Pre-excitation syndrome
|
Pre-excitation syndrome Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Associate Editor-In-Chief: Shivam Singla, M.D.[2]
Overview
Pre-excitation syndrome is a condition where ventricles of the heart depolarize earlier than the normal leading to premature contraction. Normally the atria and the ventricles are isolated electrically and only electrical passage existing in between atria and ventricles is at Atrioventricular Node. In all pre-excitation syndromes, there is also present an additional conducting pathway beside the AV junction. So the electrical impulses pass to the ventricles even before the normal wave of depolarization that is about to conduct through the AV node. This mechanism of depolarization of ventricles through an additional accessory pathway ( Bundle of Kent) much earlier than the usual depolarization pathway (through AV node) is referred to as "Pre- Excitation". The secondary conduction pathways are generally named as Bundle of His.
The typical ECG findings are shortened PR interval & widened QRS interval with a slight slurring in the upstroke region. The clinical syndrome of the above clinical finding of ECG and history of SVT is referred to as Wolff-Parkinson-White syndrome. pre-excitation syndromes are getting more common in the pediatric population as well. The main component is the presence of an additional accessory bypass pathway in the heart through which the impulse conducts faster than the physiological conduction through AV node, resulting in quick depolarization ofventricles and leads to dangerous arrhythmias. The most common subtype is Wolf-Parkinson -White syndrome. The severe consequences range from arrhythmias, SVT, and sudden cardiac death. The main therapeutic measures for managing the patients are pharmacotherapy and ablation therapy.
Historical Perspective
- WPW syndrome was described in 1930 and named for the John Parkinson, Paul Dudley White, and Louis Wolff.
- They successfully interpreted a series of 11 healthy young patients who had repeated attacks of tachycardia in the presence of short PR interval and bundle branch block pattern on the ECG findings.
- British physiologist "Albert Frank Stanley Kent" (1863 - 1958), first described the lateral branches of AV grove of the monkey heart, which was later named accessory bundle of Kent.
- In 1915, Frank Norman Wilson became the first to describe the condition which would later be referred to as Wolff–Parkinson–White syndrome.
- In 1930, it was first described by Louis Wolff, John Parkinson, and Paul Dudley White.
- They also found the association of WPW with increasing the risk of sudden cardiac death.
Classification
- Pre-excitation syndrome may be classified into sub-types
| Type | Conduction pathway | QRS interval | PR interval | Delta wave |
|---|---|---|---|---|
| Wolff-Parkinson-White syndrome | Bundle of Kent | Wide/long | Usually short | yes |
| Lown-Ganong-Levine syndrome | "James bundle" (atria to bundle of His) | Normal/Unaffected | Short | no |
| Mahaim-type | Mahaim fibers | long | normal |
- Based on their conduction properties, three types of Accessory pathways are there:
- Manifest Accessory Pathways: Conducts more rapidly as compared to AV nodal conduction. Delta waves will commonly be seen on ECG.
- Concealed Accessory Pathways: Conducts in the retrograde direction. As its name represents, the changes in ECG will be concealed. No delta waves will be seen.
- Latent Accessory Pathways: These are located in the lateral part of the heart as compared to AV node. So the impulses will be delayed in traveling to ventricles through the AV node which is at a much shorter distance as compared to latent fibers that are at the far another end.
Pathophysiology
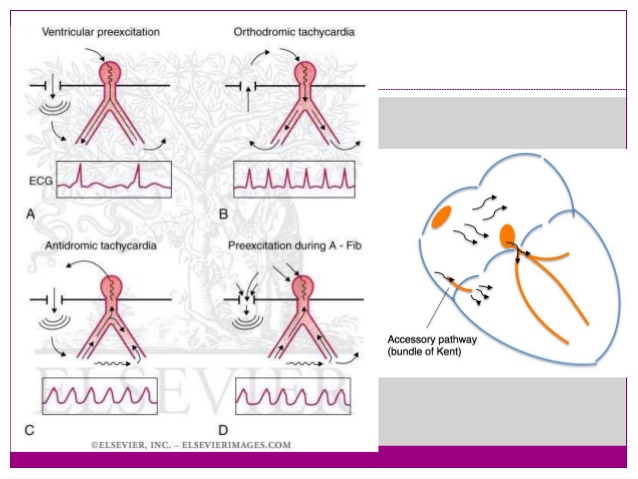
Basic concept of Pathophysiology in pre-excitation syndrome lies in the concept of bypassing the AV node conduction and letting the impulse conduct faster through atria to ventricles via accessory pathways.
These accessory pathways Usually called Bundle of Kent in WPW syndrome, James fiber in LGL syndrome and Mahaim fibers in Mahaim type pre-excitation syndrome. These conducts impulses in forward (not common), backward ( around 15-20%) and in both directions ( Most common type) as well.
The accessory pathways mediate the occurrence of tachyarrhythmia by forming a re-entry circuit and commonly known as AVRT. The direct conduction of impulses from atria to ventricles can also result in the development of tachyarrhythmia's when there is a development of Atrial Fibrillation with RVR
WPW Syndrome
- WPW syndrome is a combination of WPW pattern on ECG + Paroxysmal arrhythmias. The accessory pathways are usually named as Bundle of Kent or AV bypass tracts.
- ECG features of WPW syndrome are
- Short PR interval <120 ms ( < .12 seconds) with Normal P wave morphology.
- Widened QRS complex ( >.12 seconds)
- Delta wave - slurring upstroke of the initial QRS complex due to the early and rapid depolarization of ventricles, the most important criteria for the diagnosis of WPW syndrome.
- Deflection of T waves opposite to the direction of QRS complexes / Secondary changes in ST-segment and T wave.
- Types of AVRT varies depending on the direction of the impulse conduction in the re-entry circuit (orthodromic or antidromic). Orthodromic AVRT means the antegrade conduction will be through the AV node and retrograde will be through the accessory pathway - presents with narrow QRS complexes on ECG. Antidromic AVRT means the antegrade conduction will be through the AP and retrograde conduction through AV node - presents with wide complex QRS complexes on ECG. SO, in short, the Orthodromic AVRT preexcitation syndrome will present with narrow complex tachycardia and Antodromic AVRT pre-excitation syndrome will present with wide complex tachycardias.
- AF with RVR can be diagnosed in patients with WPW by comparing it with the baseline ECG. Means look for comparison between pre-excited QRS complexes on the baseline ECG vs those seen during irregular tachycardia.
- Mainly categorized into 2 subtypes
- Type A - Positive delta wave
- Type B - Negative delta wave
Lown-Ganong-Levine(LGL)Syndrome
- The accessory pathways here are named as James fibers, also known as atrionodal fibers connecting the atrium to the distal AV node. These usually conduct the impulses from atria to the initial portion of the AV node.
- ECG features:
- PR interval is less than 120ms or .12 seconds with usual normal P wave morphology
- Normal QRS complex
- Absence of delta waves
- Episodic paroxysmal SVT
Mahaim-Type Pre-excitation
- The accessory pathways named as mahaim fibers connect the Atrium, AV node, or bundle of His to the Purkinje fibers or ventricular myocardium.
- ECG findings are usually normal
Differentiating Pre-excitation Syndrome from other Diseases
| Arrhythmia | Rhythm | Rate | P wave | PR Interval | QRS Complex | Response to Maneuvers | Epidemiology | Co-existing Conditions | |
|---|---|---|---|---|---|---|---|---|---|
| Atrial Fibrillation (AFib) |
|
|
|
|
|
| |||
| Atrial Flutter |
|
|
|
|
|
||||
| Atrioventricular nodal reentry tachycardia (AVNRT)'''' |
|
|
|
|
|
|
|||
| Multifocal Atrial Tachycardia |
|
|
|
|
|
|
|
||
| Paroxysmal Supraventricular Tachycardia |
|
|
|
|
|
|
|
||
| Premature Atrial Contractrions (PAC) |
|
|
|
|
|
|
|||
| Wolff-Parkinson-White Syndrome |
|
|
|
|
|
|
|
| |
| Ventricular Fibrillation (VF) |
|
|
|
|
|
|
|
| |
| Ventricular Tachycardia |
|
|
|
|
|
|
|
|
Epidemiology and Demographics
- WPW is commonly found with an incidence of around 0.1-3.0 per thousand population.
- More common in the male population as compared to females.
- Familial studies are done to found its association proved that around .55% more commonly found in first degree relatives.
- More common in young and healthy individuals and as the age advances the prevalence of disease decreases because of loss of pre-excitation.
- WPW can be considered as a congenital anomaly in some cases where it is usually present since birth and in others and it is regarded as a developmental anomaly. Studies proved it's lower prevalence in children aged between 6-13 than those in the age group of 14-15 years of age.
Risk Factors
High-risk population for development of atrial fibrillation or sudden cardiac death include:
- Policemen
- Athletes
- Firemen
- Pilots
- Steelworkers
- Male gender
- Age (peak ages for the development of atrial fibrillation include 30 years and 50 years)
- Past history of syncope
Natural History, Complications and Prognosis
Natural History
- There are a lot of studies being done in the past to describe the natural history or disease course of pre-excitation syndrome. But data from a recent study- "Long term natural history of patients with WPW treated with or without catheter ablation" showed promising results in explaining the reduced long-term mortality rates in WPW patients who are matched for age and gender. Also explained the lower mortality rates in catheter ablated patients as compared to non ablated ones.
Complications
- Most common complications studied in patients having accessory pathway conduction are Arrhythmias and Sudden cardiac death
- Tachyarrhythmias:
- If there is a development of atrial fibrillation or flutter then there is fast conduction across the tracts leads to an increased risk of dangerous ventricular arrhythmias.
- AV nodal blocking agents may also be the factor responsible for the increased conduction through accessory pathways causing life-threatening ventricular arrhythmias or hemodynamic instability resulting and with a worse prognosis.
- Sudden cardiac death:
- Sudden cardiac death as a complication in patients with AP conduction is more common in a young male with age less than 35, history of arrhythmias in the past, anatomical location of accessory pathway- that is the septal location of the accessory pathway, having multiple accessory pathways.
- The studies proved the risk of sudden cardiac death related to the pre-excitation syndrome is around 1.5% in childhood with the highest risk in the first two decades of life.
Prognosis
- Prognosis is usually very good till the time patient is getting managed and treated appropriately.
- Catheter ablation showed promising results in the curative treatment of patients suffering from this disorder.
- Sudden cardiac death is rarely seen in patients with this syndrome but when it happens it is most commonly related to arrhythmias.
- The most common misconception about the prognosis of WPW syndrome is related to the severity of symptoms in a patient but the most important determinant of prognosis is the dependence on the electrophysiologic properties of the accessory pathways.
- The conduction through accessory pathways usually decreases with age. This is due to fibrotic changes that happen with time.
Diagnosis
WPW Syndrome
- WPW syndrome is a combination of WPW pattern on ECG + Paroxysmal arrhythmias. The accessory pathways are usually named as Bundle of Kent or AV bypass tracts.
- ECG features of WPW syndrome are
- Short PR interval <120 ms ( < .12 seconds) with Normal P wave morphology.
- Widened QRS complex ( >.12 seconds)
- Delta wave - slurring upstroke of the initial QRS complex due to the early and rapid depolarization of ventricles, the most important criteria for the diagnosis of WPW syndrome.
- Deflection of T waves opposite to the direction of QRS complexes / Secondary changes in ST-segment and T wave.
- Types of AVRT varies depending on the direction of the impulse conduction in the re-entry circuit (orthodromic or antidromic). Orthodromic AVRT means the antegrade conduction will be through the AV node and retrograde will be through the accessory pathway - presents with narrow QRS complexes on ECG. Antidromic AVRT means the antegrade conduction will be through the AP and retrograde conduction through AV node - presents with wide complex QRS complexes on ECG. SO, in short, the Orthodromic AVRT preexcitation syndrome will present with narrow complex tachycardia and Antidromic AVRT pre-excitation syndrome will present with wide complex tachycardia.
- AF with RVR can be diagnosed in patients with WPW by comparing it with the baseline ECG. Means look for comparison between pre-excited QRS complexes on the baseline ECG vs those seen during irregular tachycardia.
- Mainly categorized into 2 subtypes
- Type A - Positive delta wave
- Type B - Negative delta wave
Lown-Ganong-Levine(LGL) Syndrome
- The accessory pathways here are named as James fibers, also known as atrionodal fibers connecting the atrium to the distal AV node. These usually conduct the impulses from atria to the initial portion of the AV node.
- ECG features:
- PR interval is less than 120ms or .12 seconds with usual normal P wave morphology
- Normal QRS complex
- Absence of delta waves
- Episodic paroxysmal SVT
Mahaim-Type Pre-excitation
- The accessory pathways named as Mahaim fibers connect the Atrium, AV node, or bundle of His to the Purkinje fibers or ventricular myocardium.
- ECG findings are usually normal
History and Symptoms
People with Pre- Excitation syndromes may be asymptomatic, however, the individuals commonly experience the following symptoms:
- Palpitations
- Dizziness or lightheadedness.
- Shortness of breath.
- Chest pain
- Fatigue.
- Anxiety.
- Fainting
- Difficulty breathing
Treatment
Medical Treatment
HEMODYNAMICALY UNSTABLE PATIENT -- DIRECT SYNCHRONIZED CARDIOVERSION, BIPHASIC ( 100 J INITIAL LATER ON 200j OR 360J.
HEMODYNAMICALLY STABLE PATIENTS -- FOLLOWING ALGORITHM CAN BE FOLLOWED,
GENERAL PROTOCOL
- Antiarrhythmic drug
- Helps in slowing the accessory pathway conduction and thus plays a major role in the acute events.
- AV Nodal blocking agents should NOT be used
- As they aggravate WPW by increasing the conduction through the accessory pathway.
- Address the underlying cause triggering dysrhythmias which includes
- Coronary artery disease
- Cardiomyopathy
- Electrolyte derangement
- Anemia
- Thyroid disease
IN CASE OF ACUTE AVRT/AVNRT
- Treated by blocking the AV nodal conduction
- Help in blocking the pathways responsible for causing dysrhythmias through the involvement of the AV node (AVRT/AVNRT).
- Vagal Maneuvers - Valsalva maneuver, immersing the face in cold water or ice water, carotid sinus massage
- IV Adenosine- very short half-life and commonly used in dose around 6-12 mg
- IV Verapamil- this is a calcium channel blocker and commonly used as 5-10 mg.
ATRIAL FLUTTER/FIBRILLATION
- If wide complex tachycardia is present
- Use IV Amiodarone or Procainamaide
RADIOFREQUENCY ABLATION
- This modality has replaced drug therapy and other surgical treatment options by showing promising results. Best results are studied these days when it is used in conjunction with cryoblation (commonly used for septal Accessory pathways and for accessory pathways near small coronary arteries)
- This technique is used widely with best results in:
- Patients with AVRT showing symptoms of dysrhythmias
- Patients with impaired functional daily activities having no symptoms with ventricular preexcitation
- Patients with WPW and family history of sudden cardiac death in first or second-degree relatives.
- Patients with AVRT OR A.FIB with RVR
- Patients with h/o Pre-excited A.FIB
- Patients who are not willing to undergo radiofrequency ablation can be managed on medical management with the use of Anti-arrhythmics. Though its role in the prevention of future episodes of arrhythmias is limited still this is the most commonly used modality of choice.
Class 3 Antiarrhythmics and class Ic drugs are used with AV nodal blocking agents in patients with a history of atrial flutter or A.Fib.Sotalol and Flecainide would be the safe options to use in pregnancy.
Surgery
- Surgery is the mainstay of therapy for [disease name].
- [Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name].
- [Surgical procedure] can only be performed for patients with [disease stage] [disease name].
Prevention
For preventing the recurrence of episodes major options available are
- Radio frequency ablation
- Ablation of accessory pathway tracts
- cures 95% of the time
- Surgery.
- Success rate for surgical ablation is around 100 percent along with lower complication rates. Radiofrequency ablation is a less invasive option and preferred over surgery.
- Surgery can be considered if a patient is undergoing cardiac surgery for other reasons such as CABG or other heart valve surgery.
- Medications
- Although Medications can prevent recurrent episodes of tachycardia they are only used on patients who are not the candidates for ablation or surgery.
- These patients must be taught to perform Valsalva maneuvers that can relieve tachycardia during the episodes.