Pulmonary embolism: Difference between revisions
No edit summary |
No edit summary |
||
| Line 75: | Line 75: | ||
* Score 4 or less - PE unlikely. Consider [[D-dimer]] to rule out PE. | * Score 4 or less - PE unlikely. Consider [[D-dimer]] to rule out PE. | ||
== | ==[[Pulmonary embolism differential diagnosis|Differential Diagnosis]]== | ||
==[[Pulmonary embolism history & symptoms|History & Symptoms]]== | ==[[Pulmonary embolism history & symptoms|History & Symptoms]]== | ||
| Line 121: | Line 89: | ||
==[[Pulmonary embolism computed tomography|Computed Tomography]]== | ==[[Pulmonary embolism computed tomography|Computed Tomography]]== | ||
==[[Pulmonary embolism ventilation/perfusion scan|Ventilation/ | ==[[Pulmonary embolism ventilation/perfusion scan|Ventilation/Perfusion scan]]== | ||
==[[Pulmonary embolism echocardiography or ultrasound|Echocardiography or Ultrasound]]== | ==[[Pulmonary embolism echocardiography or ultrasound|Echocardiography or Ultrasound]]== | ||
Revision as of 17:02, 20 July 2011
| Pulmonary embolism | |
 | |
|---|---|
| ICD-10 | I26 |
| ICD-9 | 415.1 |
| DiseasesDB | 10956 |
| MedlinePlus | 000132 |
|
Pulmonary Embolism Microchapters |
|
Diagnosis |
|---|
|
Pulmonary Embolism Assessment of Probability of Subsequent VTE and Risk Scores |
|
Treatment |
|
Follow-Up |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Pulmonary embolism On the Web |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Synonyms and Associated Terms: PE
Pulmonary embolism (PE) is a common illness that can cause death and significant disability. PE occurs when there is an acute obstruction of the pulmonary artery (or one of its branches). Most often this is due to a venous thrombus (blood clot from a vein), which has been dislodged from its site of formation and embolizes to the arterial blood supply of one of the lungs. This process is termed thromboembolism.
Patients present with a wide array of symptoms and signs. These may include difficulty breathing, pain in the chest during breathing, and in more severe cases collapse, circulatory instability and sudden death. PE treatment requires rapid and accurate risk stratification before haemodynamic decompensation and the development of cardiogenic shock. Therapeutic application most often consists of an anticoagulant medication, such as heparin and warfarin, and rarely (in severe cases) with thrombolysis or surgery. In other, rarer forms of pulmonary embolism, material other than a blood clot is responsible; this may include fat or bone (usually in association with significant trauma), air (often when diving), clumped tumor cells, and amniotic fluid (affecting mothers during childbirth).
Epidemiology and Demographics
Risk factors
Pathophysiology
Natural History, Complications & Prognosis
Diagnosis
The diagnosis of PE is based primarily on the clinical evaluation combined with diagnostic modalities such as spiral CT, V/Q scan, use of the D-dimer and lower extremity ultrasound.
Pretest Probability
In spite of all of nonspecific clinical and lab findings, it has been shown that clinicians are actually fairly good at assigning meaningful clinical probabilities for PE.
- In PIOPED, 67% of the patients labeled as having a high clinical probability (>80% likelihood) had PE, as compared with only 9% of those give a low clinical probability (<20% likelihood).
- Unfortunately, the majority of patients (64%) were assigned an intermediate clinical probability (20 – 80% likelihood), reinforcing the fact that a clinical diagnosis can be difficult.
High Pretest Probability
Many authors, reserve the term high pretest probability for those patients with a clinical presentation consistent with PE, in whom an alternative diagnosis is not apparent (e.g. pneumonia) and who have known risk factors for venous thromboembolism (VTE).
Low Pretest Probability
Low pretest probability patients include those patients with an alternative diagnosis to explain the clinical findings or those without risk factors.
Intermediate Pretest Probability
Intermediate probability patients include those patients not fitting either high or low pretest probability definitions.
Predicting the Risk of Pulmonary Embolism
The decision to do medical imaging is usually based on clinical grounds, i.e. the medical history, symptoms and findings on physical examination.
- Development of the Wells score
The most commonly used method to predict clinical probability, the Wells score, is clinical prediction rule, whose use is complicated by multiple versions being available. In 1995, Wells et al initially developed a prediction rule (based on a literature search) to predict the likelihood of PE, based on clinical criteria.[1] The prediction rule was revised in 1998[2] This prediction rule was further revised when simplified during a validation by Wells et al in 2000.[3] In the 2000 publication, Wells proposed two different scoring systems using cutoffs or 2 or 4 with the same prediction rule.[3] In 2001, Wells published results using the more conservative cutoff of 2 to create three categories.[4] An additional version, the "modified extended version", using the more recent cutoff of 2 but including findings from Wells's initial studies[1][2] were proposed.[5] Most recently, a further study reverted to Wells's earlier use of a cutoff of 4 points[3] to create only two categories.[6]
There are additional prediction rules for PE, such as the Geneva rule. More importantly, the use of any rule is associated with reduction in recurrent thromboembolism.[7]
- Wells score
The Wells score:[8]
- clinically suspected DVT - 3.0 points
- alternative diagnosis is less likely than PE - 3.0 points
- tachycardia - 1.5 points
- immobilization/surgery in previous four weeks - 1.5 points
- history of DVT or PE - 1.5 points
- hemoptysis - 1.0 points
- malignancy (treatment for within 6 months, palliative) - 1.0 points
- Interpretation of the Wells score
Traditional interpretation[3][4]
- Score >6.0 - High (probability 59% based on pooled data[9])
- Score 2.0 to 6.0 - Moderate (probability 29% based on pooled data[9])
- Score <2.0 - Low (probability 15% based on pooled data[9])
Alternate interpretation[3][6]
- Score > 4 - PE likely. Consider diagnostic imaging.
- Score 4 or less - PE unlikely. Consider D-dimer to rule out PE.
Differential Diagnosis
History & Symptoms
Physical Examination
Laboratory Findings
Electrocardiogram
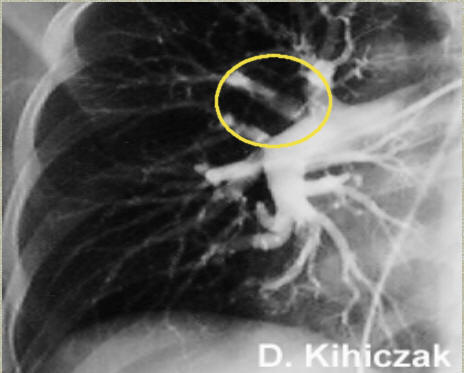
Pulmonary Angiography
Computed Tomography
Ventilation/Perfusion scan
Echocardiography or Ultrasound
Chest Xray
Magnetic Resonance Imaging
Low Probablitity Diagnostic Tests and non-Diagnostic Tests
Tests that are frequently done that are not sensitive for PE, but can be diagnostic.
- Ultrasonography of the legs, also known as leg doppler, in search of deep venous thrombosis (DVT). The presence of DVT, as shown on ultrasonography of the legs, is in itself enough to warrant anticoagulation, without requiring the V/Q or spiral CT scans (because of the strong association between DVT and PE). This may be valid approach in pregnancy, in which the other modalities would increase the risk of birth defects in the unborn child. However, a negative scan does not rule out PE, and low-radiation dose scanning may be required if the mother is deemed at high risk of having pulmonary embolism.
Combining tests into algorithms
Recent recommendations for a diagnostic algorithm have been published by the PIOPED investigators; however, these recommendations do not reflect research using 64 slice MDCT.[9] These investigators recommended:
- Low clinical probability. If negative D-dimer, PE is excluded. If positive D-dimer, obtain MDCT and based treatment on results.
- Moderate clinical probability. If negative D-dimer, PE is excluded. However, the authors were not concerned that a negative MDCT with negative D-dimer in this setting has an 5% probability of being false. Presumably, the 5% error rate will fall as 64 slice MDCT is more commonly used. If positive D-dimer, obtain MDCT and based treatment on results.
- High clinical probability. Proceed to MDCT. If positive, treat, if negative, addition tests are needed to exclude PE.
Medical Therapy
Surgery
Prognosis
Mortality from untreated PE is said to be 26%. This figure comes from a trial published in 1960 by Barrit and Jordan[10] which compared anticoagulation against placebo for the management of PE. Barritt and Jordan performed their study in the Bristol Royal Infirmary in 1957. This study is the only placebo controlled trial ever to examine the place of anticoagulants in the treatment of PE, the results of which were so convincing that the trial has never been repeated as to do so would be considered unethical. That said, the reported mortality rate of 26% in the placebo group is probably an overstatement, given that the technology of the day may have detected only severe PEs.
Prognosis depends on the amount of lung that is affected and on the co-existence of other medical conditions; chronic embolisation to the lung can lead to pulmonary hypertension. There is controversy over whether or not small subsegmental PEs need to be treated at all[11] and some evidence exists that patients with subsegmental PEs may do well without treatment.[12][13]
Predicting mortality
The PESI and Geneva prediction rules can estimate mortality and so may guide selection of patients who can be considered for outpatient therapy.[14]
Right ventricular dysfunction on echocardiography and higher than normal concentrations of troponin identify high risk patients who might need escalation of therapy with thrombolysis or embolectomy even if the blood pressure is normal on presentation.
Evaluation for underlying causes for recurrence
After a first PE, the search for secondary causes is usually brief. Only when a second PE occurs, and especially when this happens while still under anticoagulant therapy, a further search for underlying conditions is undertaken. This will include testing ("thrombophilia screen") for Factor V Leiden mutation, antiphospholipid antibodies, protein C and S and antithrombin levels, and later prothrombin mutation, MTHFR mutation, Factor VIII concentration and rarer inherited coagulation abnormalities.
For prevention of recurrences, when patients are admitted to medical wards or when patients undergo surgery, their physicians should prescribe prophylactic measures to prevent PE. After hospital discharge, prophylaxis should continue for about a month for patients at high risk of thromboembolism.
References
- ↑ 1.0 1.1 Wells PS, Hirsh J, Anderson DR, Lensing AW, Foster G, Kearon C, Weitz J, D'Ovidio R, Cogo A, Prandoni P (1995). "Accuracy of clinical assessment of deep-vein thrombosis". Lancet. 345 (8961): 1326–30. doi:doi:10.1016/S0140-6736(95)92535-X Check
|doi=value (help). PMID 7752753. - ↑ 2.0 2.1 Wells PS, Ginsberg JS, Anderson DR, Kearon C, Gent M, Turpie AG, Bormanis J, Weitz J, Chamberlain M, Bowie D, Barnes D, Hirsh J (1998). "Use of a clinical model for safe management of patients with suspected pulmonary embolism". Ann Intern Med. 129 (12): 997–1005. PMID 9867786.
- ↑ 3.0 3.1 3.2 3.3 3.4 Wells P, Anderson D, Rodger M, Ginsberg J, Kearon C, Gent M, Turpie A, Bormanis J, Weitz J, Chamberlain M, Bowie D, Barnes D, Hirsh J (2000). "Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer". Thromb Haemost. 83 (3): 416–20. PMID 10744147.
- ↑ 4.0 4.1 Wells PS, Anderson DR, Rodger M, Stiell I, Dreyer JF, Barnes D, Forgie M, Kovacs G, Ward J, Kovacs MJ (2001). "Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer". Ann Intern Med. 135 (2): 98–107. PMID 11453709.
- ↑ Sanson BJ, Lijmer JG, Mac Gillavry MR, Turkstra F, Prins MH, Büller HR (2000). "Comparison of a clinical probability estimate and two clinical models in patients with suspected pulmonary embolism. ANTELOPE-Study Group". Thromb. Haemost. 83 (2): 199–203. PMID 10739372.
- ↑ 6.0 6.1 van Belle A, Büller H, Huisman M, Huisman P, Kaasjager K, Kamphuisen P, Kramer M, Kruip M, Kwakkel-van Erp J, Leebeek F, Nijkeuter M, Prins M, Sohne M, Tick L (2006). "Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography". JAMA. 295 (2): 172–9. doi:10.1001/jama.295.2.172. PMID 16403929.
- ↑ Roy PM, Meyer G, Vielle B, Le Gall C, Verschuren F, Carpentier F, Leveau P, Furber A (2006). "Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism". Ann. Intern. Med. 144 (3): 157–64. PMID 16461959.
- ↑ Neff MJ (2003). "ACEP releases clinical policy on evaluation and management of pulmonary embolism". American family physician. 68 (4): 759–60. PMID 12952389.
- ↑ 9.0 9.1 9.2 9.3 Stein PD, Woodard PK, Weg JG, Wakefield TW, Tapson VF, Sostman HD, Sos TA, Quinn DA, Leeper KV, Hull RD, Hales CA, Gottschalk A, Goodman LR, Fowler SE, Buckley JD (2007). "Diagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II Investigators". Radiology. 242 (1): 15–21. doi:10.1148/radiol.2421060971. PMID 17185658.
- ↑ "Anticoagulant drugs in the treatment of pulmonary embolism: a controlled trial". Lancet. 1: 1309&ndash, 1312. 1960. PMID 13797091. Text " Barritt DW, Jorden SC " ignored (help)
- ↑ Le Gal G, Righini M, Parent F, van Strijen M, Couturaud F (2006). "Diagnosis and management of subsegmental pulmonary embolism". J Thromb Haemost. 4 (4): 724–31. PMID 16634736.
- ↑ Perrier A, Bounameaux H (2006). "Accuracy or outcome in suspected pulmonary embolism". N Engl J Med. 354 (22): 2383–5. PMID 16738276.
- ↑ Stein P, Fowler S, Goodman L, Gottschalk A, Hales C, Hull R, Leeper K, Popovich J, Quinn D, Sos T, Sostman H, Tapson V, Wakefield T, Weg J, Woodard P (2006). "Multidetector computed tomography for acute pulmonary embolism". N Engl J Med. 354 (22): 2317–27. PMID 16738268.
- ↑ Jiménez D, Yusen RD, Otero R; et al. (2007). "Prognostic models for selecting patients with acute pulmonary embolism for initial outpatient therapy". Chest. 132 (1): 24–30. doi:10.1378/chest.06-2921. PMID 17625081.
Sources
- Bertucci, V., Asch, M.R., Balter, M., Prognosis in a patient with an initial normal pulmonary angiogram, Chest 1994; 105: 1257-1258.
- Cvitanic, O, Marino, P.L., Improved use of arterial blood gas analysis in suspected pulmonary embolism, Chest 1989; 95: 48-51.
- Drucker, E.A., et.al., Acute pulmonary embolism: assessment of helical CT for diagnosis, Radiology 1998; 209: 235-241.
- Ferrari, E., et.al., The ECG in pulmonary embolism: predictive value of negative T waves in precordial leads – 80 case reports, Chest 1997; 111: 537-543.
- Goldhaber, S.Z., et.al., Quantitative plasma D-dimer levels among patients undergoing pulmonary angiography for suspected pulmonary embolism, JAMA 1993; 270: 2819-2822.
- Goldhaber, S.Z., Pulmonary embolism, NEJM 1998; 339: 93-104.
- Mayo, J.R., et.al., Pulmonary embolism: prospective comparison of spiral CT with ventilation-perfusion scintigraphy, Radiology 1997; 205: 447-452.
- Meaney, J.F.M., et.al., Diagnosis of pulmonary embolism with magnetic resonance angiography, NEJM 1997; 336: 1422-1427.
- The PIOPED investigators, Value of the ventilation / perfusion scan in acute pulmonary embolism: results of the prospective investigation of pulmonary embolism diagnosis (PIOPED), JAMA 1990; 263: 2753-2759.
- Remy-Jardin, M., et.al., Diagnosis of pulmonary embolism with spiral CT: comparison with pulmonary angiography and scintigraphy, Radiology 1996; 200: 6999-706.
- Stein, P.D., et.al., Clinical, laboratory, roentgenographic, and electrocardiographic findings in patients with acute pulmonary embolism and no pre-existing cardiac or pulmonary disease, Chest 1991; 100: 598-603.
- Stein, P.D., et.al., Arterial blood gas analysis in the assessment of suspected pulmonary embolism, Chest 1996; 109: 78-81.
- Thompson, B.T., Hales, C.A., Diagnostic strategies for acute pulmonary embolism, in UpToDate, September 10, 1998.
- Van Erkel, A.R., et.al., Spiral CT angiography for suspected pulmonary embolism: a cost-effective analysis, Radiology 1996; 201: 29-36.
Acknowledgements
The content on this page was first contributed by: Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3] and David Feller-Kopman, M.D.
List of contributors:
For Patients
<youtube v=gGrDAGN5pC0/>
External links
- Vascular Disease Foundation
- Venous Disease Coalition
- Goldminer, Pulmonary embolism
- Images of Pulmonary Embolism
- North American Thrombosis Forum
eo:Pulma embolio ko:폐색전증 nl:Longembolie no:Lungeemboli sr:Плућна емболија