Lyme disease history and symptoms: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (56 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Lyme disease}} | {{Lyme disease}} | ||
{{CMG}} | {{CMG}};{{AE}}{{Anmol}}, {{IMD}} | ||
==Overview== | ==Overview== | ||
Lyme disease is divided into 3 stages and symptoms are stage specific. | [[Lyme disease]] is divided into 3 stages and the symptoms are stage specific. Initial symptoms include bullseye [[rash]] called [[erythema migrans]], with accompanying flu-like symptoms. Lyme disease can progress to [[cardiovascular]], [[neurological]], [[dermatological]] and/or [[musculoskeletal]] manifestations. Multiple [[erythema migrans]] develops as [[Disseminated disease|disease disseminates]] throughout the body. Most common [[neurological]] manifestation includes [[lymphocytic]] [[meningitis]] and [[cranial nerve palsies]] (usually [[facial nerve palsy]]). Dermatological manifestation includes borrelial lymphocytoma and [[acrodermatitis chronica atrophicans]] appearing in [[Lyme disease history and symptoms#Symptoms|stage 2]] and [[Lyme disease history and symptoms#Symptoms|stage 3 Lyme disease]] respectively. [[Cardiac]] manifestation include [[Lyme carditis]]. [[Musculoskeletal]] manifestation include [[Lyme arthritis]]. There is a difference in clinical features of [[Lyme disease]] in patients living in different geographical regions depending on the genospecies of [[Borrelia burgdorferi]] sensu lato complex causing it. | ||
==History | ==History== | ||
The [[ | *The [[incubation period]] from [[infection]] to the onset of symptoms is usually 1–2 weeks, but can be much shorter (days), or much longer (months to years). Symptoms most often occur from May through September because the nymphal stage of the [[tick]] is responsible for most cases.<ref name="pmid10206627">{{cite journal| author=Falco RC, McKenna DF, Daniels TJ, Nadelman RB, Nowakowski J, Fish D et al.| title=Temporal relation between Ixodes scapularis abundance and risk for Lyme disease associated with erythema migrans. | journal=Am J Epidemiol | year= 1999 | volume= 149 | issue= 8 | pages= 771-6 | pmid=10206627 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10206627 }}</ref> [[Asymptomatic]] [[infection]] can happen, but is uncommon.<ref name="pmid12905137">{{cite journal |author=Steere AC, Sikand VK, Schoen RT, Nowakowski J |title=Asymptomatic infection with Borrelia burgdorferi |journal=Clin. Infect. Dis. |volume=37 |issue=4 |pages=528-32 |year=2003 |pmid=12905137}}</ref> | ||
*The specific areas of focus when obtaining patient history are outlined below: | |||
** [[Tick]] bite | |||
** Vacation, living, or working environment in [[Endemic (epidemiology)|endemic]] areas | |||
**Spending time outdoors (especially in woody or grassy areas) | |||
==Symptoms== | |||
[[Lyme disease]] is divided into 3 stages and symptoms are stage specific. | |||
*Stage 1 - Early localized disease | |||
*Stage 2 - Early disseminated disease | |||
*Stage 3 - Late disseminated disease | |||
===Stage 1 - Early localized disease=== | |||
{| | |||
| | |||
Features of early localized disease includes [[erythema migrans]] and flu-like symptoms. | |||
*'''[[Erythema migrans]] (EM)''' also known as [[erythema chronicum migrans]], bullseye rash, or [[Lyme]] rash develops in around 70% - 80% of patients.<ref name="pmid12802042">{{cite journal| author=Steere AC, Sikand VK| title=The presenting manifestations of Lyme disease and the outcomes of treatment. | journal=N Engl J Med | year= 2003 | volume= 348 | issue= 24 | pages= 2472-4 | pmid=12802042 | doi=10.1056/NEJM200306123482423 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12802042 }} </ref> | |||
**EM begins at the site of a [[tick]] bite after a delay of 3 to 30 days (average is about 7 days). | |||
**EM gradually expands over a period of days reaching up to 12 inches (30 cm) or more across. | |||
**EM may feel warm to touch but is rarely [[Itch|itchy]] or [[Pain|painful]]. | |||
**EM clears as it enlarges, resulting in a target or bullseye appearance. | |||
**EM may appear on any area of the body but is usually present on areas including the [[axilla]], [[inguinal region]], [[popliteal fossa]], or along the belt line. | |||
**The [[rash]] does not represent an [[allergic reaction]] to the bite, but rather a [[skin infection]] with the [[Borrelia burgdorferi|Lyme bacteria]], [[Lyme disease microbiology|''Borrelia burgdorferi'' sensu lato]]. | |||
**An [[infection]] resulting from a ''[[Borrelia mayonii|B. mayonii]]'' [[infection]] may cause a diffuse [[rash]] erupting in red spots, spanning the entire [[body]]. | |||
*Flu-like symptoms including:<ref name="pmid8644761">{{cite journal| author=Nadelman RB, Nowakowski J, Forseter G, Goldberg NS, Bittker S, Cooper D et al.| title=The clinical spectrum of early Lyme borreliosis in patients with culture-confirmed erythema migrans. | journal=Am J Med | year= 1996 | volume= 100 | issue= 5 | pages= 502-8 | pmid=8644761 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8644761 }} </ref> | |||
**[[Fatigue]] | |||
**[[Arthralgia]] | |||
**[[Myalgia]] | |||
**[[Headache]] | |||
**[[Fever]] and/or [[chills]] | |||
**[[Stiff neck]] | |||
**[[Anorexia]] | |||
| | |||
[[Image:Classic Lyme disease rash.jpg|thumb|250px|center|Classic Lyme disease rash - [https://www.cdc.gov/lyme/signs_symptoms/rashes.html Source: CDC.gov]]] | |||
=== | [[Image:Lyme disease Expanding rash with central crust.jpg|thumb|250px|center|Lyme disease, expanding rash with central clearing - [https://www.cdc.gov/lyme/signs_symptoms/rashes.html Source: CDC.gov]]] | ||
|} | |||
===Stage 2 - Early disseminate disease=== | |||
{| | |||
| | |||
Features of early disseminated disease can be divided by organ system and include: | |||
*Multiple [[erythema migrans]]<ref name="pmid158674072">{{cite journal| author=Wormser GP, McKenna D, Carlin J, Nadelman RB, Cavaliere LF, Holmgren D et al.| title=Brief communication: hematogenous dissemination in early Lyme disease. | journal=Ann Intern Med | year= 2005 | volume= 142 | issue= 9 | pages= 751-5 | pmid=15867407 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15867407 }}</ref> | |||
*Neurological symptoms: The triad of [[Neurological|neurologic]] manifestation of [[Lyme disease]] includes [[meningitis]], [[cranial]] [[neuritis]], and radiculoneuritis.<ref name="pmid184528002">{{cite journal|author=Halperin JJ|title=Nervous system Lyme disease.|journal=Infect Dis Clin North Am|year=2008|volume=22|issue=2|pages=261-74, vi|pmid=18452800|doi=10.1016/j.idc.2007.12.009|pmc=|url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18452800}}</ref> | |||
**[[Lymphocyte|Lymphocytic]] [[meningitis]] (most common [[neurological]] symptom) | |||
**[[Cranial nerve palsies|Cranial neuropathies]] (particularly [[facial nerve palsy]]) | |||
**Painful [[radiculitis]] | |||
**[[Mononeuritis multiplex]]<ref name="pmid9066359">{{cite journal| author=England JD, Bohm RP, Roberts ED, Philipp MT| title=Mononeuropathy multiplex in rhesus monkeys with chronic Lyme disease. | journal=Ann Neurol | year= 1997 | volume= 41 | issue= 3 | pages= 375-84 | pmid=9066359 | doi=10.1002/ana.410410313 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9066359 }} </ref> | |||
**[[Altered mental status]]<ref>{{cite journal|author=Chabria SB, Lawrason J|title=Altered mental status, an unusual manifestation of early disseminated Lyme disease: A case report|journal=|volume=1|issue=1|pages=62|year=2007|pmid=17688693|doi=10.1186/1752-1947-1-62}}</ref> | |||
**[[Pseudotumor cerebri]] | |||
**[[Myelitis]] | |||
**[[Chorea]] | |||
**[[Cerebellar ataxia]] | |||
| | |||
[[Image:LymeMultiple rash, disseminated infection.jpg|thumb|250px|right| Disseminated Lyme disease, multiple rash - [https://www.cdc.gov/lyme/signs_symptoms/rashes.html Source: CDC.gov]]] | |||
|} | |||
*[[Cardiac]] manifestations | |||
**[[Palpitation|Palpitations]] | |||
**[[Atrioventricular block|Atrio-ventricular block]] | |||
**[[Myopericarditis]] | |||
**[[Sudden cardiac death]] | |||
**Chronic [[cardiomyopathy]] | |||
*[[Dermatological]] manifestations<ref name="pmid15358567">{{cite journal| author=Mullegger RR| title=Dermatological manifestations of Lyme borreliosis. | journal=Eur J Dermatol | year= 2004 | volume= 14 | issue= 5 | pages= 296-309 | pmid=15358567 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15358567 }} </ref> | |||
**Borrelial lymphocytoma: most common site is [[earlobe]] | |||
*[[Ocular]] manifestations<ref name="pmid14630446">{{cite journal| author=Stanek G, Strle F| title=Lyme borreliosis. | journal=Lancet | year= 2003 | volume= 362 | issue= 9396 | pages= 1639-47 | pmid=14630446 | doi=10.1016/S0140-6736(03)14798-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14630446 }}</ref> | |||
**Primary [[ocular]] symptoms occur due to [[inflammation]] of [[ocular]] tissue. These symptoms include [[conjunctivitis]], [[keratitis]], [[iridocyclitis]], [[retinal]] [[vasculitis]], chorioiditis, and [[optic neuropathy]] (and, extremely rarely, [[episcleritis]], panuveitis, panophthalmitis). | |||
**Secondary [[ocular]] symptoms occur due to extraocular manifestations. These symptoms includes [[Cranial nerve palsies|pareses of cranial nerves]] and [[Orbit (anatomy)|orbital]] [[myositis]]. | |||
===Stage 3 - Late disseminated disease=== | |||
*Features of late disseminated disease can take months to years to manifest after the onset of [[infection]]. | |||
*[[Lyme arthritis]] is dominant months later but chronic [[neurologic]] involvement becomes more obvious years later. | |||
* The symptoms of late [[Disseminated disease|disseminated]] Lyme disease include: | |||
**[[Musculoskeletal]] manifestations: | |||
***[[Lyme arthritis]] | |||
****[[Lyme arthritis]] is the hallmark of stage 3 [[Lyme disease]]. | |||
****Most frequently presented symptom in late disseminated [[Lyme disease]]. | |||
****Commonly affects [[Knee|knee joint]]. | |||
**[[Neurology|Neurological]] manifestations: | |||
***These [[neurological]] symptoms may take months to years to manifest after the [[infection]]. In addition to acute symptoms, neuroborreliosis can manifest as a wide-range of [[Neurology|neurological]] disorders, either [[Central nervous system|central]] or [[Peripheral nervous system|peripheral]] including: | |||
**** [[Encephalopathy]] (sub-acute): Affects [[memory]], [[Mood (psychology)|mood]], [[sleep]], and sometimes with subtle [[language]] disturbances | |||
**** [[Polyneuropathy]] or [[paresthesia]] | |||
**** Leukoencephalitis<ref name="pmid192279822">{{cite journal|year=1991|title=Central nervous system abnormalities in Lyme neuroborreliosis.|url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1922798|journal=Neurology|volume=41|issue=10|pages=1571-82|doi=|pmc=|pmid=1922798|author=Halperin JJ, Volkman DJ, Wu P}}</ref> | |||
**** [[Fasciculation|Muscle twitching]] | |||
**** [[Otolaryngology|Otolaryngologic]] manifestations: [[Neck pain]], [[odynophagia]], head and neck [[dysesthesia]], [[otalgia]], [[tinnitus]], [[hearing loss]], [[vertigo]], [[temporomandibular joint pain]], [[lymphadenopathy]], and [[dysgeusia]]<ref>{{cite journal|year=1988|title=Borrelia infection and vertigo|journal=Acta Otolaryngol.|volume=106|issue=1-2|pages=111-6|pmid=3421091|author=Rosenhall U, Hanner P, Kaijser B}}</ref><ref>{{cite journal|author=Moscatello AL, Worden DL, Nadelman RB, Wormser G, Lucente F|title=Otolaryngologic aspects of Lyme disease|journal=Laryngoscope|volume=101|issue=6 Pt 1|pages=592-5|year=1991|pmid=2041438}}</ref> | |||
***[[Neuropsychiatric]] symptoms often develop much later in the disease's progression, much like tertiary [[neurosyphilis]]<ref name="LogigianKaplan1990">{{cite journal|last1=Logigian|first1=Eric L.|last2=Kaplan|first2=Richard F.|last3=Steere|first3=Allen C.|title=Chronic Neurologic Manifestations of Lyme Disease|journal=New England Journal of Medicine|volume=323|issue=21|year=1990|pages=1438–1444|issn=0028-4793|doi=10.1056/NEJM199011223232102}}</ref> | |||
*** In rare cases, frank [[psychosis|psychoses]] have been attributed to chronic [[Lyme disease]] effects, including misdiagnoses of [[schizophrenia]] and [[bipolar disorder]] | |||
*** [[Panic attack]] and [[anxiety]] can occur, as well as [[delusional]] [[behavior]], including somatoform [[delusions]] sometimes accompanied by a [[depersonalization]] or [[derealization]] syndrome similar to what was seen in the past in the prodromal or early stages of general [[paresis]]<ref>{{cite journal|year=1994|title=Lyme disease: a neuropsychiatric illness|journal=The American journal of psychiatry|volume=151|issue=11|pages=1571-83|pmid=7943444|author=Fallon BA, Nields JA}}{{cite journal|author=Hess A, Buchmann J, Zettl UK, ''et al''|title=Borrelia burgdorferi central nervous system infection presenting as an organic schizophrenialike disorder|journal=Biol. Psychiatry|volume=45|issue=6|pages=795|year=1999|pmid=10188012}})</ref> | |||
**[[Dermatological]] manifestations:<ref name="pmid15358567">{{cite journal| author=Mullegger RR| title=Dermatological manifestations of Lyme borreliosis. | journal=Eur J Dermatol | year= 2004 | volume= 14 | issue= 5 | pages= 296-309 | pmid=15358567 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15358567 }} </ref> | |||
***[[Acrodermatitis chronica atrophicans]] | |||
{| | |||
| | |||
{| | |||
! colspan="2" style="width: 80px; background: #4479BA; text-align: center;" |{{fontcolor|#FFF||Symptoms differentiated on the basis of frequency}} | |||
<ref name="Ciesielski_198922">{{cite journal|year=1989|title=Lyme disease surveillance in the United States, 1983-1986|journal=Rev. Infect. Dis.|volume=11 Suppl 6|issue=|pages=S1435-41|pmid=2682955|author=Ciesielski CA, Markowitz LE, Horsley R, Hightower AW, Russell H, Broome CV}}</ref> | |||
|- | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | '''Common symptoms''' | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | '''Less common symptoms''' | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; " | | |||
*[[Erythema migrans]] ([[erythema chronicum migrans]]) | |||
*Flu-like symptoms | |||
**[[Fatigue]] | |||
**[[Arthralgia]] | |||
**[[Myalgia]] | |||
**[[Headache]] | |||
**[[Fever]] and/or [[chills]] | |||
**[[Stiff neck]] | |||
**[[Anorexia]] | |||
*[[Lyme arthritis]] | |||
*[[Neurological]] manifestations | |||
| style="background: #DCDCDC; padding: 5px; " | | |||
*[[Cardiac]] manifestations | |||
*[[Ocular]] manifestations | |||
*[[Hepatitis]] | |||
|} | |||
| | |||
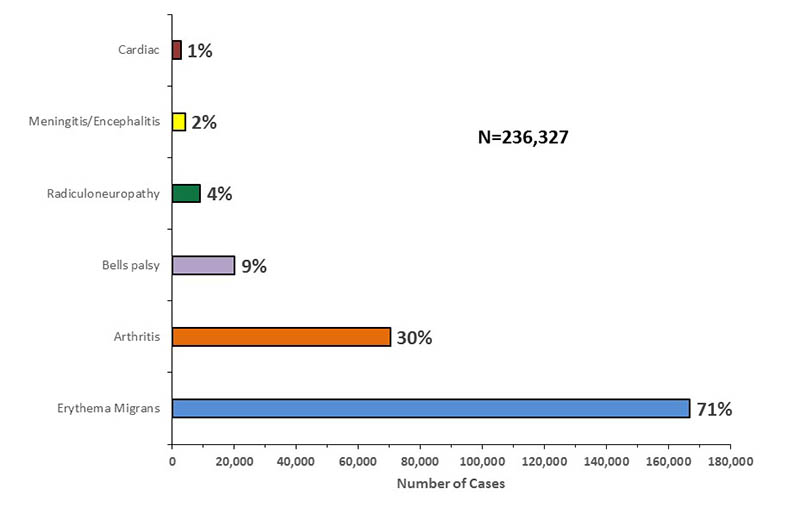
[[image:Symptoms of lyme disease 2001-2015.jpg|center|600px|thumb| Frequency of Lyme disease symptoms, 2001-2015 - [https://www.cdc.gov/lyme/stats/graphs.html Source: CDC.gov/]]] | |||
|} | |||
{| | |||
! colspan="3" style="width: 80px; background: #4479BA; text-align: center;" |{{fontcolor|#FFF||Difference in clinical features in Europe and North America}}<ref name="pmid18452805">{{cite journal| author=Stanek G, Strle F| title=Lyme disease: European perspective. | journal=Infect Dis Clin North Am | year= 2008 | volume= 22 | issue= 2 | pages= 327-39, vii | pmid=18452805 | doi=10.1016/j.idc.2008.01.001 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18452805 }}</ref> | |||
|- | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | '''Features''' | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | '''Europe''' | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | '''North America''' | |||
|- | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | [[Erythema migrans]] | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Single [[lesion]] more frequently | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Multiple [[lesions]] occurs more freuqently | |||
|- | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | Heterogenous [[Disseminated disease|dissemination]] | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Less common | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | More common | |||
|- | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | Borrelial lymphocytoma | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Present | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Absent | |||
|- | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | [[Acrodermatitis chronica atrophicans]] | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Present | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Absent | |||
|- | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | Meningoradiculoneuritis | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | More common | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Less common | |||
|- | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | [[Lyme arthritis]] | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Rarely preceded by [[erythema migrans]] | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Commonly preceded by [[erythema migrans]] | |||
|} | |||
==Erythema Migrans== | |||
{| | |||
| | |||
*'''[[Erythema migrans]] (EM)''', also known as [[erythema chronicum migrans]], bullseye rash, or [[Lyme]] rash, develops in around 70% - 80% of patients.<ref name="pmid12802042">{{cite journal| author=Steere AC, Sikand VK| title=The presenting manifestations of Lyme disease and the outcomes of treatment. | journal=N Engl J Med | year= 2003 | volume= 348 | issue= 24 | pages= 2472-4 | pmid=12802042 | doi=10.1056/NEJM200306123482423 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12802042 }} </ref> | |||
**EM is the [[pathognomonic]] [[rash]] of [[Lyme disease]]. The majority of patients with the [[rash]] do not recall a tick bite. | |||
**EM begins at the site of a [[tick]] bite after a delay of 3 to 30 days (average is about 7 days). | |||
**EM is classically 5 to 6.8 cm in diameter and appears as an annular homogenous [[erythema]] (59%), central [[erythema]] (30%), central clearing (9%), or central [[purpura]] (2%).<ref name="pmid17113969">{{cite journal| author=Feder HM, Abeles M, Bernstein M, Whitaker-Worth D, Grant-Kels JM| title=Diagnosis, treatment, and prognosis of erythema migrans and Lyme arthritis. | journal=Clin Dermatol | year= 2006 | volume= 24 | issue= 6 | pages= 509-20 | pmid=17113969 | doi=10.1016/j.clindermatol.2006.07.012 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17113969 }} </ref> | |||
**EM gradually expands over a period of days reaching up to 12 inches (30 cm) or more across. | |||
**EM may feel warm to touch but is rarely [[Itch|itchy]] or [[Pain|painful]]. | |||
**EM clears as it enlarges, resulting in a target or bullseye appearance. | |||
**EM may appear on any area of the body but is usually present in areas including the [[axilla]], [[inguinal region]], or [[popliteal fossa]]. | |||
**The [[rash]] does not represent an [[allergic reaction]] to the bite, but rather a [[skin infection]] with the [[Borrelia burgdorferi|Lyme bacteria]], [[Lyme disease microbiology|''Borrelia burgdorferi'' sensu lato]]. | |||
**EM resolves in approximately 28 days in untreated patients.<ref name="pmid6859726">{{cite journal| author=Steere AC, Bartenhagen NH, Craft JE, Hutchinson GJ, Newman JH, Rahn DW et al.| title=The early clinical manifestations of Lyme disease. | journal=Ann Intern Med | year= 1983 | volume= 99 | issue= 1 | pages= 76-82 | pmid=6859726 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6859726 }}</ref> | |||
**The characteristic bullseye rash with central clearing is present in about 20% of [[endemic]] cases in the United States, whereas in Europe and the non-endemic United States, 80% of [[rashes]] have central clearing. In [[endemic]] areas of the United States, homogeneously red [[Rash|rashes]] are more frequent.<ref name="pmid11900494">{{cite journal| author=Smith RP, Schoen RT, Rahn DW, Sikand VK, Nowakowski J, Parenti DL et al.| title=Clinical characteristics and treatment outcome of early Lyme disease in patients with microbiologically confirmed erythema migrans. | journal=Ann Intern Med | year= 2002 | volume= 136 | issue= 6 | pages= 421-8 | pmid=11900494 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11900494 }} </ref><ref name="pmid11982300">{{cite journal| author=Edlow JA| title=Erythema migrans. | journal=Med Clin North Am | year= 2002 | volume= 86 | issue= 2 | pages= 239-60 | pmid=11982300 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11982300 }} </ref> | |||
**[[Serological testing|Serologic testing]] is not recommended in patients with EM. Initially, the majority of patients are [[seronegative]].<ref name="pmid17113969">{{cite journal| author=Feder HM, Abeles M, Bernstein M, Whitaker-Worth D, Grant-Kels JM| title=Diagnosis, treatment, and prognosis of erythema migrans and Lyme arthritis. | journal=Clin Dermatol | year= 2006 | volume= 24 | issue= 6 | pages= 509-20 | pmid=17113969 | doi=10.1016/j.clindermatol.2006.07.012 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17113969 }} </ref> | |||
**Multiple [[erythema migrans]] are present in [[disseminated disease]].<ref name="pmid158674072">{{cite journal| author=Wormser GP, McKenna D, Carlin J, Nadelman RB, Cavaliere LF, Holmgren D et al.| title=Brief communication: hematogenous dissemination in early Lyme disease. | journal=Ann Intern Med | year= 2005 | volume= 142 | issue= 9 | pages= 751-5 | pmid=15867407 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15867407 }}</ref> | |||
**Mini [[erythema migrans]]: sometimes, [[erythema migrans]] may be less than 5 cm in diameter. It is an important and atypical sign of early localized [[Lyme disease]].<ref name="pmid16484816">{{cite journal| author=Weber K, Wilske B| title=Mini erythema migrans--a sign of early Lyme borreliosis. | journal=Dermatology | year= 2006 | volume= 212 | issue= 2 | pages= 113-6 | pmid=16484816 | doi=10.1159/000090650 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16484816 }} </ref> | |||
| | |||
<gallery> | |||
Image:Erythema chronicum migrans01.jpg|<small><small>Erythema chronicum migrans - [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=135 Source: Dermatology Atlas.]</small></small> | |||
Image:Bullseye Lyme Disease Rash.jpg|<small><small>Bulls eye lesion - [https://commons.wikimedia.org/wiki/File:Bullseye_Lyme_Disease_Rash.jpg Source: WIKICOMMONS]</small></small> | |||
</gallery> | |||
|} | |||
==Lyme Carditis== | ==Lyme Carditis== | ||
Cardiac involvement occurs in about | *[[Cardiac]] involvement occurs in about 5-10% of untreated [[Lyme disease]] and patients usually have symptoms related to fluctuating degrees of [[atrioventricular block]] ([[First degree AV block|first-degree block]] to [[complete heart block]]) including [[lightheadedness]], [[palpitations]], [[shortness of breath]], [[chest pain]], and [[syncope]].<ref name="pmid228688582">{{cite journal| author=Hu LT| title=In the clinic. Lyme disease. | journal=Ann Intern Med | year= 2012 | volume= 157 | issue= 3 | pages= ITC2-2 - ITC2-16 | pmid=22868858 | doi=10.7326/0003-4819-157-3-20120807-01002 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22868858 }}</ref> | ||
*Less commonly, patients may present with an acute picture of [[left ventricular dysfunction]], [[cardiomegaly]], [[perimyocarditis]], or pancarditis without noticeable [[cardiac murmurs]].<ref name="Steere1989">{{cite journal|last1=Steere|first1=Allen C.|title=Lyme Disease|journal=New England Journal of Medicine|volume=321|issue=9|year=1989|pages=586–596|issn=0028-4793|doi=10.1056/NEJM198908313210906}}</ref> | |||
*Lyme [[carditis]] can occur independently, but it is usually accompanied by other [[cutaneous]], [[joint]], or [[Neurology|neurologic]] features of [[Lyme disease]].<ref name="FishPride2008">{{cite journal|last1=Fish|first1=Airley E.|last2=Pride|first2=Yuri B.|last3=Pinto|first3=Duane S.|title=Lyme Carditis|journal=Infectious Disease Clinics of North America|volume=22|issue=2|year=2008|pages=275–288|issn=08915520|doi=10.1016/j.idc.2007.12.008}}</ref> | |||
==Lyme Arthritis== | |||
*[[Lyme arthritis]] is the hallmark of [[Lyme disease history and symptoms#symptoms|stage 3 Lyme disease]]. | |||
*[[Lyme arthritis]] is most frequently presented symptom in [[Lyme disease history and symptoms#symptoms|late disseminated Lyme disease]]. | |||
*[[Lyme arthritis]] is not necessarily preceded by [[erythema migrans]]. | |||
*[[Lyme arthritis]] may occur due to hematogenous spread of ''[[Borrelia burgdorferi|B. burgdorferi]]'' to multiple joints during early [[infection]]. This might explain migratory [[arthralgia]] during early stages of [[Lyme disease]]. | |||
*It usually takes months to years for [[Lyme disease]] to progress to [[Lyme arthritis]]. | |||
*[[Lyme arthritis]] symptoms range from intermittent attacks of [[monoarthritis]]/[[oligoarthritis]] to persistent [[arthritis]]. | |||
*Intermittent attacks of [[Lyme arthritis]] range from 3 days to 11.5 months in duration with a mean of 3 months.<ref name="pmid36622852">{{cite journal| author=Steere AC, Schoen RT, Taylor E| title=The clinical evolution of Lyme arthritis. | journal=Ann Intern Med | year= 1987 | volume= 107 | issue= 5 | pages= 725-31 | pmid=3662285 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3662285 }}</ref> | |||
*During early years of illness, attacks of [[Lyme arthritis]] are more frequent and longer in duration. Both frequency and duration of attacks subsequently decrease. | |||
* There may months or years of complete remission between each attack of [[Lyme arthritis]]. | |||
*Most of the time, [[Lyme arthritis]] involves large [[Joint|joints]]. The most commonly affected joint is the [[Knee|knee joint]], but any joint can be affected including the [[shoulder]], [[ankle]], [[elbow]], [[temporomandibular joint]], and [[wrist]]. | |||
*[[Tendonitis]] and/or [[bursitis]] may also be present in some patients. Most of the time, [[Joint|joints]] involved are the [[shoulder]], [[knee]], or [[elbow]]. | |||
*Most patients have little/no joint dysfunction after remission of attack. Some patients with persistent [[arthritis]] may show [[Erosion (dental)|erosion]] and permanent damage to [[joint]].<ref name="pmid3662285">{{cite journal| author=Steere AC, Schoen RT, Taylor E| title=The clinical evolution of Lyme arthritis. | journal=Ann Intern Med | year= 1987 | volume= 107 | issue= 5 | pages= 725-31 | pmid=3662285 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3662285 }} </ref> | |||
==Manifestations of Lyme Disease by Stage== | ==Manifestations of Lyme Disease by Stage== | ||
{| | {| align="center" style="font-size:85%;" border="1" cellspacing="0" cellpadding="4" | ||
|+ '''Manifestations of Lyme Disease by Stage<ref name=" | |+ '''Manifestations of Lyme Disease by Stage'''<ref name="Steere1989">{{cite journal|last1=Steere|first1=Allen C.|title=Lyme Disease|journal=New England Journal of Medicine|volume=321|issue=9|year=1989|pages=586–596|issn=0028-4793|doi=10.1056/NEJM198908313210906}}</ref> | ||
|- | |- | ||
| style="background:LightSlateGray; width:15%;" | '''System''' || style="background: #efefef; width:25%;" | '''Stage 1 (Localized Infection)''' || style="background: #efefef; width:25%;" | '''Stage 2 (Disseminated Infection)''' || style="background: #ffdead; width:35%" | '''Stage 3 (Persistent Infection)''' | | style="background:LightSlateGray; width:15%;" | '''System''' || style="background: #efefef; width:25%;" | '''Stage 1 (Localized Infection)''' || style="background: #efefef; width:25%;" | '''Stage 2 (Early Disseminated Infection)''' || style="background: #ffdead; width:35%" | '''Stage 3 (Late Persistent Infection)''' | ||
|- | |- | ||
| ''Skin'' ||valign="top"| | | ''Skin'' || valign="top" | | ||
* [[Erythema migrans]] | |||
| valign="top" | | |||
* Secondary annular [[lesions]] | |||
* [[Malar rash]] | |||
* Diffuse [[erythema]] or [[urticaria]] | |||
* Evanescent [[lesions]] | |||
* Lymphocytoma | |||
| valign="top" | | |||
* [[Acrodermatitis chronica atrophicans]] | |||
* Localized [[scleroderma]]-like [[lesions]] | |||
|- | |- | ||
| ''Musculoskeletal'' | |''Musculoskeletal'' | ||
|— | |||
| valign="top" | | |||
* Migratory [[arthralgia]] | |||
* Brief [[arthritis]] attacks | |||
* [[Myositis]] | |||
* [[Osteomyelitis]] | |||
* [[Panniculitis]] | |||
| valign="top" | | |||
* Prolonged [[arthritis]] attacks | |||
* Chronic [[arthritis]] | |||
* Peripheral [[enthesopathy]] | |||
* [[Periostitis]] or joint subluxations below acrodermatitis | |||
|- | |- | ||
| ''Neurologic'' || — ||valign="top"| | | ''Neurologic'' || — || valign="top" | | ||
* [[Meningitis]] | |||
* Cranial [[neuritis]] or [[Bell's palsy]] | |||
* Motor or sensory radiculoneuritis | |||
* [[Encephalitis]] | |||
* [[Mononeuritis multiplex]] | |||
* [[Pseudotumor cerebri]] | |||
* [[Myelitis]] | |||
* [[Chorea]] | |||
* [[Cerebellar ataxia]] | |||
| valign="top" | | |||
* Chronic [[encephalomyelitis]] | |||
* Spastic parapareses | |||
* [[Ataxic gait]] | |||
* Mental disorders | |||
* Chronic axonal polyradiculopathy | |||
* [[Dementia]] | |||
|- | |- | ||
| ''Lymphatic'' ||valign="top"| | | ''Lymphatic'' || valign="top" | | ||
* Regional [[lymphadenopathy]] | |||
| valign="top" | | |||
* Regional or generalized [[lymphadenopathy]] | |||
* [[Splenomegaly]] | |||
| — | |||
|- | |- | ||
| ''Heart'' || — ||valign="top"| | | ''Heart'' || — || valign="top" | | ||
* [[Atrioventricular block]] | |||
* [[Myopericarditis]] | |||
* Pancarditis | |||
| — | |||
|- | |- | ||
| ''Eyes'' || — ||valign="top"| | | ''Eyes'' || — || valign="top" | | ||
* [[Conjunctivitis]] | |||
* [[Iritis]] | |||
* [[Choroiditis]] | |||
* Retinal [[hemorrhage]] or [[retinal detachment]] | |||
* Panophthalmitis | |||
| valign="top" | | |||
* [[Keratitis]] | |||
|- | |- | ||
| ''Liver'' | |''Liver'' | ||
|— | |||
| | |||
* Mild or recurrent [[hepatitis]] | |||
| — | |||
|- | |- | ||
| ''Respiratory'' || — ||valign="top"| | | ''Respiratory'' || — || valign="top" | | ||
* Nonexudative [[sore throat]] | |||
* Nonproductive [[cough]] | |||
* [[Adult respiratory distress syndrome]] | |||
| — | |||
|- | |- | ||
| ''Kidney'' || — ||valign="top"| | | ''Kidney'' || — || valign="top" | | ||
* Microscopic [[hematuria]] or [[proteinuria]] | |||
| — | |||
|- | |- | ||
| ''Genitourinary'' || — || | | ''Genitourinary'' || — || | ||
* [[Orchitis]] | |||
| — | |||
|- | |- | ||
| '' | | ''Flu-like symptoms systems'' || | ||
* [[Fatigue]] | |||
* [[Arthralgia]] | |||
* [[Myalgia]] | |||
* [[Headache]] | |||
* [[Fever]] and/or [[chills]] | |||
* [[Stiff neck]] | |||
* [[Anorexia]] | |||
| | |||
* Severe [[malaise]] and [[fatigue]] | |||
| | |||
* [[Fatigue]] | |||
|} | |} | ||
<SMALL><span style="align=center">''Adapted from Steere AC. Lyme disease. N Engl J Med. 1989;321:586.''</span></SMALL> | <SMALL><span style="align=center">''Adapted from Steere AC. Lyme disease. N Engl J Med. 1989;321:586.''</span></SMALL> | ||
| Line 53: | Line 317: | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
[[Category:Bacterial diseases]] | [[Category:Bacterial diseases]] | ||
| Line 60: | Line 327: | ||
[[Category:Spirochaetes]] | [[Category:Spirochaetes]] | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Dermatology]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Infectious disease]] | [[Category:Infectious disease]] | ||
[[Category: | [[Category:Ophthalmology]] | ||
[[Category:Neurology]] | |||
[[Category:Cardiology]] | |||
[[Category:Rheumatology]] | |||
Latest revision as of 22:35, 29 July 2020
|
Lyme disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Lyme disease history and symptoms On the Web |
|
American Roentgen Ray Society Images of Lyme disease history and symptoms |
|
Risk calculators and risk factors for Lyme disease history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Anmol Pitliya, M.B.B.S. M.D.[2], Ilan Dock, B.S.
Overview
Lyme disease is divided into 3 stages and the symptoms are stage specific. Initial symptoms include bullseye rash called erythema migrans, with accompanying flu-like symptoms. Lyme disease can progress to cardiovascular, neurological, dermatological and/or musculoskeletal manifestations. Multiple erythema migrans develops as disease disseminates throughout the body. Most common neurological manifestation includes lymphocytic meningitis and cranial nerve palsies (usually facial nerve palsy). Dermatological manifestation includes borrelial lymphocytoma and acrodermatitis chronica atrophicans appearing in stage 2 and stage 3 Lyme disease respectively. Cardiac manifestation include Lyme carditis. Musculoskeletal manifestation include Lyme arthritis. There is a difference in clinical features of Lyme disease in patients living in different geographical regions depending on the genospecies of Borrelia burgdorferi sensu lato complex causing it.
History
- The incubation period from infection to the onset of symptoms is usually 1–2 weeks, but can be much shorter (days), or much longer (months to years). Symptoms most often occur from May through September because the nymphal stage of the tick is responsible for most cases.[1] Asymptomatic infection can happen, but is uncommon.[2]
- The specific areas of focus when obtaining patient history are outlined below:
Symptoms
Lyme disease is divided into 3 stages and symptoms are stage specific.
- Stage 1 - Early localized disease
- Stage 2 - Early disseminated disease
- Stage 3 - Late disseminated disease
Stage 1 - Early localized disease
|
Features of early localized disease includes erythema migrans and flu-like symptoms.
|
  |
Stage 2 - Early disseminate disease
|
Features of early disseminated disease can be divided by organ system and include:
|
 |
- Cardiac manifestations
- Dermatological manifestations[9]
- Borrelial lymphocytoma: most common site is earlobe
- Ocular manifestations[10]
- Primary ocular symptoms occur due to inflammation of ocular tissue. These symptoms include conjunctivitis, keratitis, iridocyclitis, retinal vasculitis, chorioiditis, and optic neuropathy (and, extremely rarely, episcleritis, panuveitis, panophthalmitis).
- Secondary ocular symptoms occur due to extraocular manifestations. These symptoms includes pareses of cranial nerves and orbital myositis.
Stage 3 - Late disseminated disease
- Features of late disseminated disease can take months to years to manifest after the onset of infection.
- Lyme arthritis is dominant months later but chronic neurologic involvement becomes more obvious years later.
- The symptoms of late disseminated Lyme disease include:
- Musculoskeletal manifestations:
- Lyme arthritis
- Lyme arthritis is the hallmark of stage 3 Lyme disease.
- Most frequently presented symptom in late disseminated Lyme disease.
- Commonly affects knee joint.
- Lyme arthritis
- Neurological manifestations:
- These neurological symptoms may take months to years to manifest after the infection. In addition to acute symptoms, neuroborreliosis can manifest as a wide-range of neurological disorders, either central or peripheral including:
- Encephalopathy (sub-acute): Affects memory, mood, sleep, and sometimes with subtle language disturbances
- Polyneuropathy or paresthesia
- Leukoencephalitis[11]
- Muscle twitching
- Otolaryngologic manifestations: Neck pain, odynophagia, head and neck dysesthesia, otalgia, tinnitus, hearing loss, vertigo, temporomandibular joint pain, lymphadenopathy, and dysgeusia[12][13]
- Neuropsychiatric symptoms often develop much later in the disease's progression, much like tertiary neurosyphilis[14]
- In rare cases, frank psychoses have been attributed to chronic Lyme disease effects, including misdiagnoses of schizophrenia and bipolar disorder
- Panic attack and anxiety can occur, as well as delusional behavior, including somatoform delusions sometimes accompanied by a depersonalization or derealization syndrome similar to what was seen in the past in the prodromal or early stages of general paresis[15]
- These neurological symptoms may take months to years to manifest after the infection. In addition to acute symptoms, neuroborreliosis can manifest as a wide-range of neurological disorders, either central or peripheral including:
- Dermatological manifestations:[9]
- Musculoskeletal manifestations:
|
 | ||||||
| Difference in clinical features in Europe and North America[17] | ||
|---|---|---|
| Features | Europe | North America |
| Erythema migrans | Single lesion more frequently | Multiple lesions occurs more freuqently |
| Heterogenous dissemination | Less common | More common |
| Borrelial lymphocytoma | Present | Absent |
| Acrodermatitis chronica atrophicans | Present | Absent |
| Meningoradiculoneuritis | More common | Less common |
| Lyme arthritis | Rarely preceded by erythema migrans | Commonly preceded by erythema migrans |
Erythema Migrans
|
|
Lyme Carditis
- Cardiac involvement occurs in about 5-10% of untreated Lyme disease and patients usually have symptoms related to fluctuating degrees of atrioventricular block (first-degree block to complete heart block) including lightheadedness, palpitations, shortness of breath, chest pain, and syncope.[23]
- Less commonly, patients may present with an acute picture of left ventricular dysfunction, cardiomegaly, perimyocarditis, or pancarditis without noticeable cardiac murmurs.[24]
- Lyme carditis can occur independently, but it is usually accompanied by other cutaneous, joint, or neurologic features of Lyme disease.[25]
Lyme Arthritis
- Lyme arthritis is the hallmark of stage 3 Lyme disease.
- Lyme arthritis is most frequently presented symptom in late disseminated Lyme disease.
- Lyme arthritis is not necessarily preceded by erythema migrans.
- Lyme arthritis may occur due to hematogenous spread of B. burgdorferi to multiple joints during early infection. This might explain migratory arthralgia during early stages of Lyme disease.
- It usually takes months to years for Lyme disease to progress to Lyme arthritis.
- Lyme arthritis symptoms range from intermittent attacks of monoarthritis/oligoarthritis to persistent arthritis.
- Intermittent attacks of Lyme arthritis range from 3 days to 11.5 months in duration with a mean of 3 months.[26]
- During early years of illness, attacks of Lyme arthritis are more frequent and longer in duration. Both frequency and duration of attacks subsequently decrease.
- There may months or years of complete remission between each attack of Lyme arthritis.
- Most of the time, Lyme arthritis involves large joints. The most commonly affected joint is the knee joint, but any joint can be affected including the shoulder, ankle, elbow, temporomandibular joint, and wrist.
- Tendonitis and/or bursitis may also be present in some patients. Most of the time, joints involved are the shoulder, knee, or elbow.
- Most patients have little/no joint dysfunction after remission of attack. Some patients with persistent arthritis may show erosion and permanent damage to joint.[27]
Manifestations of Lyme Disease by Stage
| System | Stage 1 (Localized Infection) | Stage 2 (Early Disseminated Infection) | Stage 3 (Late Persistent Infection) |
| Skin |
|
| |
| Musculoskeletal | — |
|
|
| Neurologic | — |
|
|
| Lymphatic |
|
|
— |
| Heart | — |
|
— |
| Eyes | — |
|
|
| Liver | — |
|
— |
| Respiratory | — |
|
— |
| Kidney | — |
|
— |
| Genitourinary | — | — | |
| Flu-like symptoms systems |
Adapted from Steere AC. Lyme disease. N Engl J Med. 1989;321:586.
References
- ↑ Falco RC, McKenna DF, Daniels TJ, Nadelman RB, Nowakowski J, Fish D; et al. (1999). "Temporal relation between Ixodes scapularis abundance and risk for Lyme disease associated with erythema migrans". Am J Epidemiol. 149 (8): 771–6. PMID 10206627.
- ↑ Steere AC, Sikand VK, Schoen RT, Nowakowski J (2003). "Asymptomatic infection with Borrelia burgdorferi". Clin. Infect. Dis. 37 (4): 528–32. PMID 12905137.
- ↑ 3.0 3.1 Steere AC, Sikand VK (2003). "The presenting manifestations of Lyme disease and the outcomes of treatment". N Engl J Med. 348 (24): 2472–4. doi:10.1056/NEJM200306123482423. PMID 12802042.
- ↑ Nadelman RB, Nowakowski J, Forseter G, Goldberg NS, Bittker S, Cooper D; et al. (1996). "The clinical spectrum of early Lyme borreliosis in patients with culture-confirmed erythema migrans". Am J Med. 100 (5): 502–8. PMID 8644761.
- ↑ 5.0 5.1 Wormser GP, McKenna D, Carlin J, Nadelman RB, Cavaliere LF, Holmgren D; et al. (2005). "Brief communication: hematogenous dissemination in early Lyme disease". Ann Intern Med. 142 (9): 751–5. PMID 15867407.
- ↑ Halperin JJ (2008). "Nervous system Lyme disease". Infect Dis Clin North Am. 22 (2): 261–74, vi. doi:10.1016/j.idc.2007.12.009. PMID 18452800.
- ↑ England JD, Bohm RP, Roberts ED, Philipp MT (1997). "Mononeuropathy multiplex in rhesus monkeys with chronic Lyme disease". Ann Neurol. 41 (3): 375–84. doi:10.1002/ana.410410313. PMID 9066359.
- ↑ Chabria SB, Lawrason J (2007). "Altered mental status, an unusual manifestation of early disseminated Lyme disease: A case report". 1 (1): 62. doi:10.1186/1752-1947-1-62. PMID 17688693.
- ↑ 9.0 9.1 Mullegger RR (2004). "Dermatological manifestations of Lyme borreliosis". Eur J Dermatol. 14 (5): 296–309. PMID 15358567.
- ↑ Stanek G, Strle F (2003). "Lyme borreliosis". Lancet. 362 (9396): 1639–47. doi:10.1016/S0140-6736(03)14798-8. PMID 14630446.
- ↑ Halperin JJ, Volkman DJ, Wu P (1991). "Central nervous system abnormalities in Lyme neuroborreliosis". Neurology. 41 (10): 1571–82. PMID 1922798.
- ↑ Rosenhall U, Hanner P, Kaijser B (1988). "Borrelia infection and vertigo". Acta Otolaryngol. 106 (1–2): 111–6. PMID 3421091.
- ↑ Moscatello AL, Worden DL, Nadelman RB, Wormser G, Lucente F (1991). "Otolaryngologic aspects of Lyme disease". Laryngoscope. 101 (6 Pt 1): 592–5. PMID 2041438.
- ↑ Logigian, Eric L.; Kaplan, Richard F.; Steere, Allen C. (1990). "Chronic Neurologic Manifestations of Lyme Disease". New England Journal of Medicine. 323 (21): 1438–1444. doi:10.1056/NEJM199011223232102. ISSN 0028-4793.
- ↑ Fallon BA, Nields JA (1994). "Lyme disease: a neuropsychiatric illness". The American journal of psychiatry. 151 (11): 1571–83. PMID 7943444.Hess A, Buchmann J, Zettl UK; et al. (1999). "Borrelia burgdorferi central nervous system infection presenting as an organic schizophrenialike disorder". Biol. Psychiatry. 45 (6): 795. PMID 10188012.)
- ↑ Ciesielski CA, Markowitz LE, Horsley R, Hightower AW, Russell H, Broome CV (1989). "Lyme disease surveillance in the United States, 1983-1986". Rev. Infect. Dis. 11 Suppl 6: S1435–41. PMID 2682955.
- ↑ Stanek G, Strle F (2008). "Lyme disease: European perspective". Infect Dis Clin North Am. 22 (2): 327–39, vii. doi:10.1016/j.idc.2008.01.001. PMID 18452805.
- ↑ 18.0 18.1 Feder HM, Abeles M, Bernstein M, Whitaker-Worth D, Grant-Kels JM (2006). "Diagnosis, treatment, and prognosis of erythema migrans and Lyme arthritis". Clin Dermatol. 24 (6): 509–20. doi:10.1016/j.clindermatol.2006.07.012. PMID 17113969.
- ↑ Steere AC, Bartenhagen NH, Craft JE, Hutchinson GJ, Newman JH, Rahn DW; et al. (1983). "The early clinical manifestations of Lyme disease". Ann Intern Med. 99 (1): 76–82. PMID 6859726.
- ↑ Smith RP, Schoen RT, Rahn DW, Sikand VK, Nowakowski J, Parenti DL; et al. (2002). "Clinical characteristics and treatment outcome of early Lyme disease in patients with microbiologically confirmed erythema migrans". Ann Intern Med. 136 (6): 421–8. PMID 11900494.
- ↑ Edlow JA (2002). "Erythema migrans". Med Clin North Am. 86 (2): 239–60. PMID 11982300.
- ↑ Weber K, Wilske B (2006). "Mini erythema migrans--a sign of early Lyme borreliosis". Dermatology. 212 (2): 113–6. doi:10.1159/000090650. PMID 16484816.
- ↑ Hu LT (2012). "In the clinic. Lyme disease". Ann Intern Med. 157 (3): ITC2-2–ITC2-16. doi:10.7326/0003-4819-157-3-20120807-01002. PMID 22868858.
- ↑ 24.0 24.1 Steere, Allen C. (1989). "Lyme Disease". New England Journal of Medicine. 321 (9): 586–596. doi:10.1056/NEJM198908313210906. ISSN 0028-4793.
- ↑ Fish, Airley E.; Pride, Yuri B.; Pinto, Duane S. (2008). "Lyme Carditis". Infectious Disease Clinics of North America. 22 (2): 275–288. doi:10.1016/j.idc.2007.12.008. ISSN 0891-5520.
- ↑ Steere AC, Schoen RT, Taylor E (1987). "The clinical evolution of Lyme arthritis". Ann Intern Med. 107 (5): 725–31. PMID 3662285.
- ↑ Steere AC, Schoen RT, Taylor E (1987). "The clinical evolution of Lyme arthritis". Ann Intern Med. 107 (5): 725–31. PMID 3662285.

