Esophagus: Difference between revisions
Kiran Singh (talk | contribs) No edit summary |
Kiran Singh (talk | contribs) No edit summary |
||
| Line 37: | Line 37: | ||
;Constrictions | ;Constrictions | ||
The esophagus has four points of constriction. When corrosive substances are ingested, or a solid object is swallowed, it is most likely to lodge and damage these four points. These constrictions are because of particular structures that compress on the esophagus. These constrictions are:<ref name=GRAYS2005 /> | The esophagus has four points of constriction. When corrosive substances are ingested, or a solid object is swallowed, it is most likely to lodge and damage these four points. These constrictions are because of particular structures that compress on the esophagus. These constrictions are:<ref name=GRAYS2005 /> | ||
* At the start of the esophagus, where the [[pharynx]] joins the esophagus, behind the [[cricoid cartilage]] | * At the start of the esophagus, where the [[pharynx]] joins the esophagus, behind the [[cricoid cartilage]] | ||
| Line 94: | Line 93: | ||
===Inflammation=== | ===Inflammation=== | ||
Inflammation of the esophagus is known as [[esophagitis]]. [[GERD|Reflux of gastric acids]] from the stomach, infection, substances ingested (for example, corrosives), some medications (such as [[bisphosphonate]]s), food allergies, and can all lead to esophagitis. {{As of|2014}} the cause of some forms of esophagitis, such as [[eosinophilic esophagitis]], is not known. Esophagitis can cause [[Odynophagia|painful swallowing]] and is usually treated by managing the cause of the esophagitis - such as managing reflux or treating infection.<ref name=DAVIDSONS2010>{{cite book|editor= Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston |others= illustrated by Robert Britton|title=Davidson's Principles and Practice of Medicine |year=2010|publisher=Churchill Livingstone/Elsevier|location=Edinburgh|isbn=978-0-7020-3084-0|edition=21st|pages=860–870}}</ref> | Inflammation of the esophagus is known as [[esophagitis]]. [[GERD|Reflux of gastric acids]] from the stomach, infection, substances ingested (for example, corrosives), some medications (such as [[bisphosphonate]]s), food allergies, and can all lead to esophagitis. {{As of|2014}} the cause of some forms of esophagitis, such as [[eosinophilic esophagitis]], is not known. Esophagitis can cause [[Odynophagia|painful swallowing]] and is usually treated by managing the cause of the esophagitis - such as managing reflux or treating infection.<ref name=DAVIDSONS2010>{{cite book|editor= Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston |others= illustrated by Robert Britton|title=Davidson's Principles and Practice of Medicine |year=2010|publisher=Churchill Livingstone/Elsevier|location=Edinburgh|isbn=978-0-7020-3084-0|edition=21st|pages=860–870}}</ref> | ||
===Cancer=== | ===Cancer=== | ||
[[Esophageal cancer|Cancer of the esophagus]] may occur in two forms. If the cancer occurs in the squamous cells lining the esophagus, it is called a [[carcinoma]]. Such a cancer is more common in [[China]] and [[Iran]]. If the cancer occurs in the glands or columnar tissue of the esophagus, then the cancer is an [[adenocarcinoma]]. This is most common in Western countries in those with Barrett's esophagus, and occurs in the cuboidal cells.<ref name=DAVIDSONS2010 /> | [[Esophageal cancer|Cancer of the esophagus]] may occur in two forms. If the cancer occurs in the squamous cells lining the esophagus, it is called a [[carcinoma]]. Such a cancer is more common in [[China]] and [[Iran]]. If the cancer occurs in the glands or columnar tissue of the esophagus, then the cancer is an [[adenocarcinoma]]. This is most common in Western countries in those with Barrett's esophagus, and occurs in the cuboidal cells.<ref name=DAVIDSONS2010 /> | ||
| Line 104: | Line 101: | ||
===Barrett's esophagus=== | ===Barrett's esophagus=== | ||
Prolonged esophagitis, particularly from gastric reflux, is one factor thought to play a role in the development of [[Barrett's esophagus]]. In this condition, there is [[metaplasia]] of the lining of the lower esophagus, which changes from [[stratified squamous epithelia]] to [[simple columnar epithelia]]. Barrett's esophagus is thought to be one of the main contributors to the development of esophageal cancer.<ref name=DAVIDSONS2010 /> | Prolonged esophagitis, particularly from gastric reflux, is one factor thought to play a role in the development of [[Barrett's esophagus]]. In this condition, there is [[metaplasia]] of the lining of the lower esophagus, which changes from [[stratified squamous epithelia]] to [[simple columnar epithelia]]. Barrett's esophagus is thought to be one of the main contributors to the development of esophageal cancer.<ref name=DAVIDSONS2010 /> | ||
===Varices=== | ===Varices=== | ||
[[Esophageal varices]] refer to engorged blood vessels present within the esophageal walls. These blood vessels are engorged more than normal, and in the worst cases may partially obstruct the esophagus. These blood vessels develop as part of a collateral circulation that occurs to drain blood from the [[abdomen]] as a result of [[portal hypertension]], usually as a result of [[liver disease]]s such as [[cirrhosis]].<ref name=DAVIDSONS2010>{{cite book|first=the editors Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston ; illustrated by Robert Britton|title=Davidson's Principles and Practice of Medicine |year=2010|publisher=Churchill Livingstone/Elsevier|location=Edinburgh|isbn=978-0-7020-3084-0|edition=21st|pages=941–942}}</ref> This collateral circulation occurs because the lower part of the esophagus drains into the left gastric vein, which is a branch of the portal vein. Because of the extensive venous plexus that exists between this vein and other veins, if portal hypertension occurs, the direction of blood drainage in this vein may reverse, with blood draining from the portal venous system, through the plexus. Veins in the plexus may engorge and lead to varices.<ref name=KUO2006/><ref name=PATTI1997/> | [[Esophageal varices]] refer to engorged blood vessels present within the esophageal walls. These blood vessels are engorged more than normal, and in the worst cases may partially obstruct the esophagus. These blood vessels develop as part of a collateral circulation that occurs to drain blood from the [[abdomen]] as a result of [[portal hypertension]], usually as a result of [[liver disease]]s such as [[cirrhosis]].<ref name=DAVIDSONS2010>{{cite book|first=the editors Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston ; illustrated by Robert Britton|title=Davidson's Principles and Practice of Medicine |year=2010|publisher=Churchill Livingstone/Elsevier|location=Edinburgh|isbn=978-0-7020-3084-0|edition=21st|pages=941–942}}</ref> This collateral circulation occurs because the lower part of the esophagus drains into the left gastric vein, which is a branch of the portal vein. Because of the extensive venous plexus that exists between this vein and other veins, if portal hypertension occurs, the direction of blood drainage in this vein may reverse, with blood draining from the portal venous system, through the plexus. Veins in the plexus may engorge and lead to varices.<ref name=KUO2006/><ref name=PATTI1997/> | ||
| Line 123: | Line 118: | ||
==Imaging== | ==Imaging== | ||
An [[X-ray]] of [[Barium swallow|swallowed barium]] may be used to reveal the size and shape of the esophagus, and the presence of any masses. The esophagus may also be [[medical imaging|imaged]] using a flexible camera inserted into the esophagus, in a procedure called an [[endoscopy]]. If an endoscopy is used on the stomach, the camera will also have to pass through the esophagus. During an endoscopy, a [[biopsy]] may be taken. If cancer of the esophagus is being investigated, other methods, including a [[CT scan]], may also be used.<ref name=DAVIDSONS2010 /> | An [[X-ray]] of [[Barium swallow|swallowed barium]] may be used to reveal the size and shape of the esophagus, and the presence of any masses. The esophagus may also be [[medical imaging|imaged]] using a flexible camera inserted into the esophagus, in a procedure called an [[endoscopy]]. If an endoscopy is used on the stomach, the camera will also have to pass through the esophagus. During an endoscopy, a [[biopsy]] may be taken. If cancer of the esophagus is being investigated, other methods, including a [[CT scan]], may also be used.<ref name=DAVIDSONS2010 /> | ||
Latest revision as of 19:57, 23 December 2015
|
WikiDoc Resources for Esophagus |
|
Articles |
|---|
|
Most recent articles on Esophagus |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Esophagus at Clinical Trials.gov Clinical Trials on Esophagus at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Esophagus
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Esophagus Discussion groups on Esophagus Directions to Hospitals Treating Esophagus Risk calculators and risk factors for Esophagus
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Esophagus |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
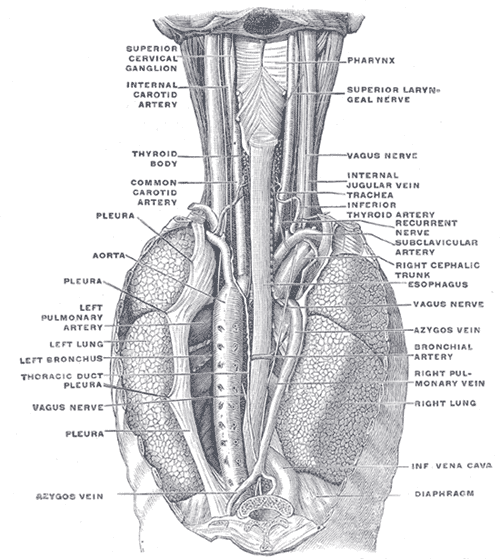
The esophagus (American English) or oesophagus (British English), commonly known as the foodpipe or gullet, is an organ in vertebrates which consists of a fibromuscular tube through which food passes, aided by peristaltic contractions, from the pharynx to the stomach. In humans, the esophagus is usually 18–25 centimeters (cm) long. During swallowing the epiglottis tilts backwards to prevent food from going down the larynx. The esophagus travels behind the trachea and heart, passes through the diaphragm and empties into the cardia of the stomach. The word esophagus derives from the Greek word oisophagos, which means "to carry to eat."[1]
The wall of the esophagus from the lumen outwards consists of mucosa, sub-mucosa (connective tissue), layers of muscle fibers between layers of fibrous tissue, and an outer layer of connective tissue. The mucosa is a stratified squamous epithelium (multiple layers of cells topped by a layer of flat cells) which contrasts to the single layer of columnar cells of the stomach. The transition between these two type of epithelium is visible as a zig-zag line. Most of the muscle is smooth muscle although striated muscle predominates in its upper two thirds. It has two muscular rings or sphincters in its wall, one at the top and one at the bottom. The lower sphincter helps to prevent reflux of acidic stomach content. The esophagus has a rich blood supply and vascular drainage. Its smooth muscle is innervated by involuntary nerves (sympathetic nerves via the sympathetic trunk and parasympathetic nerves via the vagus nerve) and in addition voluntary nerves (lower motor neurons) are carried in the vagus nerve to innervate its striated muscle.
The esophagus may be affected by gastric reflux, cancer, prominent dilated blood vessels called varices that can bleed heavily, tears, constrictions, and disorders of motility. Clinical investigations include X-rays using barium, endoscopy, and CT scans.
Structure
The esophagus is one of the upper parts of the digestive system. At the mouth opening, it is continuous with the back of the oral cavity, passing downwards through the rear part of the mediastinum, through the diaphragm, and into the stomach. In humans, the esophagus generally starts around the level of the sixth cervical vertebra (C6) behind the cricoid cartilage, enters the diaphragm at about the level of the tenth thoracic vertebra (T10), and ends at the cardia of the stomach, at the level of the eleventh thoracic vertebra (T11).[2] The esophagus is usually about 25 cm (10 in) in length.[3]
Many blood vessels serve the esophagus, with blood supply varying along its course. The cervical parts of the esophagus and the upper esophageal sphincter receive blood from inferior thyroid artery, the parts of the esophagus in the thorax from the bronchial arteries and branches directly from the thoracic aorta, and the lower parts of the esophagus and the lower esophageal sphincter (LES) receive blood from the left gastric artery and the left inferior phrenic artery.[4][5] The venous drainage also differs along the course of the esophagus. The upper and lower parts of the esophagus drain into the azygos and hemiazygos veins, and blood from the middle part drains into the left gastric vein. All these veins drain into the superior vena cava, with the exception of the left gastric vein, which is a branch of the portal vein.[4] Lymphatically, the upper third of the esophagus drains into the deep cervical lymph nodes, the middle into the superior and posterior mediastinal lymph nodes, and the lower esophagus into the gastric and celiac lymph nodes.[4]
The esophagus is innervated by the vagus nerve and the cervical and thoracic sympathetic trunk.[4] The vagus nerve has a parasympathetic function, supplying the muscles of the esophagus and stimulating glandular contraction. Two sets of nerve fibres travel in the vagus nerve to supply the muscles. The upper striated muscle, and upper esophageal sphincter, are supplied by neurons with bodies in the nucleus ambiguus, whereas fibres that supply the smooth muscle and lower esophageal sphincter have bodies situated in the dorsal motor nucleus.[4] The vagus nerve plays the primary role in initiating peristalsis.[6] The sympathetic trunk has a sympathetic function. It may enhance the function of the vagus nerve, increasing peristalsis and glandular activity, and causing sphincter contraction. In addition, sympathetic activation may relax the muscle wall and cause blood vessel constriction.[4] Sensation along the esophagus is supplied by both nerves, with gross sensation being passed in the vagus nerve and pain passed up the sympathetic trunk.[2]
- Position
The upper esophagus lies at the back of the mediastinum behind the trachea, and in front of the erector spinae muscles and the vertebral column. The lower esophagus lies behind the heart and curves in front of thoracic aorta. From the bifurcation of the trachea downwards, the esophagus passes behind the right pulmonary artery, left main bronchus, and left atrium. At this point it passes through the diaphragm.[2]
The thoracic duct, which drains the majority of the body's lymph, passes behind the esophagus, curving from lying behind the esophagus on the right in the lower part of the esophagus, to lying behind the esophagus on the left in the upper esophagus. The esophagus also lies in front of parts of the hemiazygos veins and the intercostal veins on the right side. The vagus nerve divides and covers the esophagus in a plexus.[2]
- Constrictions
The esophagus has four points of constriction. When corrosive substances are ingested, or a solid object is swallowed, it is most likely to lodge and damage these four points. These constrictions are because of particular structures that compress on the esophagus. These constrictions are:[2]
- At the start of the esophagus, where the pharynx joins the esophagus, behind the cricoid cartilage
- Where it is crossed on the front by the aortic arch and the left main bronchus
- Where it passes through the diaphragm
Sphincters
The esophagus is surrounded at the top and bottom by two muscular rings, known respectively as the upper esophageal sphincter and the lower esophageal sphincter.[2] These sphincters act to close the esophagus when food is not being swallowed. The esophageal sphincters are functional, but not anatomical sphincters, meaning that they are sections of the esophageal wall that act as a sphincter, but do not have distinct thickenings like other sphincters.[7]
The upper esophageal sphincter surrounds the upper part of the esophagus. It consists of skeletal muscle, but is not under conscious control. Opening of the upper esophageal sphincter is triggered by the swallow reflex. The primary muscle of the upper esophageal sphincter is the cricopharyngeus portion of the inferior pharyngeal constrictor.[8]
The lower esophageal sphincter surrounds the lower part of the esophagus. This sphincter surrounds the junction between the esophagus and the stomach.[7]
Gastro-esophageal junction
The gastro-esophageal junction (also known at the esophagogastic junction) is the junction between the esophagus and the stomach, and it is situated at the lower end of the esophagus.[9] The pink color of the esophageal mucosa contrasts to the a deeper red of the gastric mucosa,[4][10] and the mucosal transition can be seen as an irregular zig-zag line, which is often called the z-line.[11] Similarly, by direct vision of fresh specimens, grey-pink of the esophageal mucosa contrasts with the darker gastric mucosa,[12] but in embalmed cadavers a color contrast may not be apparent.[13] Histological examination reveals abrupt transition between the nonkeratinized stratified squamous epithelium of the esophagus and the simple columnar epithelium of the stomach.[13] Normally, the cardia of the stomach is immediately distal to the z-line[14] and the z-line coincides with the upper limit of the gastric folds of the cardia; however, when the anatomy of the mucosa is distorted in Barrets esophagus the true gastro-eshophageal junction can be identified by the upper limit of the gastric folds rather than the mucosal transition.[15] The functional location of LES is generally situated about 3 cm distal to the z-line.[4]
Histology
The human esophagus has a mucosa consisting of a tough stratified squamous epithelium without keratin, a smooth lamina propria, and a muscularis mucosa.[4] The epithelium of the esophagus has a relatively rapid turnover, and serves a protective function against the abrasive effects of food. In many animals the epithelium contains a layer of keratin, representing a coarser diet.[16] Protection is conferred by the secretion of mucus from glands.[17] There are two types of glands, with mucus-secreting esophageal glands being found in the submucosa, and esophageal cardiac glands, similar to cardiac glands of the stomach, located in the lamina propria and most frequent in the terminal part of the organ.[16][18] The submucosa also contains the submucosal plexus, a network of nerve cells part of the enteric nervous system.[16]
The muscularis propria of the esophagus has two types of muscle. The upper third of the esophagus contains striated muscle and the lower third contain smooth muscle, with the middle third containing a mixture of both.[4] Muscle is arranged in two layers: one in which the muscle fibres run longitudinal to the esophagus, and the other in which the fibres encircle the esophagus. These are separated by the myenteric plexus, a tangled interpolation of nerve fibres involved in the secretion of mucus and peristalsis of the smooth muscle of the esophagus. The esophagus also has an adventitia, but not a serosa. This makes it distinct from many other structures in the gastrointestinal tract.[4]
Development
The esophagus develops from the embryonic gut tube, an endodermal structure. Early in development, the human embryo has three layers and abuts an embryonic yolk sac. During the second week of embryological development, as the embryo grows, it begins to surround and envelop portions of this sac. The enveloped portions form the basis for the adult gastrointestinal tract. Sections of this gut begin to differentiate into the organs of the gastrointestinal tract, such as the esophagus, stomach, and intestines.[19]
The sac is surrounded by a network of arteries called the vitelline plexus. Over time, these arteries consolitate into three main arteries that supply the developing gastrointestinal tract: the celiac artery, superior mesenteric artery, and inferior mesenteric artery. The areas supplied by these arteries are used to define the midgut, hindgut and foregut.[19]
The esophagus develops as part of the foregut tube.[19] The innervation of the esophagus develops from the branchial arches.[2]
Function
Swallowing
In humans and other animals, food is ingested through the mouth. During swallowing, food passes from the mouth through the pharynx into the esophagus. The esophagus is thus one of the first components of the human digestive system and the human gastrointestinal tract. After food passes through the esophagus, it enters the stomach.[7]
When food is being swallowed, the epiglottis moves backward to cover the larynx, preventing food from entering the trachea. At the same time, the upper esophageal sphincter relaxes, allowing a bolus of food to enter. Rhythmic contraction of the esophageal muscle called peristalsis pushes the food down the esophagus. These rhythmic contractions occur both as a reflex response to food that is in the mouth, and also as a response to the sensation of food within the esophagus itself. Along with the peristalsis, the lower esophageal sphincter relaxes.[7]
Reducing gastric reflux
The stomach generates strong acids, including hydrochloric acid (HCl), and enzymes to aid in food digestion. This digestive mixture is called gastric juice. Constriction of the upper and lower esophageal sphincters help to prevent reflux of gastric contents and juices into the esophagus, protecting the esophageal mucosa. In addition, the acute angle of His and the lower crura of the diaphragm helps this sphincteric action.[7][20]
Clinical significance
The main conditions affecting the esophagus are described here. For a more complete list, see esophageal disease.
Inflammation
Inflammation of the esophagus is known as esophagitis. Reflux of gastric acids from the stomach, infection, substances ingested (for example, corrosives), some medications (such as bisphosphonates), food allergies, and can all lead to esophagitis. As of 2014[update] the cause of some forms of esophagitis, such as eosinophilic esophagitis, is not known. Esophagitis can cause painful swallowing and is usually treated by managing the cause of the esophagitis - such as managing reflux or treating infection.[3]
Cancer
Cancer of the esophagus may occur in two forms. If the cancer occurs in the squamous cells lining the esophagus, it is called a carcinoma. Such a cancer is more common in China and Iran. If the cancer occurs in the glands or columnar tissue of the esophagus, then the cancer is an adenocarcinoma. This is most common in Western countries in those with Barrett's esophagus, and occurs in the cuboidal cells.[3]
In its early stages, esophageal cancer may not have any symptoms at all. When severe, esophageal cancer may eventually cause obstruction of the esophagus, making swallowing of any solid foods very difficult and causing weight loss. The progress of the cancer is staged using a system that measures how far into the esophageal wall the cancer has invaded, how many lymph nodes possess the cancer, and whether there are any metastases in different parts of the body. Esophageal cancer is often managed with radiotherapy, chemotherapy, and may also be managed by partial surgical removal of the esophagus. Inserting a stent into the esophagus, or inserting a nasogastric tube, may also be used to ensure that a person is able to digest enough food and water. As of 2014[update], the prognosis for esophageal cancer is still poor, so palliative therapy may also be a focus of treatment.[3]
Barrett's esophagus
Prolonged esophagitis, particularly from gastric reflux, is one factor thought to play a role in the development of Barrett's esophagus. In this condition, there is metaplasia of the lining of the lower esophagus, which changes from stratified squamous epithelia to simple columnar epithelia. Barrett's esophagus is thought to be one of the main contributors to the development of esophageal cancer.[3]
Varices
Esophageal varices refer to engorged blood vessels present within the esophageal walls. These blood vessels are engorged more than normal, and in the worst cases may partially obstruct the esophagus. These blood vessels develop as part of a collateral circulation that occurs to drain blood from the abdomen as a result of portal hypertension, usually as a result of liver diseases such as cirrhosis.[3] This collateral circulation occurs because the lower part of the esophagus drains into the left gastric vein, which is a branch of the portal vein. Because of the extensive venous plexus that exists between this vein and other veins, if portal hypertension occurs, the direction of blood drainage in this vein may reverse, with blood draining from the portal venous system, through the plexus. Veins in the plexus may engorge and lead to varices.[4][5]
Esophageal varices often do not have symptoms until they rupture. A ruptured varix is considered a medical emergency, because varices can bleed a lot. A bleeding varix may cause a person to throw up blood, or may cause symptoms of hypovolemic shock. To deal with a ruptured varix, a band may be placed around the bleeding bood vessel, or a small amount of a clotting agent may be injected near the bleed. A surgeon may also try to use a small inflatable balloon to apply pressure to stop the wound. A person with a bleeding varice may also receive IV fluids in order to prevent hypovolemic shock from excess blood loss.[3]
Motility disorders
Several disorders affect the motility of food as it travels down the esophagus. This can cause difficult swallowing, called dysphagia. Achalasia refers to a failure of the lower esophageal sphincter to relax properly, and generally develops later in life. This leads to progressive enlargement of the esophagus, and possibly eventual megaesophagus. A nutcracker esophagus refers to swallowing that can be extremely painful, and diffuse esophageal spasm refers to spasm of the esophagus that can be one cause of chest pain. Sclerosis of the esophagus, such as with systemic sclerosis or in CREST syndrome may cause hardening of the walls of the esophagus and interfere with peristalsis.[3]
Malformations
Various structures may also constrict the esophagus. These esophageal strictures are usually benign and typically develop after a person has had reflux for many years. Other malformations may include esophageal webs (which can also be congenital) and damage to the esophagus by radiotherapy, corrosive ingestion, or eosinophilic esophagitis. A Schatzki ring is fibrosis at the gastro-esophageal junction. Strictures may also develop in chronic anemia, and Plummer-Vinson syndrome.[3]
Congenital malformation
The esophagus fails to develop or there is an abnormal connection between the trachea and esophagus in about 1 in 3500 births. Conventional classification divides such connections into five types, based on whether the esophagus is a continuous tube or not, and which end of the esophagus (proximal, distal, both or neither) connects to the trachea. About half the time, these abnormalities occurs with additional abnormalities in other parts of the body, especially affecting the heart.[21]
Imaging
An X-ray of swallowed barium may be used to reveal the size and shape of the esophagus, and the presence of any masses. The esophagus may also be imaged using a flexible camera inserted into the esophagus, in a procedure called an endoscopy. If an endoscopy is used on the stomach, the camera will also have to pass through the esophagus. During an endoscopy, a biopsy may be taken. If cancer of the esophagus is being investigated, other methods, including a CT scan, may also be used.[3]
History
The word esophagus (British English: oesophagus) comes from Template:Lang-el (oisophagos), from "to carry" (oesin) and "to eat" (phagos).[1] The Greek term oesophagus, from which the English term has been derived, has been documented in anatomical literature since at least the time of Hippocrates, who noted that "the oesophagus ... receives the greatest amount of what we consume." [22] Its existence in other animals and its relationship with the stomach was documented by the Ancient Roman (philosopher) and physician Pliny the Elder,[23] and the peristaltic contractions of the esophagus have been documented since at least the time of Galen.[24]
The first attempt at surgery on the esophagus focused in the neck, and was firstly conducted in dogs by Theodore Billroth in 1871, and then in people by Czerny in 1877. By 1908, an operation had been performed by Voeckler to remove the esophagus, and in 1933 the first surgical removal of parts of the lower esophagus, (to control esophageal cancer), had been conducted.[25]
The Nissen fundoplication, in which the stomach is wrapped around the lower esophageal sphincter in order to stimulate its function and control reflux, was first conducted by Rudolph Nissen in 1955.[25]
Other animals
Vertebrates
In tetrapods, the pharynx is much shorter, and the esophagus correspondingly longer, than in fish. In the majority of vertebrates, the esophagus is simply a connecting tube, but in some birds, which regurgitate components to feed their young, it is extended towards the lower end to form a crop for storing food before it enters the true stomach.[26][27] In ruminants, animals with four stomachs, a groove called the sulcus reticuli is often found in the esophagus, allowing milk to drain directly into the hind stomach, the abomasum.[28] The esophagus of snakes is remarkable for the distension it undergoes when swallowing prey.[29]
In most fish, the esophagus is extremely short, primarily due to the length of the pharynx (which is associated with the gills). However, some fish, including lampreys, chimaeras, and lungfish, have no true stomach, so that the esophagus effectively runs from the pharynx directly to the intestine, and is therefore somewhat longer.[26]
In many vertebrates, the esophagus is lined by stratified squamous epithelia without glands. In fish, the esophagus is often lined with columnar epithelia,[27] and in amphibians, sharks and rays, the esophageal epithelium is ciliated, helping to wash food along, in addition to the action of muscular peristalsis.[26] In addition, in the bat Plecotus auritus, fish and some amphibians, glands secreting pepsinogen or hydrochloric acid have been found.[27]
The muscle of the esophagus in many mammals is striated initially, but then becomes smooth muscle in the caudal third or so. In the canine and ruminants, however, it is entirely striated to allow regurgitation to feed young (canines) or regurgitation to chew cud (ruminants). It is entirely smooth muscle in amphibians, reptiles and birds.[27]
Contrary to popular belief,[30] a person would not be able to pass through the esophagus of a whale, which generally measure less than 10 cm in diameter, although in larger baleen whales may be up to ten inches when fully distended.[31]
Invertebrates
A structure with the same name is often found in invertebrates, including molluscs and arthropods, connecting the oral cavity with the stomach.[32] In the cephalopods, the brain often surrounds the esophagus.[33]
The mouth of gastropods opens into an esophagus, which connects to the stomach. Because of torsion, the esophagus usually passes around the stomach, and opens into its posterior portion, furthest from the mouth. In species that have undergone de-torsion, however, the esophagus may open into the anterior of the stomach, which is therefore reversed from the usual gastropod arrangement.[34]
In Tarebia granifera the brood pouch is above the esophagus.[35]
There is available an extensive rostrum on the anterior part of the esophagus in all carnivorous gastropods.[36]
See also
References
- ↑ 1.0 1.1 Harper, Douglas. "Esophagus". Etymology Online. Retrieved 19 March 2014.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Drake, Richard L.; Vogl, Wayne; Tibbitts, Adam W.M. Mitchell ; illustrations by Richard; Richardson, Paul (2005). Gray's anatomy for students. Philadelphia: Elsevier/Churchill Livingstone. pp. 192–194. ISBN 978-0-8089-2306-0.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Colledge, Nicki R.; Walker, Brian R.; Ralston, Stuart H., eds. (2010). Davidson's Principles and Practice of Medicine. illust. Robert Britton (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. p. 838. ISBN 978-0-7020-3084-0.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 Kuo, Braden; Urma, Daniela (2006). "Esophagus - anatomy and development". GI Motility online. doi:10.1038/gimo6. Unknown parameter
|doi_brokendate=ignored (help) - ↑ 5.0 5.1 Patti, MG; Gantert, W; Way, LW (Oct 1997). "Surgery of the esophagus. Anatomy and physiology". The Surgical clinics of North America. 77 (5): 959–70. doi:10.1016/s0039-6109(05)70600-9. PMID 9347826.
- ↑ Patterson, William G. (2006). "Esophageal peristalsis". GI Motility online. doi:10.1038/gimo13. Retrieved 24 May 2014. Unknown parameter
|doi_brokendate=ignored (help) - ↑ 7.0 7.1 7.2 7.3 7.4 Hall, Arthur C. Guyton, John E. (2005). Textbook of medical physiology (11th ed.). Philadelphia: W.B. Saunders. pp. 782–784. ISBN 978-0-7216-0240-0.
- ↑ Mu L, Wang J, Su H, Sanders I; Wang; Su; Sanders (March 2007). "Adult human upper esophageal sphincter contains specialized muscle fibers expressing unusual myosin heavy chain isoforms". J. Histochem. Cytochem. 55 (3): 199–207. doi:10.1369/jhc.6A7084.2006. PMID 17074861. Unknown parameter
|doi_brokendate=ignored (help) - ↑ John H. Dirckx (editor) (1997). Stedman's Concise Medical and Allied Health Dictionary (3rd ed.). Williams and Wilkins. p. 463. ISBN 0-683-23125-1.
- ↑ Anthony DiMarino, Jr., Stanley B. Benjamin ; section editors, Firas H. Al-Kawas, ed. (2002). Gastrointestinal disease : an endoscopic approach (2nd ed.). Thorofare, NJ: Slack. p. 166. ISBN 978-1-55642-511-0.
- ↑ Levine, editors, Richard M. Gore, Marc S. (2010). High-yield imaging (1st ed.). Philadelphia, Pa.: Saunders/Elsevier. p. 151. ISBN 1455711446.
- ↑ Gray, Henry (1942). Johnston, T.B; Whillis, J, eds. Gray's Anatomy: Descriptive and Applied (28th ed.). Longmans, Green and Co. p. 1318.
- ↑ 13.0 13.1 Moore, Keith L; Agur, Anne M.R (2002). Essential Clinical Anatomy (2nd ed.). Lippincott Williams & Wilkins. p. 145. ISBN 0-7817-2830-4.
- ↑ Barrett, Kim E. (2014). Gastrointestinal physiology (2nd ed.). New York: Mc Graw Hill. pp. Chapter 7: "Esophageal Motility". ISBN 978-0-07-177401-7.
- ↑ Long, Richard G; Scott, Brian B, eds. (2005). Specialist Training in Gastroenterology and Liver Disease. Elsevier Mosby. pp. 25–26. ISBN 0-7234-3252-X.
- ↑ 16.0 16.1 16.2 Ross M, Pawlina W (2011). Histology: A Text and Atlas (6th ed.). Lippincott Williams & Wilkins. pp. 571–573. ISBN 978-0-7817-7200-6.
- ↑ Young, Barbara, ed. (2006). Wheater's functional histology: a text and colour atlas (5th ed.). Churchill Livingstone/Elsevier. p. 86. ISBN 978-0-443-068-508.
- ↑ Takubo, Kaiyo (2007). Pathology of the esophagus an atlas and textbook (2nd ed.). Tokyo: Springer Verlag. p. 28. ISBN 9784431686163.
- ↑ 19.0 19.1 19.2 Gary C. Schoenwolf (2009). "Development of the Gastrointestinal Tract". Larsen's human embryology (4th ed.). Philadelphia: Churchill Livingstone/Elsevier. ISBN 978-0-443-06811-9.
- ↑ "Neuromuscular Anatomy of Esophagus and Lower Esophageal Sphincter - Motor Function of the Pharynx, Esophagus, and its Sphincters - NCBI Bookshelf". Ncbi.nlm.nih.gov. 2013-03-25. Retrieved 2013-04-24.
- ↑ Shaw-Smith, C (18 November 2005). "esophageal atresia, tracheo-esophageal fistula, and the VACTERL association: review of genetics and epidemiology". Journal of Medical Genetics. 43 (7): 545–54. doi:10.1136/jmg.2005.038158. PMC 2564549. PMID 16299066.
- ↑ Potter, translated by Paul, Hippocrates ;edited (2010). Coan prenotions (1. publ. ed.). Cambridge, Mass.: Harvard University Press. p. 59. ISBN 0-674-99640-2.
- ↑ Bostock, John; Riley, Henry T.; Pliny the Elder (1855). The natural history of Pliny. London: H. G. Bohn. p. 64.
- ↑ Brock, Galen ; with an English translation by Arthur John (1916). On the natural faculties (Repr. ed.). London: W. Heinemann. p. "Book 3" S8. ISBN 978-0-674-99078-4.
- ↑ 25.0 25.1 Norton, Jeffrey A., ed. (2008). Surgery : basic science and clinical evidence (2nd ed.). New York, NY: Springer. pp. 744–746. ISBN 978-0-387-30800-5.
- ↑ 26.0 26.1 26.2 Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia, PA: Holt-Saunders International. pp. 344–345. ISBN 0-03-910284-X.
- ↑ 27.0 27.1 27.2 27.3 Hume, C. Edward Stevens, Ian D. (2005). Comparative physiology of the vertebrate digestive system (1st pbk. ed.). Cambridge: Cambridge University Press. p. 15. ISBN 978-0-521-61714-7.
- ↑ Mackie, R. I. (1 April 2002). "Mutualistic Fermentative Digestion in the Gastrointestinal Tract: Diversity and Evolution". Integrative and Comparative Biology. 42 (2): 319–326. doi:10.1093/icb/42.2.319. PMID 21708724.
- ↑ Cundall D, Tuttman C, Close M.; Tuttman; Close (Mar 2014). "A model of the anterior esophagus in snakes, with functional and developmental implications". Anat Rec. 297 (3): 586–98. doi:10.1002/ar.22860.
- ↑ Eveleth, Rose (20 February 2013). "Could a Whale Accidentally Swallow You? It Is Possible". Smithsonian. Retrieved 12 April 2014.
- ↑ Tinker, Spencer Wilkie (1988). Whales of the world. Leiden: E.J. Brill. p. 60. ISBN 978-0-935848-47-2.
- ↑ Hartenstein, Volker (September 1997). "Development of the insect stomatogastric nervous system". Trends in Neurosciences. 20 (9): 421–427. doi:10.1016/S0166-2236(97)01066-7. PMID 9292972.
- ↑ Kutsch, with a coda written by T.H. Bullock ; edited by O. Breidbach, W. (1994). The nervous systems of invertebrates : an evolutionary and comparative approach. Basel: Birkhäuser. p. 117. ISBN 978-3-7643-5076-5.
- ↑ Barnes, Robert D. (1982). Invertebrate Zoology. Philadelphia, PA: Holt-Saunders International. ISBN 0-03-056747-5.
- ↑ Appleton C. C., Forbes A. T.& Demetriades N. T. (2009). "The occurrence, bionomics and potential impacts of the invasive freshwater snail Tarebia granifera (Lamarck, 1822) (Gastropoda: Thiaridae) in South Africa". Zoologische Mededelingen 83. http://www.zoologischemededelingen.nl/83/nr03/a04
- ↑ Gerlach, J.; Van Bruggen, A.C. (1998). "A first record of a terrestrial mollusc without a radula". Journal of Molluscan Studies. 64 (2): 249. doi:10.1093/mollus/64.2.249..
| Wikimedia Commons has media related to Esophagus. |
| File:Wiktionary-logo-en-v2.svg | Look up esophagus in Wiktionary, the free dictionary. |
Template:Digestive tract Template:Human systems and organs
Lua error in Module:Authority_control at line 788: attempt to index field 'wikibase' (a nil value).
- Pages with reference errors
- CS1 maint: Multiple names: authors list
- Pages with citations using unsupported parameters
- CS1 maint: Extra text: authors list
- CS1 maint: Multiple names: editors list
- Pages with script errors
- Pages with broken file links
- Articles containing potentially dated statements from 2014
- Articles with invalid date parameter in template
- All articles containing potentially dated statements
- Digestive system
- Thorax (human anatomy)
- Organs (anatomy)
- Human head and neck
- Abdomen