Sandbox Jose2
| Tuberous sclerosis | |
|---|---|
| Synonyms | Tuberous sclerosis complex (TSC), Bourneville disease |
| File:Patient with facial angiofibromas caused by tuberous sclerosis.jpg | |
| A case of tuberous sclerosis showing facial angiofibromas in characteristic butterfly pattern | |
| Specialty | Lua error in Module:WikidataIB at line 609: attempt to index field 'wikibase' (a nil value). |



Overview
Tuberous sclerosis complex (TSC), is a rare autosomal dominant congenital disorder that affects multiple organ systems and is characterized by an abnormal growth of ectodermal and mesodermal cells that causes non-cancerous tumours to grow in the brain and on other vital organs such as the kidneys, heart, liver, eyes, lungs, and skin. [1]
A combination of symptoms may include seizures, intellectual disability, developmental delay, behavioral problems, skin abnormalities, and lung and kidney disease. TSC is caused by a mutation of either of two genes, TSC1 and TSC2, which code for the proteins hamartin and tuberin, respectively. These proteins act as tumor growth suppressors, agents that regulate cell proliferation and differentiation.[2]
The disease presents with a myriad of symptoms, having been described by multiple doctors throughtout the 19th century and called by many different names, but it is now called tuberous sclerosis complex, and the relationship between benign brain tumors and the symptoms of the disease was first described by Désiré-Magloire Bourneville in 1880. [3]
Historical Perspective
Tuberous Sclerosis was described as a specific disease in the 19th century, being initially referred to adenoma sebaceum, epiloia, Pringle's disease or Bourneville's disease. Rayer, a French dermatologist, was the one to first describe the disease and the fibrovascular papules that characterize it, making illustrations of it. He described two cases of tuberous sclerosis in patients who had the nasolabial papular eruption with telangiectasias at the base. In 1850 the first written report of tuberous sclerosis appeared in "Vitiligoidea", published by Addison and Gull. It was not recognized as a distinct disease but was classified as "vitiligoidea tuberosa". In 1862, von Recklinghausen reported a tumor of the heart found in a newborn during autopsy, and by that he is credited to be the first that described the microscopic appearance of tuberous sclerosis. Bourneville in 1880, a French neurologist, described the case of a girl who presented at the age of 3 with facial eruption and died at 15 years of age due to epilepsy, which complicated with pneumonia and inanition. He found brain and kidney tumors on the autopsy which were correctly believed to be the cause of her seizures and mental retardation. In 1911, E. B. Sherlock, superintendent of Belmont Asylum of Idiots, London, coined the word "epiloia" that indicated a clinical triad of epilepsy, low intelligence and adenoma sebaceum.[3]
In 2002, treatment with rapamycin was found to be effective at shrinking tumours in animals. This has led to human trials of rapamycin as a drug to treat several of the tumors associated with TSC.[4]
Classification
There is no established system for the classification of tuberous sclerosis.
Pathophysiology
Patients with tuberous sclerosis have loss-of-function germline mutations in both alleles of the following tumor suppressor genes: TSC1 or TSC2. One third of the mutations is inherited, two thirds are de novo mutations. The mutations causes the loss of one allele, but as long as the second one remains intact, the cell won't present any metabolic change. When there is a second TSC1 or TSC2 mutation, which typically occurs in multiple cells over a person's lifetime, then the disease starts to manifest (fitting the "two-hit" tumor-suppressor gene model, with the germline mutation inactivating one gene and then a somatic event inactivating the remaining other one). TSC1 codes for a protein called hamartin, and TSC2 codes for a protein called tuberin. They belong to a protein complex that inhibits the mammalian target of rapamycin (mTOR) complex 1 via RAS homologue enriched in brain (RHEB) which regulates cell growth. In a normal patient, RHEB activates mTORC1 when bound to GTP, but in TSC there is a hyperactivarion of RHEB and consequently of mTORC1. mTOR regulates cellular proliferation, autophagy, growth and protein and lipid synthesis and it enhances protein translation when activated, reprograming the cell metabolism, which increases cell proliferation but also may make it vulnerable to death in nutrient-restricted media. Besides the TSC-RHEB-mTORC1 pathway, there is evidence of alternate pathways also having a role in the disease that are mTORC1 independent, but they are currently under investigation.[5][1]
Causes
Loss of function mutation of the genes TSC1 and TSC2 which are responsible for the production of hamartin and tuberin. These proteins regulate the cell cycle. Damage to this pathway leads to a very variable presentation of benign tumors in multiple systems. TSC1 and TSC2 are both tumor suppressor genes that function according to Knudson's "two hit" hypothesis. That is, a second random mutation must occur before a tumor can develop. This explains why, despite its high penetrance, TSC has wide expressivity.
|
|
|||||||||||||||||||||||||||||||||||||||||
Symptoms
Skin
Symptoms develop in almost all patients with TSC and include ungual fibromas, facial angiofibromas (may demand treatment and may worsen with UV exposure), shagreen patches (oval-shaped lesions, generally skin-colored but can be sometimes pigmented, may be crinkled or smooth), focal hypopigmented macules (ash-leaf spots), dental enamel pits (present in 100% of the patients), oral fibromas, retinal astrocytic hamartomas (tumors of the retinal nerve), retinal achromic patches (light or dark spots on the eye).[1]
Renal
TSC leads to the formation of renal angiomyolipomas (present in 60-80% of the TSC patients), benign tumors composed of abnormal vessels, smooth-muscle cells and fat cells which may cause hematuria. These tumors can be detectable in early childhood by MRI, CT or ultrasound. Although benign, in TSC they are commonly multiple and bilateral. Angiomyolipomas larger than 4 cm are at risk for potentially catastrophic hemorrhage either spontaneously or with minimal trauma. Patients may also develop epithelial cysts, polycystic kidney disease (as 2-3% of the patients carries a deletion that affects both TSC2 gene and one of the genes that lead to autosomal dominant polycystic kidney disease) and renal-cell carcinomas that may be diagnosed at a younger age (mean 28 years).[6][1]
Pulmonary
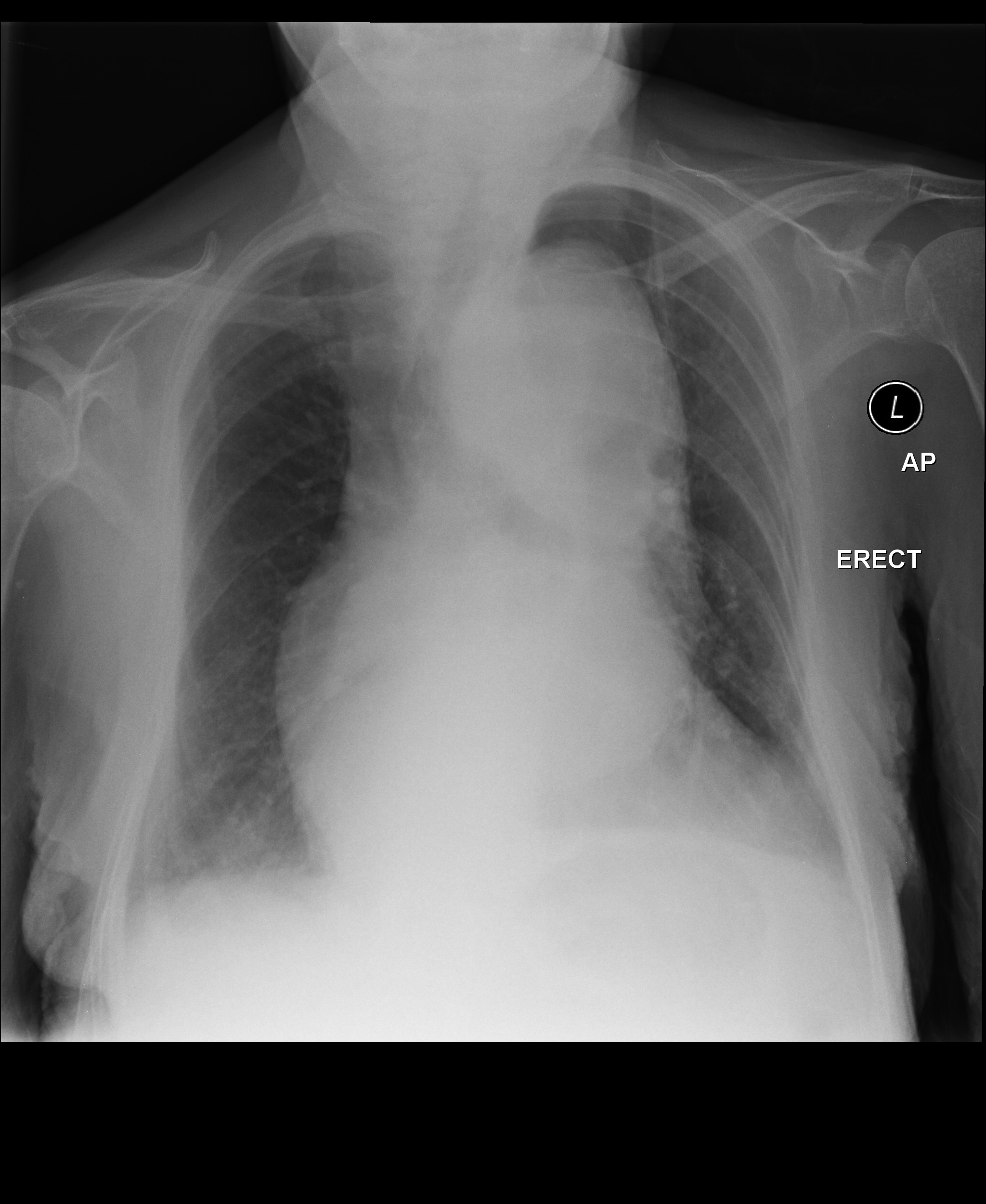
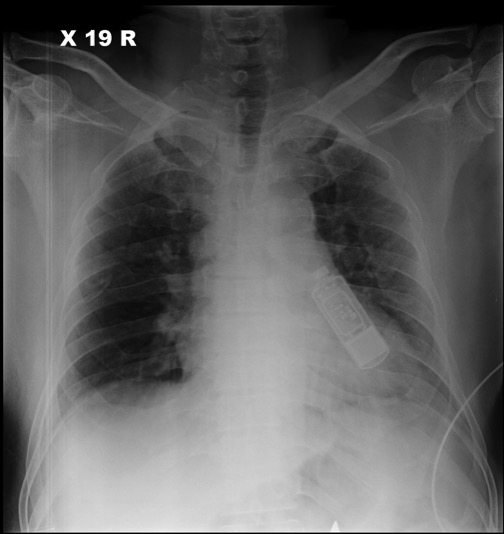
Lymphangiomyomatosis affects mostly women and is a proliferation of smooth-muscle cells that may result in cystic changes in the lungs. Recent genetic analysis has shown that the proliferative bronchiolar smooth muscle in TSC-related lymphangioleiomyomatosis is monoclonal metastasis from a coexisting renal angiomyolipoma. Cases of TSC-related lymphangioleiomyomatosis recurring following lung transplant have been reported.[7] Diagnosed mostly during early adulthood, may cause pneumothorax. Multifocal micronodular pneumocyte hyperplasia can occur in both men and women and are mostly asymptomatic.[6][1]
Neurologic
These manifestations are one of the major causes of morbidity in patients with TSC. TSC may cause epilepsy, which is the most common neurological presentation occurring in 70-80% of patients and may complicate with infantile spasms, a severe form of epileptic syndrome. If epilepsy presents with an early onset t is associated with cognitive disabilities, which are also very prevalent in such patients. Neuropsychiatric disorders are present in two-thirds of the patients and anxiety is one of the most common presentations. Autism is one possible manifestation and is especially associated with cerebral cortical tubers. It consists of neurologic tissue that grows in a different pattern, losing the normal six-layered cortical structure, with dysmorphic neurons, large astrocytes and giant cells. Some patients may also present with subependymal giant cell astrocytomas, which may cause obstructive hydrocephalus. Risk of such benign tumors decreases after age of 20.[6][1]
Cardiovascular
Rhabdomyomas may be present, being intramural or intracavitary in its distribution along the myocardium. May be detected in utero on fetuses and is associated with cardiac failure. Often disappear spontaneously in later life.[1] 80% of children under two-years-old with TSC have at least one rhabdomyoma, and about 90% of those will have several.[8]
Differentiating Tuberous Sclerosis from other Diseases
Tuberous sclerosis must be differentiated from other diseases that cause myxoma or other benign tumors and/or seizures, such as Sturge Weber, hypomelanosis of Ito, Birt-Hogg-Dube syndrome, multiple endocrine neoplasia and various seizures disorders.[9]
Epidemiology and Demographics
Tuberous sclerosis complex affects about 1 in 6,000 people, occurring in all races and ethnic groups, and in both genders. Prior to the invention of CT scanning to identify the nodules and tubers in the brain, the prevalence was thought to be much lower and the disease associated with those people diagnosed clinically with learning disability, seizures, and facial angiofibroma. Whilst still regarded as a rare disease, TSC is common when compared to many other genetic diseases, with at least 1 million individuals worldwide.[10][11]
Risk Factors
There are no established environmental risk factors for tuberous sclerosis. One third of the cases are familial, so family history can be a risk factor for the disease.[12]
Screening
As it is a rare disease, screening is not recommended.
Natural History, Complications, and Prognosis
Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%.
Common complications of tuberous sclerosis include spontaneous life-threatening bleeding from renal angiomyolipomas if greater than 3cm, renal failure,
Diagnosis
Tuberous sclerosis complex is diagnosed if a set of diagnostic criteria are met. These criteria include major and minor features. If a case meets the clinical diagnostic criteria, then it is performed a genetic molecular testing which is seem mostly as corroborative. Most of the patients seek medical assistance due to their dermatologic lesions or seizures but for making this diagnosis an evaluation that assesses all the clinical features of the tuberous sclerosis complex is necessary, as these manifestations have variable penetrance.[13] REF NEJM The latest diagnostic criteria was developed by the 2012 International Tuberous Sclerosis Complex Consensus Conference, and it is showed at the table below:
| Major Features | ||||
|---|---|---|---|---|
| Location | Sign | Onset[6] | Note | |
| 1 | Skin | Hypomelanotic macules | Infant – child | At least three, at least 5 mm in diameter. |
| 2 | Head | Facial angiofibromas or fibrous cephalic plaque | Infant – adult | At least three angiofibromas |
| 3 | Fingers and toes | Ungual fibroma | Adolescent – adult | At least two |
| 4 | Skin | Shagreen patch (connective tissue nevus) | Child | |
| 5 | Eyes | Multiple retinal nodular hamartomas | Infant | |
| 6 | Brain | Cortical dysplasias (includes tubers and cerebral white matter radial migration lines) | Fetus | |
| 7 | Brain | Subependymal nodule | Child – adolescent | |
| 8 | Brain | Subependymal giant cell astrocytoma | Child – adolescent | |
| 9 | Heart | Cardiac rhabdomyoma | Fetus | |
| 10 | Lungs | Lymphangioleiomyomatosis | Adolescent – adult | |
| 11 | Kidneys | Renal angiomyolipoma | Child – adult | At least two. Together, 10 and 11 count as one major feature. |
| Minor Features | ||||
| Location | Sign | Note | ||
| 1 | Skin | "Confetti" skin lesions | ||
| 2 | Teeth | Dental enamel pits | At least three | |
| 3 | Gums | Intraoral fibromas | At least two | |
| 4 | Eyes | Retinal achromic patch | ||
| 5 | Kidneys | Multiple renal cysts | ||
| 6 | Liver, spleen and other organs | Nonrenal hamartoma | ||
TSC can be first diagnosed at any stage of life. Prenatal diagnosis is possible by chance if heart tumours are discovered during routine ultrasound. In infancy, white patches on the skin may be noticed, or the child may present with epilepsy, particularly infantile spasms, or developmental delay may lead to neurological tests. In childhood, behavioural problems and autism spectrum disorder may also lead to a clinical investigation and a diagnosis. During adolescence it is usually that skin problems appear while in adulthood, kidney and lung problems may become evident. An individual may also be diagnosed at any time as a result of genetic testing of family members of another affected person.[15]
History and Symptoms
The most common symptoms of tuberous sclerosis include [symptom 1], [symptom 2], and [symptom 3]. Common symptoms of [disease] include [symptom 1], [symptom 2], and [symptom 3]. Less common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3].
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Laboratory Findings
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal among patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Electrocardiogram
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Embolization of angiomyolipomas is an option if they are bigger than 3 cm, but the preferred therapy the use of mTOR inhibtors due to the high recurrence after embolization NATURE NEJm Sirolimus, and mTOR inhibitor has been investigated as a potential therapeutic agent, but there is a fear that by activating AKT it may increase the risk of malignancy. NEJM Epilepsy should be treated with vigabatrin as first-line treatment. Diet changes like ketogenic diet and the low glycemic index treatment may be helpful. Vagal nerve stimulation can be effective. Surgical resection is the only treatment for CNS tumors NATURE - REESCREVER Since estrogen may promote renal angiomyolipomas's growth, estrogen exposure should be avoided. For skin lesions, use of systemic sirolimus or topical rapamycin has been shown to be effective (NATURE)
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Henske, Elizabeth P., et al. "Tuberous sclerosis complex." Nature reviews Disease primers 2.1 (2016): 1-18.
- ↑ "Tuberous Sclerosis Fact Sheet". National Institute of Neurological Disorders and Stroke. 2018-07-06. Retrieved 16 December 2018.
- ↑ 3.0 3.1 Morgan, J. Elizabeth, and Francis Wolfort. "The early history of tuberous sclerosis." Archives of dermatology 115.11 (1979): 1317-1319.
- ↑ Rott HD, Mayer K, Walther B, Wienecke R (March 2005). "Zur Geschichte der Tuberösen Sklerose (The History of Tuberous Sclerosis)" (PDF) (in German). Tuberöse Sklerose Deutschland e.V. Archived from the original (PDF) on 15 March 2007. Retrieved 8 January 2007.
- ↑ NIH - Tuberous Sclerosis - https://ghr.nlm.nih.gov/condition/tuberous-sclerosis-complex#genes - accessed at 06/10/2020
- ↑ 6.0 6.1 6.2 6.3 Crino PB, Nathanson KL, Henske EP (September 2006). "The tuberous sclerosis complex". The New England Journal of Medicine. 355 (13): 1345–56. doi:10.1056/NEJMra055323. PMID 17005952.
- ↑ Henske EP (December 2003). "Metastasis of benign tumor cells in tuberous sclerosis complex". Genes, Chromosomes & Cancer. 38 (4): 376–81. doi:10.1002/gcc.10252. PMID 14566858.
- ↑ Hinton RB, Prakash A, Romp RL, Krueger DA, Knilans TK (November 2014). "Cardiovascular manifestations of tuberous sclerosis complex and summary of the revised diagnostic criteria and surveillance and management recommendations from the International Tuberous Sclerosis Consensus Group". Journal of the American Heart Association. 3 (6): e001493. doi:10.1161/JAHA.114.001493. PMC 4338742. PMID 25424575.
- ↑ NORD: National Organization for Rare Diseases - Tuberous Sclerosis - available at: https://rarediseases.org/rare-diseases/tuberous-sclerosis/#:~:text=Examples%20of%20such%20disorders%20include,be%20differentiated%20from%20tuberous%20sclerosis. accessed at 06/12/2020
- ↑ Curatolo, Paolo, ed. Tuberous sclerosis complex: from basic science to clinical phenotypes. Cambridge University Press, 2003.
- ↑ NIH - Tuberous Sclerosis - https://ghr.nlm.nih.gov/condition/tuberous-sclerosis-complex#genes - accessed at 06/10/2020
- ↑ Henske, Elizabeth P., et al. "Tuberous sclerosis complex." Nature reviews Disease primers 2.1 (2016): 1-18.
- ↑ Crino, Peter B., Katherine L. Nathanson, and Elizabeth Petri Henske. "The tuberous sclerosis complex." New England Journal of Medicine 355.13 (2006): 1345-1356.
- ↑ Northrup H, Krueger DA (October 2013). "Tuberous sclerosis complex diagnostic criteria update: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference". Pediatric Neurology. 49 (4): 243–54. doi:10.1016/j.pediatrneurol.2013.08.001. PMC 4080684. PMID 24053982.
- ↑ "Tuberous Sclerosis Complex". University Hospitals Birmingham NHS Foundation Trust. Retrieved 16 December 2018.
External links
| Classification | [[d:Lua error in Module:WikidataIB/sandbox at line 2057: attempt to index field 'wikibase' (a nil value). |D]] |
|---|---|
| External resources |
| Wikimedia Commons has media related to [[commons:Lua error in Module:WikidataIB at line 428: attempt to index field 'wikibase' (a nil value).|Lua error in Module:WikidataIB at line 428: attempt to index field 'wikibase' (a nil value).]]. |
Lua error in Module:Authority_control at line 788: attempt to index field 'wikibase' (a nil value).
| Syncope classification | |||||||||||||||||||||||||||||
| Vasovagal | |||||||||||||||||||||||||||||
| Micturation | cough | ||||||||||||||||||||||||||||
| xxxx | KKKKKKK | yyyyy | |||||||||||||||||||||||||||
| Disease | Type | Sign | Symptom | ||
|---|---|---|---|---|---|
Syncope is classified into three categories:
| Disease Name | Age of Onset | Gender Preponderance | Signs/Symptoms | Imaging Feature(s) | Macroscopic Feature(s) | Microscopic Feature(s) | Laboratory Findings(s) | Other Feature(s) | ECG view |
|---|---|---|---|---|---|---|---|---|---|
- Pages with script errors
- CS1 maint: Unrecognized language
- Pages with broken file links
- Infobox medical condition (new)
- Pages using columns with the default column width
- Protein pages needing a picture
- Genes on human chromosome 9
- Genes on human chromosome 16
- Commons category link from Wikidata
- Commons category link is on Wikidata using P373
- Use dmy dates from January 2011
- Articles with invalid date parameter in template
- Autosomal dominant disorders
- Genodermatoses
- Rare diseases
- Biology of attention deficit hyperactivity disorder
- Autism
- Intellectual disability
- Biology of obsessive–compulsive disorder
- Disorders causing seizures