Lupus nephritis MRI
|
Lupus nephritis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Lupus nephritis MRI On the Web |
|
American Roentgen Ray Society Images of Lupus nephritis MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Omer Kamal, M.D. [2]
Overview
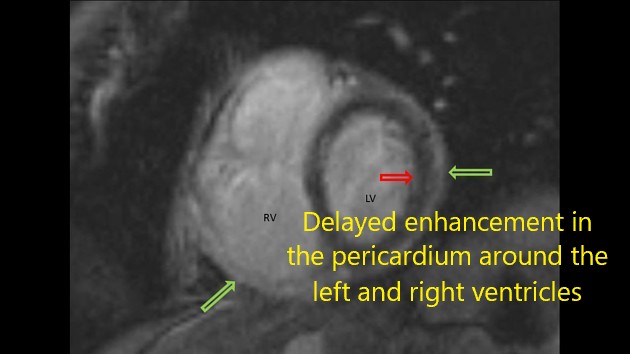
On abdominal MRI, systemic lupus erythematosus (SLE) may be characterized by hepatomegaly, pancreatic parenchymal enlargement, and hypervascularity of mesentery. On cardiac MRI, SLE may be characterized by mitral leaflet thickening, pericardial thickness, and pericardial effusions. On brain MRI, SLE may be characterized by white matter lesions, changes in blood circulation of the brain, and patchy areas of enhancement. On musculoskeletal MRI, SLE may be characterized by intramuscular edema, proliferative tenosynovitis, and bone marrow edema.
Key MRI findings in systemic lupus erythematosus
| Organ involvement | Disease | MRI | Preview |
|---|---|---|---|
| Gastrointestinal | Hepatitis |
|
  |
| Cholecystitis |
|
 | |
| Pancreatitis |
|
 | |
| Mesenteric vasculitis |
|
||
| Cardiac | Mitral stenosis |
|
|
| Pericarditis |
|
 | |
| Pericardial effusion |
|
||
| Myocarditis |
|
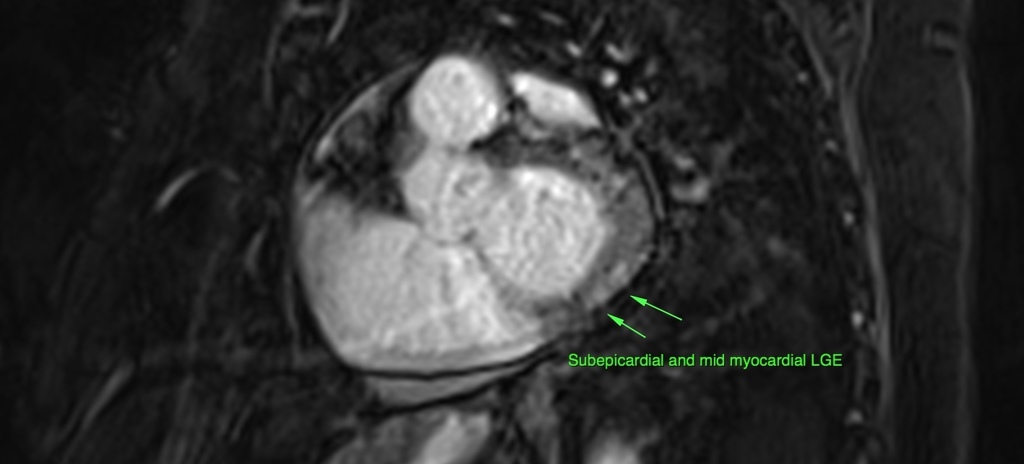 | |
| Neurological | Vasculitis |
|
 |
| Stroke |
 | ||
| Neuropathies |
|
  | |
| Autoimmune encephalitis |
|
 | |
| Musculoskeletal | Raynaud phenomen |
|
 |
| Myositis |
|
 | |
| Arthritis/tenosynovitis |
|
 | |
| Osteonecrosis (Avascular necrosis) |
|
  |