Lymphoplasmacytic lymphoma physical examination: Difference between revisions
Sara Mohsin (talk | contribs) (→HEENT) |
(→HEENT) |
||
| (16 intermediate revisions by 2 users not shown) | |||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
Patients with | [[Patients]] with [[lymphoplasmacytic lymphoma]] usually [[Appearance|appear]] oriented to [[Time constant|time]], place, and [[person]]. [[Physical examination]] of [[patients]] with [[lymphoplasmacytic lymphoma]] is usually remarkable for various findings [[Dependency ratio|depending]] on the [[Degree (angle)|degree]] of [[Tissue (biology)|tissue]] [[Infiltration (medical)|infiltration]] by [[malignant]] [[Tumor cell|tumor cells]], [[hyperviscosity syndrome]], and accumulation of [[paraprotein]]. Common [[Physical examination|physical exam]] findings include [[Maculopapular rash|maculopapular lesions]], [[purpura]], [[petechiae]], [[raynaud's phenomenon]], [[Skin ulcer|skin ulcers]], [[skin]] [[necrosis]], [[cold urticaria]], [[macroglobulinemia]] [[Cutis (anatomy)|cutis]], [[pallor]], [[papilledema]], [[retinopathy]], [[lymphadenopathy]], [[jugular venous distension]], [[pleural effusion]], [[lung]] [[rales]], [[pulmonary]] [[Infiltration (medical)|infiltrates]], [[Displaced point of maximal impulse|displaced apical impulse]], [[S3 gallop]], [[hepatosplenomegaly]] [[Causes|causing]] [[abdominal distension]], [[peripheral edema]] due to [[congestive heart failure]], and [[distal]], [[Symmetric function|symmetric]], [[sensorimotor]] [[peripheral neuropathy]]. | ||
==Physical Examination== | ==Physical Examination== | ||
====General Appearance==== | ====General Appearance==== | ||
Patients with | [[Patients]] with [[lymphoplasmacytic lymphoma]] are generally well-[[Appearance|appearing]].<ref name="aa">Waldenström's macroglobulinemia. MedlinePlus (2015) https://www.nlm.nih.gov/medlineplus/ency/article/000588.htm Accessed on November 15th, 2015</ref> | ||
====Skin==== | ====Skin==== | ||
*Maculopapular lesions, plaques, or nodules | *[[Maculopapular]] [[lesions]], [[plaques]], or [[nodules]]<ref name="pmid12883242">{{cite journal| author=Lin P, Bueso-Ramos C, Wilson CS, Mansoor A, Medeiros LJ| title=Waldenstrom macroglobulinemia involving extramedullary sites: morphologic and immunophenotypic findings in 44 patients. | journal=Am J Surg Pathol | year= 2003 | volume= 27 | issue= 8 | pages= 1104-13 | pmid=12883242 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12883242 }} </ref><ref name="pmid10188670">{{cite journal| author=Daoud MS, Lust JA, Kyle RA, Pittelkow MR| title=Monoclonal gammopathies and associated skin disorders. | journal=J Am Acad Dermatol | year= 1999 | volume= 40 | issue= 4 | pages= 507-35; quiz 536-8 | pmid=10188670 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10188670 }} </ref><ref name="pmid9198063">{{cite journal| author=Veltman GA, van Veen S, Kluin-Nelemans JC, Bruijn JA, van Es LA| title=Renal disease in Waldenström's macroglobulinaemia. | journal=Nephrol Dial Transplant | year= 1997 | volume= 12 | issue= 6 | pages= 1256-9 | pmid=9198063 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9198063 }} </ref> | ||
*[[Purpura]] | *[[Purpura]] | ||
*[[Raynaud phenomenon]] | *[[Raynaud phenomenon]] | ||
*[[Petechiae]] (if platelet count is low) | *[[Petechiae]] (if [[platelet count]] is low) | ||
*Skin ulcers | *[[Skin]] [[ulcers]] | ||
*Skin necrosis | *[[Skin]] [[necrosis]] | ||
*Cold urticaria | *[[Cold urticaria]] | ||
*Firm, flesh-colored skin papules and nodules also called macroglobulinemia cutis | *Firm, [[flesh]]-[[Color|colored]] [[skin]] [[papules]] and [[nodules]] also called [[macroglobulinemia]] [[Cutis (anatomy)|cutis]]<ref name="pmid10188670">{{cite journal| author=Daoud MS, Lust JA, Kyle RA, Pittelkow MR| title=Monoclonal gammopathies and associated skin disorders. | journal=J Am Acad Dermatol | year= 1999 | volume= 40 | issue= 4 | pages= 507-35; quiz 536-8 | pmid=10188670 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10188670 }} </ref> | ||
{| | {| | ||
| | | | ||
[[File:Penile ulcer. wm. | [[File:Penile ulcer. wm gif.gif|thumb|250px|none| [[Lesion]] measuring 4 centimeters on the penis base, with a clear background source[https://openi.nlm.nih.gov/detailedresult.php?img=PMC4861576_abd-91-02-0236-g01&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=62 : Oliveira CC. et al, Universidade do Oeste Paulista, Presidente Prudente, SP, Brazil.]]] | ||
| | | | ||
[[File:Hyperpigmented nodules | [[File:Hyperpigmented nodules gif.gif|thumb|250px|none| Hyperpigmented nodules with hemorrhagic crusting on the back.[https://openi.nlm.nih.gov/detailedresult.php?img=PMC3886335_CRIM.ONCMED2013-890864.001&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=80 Source: Haider S. et al, Department of Internal Medicine, University of Cincinnati College of Medicine, Cincinnati, OH 45267, USA.]]] | ||
| | | | ||
[[File:Ulcers tingling. | [[File:Ulcers tingling gif.gif|thumb|250px|none|The patient presented with tingling ulcers on the feet. [Copyright: ©2013 Fischer et al.]Figure 1B. On further examination, papules were noted on the knees. [Copyright: ©2013 Fischer et al.]Figure1C. Biopsy from a knee papule showed homogeneous extra-vascular eosinophilic hyaline deposits throughout the papillary and reticular dermis (H&E 40×). [Copyright: ©2013 Fischer et al.]Figure 1D. IgM stain demonstrates the extravascular IgM deposits in the dermis (40×). [Copyright: ©2013 Fischer et al.][https://openi.nlm.nih.gov/detailedresult.php?img=PMC3791964_dp0303a03g001&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=37 Source: Fischer I. et al, Department of Dermatology, Klinikum Schwabing, Munich, Germany.]]] | ||
|} | |} | ||
====HEENT==== | ====HEENT==== | ||
*[[Pallor]] | *[[Pallor]] | ||
*[[Papilledema]] | *[[Papilledema]] | ||
*Malignant | *[[Malignant]] vitritis<ref name="pmid6801795">{{cite journal| author=Orellana J, Friedman AH| title=Ocular manifestations of multiple myeloma, Waldenström's macroglobulinemia and benign monoclonal gammopathy. | journal=Surv Ophthalmol | year= 1981 | volume= 26 | issue= 3 | pages= 157-69 | pmid=6801795 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6801795 }} </ref> | ||
*Congestion/sludging of blood in conjunctival vessels | *[[Congestion]]/sludging of [[blood]] in [[conjunctival]] [[vessels]] | ||
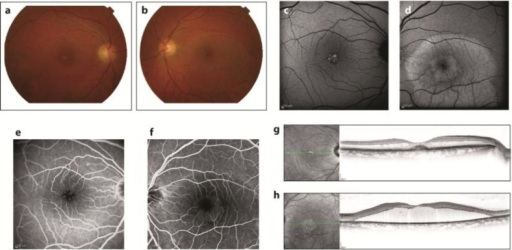
*Retinitis/retinopathy including dilation, segmentation and tortuosity of retinal vessels, mid-peripheral retinal hemorrhages, serous retinal/macular neurosensory detachment, blurred disc margins and fundal exudates on fundoscopic examination | *[[Retinitis]]/[[retinopathy]] including [[dilation]], [[segmentation]] and [[tortuosity]] of [[retinal]] [[vessels]], mid-peripheral [[retinal]] [[hemorrhages]], [[serous]] [[retinal]]/[[macular]] neurosensory detachment, blurred [[disc margins]] and [[Fundus (eye)|fundal]] [[Exudate|exudates]] on [[Fundoscopy|fundoscopic examination]]<ref name="pmid16044069">{{cite journal| author=Pilon AF, Rhee PS, Messner LV| title=Bilateral, persistent serous macular detachments with Waldenström's macroglobulinemia. | journal=Optom Vis Sci | year= 2005 | volume= 82 | issue= 7 | pages= 573-8 | pmid=16044069 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16044069 }} </ref><ref name="pmid2507620">{{cite journal| author=Avashia JH, Fath DF| title=Bilateral central retinal vein occlusion in Waldenström's macroglobulinemia. | journal=J Am Optom Assoc | year= 1989 | volume= 60 | issue= 9 | pages= 657-8 | pmid=2507620 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2507620 }} </ref><ref name="pmid3081619">{{cite journal| author=Goen TM, Terry JE| title=Mid-peripheral hemorrhages secondary to Waldenström's macroglobulinemia. | journal=J Am Optom Assoc | year= 1986 | volume= 57 | issue= 2 | pages= 109-12 | pmid=3081619 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3081619 }} </ref> | ||
* | *[[Fundoscopy|Fundoscopic examination]] should be [[Performance status|performed]] in all [[patients]] with [[symptoms]] of [[hyperviscosity]] and/or [[IgM]] ≥3000 mg/dL | ||
{| | {| | ||
| | | | ||
[[File: | [[File:Retinal veins dilation gif.gif|thumb|300px|none|Ophthalmoscopic examination revealed dilatation and tortuosity of the retinal veins.[https://openi.nlm.nih.gov/detailedresult.php?img=PMC3102879_jkms-26-824-g004&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=43 Source: Kim YL. et al, Department of Internal Medicine, Eulji University College of Medicine, Seoul, Korea.]]] | ||
| | | | ||
[[File: | [[File:Retinal vein gif.gif|thumb|300px|none|[[Ophthalmology|Ophthalmologic]] findings in the presented case. The [[Optic disc|optic disk]] of the left [[eye]] is shown. The perivenous sheathing is indicated (black arrow). [https://openi.nlm.nih.gov/detailedresult.php?img=PMC4163423_CRIONM2014-165670.002&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=30 Source: Nipp R. et al, Dana-Farber Cancer Institute, 450 Brookline Avenue, Boston, MA 02215, USA.]]] | ||
|- | |||
| | | | ||
[[File:Fluorescein angiography. | [[File:After therapy.png|thumb|300px|none| One year after therapy. The right [[fundus]] exhibited a roundish, subretinal, pseudovitelliform deposit (a). The deposit displayed uneven hyper-[[autofluorescence]] on a fundus [[autofluorescence]] photograph (c) and an uneven staining in [[fluorescein angiography]] (e). It was associated with [[macular edema]] in an [[OCT]] horizontal scan (g). The left eye fundus exhibited a large retinal [[serous]] detachment (b), with the accumulation of hyper-autofluorescent [[lipofuscin]] material in [[autofluorescence]] fundus photography (d). [[Fluorescein angiography]] was not contributive (f), but OCT showed the absence of central [[photoreceptors]] (h). [https://openi.nlm.nih.gov/detailedresult.php?img=PMC3433005_cop-0003-0236-g02&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=27 Source: Brolly A. et al, Department of Ophthalmology, APHP, Hôpital Lariboisière, University Paris Diderot, Sorbonne Paris Cité, Bourges, France.]]] | ||
| | |||
[[File:Flor angiography gif.gif|thumb|300px|none| [[Fluorescein angiography]]: [[Hyperviscosity syndrome|Hyperviscosity]] syndrome characterized by bilateral retinal venous dilation and [[tortuosity]], retinal [[hemorrhages]] and peripheral microaneurysms.[https://openi.nlm.nih.gov/detailedresult.php?img=PMC3433005_cop-0003-0236-g01&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=26 Source: Brolly A. et al, Department of Ophthalmology, APHP, Hôpital Lariboisière, University Paris Diderot, Sorbonne Paris Cité, Bourges, France.]]] | |||
|} | |} | ||
====Neck==== | ====Neck==== | ||
*[[Lymphadenopathy]] | *[[Lymphadenopathy]]<ref name="DimopoulosPanayiotidis2000">{{cite journal|last1=Dimopoulos|first1=Meletios A.|last2=Panayiotidis|first2=Panayiotis|last3=Moulopoulos|first3=Lia A.|last4=Sfikakis|first4=Petros|last5=Dalakas|first5=Marinos|title=Waldenström’s Macroglobulinemia: Clinical Features, Complications, and Management|journal=Journal of Clinical Oncology|volume=18|issue=1|year=2000|pages=214–214|issn=0732-183X|doi=10.1200/JCO.2000.18.1.214}}</ref> | ||
*[[Jugular venous distension]] | *[[Jugular venous distension]] | ||
====Respiratory==== | ====Respiratory==== | ||
*[[Pleural effusion]] - in 3-5% of patients | *[[Pleural effusion]] - in 3-5% of [[patients]]<ref name="pmid9671845">{{cite journal| author=Fadil A, Taylor DE| title=The lung and Waldenström's macroglobulinemia. | journal=South Med J | year= 1998 | volume= 91 | issue= 7 | pages= 681-5 | pmid=9671845 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9671845 }} </ref> | ||
*[[Rales]] on auscultation | *[[Rales]] on [[auscultation]] | ||
*Pulmonary infiltrates, nodules, masses | *[[Pulmonary]] [[Infiltration (medical)|infiltrates]], [[nodules]], [[Mass|masses]]<ref name="pmid9671845">{{cite journal| author=Fadil A, Taylor DE| title=The lung and Waldenström's macroglobulinemia. | journal=South Med J | year= 1998 | volume= 91 | issue= 7 | pages= 681-5 | pmid=9671845 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9671845 }} </ref> | ||
====Cardiovascular system==== | ====Cardiovascular system==== | ||
*[[Apical impulse|Displaced apical impulse]] | *[[Apical impulse|Displaced apical impulse]] | ||
*[[S3 gallop]] | *[[S3 gallop]] | ||
====Abdomen==== | ====Abdomen==== | ||
*Swollen abdomen/belly | *[[Swollen belly|Swollen abdomen/belly]] | ||
*[[Splenomegaly]] | *[[Splenomegaly]] | ||
*[[Hepatomegaly]] | *[[Hepatomegaly]] | ||
====Extremity==== | ====Extremity==== | ||
*[[Raynaud phenomenon]] | *[[Raynaud phenomenon]] | ||
*Patients may have [[peripheral edema]] if disease is complicated by [[congestive heart failure]] | *[[Patients]] may have [[peripheral edema]] if [[disease]] is [[Complication|complicated]] by [[congestive heart failure]] | ||
====Neuromuscular==== | ====Neuromuscular==== | ||
*[[Peripheral neuropathy]] - distal, symmetric, and sensorimotor | *[[Peripheral neuropathy]] - [[distal]], [[Symmetric function|symmetric]], and [[sensorimotor]]<ref name="cns">{{cite journal |vauthors=Coimbra J, Costa AP, Pita F, Rosado P, de Almeida LB |title=[Neuropathy in Waldenstrom's macroglobulinemia] |language=Portuguese |journal=Acta Med Port |volume=8 |issue=4 |pages=253–7 |year=1995 |pmid=7625222 |doi= |url=}}</ref> | ||
==References== | ==References== | ||
| Line 77: | Line 79: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category: | [[Category:Disease]] | ||
[[Category:Blood]] | |||
[[Category:Hematology]] | |||
Latest revision as of 14:34, 29 October 2019
|
Lymphoplasmacytic lymphoma Microchapters |
|
Differentiating Lymphoplasmacytic Lymphoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Lymphoplasmacytic lymphoma physical examination On the Web |
|
American Roentgen Ray Society Images of Lymphoplasmacytic lymphoma physical examination |
|
Risk calculators and risk factors for Lymphoplasmacytic lymphoma physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mohsin, M.D.[2]
Overview
Patients with lymphoplasmacytic lymphoma usually appear oriented to time, place, and person. Physical examination of patients with lymphoplasmacytic lymphoma is usually remarkable for various findings depending on the degree of tissue infiltration by malignant tumor cells, hyperviscosity syndrome, and accumulation of paraprotein. Common physical exam findings include maculopapular lesions, purpura, petechiae, raynaud's phenomenon, skin ulcers, skin necrosis, cold urticaria, macroglobulinemia cutis, pallor, papilledema, retinopathy, lymphadenopathy, jugular venous distension, pleural effusion, lung rales, pulmonary infiltrates, displaced apical impulse, S3 gallop, hepatosplenomegaly causing abdominal distension, peripheral edema due to congestive heart failure, and distal, symmetric, sensorimotor peripheral neuropathy.
Physical Examination
General Appearance
Patients with lymphoplasmacytic lymphoma are generally well-appearing.[1]
Skin
- Maculopapular lesions, plaques, or nodules[2][3][4]
- Purpura
- Raynaud phenomenon
- Petechiae (if platelet count is low)
- Skin ulcers
- Skin necrosis
- Cold urticaria
- Firm, flesh-colored skin papules and nodules also called macroglobulinemia cutis[3]
 |
 |
 |
HEENT
- Pallor
- Papilledema
- Malignant vitritis[5]
- Congestion/sludging of blood in conjunctival vessels
- Retinitis/retinopathy including dilation, segmentation and tortuosity of retinal vessels, mid-peripheral retinal hemorrhages, serous retinal/macular neurosensory detachment, blurred disc margins and fundal exudates on fundoscopic examination[6][7][8]
- Fundoscopic examination should be performed in all patients with symptoms of hyperviscosity and/or IgM ≥3000 mg/dL
 |
 |
 |
 |
Neck
Respiratory
- Pleural effusion - in 3-5% of patients[10]
- Rales on auscultation
- Pulmonary infiltrates, nodules, masses[10]
Cardiovascular system
Abdomen
Extremity
- Raynaud phenomenon
- Patients may have peripheral edema if disease is complicated by congestive heart failure
Neuromuscular
References
- ↑ Waldenström's macroglobulinemia. MedlinePlus (2015) https://www.nlm.nih.gov/medlineplus/ency/article/000588.htm Accessed on November 15th, 2015
- ↑ Lin P, Bueso-Ramos C, Wilson CS, Mansoor A, Medeiros LJ (2003). "Waldenstrom macroglobulinemia involving extramedullary sites: morphologic and immunophenotypic findings in 44 patients". Am J Surg Pathol. 27 (8): 1104–13. PMID 12883242.
- ↑ 3.0 3.1 Daoud MS, Lust JA, Kyle RA, Pittelkow MR (1999). "Monoclonal gammopathies and associated skin disorders". J Am Acad Dermatol. 40 (4): 507–35, quiz 536-8. PMID 10188670.
- ↑ Veltman GA, van Veen S, Kluin-Nelemans JC, Bruijn JA, van Es LA (1997). "Renal disease in Waldenström's macroglobulinaemia". Nephrol Dial Transplant. 12 (6): 1256–9. PMID 9198063.
- ↑ Orellana J, Friedman AH (1981). "Ocular manifestations of multiple myeloma, Waldenström's macroglobulinemia and benign monoclonal gammopathy". Surv Ophthalmol. 26 (3): 157–69. PMID 6801795.
- ↑ Pilon AF, Rhee PS, Messner LV (2005). "Bilateral, persistent serous macular detachments with Waldenström's macroglobulinemia". Optom Vis Sci. 82 (7): 573–8. PMID 16044069.
- ↑ Avashia JH, Fath DF (1989). "Bilateral central retinal vein occlusion in Waldenström's macroglobulinemia". J Am Optom Assoc. 60 (9): 657–8. PMID 2507620.
- ↑ Goen TM, Terry JE (1986). "Mid-peripheral hemorrhages secondary to Waldenström's macroglobulinemia". J Am Optom Assoc. 57 (2): 109–12. PMID 3081619.
- ↑ Dimopoulos, Meletios A.; Panayiotidis, Panayiotis; Moulopoulos, Lia A.; Sfikakis, Petros; Dalakas, Marinos (2000). "Waldenström's Macroglobulinemia: Clinical Features, Complications, and Management". Journal of Clinical Oncology. 18 (1): 214–214. doi:10.1200/JCO.2000.18.1.214. ISSN 0732-183X.
- ↑ 10.0 10.1 Fadil A, Taylor DE (1998). "The lung and Waldenström's macroglobulinemia". South Med J. 91 (7): 681–5. PMID 9671845.
- ↑ Coimbra J, Costa AP, Pita F, Rosado P, de Almeida LB (1995). "[Neuropathy in Waldenstrom's macroglobulinemia]". Acta Med Port (in Portuguese). 8 (4): 253–7. PMID 7625222.