Cervical vertebrae
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
In vertebrates, cervical vertebrae (singular: vertebra) are those vertebrae immediately behind (caudal to) the skull.
Variation among species
In some species, some parts of the skull may be composed of vertebra-like elements, e.g. the occipital bone in humans is composed of four vertebra-like segments.
In many vertebrate species, cervical vertebrae are variable in number; however, almost all mammals have seven (including those with very short necks, such as elephants or whales, and those with very long necks, such as giraffes).
The few exceptions include the manatee and the two-toed sloth, which each have only six cervical vertebrae, and the three-toed sloth with nine cervical vertebrae.
Thoracic vertebrae in all species are defined as those vertebrae which also carry a pair of ribs, and lie caudal to the cervical vertebrae.
In humans, cervical vertebrae are the smallest of the true vertebrae, and can be readily distinguished from those of the thoracic or lumbar regions by the presence of a foramen (hole) in each transverse process, through which passes the vertebral artery.
The remainder of this article focuses upon human anatomy.
General characteristics (C3-C6)
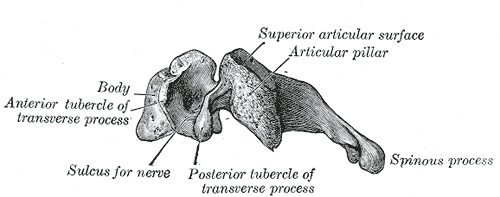
These are the general characteristics of the third through sixth cervical vertebrae. (The first, second, and seventh vertebrae are extraordinary, and detailed later.)
The body of these four vertebrae is small, and broader from side to side than from front to back.
The anterior and posterior surfaces are flattened and of equal depth; the former is placed on a lower level than the latter, and its inferior border is prolonged downward, so as to overlap the upper and forepart of the vertebra below.
The upper surface is concave transversely, and presents a projecting lip on either side; the lower surface is concave from front to back, convex from side to side, and presents laterally shallow concavities which receive the corresponding projecting lips of the underlying vertebra.
The pedicles are directed laterally and backward, and are attached to the body midway between its upper and lower borders, so that the superior vertebral notch is as deep as the inferior, but it is, at the same time, narrower.
The laminae are narrow, and thinner above than below; the vertebral foramen is large, and of a triangular form.
The spinous process is short and bifid, the two divisions being often of unequal size.
The superior and inferior articular processes of neighboring vertebrae often fuse on either or both sides to form an articular pillar, a column of bone which projects laterally from the junction of the pedicle and lamina.
The articular facets are flat and of an oval form:
- the superior face backward, upward, and slightly medially.
- the inferior face forward, downward, and slightly laterally.
The transverse processes are each pierced by the foramen transversarium, which, in the upper six vertebrae, gives passage to the vertebral artery and vein, as well as a plexus of sympathetic nerves.
Each process consists of an anterior and a posterior part.
The anterior portion is the homologue of the rib in the thoracic region, and is therefore named the costal process or costal element.
It arises from the side of the body, is directed laterally in front of the foramen, and ends in a tubercle, the anterior tubercle.
The posterior part, the true transverse process, springs from the vertebral arch behind the foramen, and is directed forward and laterally; it ends in a flattened vertical tubercle, the posterior tubercle.
These two parts are joined, outside the foramen, by a bar of bone which exhibits a deep sulcus on its upper surface for the passage of the corresponding spinal nerve.
Special cervical vertebrae (C1, C2, and C7)
- C1 or atlas: The Atlas is the topmost vertebra, and – along with C2 – forms the joint connecting the skull and spine. Its chief peculiarity is that it has no body, and this is due to the fact that the body of the atlas has fused with that of the next vertebra.
- C2 or axis: It forms the pivot upon which C1 rotates. The most distinctive characteristic of this bone is the strong odontoid process (dens) which rises perpendicularly from the upper surface of the body. The body is deeper in front than behind, and prolonged downward anteriorly so as to overlap the upper and front part of the third vertebra.
- C7 or vertebra prominens: The most distinctive characteristic of this vertebra is the existence of a long and prominent spinous process, hence the name vertebra prominens. In some subjects, the seventh cervical vertebra is associated with an abnormal pair of ribs, known as cervical ribs. These ribs are usually small, but may occasionally compress blood vessels (such as the subclavian artery) or nerves in the brachial plexus, causing unpleasant symptoms.
Movements of the cervical spine
The movements of flexion and extension of the head take place predominantly at the joint between the first cervical vertebra and the occipital bone, the atlanto-occipital joint. However, the cervical spine is comparatively mobile, and some component of this movement is due to flexion and extension of the vertebral column itself.
The movement of rotating the head to left and right happens almost entirely at the joint between the first and second cervical vertebrae, the atlanto-axial joint. A small amount of rotation of the vertebral column itself contributes to the movement.
Landmarks
The thyroid cartilage is from C4 to C5.[1]
The cricoid cartilage is from C6 to C7.[1]
Clinical significance
Injuries to the cervical spine are common at the level of the second cervical vertebrae, but neurological injury is uncommon.
If it does occur, however, it may cause death or profound disability, including paralysis of the arms, legs, and diaphragm, which leads to respiratory failure.
Common patterns of injury include the odontoid fracture and the hangman's fracture, both of which are often treated with immobilization in a cervical collar or Halo brace.
Additional images
-
Cervical column
-
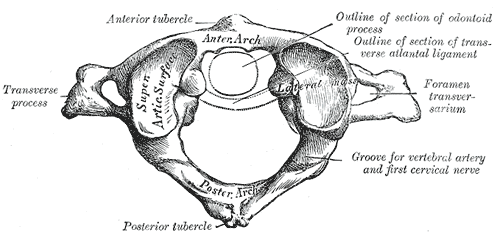
First cervical vertebra, or Atlas
-
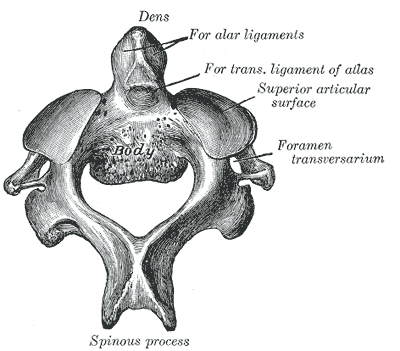
Second cervical vertebra, or epistropheus, from above.
-
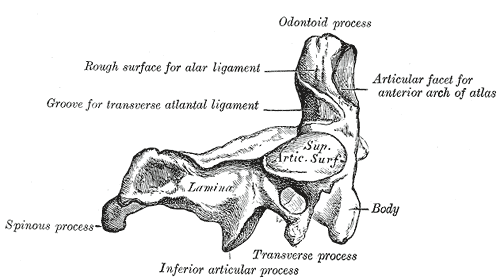
Second cervical vertebra, epistropheus, or axis, from the side.
-
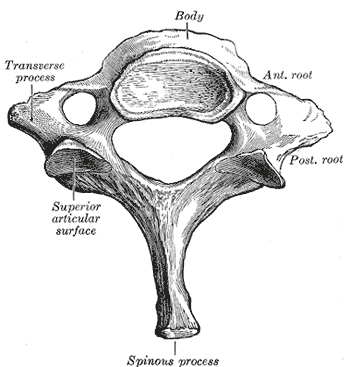
Seventh cervical vertebra.
-
Vertebral column.
-
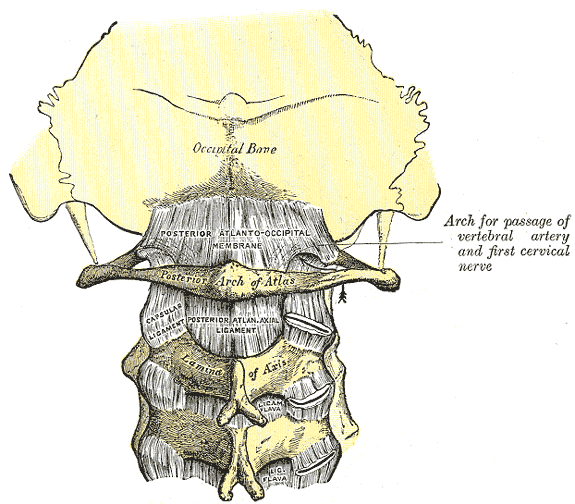
Posterior atlantoöccipital membrane and atlantoaxial ligament.
-
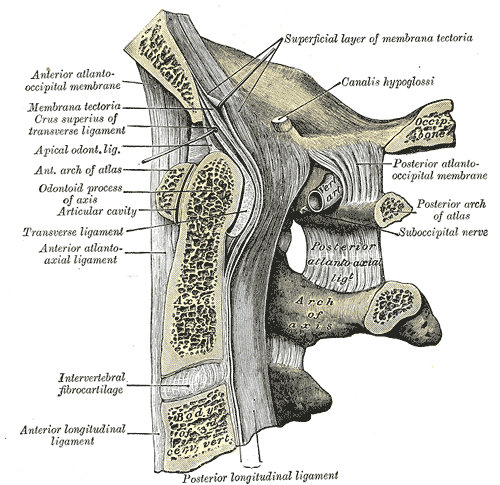
Median sagittal section through the occipital bone and first three cervical vertebræ.
-
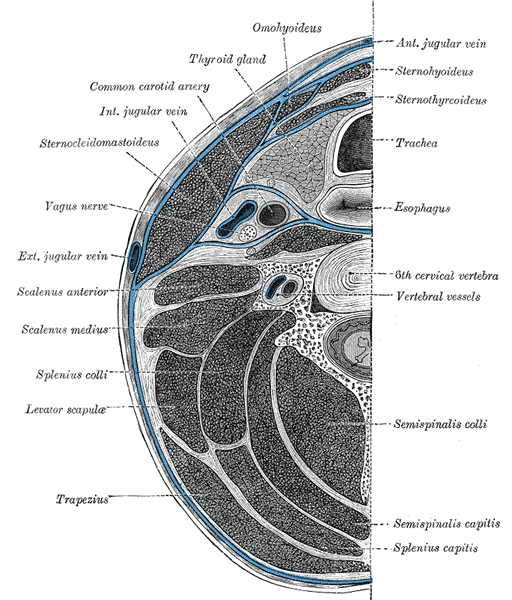
Section of the neck at about the level of the sixth cervical vertebra.
Cervical Degenerative Disc Disease
In between the cervical vertebrae are intervertebral discs. These discs are made of a flexible material that act as shock absorbers. In all humans, these discs naturally shrink over time. They can also shrink due to being damaged, either by trauma or overuse. The speed at which they degenerate can also be genetic. In any case, when a disc shrinks, at a minimum it causes the vertebra in the neck to become unstable. The body recognizes this physiological change and tries to compensate by growing new bone in and around the affected vertebrae. This bone growth is called bone spurs. This can cause irritation and inflammation which results in arthritis. In the worst case, the disc not only shrinks but can bulge or split open. If this happens the protrusion can press on the adjacent nerves and cause pain and symptoms like tingling, numbing, and weakness in one or both arms. A person may have all or none of these symptoms regardless of the severity of disc degeneration. Treatment of this condition is done in many ways. The first method is conservative and involves the patient resting, performing neck stretching exercises, traction, and taking non steroidal anti-inflammatory medication. This is usually enough for most cases. In cases that do not respond to conservative treatment, other methods are considered. The gold standard at this time is disc fusion. Fusion involves removal of the diseased disc, then prepping the space where the disc was. A piece of bone is then inserted to fill the space where the disc was and two metal stabilizers are screwed to the vertebrae above and below the disc cavity. The body then grafts to the new bone creating a solid connection between the two vertebra. This returns the area of the neck to stability and stops the bone spurs from growing. It also relieves and pressure on the adjacent nerves due to the spurs and the bulging disc. This usually causes the inflammation to go down and the arthritis to subside. However, this technique has a negative side effect. Because the upper and lower vertebra are now solidly connected, the shock of the neck movement in that area is projected onto the adjacent discs. This can cause the adjacent discs to degenerate a quicker rate then they would normally. Depending on how quickly this occurs the patient could have problems in the adjacent discs. A relatively new treatment method has recently been introduced called cervical disc replacement. This involves removing the diseased disc and replacing it with an artificial one. The replacement is meant to restore flexibility and movement to the area. Because of this the adjacent discs are not adversely loaded with extra shock caused by normal neck movement. This type of treatment looks promising, however there is much to overcome to do it successfully. It is absolutely necessary that the artificial disc not move at all when it is implanted. The disc must not touch any of the adjacent nerves and especially the spinal cord.
Soft Tissue Damage and Instability Conditions of the Upper Cervical Joints
Cranio-atlanto-axial instability can be caused by torn or overstretched alar ligaments and/or of the ligamentum transversum - often in combination with injured (ruptured) facet joints of the upper cervical vertebrae. Such injuries are often caused by severe whiplash movement.
References
External links
- Cervical spine in special context to the head neck joint function
- Symptoms caused by head neck joint instabilities
- Head neck joint instability causality and intervention strategies
- Diagram at kenyon.edu
- Cervical Spine Anatomy
- Degenerative Cervical Spine Disorders
Template:Gray's Template:Spine