Ulcerative colitis laboratory findings: Difference between revisions
Kiran Singh (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (6 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Ulcerative colitis}} | {{Ulcerative colitis}} | ||
{{CMG}} | {{CMG}}; {{AE}} {{USAMA}} | ||
==Overview== | |||
The laboratory findings in a patient with ulcerative colitis include anemia, low albumin, elevated [[ESR]], elevated serum alkaline phosphatase, deranged [[LFTs]] and electrolyte abnormalities.<ref name="pmid17436102">{{cite journal| author=Rodgers AD, Cummins AG| title=CRP correlates with clinical score in ulcerative colitis but not in Crohn's disease. | journal=Dig Dis Sci | year= 2007 | volume= 52 | issue= 9 | pages= 2063-8 | pmid=17436102 | doi=10.1007/s10620-006-9691-2 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17436102 }} </ref><ref name="pmid15472532">{{cite journal| author=Vermeire S, Van Assche G, Rutgeerts P| title=C-reactive protein as a marker for inflammatory bowel disease. | journal=Inflamm Bowel Dis | year= 2004 | volume= 10 | issue= 5 | pages= 661-5 | pmid=15472532 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15472532 }} </ref> | |||
==Laboratory Findings== | ==Laboratory Findings== | ||
The initial [[diagnosis|diagnostic]] workup for ulcerative colitis includes the following:<ref>Al-Ataie MB, Shinoy VN. eMedicine: Ulcerative colitis. [http://www.emedicine.com/med/topic2336.htm Fulltext].</ref><ref name=ACGGuideline>Ulcerative Colitis Practice Guidelines in Adults, Am. Coll. Gastroenterology, 2004. [http://www.acg.gi.org/physicians/guidelines/UlcerativeColitisUpdate.pdf PDF]</ref> | The initial [[diagnosis|diagnostic]] workup for ulcerative colitis includes the following:<ref>Al-Ataie MB, Shinoy VN. eMedicine: Ulcerative colitis. [http://www.emedicine.com/med/topic2336.htm Fulltext].</ref><ref name=ACGGuideline>Ulcerative Colitis Practice Guidelines in Adults, Am. Coll. Gastroenterology, 2004. [http://www.acg.gi.org/physicians/guidelines/UlcerativeColitisUpdate.pdf PDF]</ref><ref name="pmid17436102">{{cite journal| author=Rodgers AD, Cummins AG| title=CRP correlates with clinical score in ulcerative colitis but not in Crohn's disease. | journal=Dig Dis Sci | year= 2007 | volume= 52 | issue= 9 | pages= 2063-8 | pmid=17436102 | doi=10.1007/s10620-006-9691-2 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17436102 }} </ref><ref name="pmid15472532">{{cite journal| author=Vermeire S, Van Assche G, Rutgeerts P| title=C-reactive protein as a marker for inflammatory bowel disease. | journal=Inflamm Bowel Dis | year= 2004 | volume= 10 | issue= 5 | pages= 661-5 | pmid=15472532 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15472532 }} </ref><ref name="pmid3356884">{{cite journal| author=Prantera C, Davoli M, Lorenzetti R, Pallone F, Marcheggiano A, Iannoni C et al.| title=Clinical and laboratory indicators of extent of ulcerative colitis. Serum C-reactive protein helps the most. | journal=J Clin Gastroenterol | year= 1988 | volume= 10 | issue= 1 | pages= 41-5 | pmid=3356884 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3356884 }} </ref><ref name="pmid20634346">{{cite journal| author=van Rheenen PF, Van de Vijver E, Fidler V| title=Faecal calprotectin for screening of patients with suspected inflammatory bowel disease: diagnostic meta-analysis. | journal=BMJ | year= 2010 | volume= 341 | issue= | pages= c3369 | pmid=20634346 | doi=10.1136/bmj.c3369 | pmc=2904879 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20634346 }} [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21242354 Review in: Ann Intern Med. 2011 Jan 18;154(2):JC1-12] </ref> | ||
* A [[complete blood count]] | * A [[complete blood count]] shows | ||
* [[Electrolyte]] studies and [[renal function|renal function tests]] are done, as chronic [[diarrhea]] may be associated with [[ | **[[Anemia]] | ||
**[[Thrombocytosis]] | |||
**A high [[platelet]] count | |||
*Elvated ESR (>30mm/hr) | |||
*Low albumin | |||
* [[Electrolyte]] studies and [[renal function|renal function tests]] are done, as chronic [[diarrhea]] may be associated with | |||
**[[Hypokalemia]] | |||
**[[Hypomagnesemia]] | |||
**Pre-renal failure | |||
* [[Liver function tests]] are performed to screen for bile duct involvement: [[primary sclerosing cholangitis]]. | * [[Liver function tests]] are performed to screen for bile duct involvement: [[primary sclerosing cholangitis]]. | ||
* | *Fecal lactoferrin or calprotectin may be checked to depict intestinal inflammation | ||
* [[Urinalysis]] | * [[Urinalysis]] | ||
* Elevated serum alkaline phosphatase (in case of uc and psc) | |||
* Stool culture, to rule out parasites and infectious causes. | * Stool culture, to rule out parasites and infectious causes. | ||
* [[C-reactive protein]] can be measured, with an elevated level being another indication of inflammation. | * [[C-reactive protein]] can be measured, with an elevated level being another indication of inflammation. | ||
Although ulcerative colitis is a disease of unknown causation, inquiry should be made as to unusual factors believed to trigger the disease.<ref name=ACGGuideline/> Factors may include: recent cessation of tobacco smoking; recent administration of large doses of [[iron]] or [[vitamin B6]]; [[hydrogen peroxide]] in enemas or other procedures. | Although ulcerative colitis is a disease of unknown causation, inquiry should be made as to unusual factors believed to trigger the disease.<ref name=ACGGuideline/> Factors may include: recent cessation of tobacco smoking; recent administration of large doses of [[iron]] or [[vitamin B6]]; [[hydrogen peroxide]] in enemas or other procedures. | ||
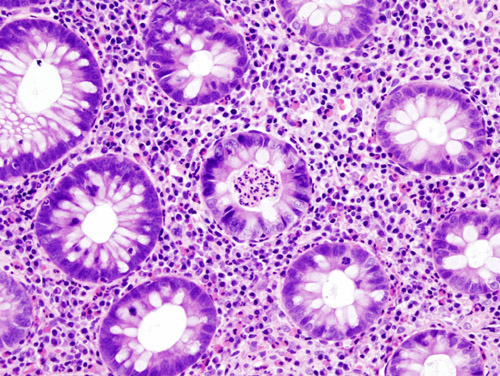
[[Image:Ulcerative colitis (2) active.jpg|thumb|center|H&E stain of a colonic biopsy showing a crypt abscess, a classic finding in ulcerative colitis]] | [[Image:Ulcerative colitis (2) active.jpg|thumb|center|H&E stain of a colonic biopsy showing a crypt abscess, a classic finding in ulcerative colitis - By User:KGH - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=510531]] | ||
== References == | == References == | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Autoimmune diseases]] | [[Category:Autoimmune diseases]] | ||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
| Line 30: | Line 40: | ||
[[Category:Abdominal pain]] | [[Category:Abdominal pain]] | ||
[[Category:Needs overview]] | [[Category:Needs overview]] | ||
Latest revision as of 00:33, 30 July 2020
|
Ulcerative colitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ulcerative colitis laboratory findings On the Web |
|
American Roentgen Ray Society Images of Ulcerative colitis laboratory findings |
|
Risk calculators and risk factors for Ulcerative colitis laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [2]
Overview
The laboratory findings in a patient with ulcerative colitis include anemia, low albumin, elevated ESR, elevated serum alkaline phosphatase, deranged LFTs and electrolyte abnormalities.[1][2]
Laboratory Findings
The initial diagnostic workup for ulcerative colitis includes the following:[3][4][1][2][5][6]
- A complete blood count shows
- Anemia
- Thrombocytosis
- A high platelet count
- Elvated ESR (>30mm/hr)
- Low albumin
- Electrolyte studies and renal function tests are done, as chronic diarrhea may be associated with
- Hypokalemia
- Hypomagnesemia
- Pre-renal failure
- Liver function tests are performed to screen for bile duct involvement: primary sclerosing cholangitis.
- Fecal lactoferrin or calprotectin may be checked to depict intestinal inflammation
- Urinalysis
- Elevated serum alkaline phosphatase (in case of uc and psc)
- Stool culture, to rule out parasites and infectious causes.
- C-reactive protein can be measured, with an elevated level being another indication of inflammation.
Although ulcerative colitis is a disease of unknown causation, inquiry should be made as to unusual factors believed to trigger the disease.[4] Factors may include: recent cessation of tobacco smoking; recent administration of large doses of iron or vitamin B6; hydrogen peroxide in enemas or other procedures.
References
- ↑ 1.0 1.1 Rodgers AD, Cummins AG (2007). "CRP correlates with clinical score in ulcerative colitis but not in Crohn's disease". Dig Dis Sci. 52 (9): 2063–8. doi:10.1007/s10620-006-9691-2. PMID 17436102.
- ↑ 2.0 2.1 Vermeire S, Van Assche G, Rutgeerts P (2004). "C-reactive protein as a marker for inflammatory bowel disease". Inflamm Bowel Dis. 10 (5): 661–5. PMID 15472532.
- ↑ Al-Ataie MB, Shinoy VN. eMedicine: Ulcerative colitis. Fulltext.
- ↑ 4.0 4.1 Ulcerative Colitis Practice Guidelines in Adults, Am. Coll. Gastroenterology, 2004. PDF
- ↑ Prantera C, Davoli M, Lorenzetti R, Pallone F, Marcheggiano A, Iannoni C; et al. (1988). "Clinical and laboratory indicators of extent of ulcerative colitis. Serum C-reactive protein helps the most". J Clin Gastroenterol. 10 (1): 41–5. PMID 3356884.
- ↑ van Rheenen PF, Van de Vijver E, Fidler V (2010). "Faecal calprotectin for screening of patients with suspected inflammatory bowel disease: diagnostic meta-analysis". BMJ. 341: c3369. doi:10.1136/bmj.c3369. PMC 2904879. PMID 20634346. Review in: Ann Intern Med. 2011 Jan 18;154(2):JC1-12