Lyme disease history and symptoms: Difference between revisions
No edit summary |
No edit summary |
||
| Line 21: | Line 21: | ||
{| | {| | ||
| | | | ||
Features of early localized disease includes erythema migrans and flu-like symptoms. | Features of early localized disease includes [[erythema migrans]] and flu-like symptoms. | ||
*'''Erythema migrans (EM)''' also known as | *'''[[Erythema migrans]] (EM)''' also known as [[erythema chronicum migrans]], "bull’s-eye" rash, or [[Lyme]] rash develops in around 70% - 80% of patients.<ref name="pmid12802042">{{cite journal| author=Steere AC, Sikand VK| title=The presenting manifestations of Lyme disease and the outcomes of treatment. | journal=N Engl J Med | year= 2003 | volume= 348 | issue= 24 | pages= 2472-4 | pmid=12802042 | doi=10.1056/NEJM200306123482423 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12802042 }} </ref> | ||
**EM begins at the site of a [[tick]] bite after a delay of 3 to 30 days (average is about 7 days). | **EM begins at the site of a [[tick]] bite after a delay of 3 to 30 days (average is about 7 days). | ||
**EM gradually expands over a period of days reaching up to 12 inches(30 cm)or more across. | **EM gradually expands over a period of days reaching up to 12 inches(30 cm)or more across. | ||
| Line 48: | Line 48: | ||
| | | | ||
Features of early disseminated disease can be divided system wise and includes: | Features of early disseminated disease can be divided system wise and includes: | ||
*Multiple | *Multiple [[erythema migrans]]<ref name="pmid158674072">{{cite journal| author=Wormser GP, McKenna D, Carlin J, Nadelman RB, Cavaliere LF, Holmgren D et al.| title=Brief communication: hematogenous dissemination in early Lyme disease. | journal=Ann Intern Med | year= 2005 | volume= 142 | issue= 9 | pages= 751-5 | pmid=15867407 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15867407 }}</ref> | ||
*Neurological symptoms: The triad of neurologic manifestation of [[Lyme disease]] includes [[meningitis]], [[cranial]] [[neuritis]], and radiculoneuritis.<ref name="pmid184528002">{{cite journal|author=Halperin JJ|title=Nervous system Lyme disease.|journal=Infect Dis Clin North Am|year=2008|volume=22|issue=2|pages=261-74, vi|pmid=18452800|doi=10.1016/j.idc.2007.12.009|pmc=|url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18452800}}</ref> | *Neurological symptoms: The triad of [[Neurological|neurologic]] manifestation of [[Lyme disease]] includes [[meningitis]], [[cranial]] [[neuritis]], and radiculoneuritis.<ref name="pmid184528002">{{cite journal|author=Halperin JJ|title=Nervous system Lyme disease.|journal=Infect Dis Clin North Am|year=2008|volume=22|issue=2|pages=261-74, vi|pmid=18452800|doi=10.1016/j.idc.2007.12.009|pmc=|url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18452800}}</ref> | ||
**[[Lymphocyte|Lymphocytic]] [[meningitis]] (most common neurological symptom) | **[[Lymphocyte|Lymphocytic]] [[meningitis]] (most common [[neurological]] symptom) | ||
**[[Cranial nerve palsies|Cranial neuropathies]] (particularly facial nerve palsy) | **[[Cranial nerve palsies|Cranial neuropathies]] (particularly [[facial nerve palsy]]) | ||
**Painful [[radiculitis]] | **Painful [[radiculitis]] | ||
**[[Mononeuritis multiplex]]<ref name="pmid9066359">{{cite journal| author=England JD, Bohm RP, Roberts ED, Philipp MT| title=Mononeuropathy multiplex in rhesus monkeys with chronic Lyme disease. | journal=Ann Neurol | year= 1997 | volume= 41 | issue= 3 | pages= 375-84 | pmid=9066359 | doi=10.1002/ana.410410313 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9066359 }} </ref> | **[[Mononeuritis multiplex]]<ref name="pmid9066359">{{cite journal| author=England JD, Bohm RP, Roberts ED, Philipp MT| title=Mononeuropathy multiplex in rhesus monkeys with chronic Lyme disease. | journal=Ann Neurol | year= 1997 | volume= 41 | issue= 3 | pages= 375-84 | pmid=9066359 | doi=10.1002/ana.410410313 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9066359 }} </ref> | ||
| Line 76: | Line 76: | ||
===Stage 3 - Late disseminated disease=== | ===Stage 3 - Late disseminated disease=== | ||
*Features of late disseminated disease can take months to years to manifest after the onset of [[infection]]. | *Features of late disseminated disease can take months to years to manifest after the onset of [[infection]]. | ||
*Lyme arthritis is dominant months later but chronic neurologic involvement becomes more obvious years later. | *[[Lyme arthritis]] is dominant months later but chronic [[neurologic]] involvement becomes more obvious years later. | ||
* The symptoms of late disseminated lyme disease includes: | * The symptoms of late [[Disseminated disease|disseminated]] lyme disease includes: | ||
**[[Musculoskeletal]] manifestation: | **[[Musculoskeletal]] manifestation: | ||
***Lyme arthritis | ***[[Lyme arthritis]] | ||
****Lyme arthritis is the hallmark of stage 3 [[Lyme disease]]. | ****[[Lyme arthritis]] is the hallmark of stage 3 [[Lyme disease]]. | ||
****Most frequently presented symptom in late disseminated [[Lyme disease]]. | ****Most frequently presented symptom in late disseminated [[Lyme disease]]. | ||
****Commonly affects [[Knee|knee joint]]. | ****Commonly affects [[Knee|knee joint]]. | ||
| Line 92: | Line 92: | ||
***[[Neuropsychiatric]] symptoms often develop much later in the disease progression, much like tertiary [[neurosyphilis]].<ref name="LogigianKaplan1990">{{cite journal|last1=Logigian|first1=Eric L.|last2=Kaplan|first2=Richard F.|last3=Steere|first3=Allen C.|title=Chronic Neurologic Manifestations of Lyme Disease|journal=New England Journal of Medicine|volume=323|issue=21|year=1990|pages=1438–1444|issn=0028-4793|doi=10.1056/NEJM199011223232102}}</ref> | ***[[Neuropsychiatric]] symptoms often develop much later in the disease progression, much like tertiary [[neurosyphilis]].<ref name="LogigianKaplan1990">{{cite journal|last1=Logigian|first1=Eric L.|last2=Kaplan|first2=Richard F.|last3=Steere|first3=Allen C.|title=Chronic Neurologic Manifestations of Lyme Disease|journal=New England Journal of Medicine|volume=323|issue=21|year=1990|pages=1438–1444|issn=0028-4793|doi=10.1056/NEJM199011223232102}}</ref> | ||
*** In rare cases, frank [[psychosis]] have been attributed to chronic [[Lyme disease]] effects, including misdiagnoses of [[schizophrenia]] and [[bipolar disorder]]. | *** In rare cases, frank [[psychosis]] have been attributed to chronic [[Lyme disease]] effects, including misdiagnoses of [[schizophrenia]] and [[bipolar disorder]]. | ||
*** [[Panic attack]] and [[anxiety]] can occur, also [[delusional]] [[behavior]], including somatoform [[delusions]], sometimes accompanied by a [[depersonalization]] or [[derealization]] syndrome similar to what was seen in the past in the prodromal or early stages of general paresis.<ref>{{cite journal|year=1994|title=Lyme disease: a neuropsychiatric illness|journal=The American journal of psychiatry|volume=151|issue=11|pages=1571-83|pmid=7943444|author=Fallon BA, Nields JA}}{{cite journal|author=Hess A, Buchmann J, Zettl UK, ''et al''|title=Borrelia burgdorferi central nervous system infection presenting as an organic schizophrenialike disorder|journal=Biol. Psychiatry|volume=45|issue=6|pages=795|year=1999|pmid=10188012}})</ref> | *** [[Panic attack]] and [[anxiety]] can occur, also [[delusional]] [[behavior]], including somatoform [[delusions]], sometimes accompanied by a [[depersonalization]] or [[derealization]] syndrome similar to what was seen in the past in the prodromal or early stages of general [[paresis]].<ref>{{cite journal|year=1994|title=Lyme disease: a neuropsychiatric illness|journal=The American journal of psychiatry|volume=151|issue=11|pages=1571-83|pmid=7943444|author=Fallon BA, Nields JA}}{{cite journal|author=Hess A, Buchmann J, Zettl UK, ''et al''|title=Borrelia burgdorferi central nervous system infection presenting as an organic schizophrenialike disorder|journal=Biol. Psychiatry|volume=45|issue=6|pages=795|year=1999|pmid=10188012}})</ref> | ||
**Dermatological manifestation<ref name="pmid15358567">{{cite journal| author=Mullegger RR| title=Dermatological manifestations of Lyme borreliosis. | journal=Eur J Dermatol | year= 2004 | volume= 14 | issue= 5 | pages= 296-309 | pmid=15358567 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15358567 }} </ref> | **[[Dermatological]] manifestation<ref name="pmid15358567">{{cite journal| author=Mullegger RR| title=Dermatological manifestations of Lyme borreliosis. | journal=Eur J Dermatol | year= 2004 | volume= 14 | issue= 5 | pages= 296-309 | pmid=15358567 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15358567 }} </ref> | ||
***Acrodermatitis chronica atrophicans | ***[[Acrodermatitis chronica atrophicans]] | ||
{| | {| | ||
| Line 106: | Line 106: | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; " | | | style="background: #DCDCDC; padding: 5px; " | | ||
*Erythema migrans( | *[[Erythema migrans]] ([[erythema chronicum migrans]]) | ||
*Flu-like symptoms | *Flu-like symptoms | ||
**[[Fatigue]] | **[[Fatigue]] | ||
| Line 116: | Line 116: | ||
**[[Anorexia]] | **[[Anorexia]] | ||
* | *[[Lyme arthritis]] | ||
*Neurological manifestation | *[[Neurological]] manifestation | ||
| style="background: #DCDCDC; padding: 5px; " | | | style="background: #DCDCDC; padding: 5px; " | | ||
*Cardiac manifestations | *[[Cardiac]] manifestations | ||
*Ocular manifestations | *[[Ocular]] manifestations | ||
*Hepatitis | *[[Hepatitis]] | ||
|} | |} | ||
| | | | ||
| Line 134: | Line 134: | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | '''North America''' | | style="background: #F5F5F5; padding: 5px; text-align: center;" | '''North America''' | ||
|- | |- | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | Erythema migrans | | style="background: #F5F5F5; padding: 5px; text-align: center;" | [[Erythema migrans]] | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Single lesion more frequently | | style="background: #DCDCDC; padding: 5px; text-align: center;" |Single lesion more frequently | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Multiple lesions occurs more freuqently | | style="background: #DCDCDC; padding: 5px; text-align: center;" |Multiple lesions occurs more freuqently | ||
|- | |- | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | Heterogenous dissemination | | style="background: #F5F5F5; padding: 5px; text-align: center;" | Heterogenous [[Disseminated disease|dissemination]] | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Less common | | style="background: #DCDCDC; padding: 5px; text-align: center;" | Less common | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | More common | | style="background: #DCDCDC; padding: 5px; text-align: center;" | More common | ||
| Line 146: | Line 146: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Absent | | style="background: #DCDCDC; padding: 5px; text-align: center;" | Absent | ||
|- | |- | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | Acrodermatitis chronica atrophicans | | style="background: #F5F5F5; padding: 5px; text-align: center;" | [[Acrodermatitis chronica atrophicans]] | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Present | | style="background: #DCDCDC; padding: 5px; text-align: center;" | Present | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Absent | | style="background: #DCDCDC; padding: 5px; text-align: center;" | Absent | ||
| Line 154: | Line 154: | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Less common | | style="background: #DCDCDC; padding: 5px; text-align: center;" | Less common | ||
|- | |- | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | Lyme arthritis | | style="background: #F5F5F5; padding: 5px; text-align: center;" | [[Lyme arthritis]] | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Rarely preceded by | | style="background: #DCDCDC; padding: 5px; text-align: center;" | Rarely preceded by [[erythema migrans]] | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Commonly preceded by | | style="background: #DCDCDC; padding: 5px; text-align: center;" | Commonly preceded by [[erythema migrans]] | ||
|} | |} | ||
| Line 162: | Line 162: | ||
{| | {| | ||
| | | | ||
*'''Erythema migrans (EM)''' also known as | *'''[[Erythema migrans]] (EM)''' also known as [[erythema chronicum migrans]], "bull’s-eye" rash, or [[Lyme]] rash develops in around 70% - 80% of patients.<ref name="pmid12802042">{{cite journal| author=Steere AC, Sikand VK| title=The presenting manifestations of Lyme disease and the outcomes of treatment. | journal=N Engl J Med | year= 2003 | volume= 348 | issue= 24 | pages= 2472-4 | pmid=12802042 | doi=10.1056/NEJM200306123482423 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12802042 }} </ref> | ||
**EM is the the pathognomonic rash of Lyme disease. Majority of patients with the rash do not recall tick bite. | **EM is the the pathognomonic [[rash]] of [[Lyme disease]]. Majority of patients with the [[rash]] do not recall tick bite. | ||
**EM begins at the site of a [[tick]] bite after a delay of 3 to 30 days (average is about 7 days). | **EM begins at the site of a [[tick]] bite after a delay of 3 to 30 days (average is about 7 days). | ||
**EM is classically 5 to 6.8 cm in diameter appearing as an annular homogenous erythema (59%), central erythema (30%), central clearing (9%), or central purpura (2%).<ref name="pmid17113969">{{cite journal| author=Feder HM, Abeles M, Bernstein M, Whitaker-Worth D, Grant-Kels JM| title=Diagnosis, treatment, and prognosis of erythema migrans and Lyme arthritis. | journal=Clin Dermatol | year= 2006 | volume= 24 | issue= 6 | pages= 509-20 | pmid=17113969 | doi=10.1016/j.clindermatol.2006.07.012 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17113969 }} </ref> | **EM is classically 5 to 6.8 cm in diameter appearing as an annular homogenous [[erythema]] (59%), central [[erythema]] (30%), central clearing (9%), or central [[purpura]] (2%).<ref name="pmid17113969">{{cite journal| author=Feder HM, Abeles M, Bernstein M, Whitaker-Worth D, Grant-Kels JM| title=Diagnosis, treatment, and prognosis of erythema migrans and Lyme arthritis. | journal=Clin Dermatol | year= 2006 | volume= 24 | issue= 6 | pages= 509-20 | pmid=17113969 | doi=10.1016/j.clindermatol.2006.07.012 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17113969 }} </ref> | ||
**EM gradually expands over a period of days reaching up to 12 inches(30 cm)or more across. | **EM gradually expands over a period of days reaching up to 12 inches (30 cm) or more across. | ||
**EM may feel warm to touch but is rarely [[Itch|itchy]] or [[Pain|painful]]. | **EM may feel warm to touch but is rarely [[Itch|itchy]] or [[Pain|painful]]. | ||
**EM clears as it enlarges, resulting in a target or “bull’s-eye” appearance. | **EM clears as it enlarges, resulting in a target or “bull’s-eye” appearance. | ||
| Line 172: | Line 172: | ||
**The [[rash]] does not represent an [[allergic reaction]] to the bite, but rather a [[skin infection]] with the [[Borrelia burgdorferi|Lyme bacteria]], [[Lyme disease microbiology|''Borrelia burgdorferi'' sensu lato]]. | **The [[rash]] does not represent an [[allergic reaction]] to the bite, but rather a [[skin infection]] with the [[Borrelia burgdorferi|Lyme bacteria]], [[Lyme disease microbiology|''Borrelia burgdorferi'' sensu lato]]. | ||
**EM resolves in approximately 28 days in untreated patients.<ref name="pmid6859726">{{cite journal| author=Steere AC, Bartenhagen NH, Craft JE, Hutchinson GJ, Newman JH, Rahn DW et al.| title=The early clinical manifestations of Lyme disease. | journal=Ann Intern Med | year= 1983 | volume= 99 | issue= 1 | pages= 76-82 | pmid=6859726 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6859726 }}</ref> | **EM resolves in approximately 28 days in untreated patients.<ref name="pmid6859726">{{cite journal| author=Steere AC, Bartenhagen NH, Craft JE, Hutchinson GJ, Newman JH, Rahn DW et al.| title=The early clinical manifestations of Lyme disease. | journal=Ann Intern Med | year= 1983 | volume= 99 | issue= 1 | pages= 76-82 | pmid=6859726 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6859726 }}</ref> | ||
**The characteristic "bull's-eye" rash with central clearing is present in about 20% of endemic cases in the United States; whereas in Europe and the non-endemic United States 80% of rashes have central clearing. In endemic areas of the United States homogeneously red rashes are more frequent.<ref name="pmid11900494">{{cite journal| author=Smith RP, Schoen RT, Rahn DW, Sikand VK, Nowakowski J, Parenti DL et al.| title=Clinical characteristics and treatment outcome of early Lyme disease in patients with microbiologically confirmed erythema migrans. | journal=Ann Intern Med | year= 2002 | volume= 136 | issue= 6 | pages= 421-8 | pmid=11900494 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11900494 }} </ref><ref name="pmid11982300">{{cite journal| author=Edlow JA| title=Erythema migrans. | journal=Med Clin North Am | year= 2002 | volume= 86 | issue= 2 | pages= 239-60 | pmid=11982300 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11982300 }} </ref> | **The characteristic "bull's-eye" rash with central clearing is present in about 20% of [[endemic]] cases in the United States; whereas in Europe and the non-endemic United States 80% of [[rashes]] have central clearing. In [[endemic]] areas of the United States homogeneously red [[Rash|rashes]] are more frequent.<ref name="pmid11900494">{{cite journal| author=Smith RP, Schoen RT, Rahn DW, Sikand VK, Nowakowski J, Parenti DL et al.| title=Clinical characteristics and treatment outcome of early Lyme disease in patients with microbiologically confirmed erythema migrans. | journal=Ann Intern Med | year= 2002 | volume= 136 | issue= 6 | pages= 421-8 | pmid=11900494 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11900494 }} </ref><ref name="pmid11982300">{{cite journal| author=Edlow JA| title=Erythema migrans. | journal=Med Clin North Am | year= 2002 | volume= 86 | issue= 2 | pages= 239-60 | pmid=11982300 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11982300 }} </ref> | ||
**Serologic testing is not recommended in patients with EM. Initially, majority of patients are seronegative.<ref name="pmid17113969">{{cite journal| author=Feder HM, Abeles M, Bernstein M, Whitaker-Worth D, Grant-Kels JM| title=Diagnosis, treatment, and prognosis of erythema migrans and Lyme arthritis. | journal=Clin Dermatol | year= 2006 | volume= 24 | issue= 6 | pages= 509-20 | pmid=17113969 | doi=10.1016/j.clindermatol.2006.07.012 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17113969 }} </ref> | **[[Serological testing|Serologic testing]] is not recommended in patients with EM. Initially, majority of patients are [[seronegative]].<ref name="pmid17113969">{{cite journal| author=Feder HM, Abeles M, Bernstein M, Whitaker-Worth D, Grant-Kels JM| title=Diagnosis, treatment, and prognosis of erythema migrans and Lyme arthritis. | journal=Clin Dermatol | year= 2006 | volume= 24 | issue= 6 | pages= 509-20 | pmid=17113969 | doi=10.1016/j.clindermatol.2006.07.012 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17113969 }} </ref> | ||
**Multiple | **Multiple [[erythema migrans]] are present in [[disseminated disease]].<ref name="pmid158674072">{{cite journal| author=Wormser GP, McKenna D, Carlin J, Nadelman RB, Cavaliere LF, Holmgren D et al.| title=Brief communication: hematogenous dissemination in early Lyme disease. | journal=Ann Intern Med | year= 2005 | volume= 142 | issue= 9 | pages= 751-5 | pmid=15867407 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15867407 }}</ref> | ||
**Mini erythema migrans - Sometimes , erythema migrans may be less than 5 cm in diameter. It is an important and atypical sign of early localized [[Lyme disease]].<ref name="pmid16484816">{{cite journal| author=Weber K, Wilske B| title=Mini erythema migrans--a sign of early Lyme borreliosis. | journal=Dermatology | year= 2006 | volume= 212 | issue= 2 | pages= 113-6 | pmid=16484816 | doi=10.1159/000090650 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16484816 }} </ref> | **Mini [[erythema migrans]] - Sometimes , [[erythema migrans]] may be less than 5 cm in diameter. It is an important and atypical sign of early localized [[Lyme disease]].<ref name="pmid16484816">{{cite journal| author=Weber K, Wilske B| title=Mini erythema migrans--a sign of early Lyme borreliosis. | journal=Dermatology | year= 2006 | volume= 212 | issue= 2 | pages= 113-6 | pmid=16484816 | doi=10.1159/000090650 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16484816 }} </ref> | ||
| | | | ||
<gallery> | <gallery> | ||
| Line 193: | Line 193: | ||
==Lyme Arthritis== | ==Lyme Arthritis== | ||
*'''Lyme arthritis''' is the hallmark of stage 3 | *'''[[Lyme arthritis]]''' is the hallmark of [[Lyme disease history and symptoms#symptoms|stage 3 Lyme disease]]. | ||
*Lyme arthritis is most frequently presented symptom in late disseminated | *[[Lyme arthritis]] is most frequently presented symptom in [[Lyme disease history and symptoms#symptoms|late disseminated Lyme disease]]. | ||
*Lyme arthritis is not necessarily preceded by erythema migrans. | *[[Lyme arthritis]] is not necessarily preceded by [[erythema migrans]]. | ||
*Lyme arthritis may occur due to hematogenous spread of ''[[Borrelia burgdorferi|B. burgdorferi]]'' to multiple joints during early [[infection]]. This might explain migratory arthralgia during early stage of Lyme disease. | *[[Lyme arthritis]] may occur due to hematogenous spread of ''[[Borrelia burgdorferi|B. burgdorferi]]'' to multiple joints during early [[infection]]. This might explain migratory [[arthralgia]] during early stage of [[Lyme disease]]. | ||
*It usually takes months to years for Lyme disease to progress to Lyme arthritis. | *It usually takes months to years for [[Lyme disease]] to progress to [[Lyme arthritis]]. | ||
*Lyme arthritis symptoms ranges from intermittent attack of monoarthritis/oligoarthritis to persistent arthritis. | *[[Lyme arthritis]] symptoms ranges from intermittent attack of [[monoarthritis]]/[[oligoarthritis]] to persistent [[arthritis]]. | ||
*Intermittent attack of Lyme arthritis ranges from 3 days to 11.5 months with a mean of 3 months.<ref name="pmid36622852">{{cite journal| author=Steere AC, Schoen RT, Taylor E| title=The clinical evolution of Lyme arthritis. | journal=Ann Intern Med | year= 1987 | volume= 107 | issue= 5 | pages= 725-31 | pmid=3662285 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3662285 }}</ref> | *Intermittent attack of [[Lyme arthritis]] ranges from 3 days to 11.5 months in duration with a mean of 3 months.<ref name="pmid36622852">{{cite journal| author=Steere AC, Schoen RT, Taylor E| title=The clinical evolution of Lyme arthritis. | journal=Ann Intern Med | year= 1987 | volume= 107 | issue= 5 | pages= 725-31 | pmid=3662285 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3662285 }}</ref> | ||
*During early years of illness, attacks of Lyme arthritis are more frequent and longer in duration. Both frequency and duration of attacks decreases subsequently. | *During early years of illness, attacks of [[Lyme arthritis]] are more frequent and longer in duration. Both frequency and duration of attacks decreases subsequently. | ||
* There may month or years of complete remission between each attack of Lyme arthritis. | * There may month or years of complete remission between each attack of [[Lyme arthritis]]. | ||
*Majority of times Lyme arthritis involves large joints. Most commonly affected joint is [[Knee|knee joint]], but any joint can be affected including shoulder, ankle, elbow, temporomandibular joint, and wrist. | *Majority of times [[Lyme arthritis]] involves large [[Joint|joints]]. Most commonly affected joint is [[Knee|knee joint]], but any joint can be affected including [[shoulder]], [[ankle]], [[elbow]], [[temporomandibular joint]], and [[wrist]]. | ||
*Tendonitis and/or bursitis may also be present in few patients. Majority of times joints involved were shoulder, knee, or elbow . | *[[Tendonitis]] and/or [[bursitis]] may also be present in few patients. Majority of times [[Joint|joints]] involved were [[shoulder]], [[knee]], or [[elbow]] . | ||
*Majority of patients have little/no joint dysfunction after remission of attack. Few patients with persistent arthritis may show erosion and permanent damage to joint.<ref name="pmid3662285">{{cite journal| author=Steere AC, Schoen RT, Taylor E| title=The clinical evolution of Lyme arthritis. | journal=Ann Intern Med | year= 1987 | volume= 107 | issue= 5 | pages= 725-31 | pmid=3662285 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3662285 }} </ref> | *Majority of patients have little/no joint dysfunction after remission of attack. Few patients with persistent [[arthritis]] may show [[Erosion (dental)|erosion]] and permanent damage to [[joint]].<ref name="pmid3662285">{{cite journal| author=Steere AC, Schoen RT, Taylor E| title=The clinical evolution of Lyme arthritis. | journal=Ann Intern Med | year= 1987 | volume= 107 | issue= 5 | pages= 725-31 | pmid=3662285 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3662285 }} </ref> | ||
==Manifestations of Lyme Disease by Stage== | ==Manifestations of Lyme Disease by Stage== | ||
Revision as of 19:18, 4 August 2017
|
Lyme disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Lyme disease history and symptoms On the Web |
|
American Roentgen Ray Society Images of Lyme disease history and symptoms |
|
Risk calculators and risk factors for Lyme disease history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Anmol Pitliya, M.B.B.S. M.D.[2], Ilan Dock, B.S.
Overview
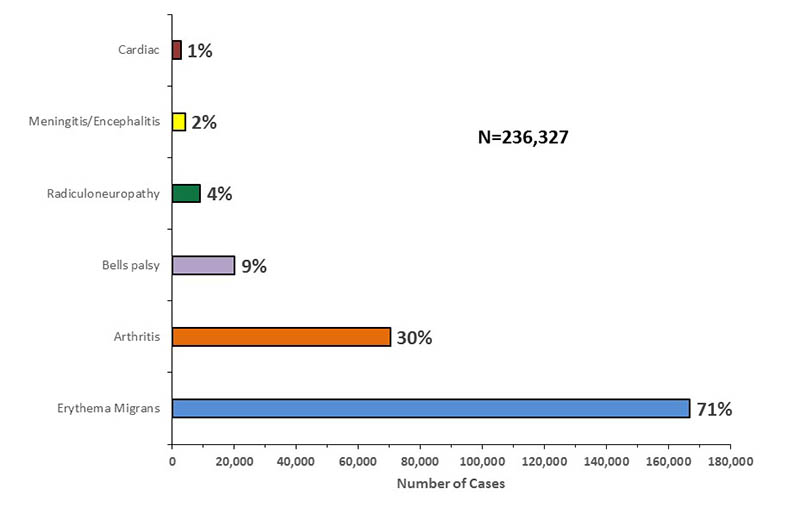
Lyme disease is divided into 3 stages and symptoms are stage specific. Initial symptoms include "bulls-eye" rash, with accompanying flu-like symptoms. It can progress to cardiovascular or neurological complications.
History
- The incubation period from infection to the onset of symptoms is usually 1–2 weeks, but can be much shorter (days), or much longer (months to years). Symptoms most often occur from May through September because the nymphal stage of the tick is responsible for most cases. [1]Asymptomatic infection exists, but is uncommon.[2]
- The specific areas of focus when obtaining the history, are outlined below:
Symptoms
Lyme disease is divided into 3 stages and symptoms are stage specific.
- Stage 1 - Early localized disease
- Stage 2 - Early disseminated disease
- Stage 3 - Late disseminated disease
Stage 1 - Early localized disease
|
Features of early localized disease includes erythema migrans and flu-like symptoms.
|
  |
Stage 2 - Early disseminate disease
|
Features of early disseminated disease can be divided system wise and includes:
|
 |
- Cardiac manifestations
- Dermatological manifestations[9]
- Borrelial lymphocytoma: Most common site is earlobe.
- Ocular manifestations[10]
- Primary ocular symptoms occurs due to inflammation of ocular tissue. These symptoms includes conjunctivitis, keratitis, iridocyclitis, retinal vasculitis, chorioiditis, and optic neuropathy (extremely rarely episcleritis, panuveitis, panophthalmitis).
- Secondary ocular symptoms occurs due to extraocular manifestations. These symptoms includes pareses of cranial nerves and orbital myositis.
Stage 3 - Late disseminated disease
- Features of late disseminated disease can take months to years to manifest after the onset of infection.
- Lyme arthritis is dominant months later but chronic neurologic involvement becomes more obvious years later.
- The symptoms of late disseminated lyme disease includes:
- Musculoskeletal manifestation:
- Lyme arthritis
- Lyme arthritis is the hallmark of stage 3 Lyme disease.
- Most frequently presented symptom in late disseminated Lyme disease.
- Commonly affects knee joint.
- Lyme arthritis
- Neurological manifestations:
- These neurological symptoms may take months to years to manifest after the infection. In addition to acute symptoms, Neuroborrerliosis can be manifested by a wide-range of neurological disorders, either central or peripheral including:
- Encephalopathy (sub-acute): Affects memory, mood, sleep, and sometimes with subtle language disturbances.
- Polyneuropathy or Paresthesia
- Leukoencephalitis[11]
- Muscle twitching
- Otolaryngologic manifestations: Neck pain, odynophagia, head and neck dysesthesia, otalgia, tinnitus, hearing loss, vertigo, temporomandibular joint pain, lymphadenopathy, dysgeusia.[12][13]
- Neuropsychiatric symptoms often develop much later in the disease progression, much like tertiary neurosyphilis.[14]
- In rare cases, frank psychosis have been attributed to chronic Lyme disease effects, including misdiagnoses of schizophrenia and bipolar disorder.
- Panic attack and anxiety can occur, also delusional behavior, including somatoform delusions, sometimes accompanied by a depersonalization or derealization syndrome similar to what was seen in the past in the prodromal or early stages of general paresis.[15]
- These neurological symptoms may take months to years to manifest after the infection. In addition to acute symptoms, Neuroborrerliosis can be manifested by a wide-range of neurological disorders, either central or peripheral including:
- Dermatological manifestation[9]
- Musculoskeletal manifestation:
|
 | ||||||
| Difference in clinical features in Europe and North America[17] | ||
|---|---|---|
| Features | Europe | North America |
| Erythema migrans | Single lesion more frequently | Multiple lesions occurs more freuqently |
| Heterogenous dissemination | Less common | More common |
| Borrelial lymphocytoma | Present | Absent |
| Acrodermatitis chronica atrophicans | Present | Absent |
| Meningoradiculoneuritis | More common | Less common |
| Lyme arthritis | Rarely preceded by erythema migrans | Commonly preceded by erythema migrans |
Erythema Migrans
|
|
Lyme Carditis
- Cardiac involvement occurs in about 5—10% of untreated Lyme disease and patients usually have symptoms related to fluctuating degrees of atrioventricular block (first-degree block to complete heart block) including lightheadedness, palpitations, shortness of breath, chest pain, and syncope.[24]
- Less commonly, patients may present with an acute picture of left ventricular dysfunction, cardiomegaly, perimyocarditis, or pancarditis without noticeable cardiac murmurs.[25]
- Lyme carditis can occur independently, it is usually accompanied by other cutaneous, joint, or neurologic features of Lyme disease.[26]
Lyme Arthritis
- Lyme arthritis is the hallmark of stage 3 Lyme disease.
- Lyme arthritis is most frequently presented symptom in late disseminated Lyme disease.
- Lyme arthritis is not necessarily preceded by erythema migrans.
- Lyme arthritis may occur due to hematogenous spread of B. burgdorferi to multiple joints during early infection. This might explain migratory arthralgia during early stage of Lyme disease.
- It usually takes months to years for Lyme disease to progress to Lyme arthritis.
- Lyme arthritis symptoms ranges from intermittent attack of monoarthritis/oligoarthritis to persistent arthritis.
- Intermittent attack of Lyme arthritis ranges from 3 days to 11.5 months in duration with a mean of 3 months.[27]
- During early years of illness, attacks of Lyme arthritis are more frequent and longer in duration. Both frequency and duration of attacks decreases subsequently.
- There may month or years of complete remission between each attack of Lyme arthritis.
- Majority of times Lyme arthritis involves large joints. Most commonly affected joint is knee joint, but any joint can be affected including shoulder, ankle, elbow, temporomandibular joint, and wrist.
- Tendonitis and/or bursitis may also be present in few patients. Majority of times joints involved were shoulder, knee, or elbow .
- Majority of patients have little/no joint dysfunction after remission of attack. Few patients with persistent arthritis may show erosion and permanent damage to joint.[28]
Manifestations of Lyme Disease by Stage
| System | Stage 1 (Localized Infection) | Stage 2 (Early Disseminated Infection) | Stage 3 (Late Persistent Infection) |
| Skin |
|
| |
| Musculoskeletal | — |
|
|
| Neurologic | — |
|
|
| Lymphatic |
|
|
— |
| Heart | — |
|
— |
| Eyes | — |
|
|
| Liver | — |
|
— |
| Respiratory | — |
|
— |
| Kidney | — |
|
— |
| Genitourinary | — | — | |
| Flu-like symptoms systems |
Adapted from Steere AC. Lyme disease. N Engl J Med. 1989;321:586.
References
- ↑ Falco RC, McKenna DF, Daniels TJ, Nadelman RB, Nowakowski J, Fish D; et al. (1999). "Temporal relation between Ixodes scapularis abundance and risk for Lyme disease associated with erythema migrans". Am J Epidemiol. 149 (8): 771–6. PMID 10206627.
- ↑ Steere AC, Sikand VK, Schoen RT, Nowakowski J (2003). "Asymptomatic infection with Borrelia burgdorferi". Clin. Infect. Dis. 37 (4): 528–32. PMID 12905137.
- ↑ 3.0 3.1 Steere AC, Sikand VK (2003). "The presenting manifestations of Lyme disease and the outcomes of treatment". N Engl J Med. 348 (24): 2472–4. doi:10.1056/NEJM200306123482423. PMID 12802042.
- ↑ Nadelman RB, Nowakowski J, Forseter G, Goldberg NS, Bittker S, Cooper D; et al. (1996). "The clinical spectrum of early Lyme borreliosis in patients with culture-confirmed erythema migrans". Am J Med. 100 (5): 502–8. PMID 8644761.
- ↑ 5.0 5.1 Wormser GP, McKenna D, Carlin J, Nadelman RB, Cavaliere LF, Holmgren D; et al. (2005). "Brief communication: hematogenous dissemination in early Lyme disease". Ann Intern Med. 142 (9): 751–5. PMID 15867407.
- ↑ Halperin JJ (2008). "Nervous system Lyme disease". Infect Dis Clin North Am. 22 (2): 261–74, vi. doi:10.1016/j.idc.2007.12.009. PMID 18452800.
- ↑ England JD, Bohm RP, Roberts ED, Philipp MT (1997). "Mononeuropathy multiplex in rhesus monkeys with chronic Lyme disease". Ann Neurol. 41 (3): 375–84. doi:10.1002/ana.410410313. PMID 9066359.
- ↑ Chabria SB, Lawrason J (2007). "Altered mental status, an unusual manifestation of early disseminated Lyme disease: A case report". 1 (1): 62. doi:10.1186/1752-1947-1-62. PMID 17688693.
- ↑ 9.0 9.1 Mullegger RR (2004). "Dermatological manifestations of Lyme borreliosis". Eur J Dermatol. 14 (5): 296–309. PMID 15358567.
- ↑ Stanek G, Strle F (2003). "Lyme borreliosis". Lancet. 362 (9396): 1639–47. doi:10.1016/S0140-6736(03)14798-8. PMID 14630446.
- ↑ Halperin JJ, Volkman DJ, Wu P (1991). "Central nervous system abnormalities in Lyme neuroborreliosis". Neurology. 41 (10): 1571–82. PMID 1922798.
- ↑ Rosenhall U, Hanner P, Kaijser B (1988). "Borrelia infection and vertigo". Acta Otolaryngol. 106 (1–2): 111–6. PMID 3421091.
- ↑ Moscatello AL, Worden DL, Nadelman RB, Wormser G, Lucente F (1991). "Otolaryngologic aspects of Lyme disease". Laryngoscope. 101 (6 Pt 1): 592–5. PMID 2041438.
- ↑ Logigian, Eric L.; Kaplan, Richard F.; Steere, Allen C. (1990). "Chronic Neurologic Manifestations of Lyme Disease". New England Journal of Medicine. 323 (21): 1438–1444. doi:10.1056/NEJM199011223232102. ISSN 0028-4793.
- ↑ Fallon BA, Nields JA (1994). "Lyme disease: a neuropsychiatric illness". The American journal of psychiatry. 151 (11): 1571–83. PMID 7943444.Hess A, Buchmann J, Zettl UK; et al. (1999). "Borrelia burgdorferi central nervous system infection presenting as an organic schizophrenialike disorder". Biol. Psychiatry. 45 (6): 795. PMID 10188012.)
- ↑ Ciesielski CA, Markowitz LE, Horsley R, Hightower AW, Russell H, Broome CV (1989). "Lyme disease surveillance in the United States, 1983-1986". Rev. Infect. Dis. 11 Suppl 6: S1435–41. PMID 2682955.
- ↑ Stanek G, Strle F (2008). "Lyme disease: European perspective". Infect Dis Clin North Am. 22 (2): 327–39, vii. doi:10.1016/j.idc.2008.01.001. PMID 18452805.
- ↑ 18.0 18.1 Feder HM, Abeles M, Bernstein M, Whitaker-Worth D, Grant-Kels JM (2006). "Diagnosis, treatment, and prognosis of erythema migrans and Lyme arthritis". Clin Dermatol. 24 (6): 509–20. doi:10.1016/j.clindermatol.2006.07.012. PMID 17113969.
- ↑ Steere AC, Bartenhagen NH, Craft JE, Hutchinson GJ, Newman JH, Rahn DW; et al. (1983). "The early clinical manifestations of Lyme disease". Ann Intern Med. 99 (1): 76–82. PMID 6859726.
- ↑ Smith RP, Schoen RT, Rahn DW, Sikand VK, Nowakowski J, Parenti DL; et al. (2002). "Clinical characteristics and treatment outcome of early Lyme disease in patients with microbiologically confirmed erythema migrans". Ann Intern Med. 136 (6): 421–8. PMID 11900494.
- ↑ Edlow JA (2002). "Erythema migrans". Med Clin North Am. 86 (2): 239–60. PMID 11982300.
- ↑ Weber K, Wilske B (2006). "Mini erythema migrans--a sign of early Lyme borreliosis". Dermatology. 212 (2): 113–6. doi:10.1159/000090650. PMID 16484816.
- ↑ "Dermatology Atlas".
- ↑ Hu LT (2012). "In the clinic. Lyme disease". Ann Intern Med. 157 (3): ITC2-2–ITC2-16. doi:10.7326/0003-4819-157-3-20120807-01002. PMID 22868858.
- ↑ 25.0 25.1 Steere, Allen C. (1989). "Lyme Disease". New England Journal of Medicine. 321 (9): 586–596. doi:10.1056/NEJM198908313210906. ISSN 0028-4793.
- ↑ Fish, Airley E.; Pride, Yuri B.; Pinto, Duane S. (2008). "Lyme Carditis". Infectious Disease Clinics of North America. 22 (2): 275–288. doi:10.1016/j.idc.2007.12.008. ISSN 0891-5520.
- ↑ Steere AC, Schoen RT, Taylor E (1987). "The clinical evolution of Lyme arthritis". Ann Intern Med. 107 (5): 725–31. PMID 3662285.
- ↑ Steere AC, Schoen RT, Taylor E (1987). "The clinical evolution of Lyme arthritis". Ann Intern Med. 107 (5): 725–31. PMID 3662285.
![Erythema chronicum migrans Adapted from Dermatology Atlas.[23]](/images/3/3d/Erythema_chronicum_migrans01.jpg)
