Ulcerative colitis laboratory findings
|
Ulcerative colitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ulcerative colitis laboratory findings On the Web |
|
American Roentgen Ray Society Images of Ulcerative colitis laboratory findings |
|
Risk calculators and risk factors for Ulcerative colitis laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [2]
Overview
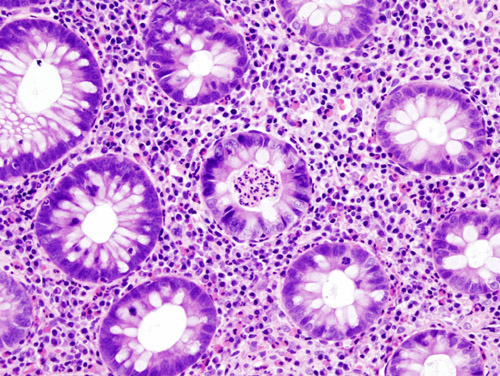
The laboratory findings in a patient with ulcerative colitis include anemia, low albumin, elevated ESR, elevated serum alkaline phosphatase, deranged LFTs and electrolyte abnormalities.[1][2]
Laboratory Findings
The initial diagnostic workup for ulcerative colitis includes the following:[3][4][1][2][5][6]
- A complete blood count shows
- Anemia
- Thrombocytosis
- A high platelet count
- Elvated ESR (>30mm/hr)
- Low albumin
- Electrolyte studies and renal function tests are done, as chronic diarrhea may be associated with
- Hypokalemia
- Hypomagnesemia
- Pre-renal failure
- Liver function tests are performed to screen for bile duct involvement: primary sclerosing cholangitis.
- Fecal lactoferrin or calprotectin may be checked to depict intestinal inflammation
- Urinalysis
- Elevated serum alkaline phosphatase (in case of uc and psc)
- Stool culture, to rule out parasites and infectious causes.
- C-reactive protein can be measured, with an elevated level being another indication of inflammation.
Although ulcerative colitis is a disease of unknown causation, inquiry should be made as to unusual factors believed to trigger the disease.[4] Factors may include: recent cessation of tobacco smoking; recent administration of large doses of iron or vitamin B6; hydrogen peroxide in enemas or other procedures.
References
- ↑ 1.0 1.1 Rodgers AD, Cummins AG (2007). "CRP correlates with clinical score in ulcerative colitis but not in Crohn's disease". Dig Dis Sci. 52 (9): 2063–8. doi:10.1007/s10620-006-9691-2. PMID 17436102.
- ↑ 2.0 2.1 Vermeire S, Van Assche G, Rutgeerts P (2004). "C-reactive protein as a marker for inflammatory bowel disease". Inflamm Bowel Dis. 10 (5): 661–5. PMID 15472532.
- ↑ Al-Ataie MB, Shinoy VN. eMedicine: Ulcerative colitis. Fulltext.
- ↑ 4.0 4.1 Ulcerative Colitis Practice Guidelines in Adults, Am. Coll. Gastroenterology, 2004. PDF
- ↑ Prantera C, Davoli M, Lorenzetti R, Pallone F, Marcheggiano A, Iannoni C; et al. (1988). "Clinical and laboratory indicators of extent of ulcerative colitis. Serum C-reactive protein helps the most". J Clin Gastroenterol. 10 (1): 41–5. PMID 3356884.
- ↑ van Rheenen PF, Van de Vijver E, Fidler V (2010). "Faecal calprotectin for screening of patients with suspected inflammatory bowel disease: diagnostic meta-analysis". BMJ. 341: c3369. doi:10.1136/bmj.c3369. PMC 2904879. PMID 20634346. Review in: Ann Intern Med. 2011 Jan 18;154(2):JC1-12