CCB]] should also be [[Avoidance response|avoided]] in [[patients]] with [[Atrioventricular block|atrioventricular blocks]] unless a [[pacemaker]] has already been [[Implanted pacemaker|implanted]]. | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Beta blockers]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Beta blockers]]''' | ||
| | | | ||
*[[Beta-blockers]] are the [[First-line treatment|first-line agents]] in the [[Treatments|treatment]] of [[Multifocal atrial tachycardia (MAT)|MAT]] [[patients]] with no [[Underlying representation|underlying]] [[pulmonary disease]]. | |||
*[[Beta-blockers]] act by [[Suppression (eye)|suppressing]] the [[ectopic]] [[Focus (optics)|foci]] and thus, [[Reduced|reduce]] the [[Sympathetic nervous system|sympathetic]] [[Stimulated emission|stimulation]] [[Lead|leading]] to a decrease in [[Conduction System|conduction]] through the [[atrioventricular node]], ultimately [[Slow|slowing]] the [[ventricular]] [[Response element|response]]. | |||
* They [[Causes|cause]] an [[average]] decrease in [[heart rate]] of 51 [[beats per minute]] and [[Reversal potential|reversion]] of 79% of the [[Multifocal atrial tachycardia (MAT)|MAT]] [[patients]] to [[normal sinus rhythm]]. | |||
* Only 20% of the [[Multifocal atrial tachycardia (MAT)|MAT]] [[patients]] require long-term [[therapy]] with [[beta-blockers]]. | |||
*[[Beta-blockers]] should be [[Usage analysis|used]] with caution in [[patients]] with an [[Underlying representation|underlying]] [[pulmonary disease]] such as [[Chronic obstructive pulmonary disease|COPD]] and [[decompensated heart failure]] due to an increased [[RiskMetrics|risk]] for [[bronchospasm]] and decreased [[cardiac output]]. | |||
*[[Beta-blockers]] should be [[Avoidance response|avoided]] in [[patients]] with [[atrioventricular]] blocks unless a [[pacemaker]] has already been [[Implanted pacemaker|implanted]]. | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Antiarrhythmic drugs]]<ref name="pmid30536490">{{cite journal| author=Sakurai K, Takahashi K, Nakayashiro M| title=Combined flecainide and sotalol therapy for multifocal atrial tachycardia in cardio-facio-cutaneous syndrome. | journal=Pediatr Int | year= 2018 | volume= 60 | issue= 11 | pages= 1036-1037 | pmid=30536490 | doi=10.1111/ped.13695 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30536490 }} </ref><ref name="pmid8916490" /><ref name="pmid11455238">{{cite journal| author=Pierce WJ, McGroary K| title=Multifocal atrial tachycardia and Ibutilide. | journal=Am J Geriatr Cardiol | year= 2001 | volume= 10 | issue= 4 | pages= 193-5 | pmid=11455238 | doi=10.1111/j.1076-7460.2001.00016.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11455238 }} </ref>''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Antiarrhythmic drugs]]<ref name="pmid30536490">{{cite journal| author=Sakurai K, Takahashi K, Nakayashiro M| title=Combined flecainide and sotalol therapy for multifocal atrial tachycardia in cardio-facio-cutaneous syndrome. | journal=Pediatr Int | year= 2018 | volume= 60 | issue= 11 | pages= 1036-1037 | pmid=30536490 | doi=10.1111/ped.13695 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30536490 }} </ref><ref name="pmid8916490" /><ref name="pmid11455238">{{cite journal| author=Pierce WJ, McGroary K| title=Multifocal atrial tachycardia and Ibutilide. | journal=Am J Geriatr Cardiol | year= 2001 | volume= 10 | issue= 4 | pages= 193-5 | pmid=11455238 | doi=10.1111/j.1076-7460.2001.00016.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11455238 }} </ref>''' | ||
| | | | ||
*Combined flecainide and sotalol therapy for multifocal atrial tachycardia | *[[Combination therapy|Combined]] [[flecainide]] and [[sotalol]] [[therapy]] is [[Proof|proven]] [[efficacious]] for [[Multifocal atrial tachycardia (MAT)|multifocal atrial tachycardia]] [[patients]] with the [[cardio]]-[[Facial|facio]]-[[cutaneous]] [[syndrome]]. | ||
* | *The successful [[Treatments|treatment]] of [[Multifocal atrial tachycardia (MAT)|MAT]] with [[ibutilide]] is also demonstrated. | ||
*Antiarrhythmics such as quinidine, procainamide, lidocaine, and phenytoin | *[[Treatments|Treatment]] with a [[Class (biology)|Class]] III [[antiarrhythmic agent]] opposes the [[Frequentist|frequently]] [[Acceptor|accepted]] [[Mechanism (biology)|mechanism]] of [[Trigger|triggered]] [[Activity (chemistry)|activity]] in [[Causes|causing]] this [[Cardiac arrhythmia|arrhythmia]]. | ||
*[[Antiarrhythmics]] such as [[quinidine]], [[procainamide]], [[lidocaine]], and [[phenytoin]] are not yet [[Proof|proven]] successful. | |||
*[[Digitalis]] has also not been [[Proof|proven]] to be beneficial in [[Multifocal atrial tachycardia (MAT)|MAT]] [[Treatments|treatment]]. | |||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Radiofrequency ablation|Radiofrequency]] [[AV nodal ablation]]''' | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Radiofrequency ablation|Radiofrequency]] [[AV nodal ablation]]''' | ||
|In | | | ||
* In a [[Fewmets|few]] [[Selection|selected]] [[Case-based reasoning|cases]] of [[refractory]] [[Multifocal atrial tachycardia (MAT)|multifocal atrial tachycardia]], [[AV nodal ablation]] has been [[Proof|proven]] beneficial. | |||
*According to [[Study design|studies]], an [[average]] [[reduction]] of 56 [[beats per minute]] in the [[ventricular]] [[rate]] is found with [[Adequate stimulus|adequate]] [[control]] of [[ventricular]] [[Response element|response]] in 84% of the [[patients]]. | |||
*However, [[AV nodal ablation]] [[causes]] a [[complete heart block]] and requires the placement of a [[permanent pacemaker]]. | |||
|} | |} | ||
| Line 415: | Line 414: | ||
*[[Patients]] with [[chronic obstructive pulmonary disease]] and [[congestive heart failure]], both [[conditions]] [[Association (statistics)|associated]] with [[Magnesium deficiency (medicine)|magnesium deficiency]] and [[Multifocal atrial tachycardia (MAT)|MAT]], should be [[Treatments|treated]] with [[magnesium]]-sparing [[diuretics]] in order to [[Prevention (medical)|prevent]] [[Magnesium deficiency (medicine)|magnesium deficiency]] [[Lead|leading]] to [[Multifocal atrial tachycardia (MAT)|MAT]].<ref name="pmid3275209">{{cite journal| author=Cohen L, Kitzes R, Shnaider H| title=Multifocal atrial tachycardia responsive to parenteral magnesium. | journal=Magnes Res | year= 1988 | volume= 1 | issue= 3-4 | pages= 239-42 | pmid=3275209 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3275209 }} </ref> | *[[Patients]] with [[chronic obstructive pulmonary disease]] and [[congestive heart failure]], both [[conditions]] [[Association (statistics)|associated]] with [[Magnesium deficiency (medicine)|magnesium deficiency]] and [[Multifocal atrial tachycardia (MAT)|MAT]], should be [[Treatments|treated]] with [[magnesium]]-sparing [[diuretics]] in order to [[Prevention (medical)|prevent]] [[Magnesium deficiency (medicine)|magnesium deficiency]] [[Lead|leading]] to [[Multifocal atrial tachycardia (MAT)|MAT]].<ref name="pmid3275209">{{cite journal| author=Cohen L, Kitzes R, Shnaider H| title=Multifocal atrial tachycardia responsive to parenteral magnesium. | journal=Magnes Res | year= 1988 | volume= 1 | issue= 3-4 | pages= 239-42 | pmid=3275209 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3275209 }} </ref> | ||
==Differentiating Multifocal Atrial Tachycardia | ==Differentiating Multifocal Atrial Tachycardia from other Diseases== | ||
[[Multifocal atrial tachycardia (MAT)|Multifocal atrial tachycardia]] must be [[Differentiate|differentiated]] from the following: | [[Multifocal atrial tachycardia (MAT)|Multifocal atrial tachycardia]] must be [[Differentiate|differentiated]] from the following: | ||
*[[Atrial fibrillation]] (has [[Discrete distribution|discrete]] [[P wave]] [[Morphology (biology)|morphologies]]) | *[[Atrial fibrillation]] (has [[Discrete distribution|discrete]] [[P wave]] [[Morphology (biology)|morphologies]]) | ||
| Line 675: | Line 674: | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Disease]] | |||
[[Category: | |||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Arrhythmias]] | |||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
[[Category: | [[Category:Medicine]] | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Latest revision as of 20:58, 19 August 2020
|
Multifocal atrial tachycardia Microchapters |
|
Differentiating Multifocal Atrial Tachycardia from other Diseases |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor-In-Chief: Sara Mohsin, M.D.[2], Cafer Zorkun, M.D., Ph.D. [3], Syed Hassan A. Kazmi BSc, MD [4]
Synonyms and keywords: MAT, Chaotic atrial tachycardia, Supraventricular tachycardia
Overview
Multifocal atrial tachycardia (MAT) is a cardiac arrhythmia which is specifically a type of supraventricular tachycardia with an irregular, rapid atrial rhythm arising from multiple ectopic foci within the atria with a heart rate exceeding 100 beats per minute. It is characterized by an organized atrial activity yielding three or more different non-sinus P wave morphologies in the same lead with variable or irregular PP, PR and RR intervals. There's an isoelectric baseline between P waves with the most P waves being conducted to the ventricles and some R waves being aberrantly conducted. This variability pattern makes MAT look irregular on the surface ECG, thus oftenly leading to misinterpretion as atrial fibrillation. It is typically seen in elderly patients with a variety of underlying comorbidities, the most common being chronic obstructive pulmonary disease (COPD) and congestive heart failure (CHF) and eventually it develops into atrial fibrillation. A rhythm with similar ECG characteristics but at a slow rate is referred to as multifocal atrial rhythm (MAR). The pathogenesis of MAT is not well understood and the patients are generally asymptomatic with mostly being hemodynamically stable. Typically, no treatment is required beyond treatment of underlying conditions in the majority of the MAT patients. However, it is very important to evaluate such patients as this arrhythmia is a poor prognostic sign in the setting of an acute illness.
Historical Perspective
- In the late 1960s, the term ''MAT'' became a commonplace terminology.[1]
- In 2001, Bradley et al reported the clinical course of MAT in infants and children.[2]
Pathophysiology
- The exact pathology behind production of MAT is not well understood, however, the multiple discrete p wave morphologies along with variable PR intervals suggest an atrial pacemaker activity most likely originating from multiple ectopic foci within the atria. Hence, each unique P wave corresponds to a different site of atrial origin.
- The possible underlying mechanism for MAT includes:
- MAT has been reported in >20% of the pediatric patients and up to 60% of the adult patients with coexisting pulmonary disease.
- The following factors are considered to be responsible for the infant-predominant age distribution of MAT and its favorable outcome in idiopathic infant cases:[3][4][5][6][7][8][9]
- The immaturity of both the lungs and the heart in infants.
- The growth and development of bronchopulmonary system and pulmonary vessels in infants continues for at least 2 years (unlike that in adults).
- Immature and vulnerable atrium in utero is considered as an important contributor for fetal MAT detected in utero.
- The following table shows the proposed theories explaining the underlying mechanism of MAT but none of these theories has yet been demonstrated conclusively.
 |
 |
Causes
Following is a list of potential causes of multifocal atrial tachycardia:
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated and include the following:
- Aminophylline toxicity[10]
- Theophylline toxicity[11][12][13][14][15]
- Isoproterenol toxicity
- Congestive heart failure
- Hypokalemia
- Hypoxia
- Myocardial infarction
- Pulmonary embolism
- Sepsis
- Pneumomediastinum (is a complication of surgical emphysema, the MAT gets reverted to sinus rhythm after aspiration of air from mediastinum).[16]
Common Causes
- Chronic obstructive pulmonary disease is the most common cause, as MAT is associated with:[17][18]
- 60% cases of significant lung disease
- 20% patients of acute respiratory failure
- 17% patients hospitalized with COPD
- Chronic renal failure
- Congestive heart failure
- Coronary artery disease
- Diabetes mellitus
- Major surgery
- Hypokalemia
- Hypoxia
- Myocardial infarction
- Valvular heart disease
- Pneumonia
- Pulmonary embolism
- Sepsis
Causes by Organ System
| Cardiovascular | Congestive heart failure, myocardial infarction, |
| Chemical/Poisoning | No underlying causes |
| Dental | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | Aminophylline,, theophylline |
| Ear Nose Throat | No underlying causes |
| Endocrine | Diabetes mellitus |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | No underlying causes |
| Iatrogenic | Postoperative complication |
| Infectious Disease | Pneumonia, sepsis |
| Musculoskeletal/Orthopedic | No underlying causes |
| Neurologic | No underlying causes |
| Nutritional/Metabolic | No underlying causes |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | Lung cancer |
| Ophthalmologic | No underlying causes |
| Overdose/Toxicity | Aminophylline |
| Psychiatric | No underlying causes |
| Pulmonary | Chronic obstructive pulmonary disease, hypoxia, lung cancer, pneumonia, pulmonary embolism |
| Renal/Electrolyte | Chronic renal failure, hypokalemia, hypomagnesemia |
| Rheumatology/Immunology/Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | No underlying causes |
| Urologic | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
- Aminophylline
- Chronic obstructive pulmonary disease
- Chronic renal failure
- Congestive heart failure
- Diabetes mellitus
- Hypercapnia
- Hypokalemia
- Hypomagnesemia
- Hypoxia
- Isoproterenol
- Lung cancer
- Myocardial infarction
- Pneumonia
- Postoperative complication
- Pulmonary embolism
- Sepsis
- Valvular heart disease
Epidemiology and Demographics
- Multifocal atrial tachycardia is a relatively uncommon arrhythmia with low incidence.
- It is seen only in 0.05% to 0.32% of electrocardiograms in general hospital admissions.
- The average age of patients affected by MAT is approximately 70 years.[19]
- Prevalence of pulmonary disease in MAT has been well established in adult MAT patients with up to 60% of the adult patients having a coexisting pulmonary disease, particularly those with chronic obstructive pulmonary disease.
- MAT is a relatively rare condition with clinical features not well established in pediatric ages.
- It accounts for less than 1% of supraventricular tachycardia in infants and children and is reported to affect >20% of the pediatric patients.[20][21]
- Multifocal atrial tachycardia though rare in neonates, can be diagnosed prenatally by cardiotocography.[22][23][24]
- MAT is difficult to treat in infancy but it resolves frequently and spontaneously within the first year of life.[25]
Natural history, Complications and Prognosis
- Multifocal atrial tachycardia is considered to be a relatively benign arrhythmia with likely good outcome in the absence of a severe underlying illness.
- MAT can be well controlled if treated with appropriate drugs along with a suggested long follow-up period.
- In the case of a required pharmacologic intervention, amiodarone is suggested as an excellent choice.[21]
- Baek et al reported in a study that:[26]
- Although most patients with multifocal atrial tachycardia are hemodynamically stable, still MAT is a poor prognostic sign in the setting of an acute illness.
- MAT is associated with a 60% in-hospital mortality rate.
- The mean survival of patients with MAT is just over one year.[27][28]
Diagnosis
The diagnosis of MAT is usually not clinical rather the following electrocardiographic diagnostic criteria is used:
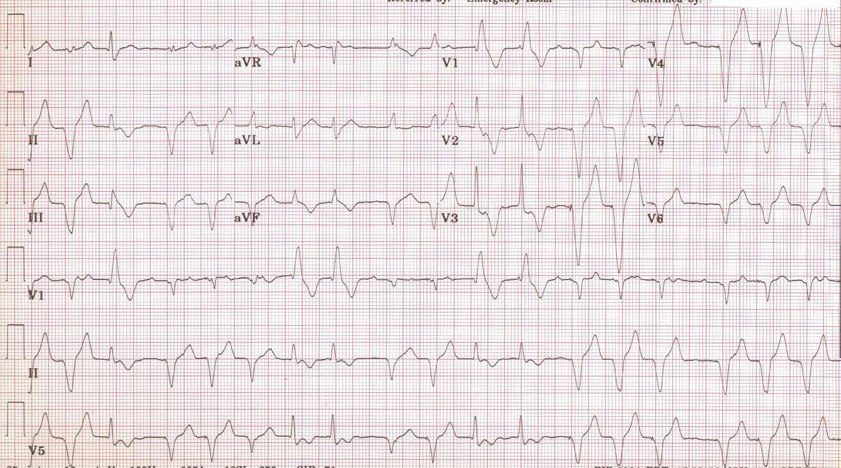
Electrocardiography
ECG of MAT has following characteristics:
- Atrial rate of greater than 100 beats per minute (although some also suggest a threshold of 90 beats per minute for MAT diagnosis)
- Irregularly irregular rhythm
- There are P waves of varying morphology from at least three different foci.
- There is an absence of one dominant atrial pacemaker.
- Variable or irregular PP intervals, RR intervals, and PR intervals (however, variation in PR intervals is not yet included in the diagnostic criteria because of the variation of PR interval depends on the length of the preceding RP interval).[29]
- Can be mistaken for atrial fibrillation if the p waves are of low amplitude.
Other diagnostic workup
- As multifocal atrial tachycardia is mostly associated with the underlying medical conditions such as cardiac and pulmonary disease, so its diagnosis does not typically warrant any additional workup, other than the workup required for the suspected underlying conditions.
- If the arrhythmia persists despite of treating the underlying medical conditions, following tests should be done to check for any signs of infection, anemia, or electrolyte abnormalities such as hypokalemia and hypomagnesemia:
Challenges in MAT pediatric patients
| Challenges | Details |
|---|---|
| How to detect MAT early |
|
| How to control MAT |
|
| How deep to investigate etiologies of MAT[30] |
|
| How to predict another arrhythmia and outcome[2][26][31][32] |
|
History and Symptoms
- Mostly patients with multifocal atrial tachycardia are asymptomatic.
- MAT is often incidentally found during the routine electrocardiogram.
- Once the diagnosis of MAT is made, a thorough history should be obtained with main focus on commonly associated conditions such as cardiac and pulmonary diseases particularly congestive heart failure and chronic obstructive pulmonary disease respectively.
- The clinical manifestations of MAT differ from those of other tachyarrhythmias in that symptoms predominantly relate to the underlying precipitating illness rather than the arrhythmia itself.
- Patients usually present with:
- Irregular heart rate greater than 100 beats per minute (mostly identified only during the physical examination by the health care provider)
- Palpitations (rare)
- Presyncope (rare)
- Syncope (rare)
- Picture of a typical MAT patient is as follows:[4][1]
- Elderly patient
- Decompensated pulmonary disease
- Decompensated heart failure
- Postoperative
- Usually hemodynamically stable (no severe hemodynamic compromise associated with MAT)
- High mortality ECG features in MAT patients include:
- P waves with ≥3 forms
- Atrial rate usually 100 to 200 bpm
- Irregular atrial rate
- Variable PR interval
- Isoelectric baseline between P waves
- May progress to atrial fibrillation
Physical Examination
- Physical examination findings of patients with multifocal atrial tachycardia include:
- Elevated heart rate usually greater than 100 bpm
- Irregularly irregular rhythm
- Hemodynamically stable (mostly)
- As MAT is associated with underlying medical conditions, hence, it is suggested to carry out a general assessment for the signs of cardiopulmonary disease, especially because MAT can trigger the decompensation of underlying cardiac and pulmonary disease.
Treatment
Prevention
Primary Prevention
- Patients with chronic obstructive pulmonary disease and congestive heart failure, both conditions associated with magnesium deficiency and MAT, should be treated with magnesium-sparing diuretics in order to prevent magnesium deficiency leading to MAT.[33]
Differentiating Multifocal Atrial Tachycardia from other Diseases
Multifocal atrial tachycardia must be differentiated from the following:
- Atrial fibrillation (has discrete P wave morphologies)
- Atrial flutter with variable AV node conduction (has regular PP intervals and flutter waves)
- Atrioventricular nodal reentry tachycardia (AVNRT)
- Paroxysmal supraventricular tachycardia
- Premature atrial contractions (PAC)
- Wolff-Parkinson-White syndrome (WPW)
- Ventricular fibrillation (VF)
- Ventricular tachycardia (VT) with frequent premature atrial contractions (has regular PP intervals)
- Wandering atrial pacemaker (has heart rate less than 100 beats per minute)
References
- ↑ 1.0 1.1 Shine KI, Kastor JA, Yurchak PM (1968). "Multifocal atrial tachycardia. Clinical and electrocardiographic features in 32 patients". N Engl J Med. 279 (7): 344–9. doi:10.1056/NEJM196808152790703. PMID 5662166.
- ↑ 2.0 2.1 Bradley DJ, Fischbach PS, Law IH, Serwer GA, Dick M (2001). "The clinical course of multifocal atrial tachycardia in infants and children". J Am Coll Cardiol. 38 (2): 401–8. doi:10.1016/s0735-1097(01)01390-0. PMID 11499730.
- ↑ Huh J (2018). "Clinical Implication of Multifocal Atrial Tachycardia in Children for Pediatric Cardiologist". Korean Circ J. 48 (2): 173–175. doi:10.4070/kcj.2018.0037. PMC 5861009. PMID 29441751.
- ↑ 4.0 4.1 Kastor JA (1990). "Multifocal atrial tachycardia". N Engl J Med. 322 (24): 1713–7. doi:10.1056/NEJM199006143222405. PMID 2188131.
- ↑ Pickoff AS, Singh S, Flinn CJ, McCormack J, Stolfi A, Gelband H (1985). "Atrial vulnerability in the immature canine heart". Am J Cardiol. 55 (11): 1402–6. doi:10.1016/0002-9149(85)90513-2. PMID 3993578.
- ↑ Wang K, Goldfarb BL, Gobel FL, Richman HG (1977). "Multifocal atrial tachycardia". Arch Intern Med. 137 (2): 161–4. PMID 836113.
- ↑ McCord J, Borzak S (1998). "Multifocal atrial tachycardia". Chest. 113 (1): 203–9. doi:10.1378/chest.113.1.203. PMID 9440591.
- ↑ Serra Torres A, Ferriol Bergas J, García De La Villa Redondo B (2009). "[Multifocal atrial tachycardia]". Med Clin (Barc). 132 (3): 106–7. doi:10.1016/j.medcli.2008.09.015. PMID 19211063.
- ↑ Esser H, Kikis D, Trübestein G (1975). "[Proceedings: Multifocal atrial tachycardia]". MMW Munch Med Wochenschr. 117 (20): 837–8. PMID 805961.
- ↑ Kim LK, Lee CS, Jeun JG (2010). "Development of multifocal atrial tachycardia in a patient using aminophylline -A case report-". Korean J Anesthesiol. 59 Suppl: S77–81. doi:10.4097/kjae.2010.59.S.S77. PMC 3030063. PMID 21286467.
- ↑ Sessler CN, Cohen MD (1990). "Cardiac arrhythmias during theophylline toxicity. A prospective continuous electrocardiographic study". Chest. 98 (3): 672–8. doi:10.1378/chest.98.3.672. PMID 2394145.
- ↑ Poukkula A, Korhonen UR, Huikuri H, Linnaluoto M (1989). "Theophylline and salbutamol in combination in patients with obstructive pulmonary disease and concurrent heart disease: effect on cardiac arrhythmias". J Intern Med. 226 (4): 229–34. doi:10.1111/j.1365-2796.1989.tb01385.x. PMID 2681505.
- ↑ Sessler CN (1990). "Theophylline toxicity: clinical features of 116 consecutive cases". Am J Med. 88 (6): 567–76. doi:10.1016/0002-9343(90)90519-j. PMID 2189301.
- ↑ Bittar G, Friedman HS (1991). "The arrhythmogenicity of theophylline. A multivariate analysis of clinical determinants". Chest. 99 (6): 1415–20. doi:10.1378/chest.99.6.1415. PMID 2036824.
- ↑ Levine JH, Michael JR, Guarnieri T (1985). "Multifocal atrial tachycardia: a toxic effect of theophylline". Lancet. 1 (8419): 12–4. doi:10.1016/s0140-6736(85)90964-x. PMID 2856947.
- ↑ Sharma SN, Iyengar SS, Verma M (1993). "Multifocal atrial tachycardia: a complication of pneumomediastinum". J Assoc Physicians India. 41 (1): 50–1. PMID 8340335.
- ↑ Goudis CA, Konstantinidis AK, Ntalas IV, Korantzopoulos P (2015). "Electrocardiographic abnormalities and cardiac arrhythmias in chronic obstructive pulmonary disease". Int J Cardiol. 199: 264–73. doi:10.1016/j.ijcard.2015.06.096. PMID 26218181.
- ↑ Kothari SA, Apiyasawat S, Asad N, Spodick DH (2005). "Evidence supporting a new rate threshold for multifocal atrial tachycardia". Clin Cardiol. 28 (12): 561–3. doi:10.1002/clc.4960281205. PMC 6654295 Check
|pmc=value (help). PMID 16405199. - ↑ "StatPearls". 2020. PMID 29083603.
- ↑ Lazaros G, Chrysohoou C, Oikonomou E, Tsiachris D, Mazaris S, Venieri E; et al. (2014). "The natural history of multifocal atrial rhythms in elderly outpatients: insights from the "Ikaria study"". Ann Noninvasive Electrocardiol. 19 (5): 483–9. doi:10.1111/anec.12165. PMID 24750225.
- ↑ 21.0 21.1 Hsieh MY, Lee PC, Hwang B, Meng CC (2006). "Multifocal atrial tachycardia in 2 children". J Chin Med Assoc. 69 (9): 439–43. doi:10.1016/S1726-4901(09)70288-6. PMID 17051756.
- ↑ Haenel AF, Olafsson A (1985). "[Multifocal atrial tachycardia in the newborn infant--obstetrical implications]". Z Geburtshilfe Perinatol. 189 (5): 228–31. PMID 4072318.
- ↑ Esterl D, Rösel HD (1987). "[Multifocal (chaotic) atrial tachycardia in a newborn infant]". Zentralbl Gynakol. 109 (14): 919–22. PMID 3660970.
- ↑ Bouziri A, Khaldi A, Hamdi A, Ben Massoud I, Borgi A, Menif K; et al. (2011). "Multifocal atrial tachycardia: an unusual cause of cardiogenic shock in a newborn". Tunis Med. 89 (1): 59–61. PMID 21267831.
- ↑ Toussaint R, Hofstetter R, von Bernuth G (1984). "[Multifocal atrial tachycardia in infancy]". Klin Padiatr. 196 (2): 118–20. doi:10.1055/s-2007-1025591. PMID 6737948.
- ↑ 26.0 26.1 26.2 Baek SM, Chung H, Song MK, Bae EJ, Kim GB, Noh CI (2018). "The Complexity of Pediatric Multifocal Atrial Tachycardia and Its Prognostic Factors". Korean Circ J. 48 (2): 148–158. doi:10.4070/kcj.2017.0179. PMC 5861005. PMID 29441747.
- ↑ "StatPearls". 2020. PMID 30571060.
- ↑ Levin MD, Saitta SC, Gripp KW, Wenger TL, Ganesh J, Kalish JM; et al. (2018). "Nonreentrant atrial tachycardia occurs independently of hypertrophic cardiomyopathy in RASopathy patients". Am J Med Genet A. 176 (8): 1711–1722. doi:10.1002/ajmg.a.38854. PMC 6107379. PMID 30055033.
- ↑ van der Watt MJ, Aboo AA, Millar RN (1995). "A prospective study of electrical cardioversion for sustained tachycardias by emergency unit personnel". S Afr Med J. 85 (6): 508–11. PMID 7652630.
- ↑ Lin AE, Alexander ME, Colan SD, Kerr B, Rauen KA, Noonan J; et al. (2011). "Clinical, pathological, and molecular analyses of cardiovascular abnormalities in Costello syndrome: a Ras/MAPK pathway syndrome". Am J Med Genet A. 155A (3): 486–507. doi:10.1002/ajmg.a.33857. PMID 21344638.
- ↑ 31.0 31.1 Fish FA, Mehta AV, Johns JA (1996). "Characteristics and management of chaotic atrial tachycardia of infancy". Am J Cardiol. 78 (9): 1052–5. doi:10.1016/s0002-9149(96)00536-x. PMID 8916490.
- ↑ Broendberg AK, Nielsen JC, Bjerre J, Pedersen LN, Kristensen J, Henriksen FL; et al. (2017). "Nationwide experience of catecholaminergic polymorphic ventricular tachycardia caused by RyR2 mutations". Heart. 103 (12): 901–909. doi:10.1136/heartjnl-2016-310509. PMID 28237968.
- ↑ 33.0 33.1 Cohen L, Kitzes R, Shnaider H (1988). "Multifocal atrial tachycardia responsive to parenteral magnesium". Magnes Res. 1 (3–4): 239–42. PMID 3275209.
- ↑ 34.0 34.1 Iseri LT, Fairshter RD, Hardemann JL, Brodsky MA (1985). "Magnesium and potassium therapy in multifocal atrial tachycardia". Am Heart J. 110 (4): 789–94. doi:10.1016/0002-8703(85)90458-2. PMID 4050650.
- ↑ Moran JL, Gallagher J, Peake SL, Cunningham DN, Salagaras M, Leppard P (1995). "Parenteral magnesium sulfate versus amiodarone in the therapy of atrial tachyarrhythmias: a prospective, randomized study". Crit Care Med. 23 (11): 1816–24. doi:10.1097/00003246-199511000-00005. PMID 7587256.
- ↑ 36.0 36.1 Ho KM (2008). "Intravenous magnesium for cardiac arrhythmias: jack of all trades". Magnes Res. 21 (1): 65–8. PMID 18557136.
- ↑ Stühlinger HG, Kiss K, Smetana R (2000). "[Significance of magnesium in cardiac arrhythmias]". Wien Med Wochenschr. 150 (15–16): 330–4. PMID 11105328.
- ↑ Zehender M (1996). "[Magnesium as an anti-arrhythmic therapy principle in supraventricular and ventricular cardiac arrhythmias]". Z Kardiol. 85 Suppl 6: 135–45. PMID 9064958.
- ↑ Vester EG (1997). "[Clinico-electrophysiologic effects of magnesium, especially in supraventricular tachycardia]". Herz. 22 Suppl 1: 40–50. doi:10.1007/bf03042654. PMID 9333591.
- ↑ Kantoch MJ, Gulamhusein SS, Sanatani S (2011). "Short- and long-term outcomes in children undergoing radiofrequency catheter ablation before their second birthday". Can J Cardiol. 27 (4): 523.e3–9. doi:10.1016/j.cjca.2010.12.043. PMID 21621374.
- ↑ Sakurai K, Takahashi K, Nakayashiro M (2018). "Combined flecainide and sotalol therapy for multifocal atrial tachycardia in cardio-facio-cutaneous syndrome". Pediatr Int. 60 (11): 1036–1037. doi:10.1111/ped.13695. PMID 30536490.
- ↑ Pierce WJ, McGroary K (2001). "Multifocal atrial tachycardia and Ibutilide". Am J Geriatr Cardiol. 10 (4): 193–5. doi:10.1111/j.1076-7460.2001.00016.x. PMID 11455238.
- ↑ Lankveld TA, Zeemering S, Crijns HJ, Schotten U (July 2014). "The ECG as a tool to determine atrial fibrillation complexity". Heart. 100 (14): 1077–84. doi:10.1136/heartjnl-2013-305149. PMID 24837984.
- ↑ Harris K, Edwards D, Mant J (2012). "How can we best detect atrial fibrillation?". J R Coll Physicians Edinb. 42 Suppl 18: 5–22. doi:10.4997/JRCPE.2012.S02. PMID 22518390.
- ↑ Cosío FG (June 2017). "Atrial Flutter, Typical and Atypical: A Review". Arrhythm Electrophysiol Rev. 6 (2): 55–62. doi:10.15420/aer.2017.5.2. PMC 5522718. PMID 28835836.
- ↑ Katritsis DG, Josephson ME (August 2016). "Classification, Electrophysiological Features and Therapy of Atrioventricular Nodal Reentrant Tachycardia". Arrhythm Electrophysiol Rev. 5 (2): 130–5. doi:10.15420/AER.2016.18.2. PMC 5013176. PMID 27617092.
- ↑ Letsas KP, Weber R, Siklody CH, Mihas CC, Stockinger J, Blum T, Kalusche D, Arentz T (April 2010). "Electrocardiographic differentiation of common type atrioventricular nodal reentrant tachycardia from atrioventricular reciprocating tachycardia via a concealed accessory pathway". Acta Cardiol. 65 (2): 171–6. doi:10.2143/AC.65.2.2047050. PMID 20458824.
- ↑ "Atrioventricular Nodal Reentry Tachycardia (AVNRT) - StatPearls - NCBI Bookshelf".
- ↑ Schernthaner C, Danmayr F, Strohmer B (2014). "Coexistence of atrioventricular nodal reentrant tachycardia with other forms of arrhythmias". Med Princ Pract. 23 (6): 543–50. doi:10.1159/000365418. PMC 5586929. PMID 25196716.
- ↑ Scher DL, Arsura EL (September 1989). "Multifocal atrial tachycardia: mechanisms, clinical correlates, and treatment". Am. Heart J. 118 (3): 574–80. doi:10.1016/0002-8703(89)90275-5. PMID 2570520.
- ↑ Goodacre S, Irons R (March 2002). "ABC of clinical electrocardiography: Atrial arrhythmias". BMJ. 324 (7337): 594–7. doi:10.1136/bmj.324.7337.594. PMC 1122515. PMID 11884328.
- ↑ Lin CY, Lin YJ, Chen YY, Chang SL, Lo LW, Chao TF, Chung FP, Hu YF, Chong E, Cheng HM, Tuan TC, Liao JN, Chiou CW, Huang JL, Chen SA (August 2015). "Prognostic Significance of Premature Atrial Complexes Burden in Prediction of Long-Term Outcome". J Am Heart Assoc. 4 (9): e002192. doi:10.1161/JAHA.115.002192. PMC 4599506. PMID 26316525.
- ↑ Strasburger JF, Cheulkar B, Wichman HJ (December 2007). "Perinatal arrhythmias: diagnosis and management". Clin Perinatol. 34 (4): 627–52, vii–viii. doi:10.1016/j.clp.2007.10.002. PMC 3310372. PMID 18063110.
- ↑ Rao AL, Salerno JC, Asif IM, Drezner JA (July 2014). "Evaluation and management of wolff-Parkinson-white in athletes". Sports Health. 6 (4): 326–32. doi:10.1177/1941738113509059. PMC 4065555. PMID 24982705.
- ↑ Rosner MH, Brady WJ, Kefer MP, Martin ML (November 1999). "Electrocardiography in the patient with the Wolff-Parkinson-White syndrome: diagnostic and initial therapeutic issues". Am J Emerg Med. 17 (7): 705–14. doi:10.1016/s0735-6757(99)90167-5. PMID 10597097.
- ↑ Glinge C, Sattler S, Jabbari R, Tfelt-Hansen J (September 2016). "Epidemiology and genetics of ventricular fibrillation during acute myocardial infarction". J Geriatr Cardiol. 13 (9): 789–797. doi:10.11909/j.issn.1671-5411.2016.09.006. PMC 5122505. PMID 27899944.
- ↑ Samie FH, Jalife J (May 2001). "Mechanisms underlying ventricular tachycardia and its transition to ventricular fibrillation in the structurally normal heart". Cardiovasc. Res. 50 (2): 242–50. doi:10.1016/s0008-6363(00)00289-3. PMID 11334828.
- ↑ Adabag AS, Luepker RV, Roger VL, Gersh BJ (April 2010). "Sudden cardiac death: epidemiology and risk factors". Nat Rev Cardiol. 7 (4): 216–25. doi:10.1038/nrcardio.2010.3. PMC 5014372. PMID 20142817.
- ↑ Koplan BA, Stevenson WG (March 2009). "Ventricular tachycardia and sudden cardiac death". Mayo Clin. Proc. 84 (3): 289–97. doi:10.1016/S0025-6196(11)61149-X. PMC 2664600. PMID 19252119.
- ↑ Levis JT (2011). "ECG Diagnosis: Monomorphic Ventricular Tachycardia". Perm J. 15 (1): 65. doi:10.7812/tpp/10-130. PMC 3048638. PMID 21505622.