Dressler's syndrome: Difference between revisions
| Line 132: | Line 132: | ||
* Variations in the amplitude or directionality of QRS from beat to beat and/or a low voltage QRS. | * Variations in the amplitude or directionality of QRS from beat to beat and/or a low voltage QRS. | ||
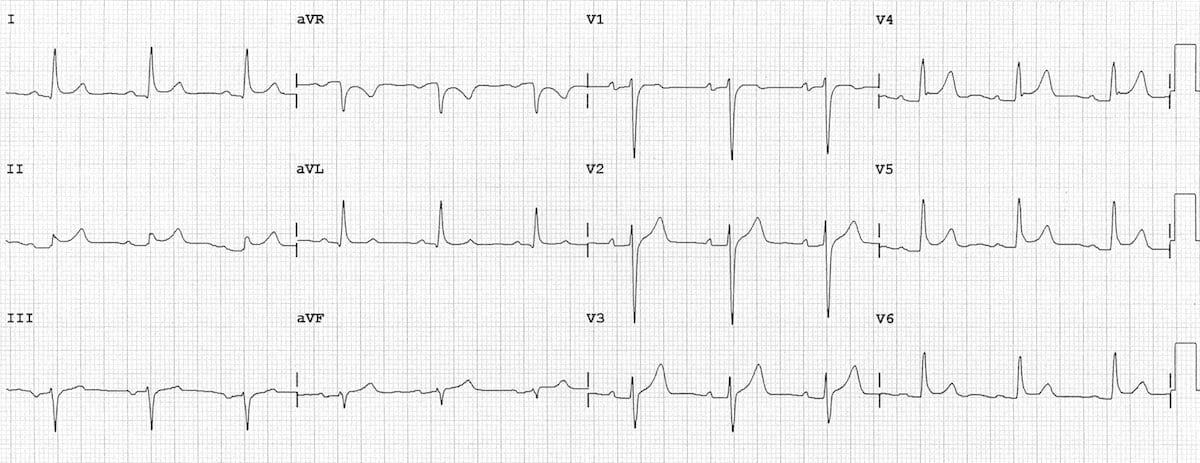
[[File:ECG-Pericarditis.jpg|center|thumb|Widespread concave ST elevation and PR depression is present throughout the precordial (V2-6) and limb leads (I, II, aVL, aVF). Case Courtesy of Ed Burns.]] | [[File:ECG-Pericarditis.jpg|center|thumb|Widespread concave ST elevation and PR depression is present throughout the precordial (V2-6) and limb leads (I, II, aVL, aVF). Case Courtesy of Ed Burns <ref>https://litfl.com/wp-content/uploads/2018/08/ECG-Pericarditis.jpg</ref>]] | ||
<br /> | <br /> | ||
=== X-ray === | === X-ray === | ||
A chest x-ray will reveal flattening of the costophrenic angles and be employed if echocardiography is not available enlargement of the cardiac silhouette as a result of both pleural and pericardial effusions.<ref name="pmid20511488">{{cite journal |vauthors=Khandaker MH, Espinosa RE, Nishimura RA, Sinak LJ, Hayes SN, Melduni RM, Oh JK |title=Pericardial disease: diagnosis and management |journal=Mayo Clin. Proc. |volume=85 |issue=6 |pages=572–93 |date=June 2010 |pmid=20511488 |pmc=2878263 |doi=10.4065/mcp.2010.0046 |url=}}</ref> | A chest x-ray will reveal flattening of the costophrenic angles and be employed if echocardiography is not available enlargement of the cardiac silhouette as a result of both pleural and pericardial effusions.<ref name="pmid20511488">{{cite journal |vauthors=Khandaker MH, Espinosa RE, Nishimura RA, Sinak LJ, Hayes SN, Melduni RM, Oh JK |title=Pericardial disease: diagnosis and management |journal=Mayo Clin. Proc. |volume=85 |issue=6 |pages=572–93 |date=June 2010 |pmid=20511488 |pmc=2878263 |doi=10.4065/mcp.2010.0046 |url=}}</ref> | ||
Revision as of 00:34, 1 January 2020
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Abdelrahman Ibrahim Abushouk, MD[2]; Mohammed A. Sbeih, M.D.[3]; Cafer Zorkun, M.D., Ph.D. [4]; Nabeel Ahmed, M.B.B.S
Synonyms and keywords: Postmyocardial infarction syndrome; PMIS; Post-cardiac injury syndrome
Overview
Dressler's syndrome or post myocardial infarction syndrome is a form of pericarditis that occurs in the setting of injury to the heart as a result of myocardial infarction. Dressler's syndrome typically occurs 2 to 10 weeks after myocardial infarction. This differentiates Dressler's syndrome from the much more common post myocardial infarction pericarditis which occurs between days 2 and 4 after myocardial infarction.
Historical Perspective
- Dressler's syndrome was first characterized by William Dressler in 1956.
- It should not be confused with the Dressler's syndrome of hemoglobinuria, named after Lucas Dressler who characterized it in 1854.[1][2][3]
Classification
- There is no established system for the classification of Dressler's syndrome.
Pathophysiology
- Although the exact cause remains unknown, Dressler's syndrome is believed to result from an autoimmune inflammatory reaction to myocardial neo-antigens, as well as injury to the mesothelial pericardial cells.
- It usually occurs within weeks or months of the infarction due to antimyocardial antibodies; this begins with myocardial injury that releases cardiac antigens and stimulates antibody formation.
- The immune complexes that are generated as anti-actin and actomycin antibodies deposit onto the pericardium and causes inflammation.
- The autoimmune response and syndrome may also develop secondary to pulmonary embolism.[4]
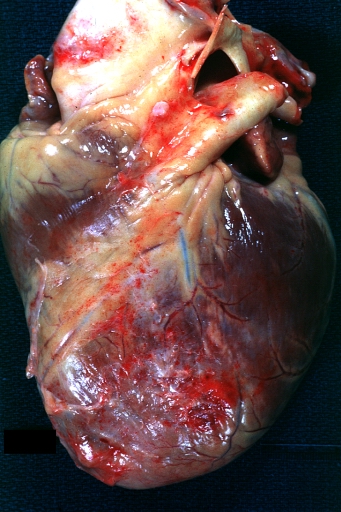
Gross Pathology
Causes
The common causes of Dressler's syndrome include:
- Surgeries associated with myocardial damage as
- Coronary artery bypass grafting and
- Aortic valve replacement.
- Myocardial infarction
- Pulmonary embolism
Differentiating Dressler's Syndrome from other Diseases
Dressler's syndrome typically occurs 2 to 10 weeks after a myocardial infarction has occurred.[6][7] This differentiates Dressler's syndrome from
- Post myocardial infarction pericarditis that occurs in 17,000 to 25,000 in every 100,000 cases of acute myocardial infarction between days 2 and 4 after the myocardial infarction.
- Pulmonary embolism, another identifiable cause of pleuritic (and non-pleuritic) chest pain in people who have been hospitalized and/or undergone surgical procedures within the preceding weeks.
Further, Dressler's syndrome should be differentiated from:
- Congestive Heart Failure
- Influenza
- Acute anemia with or without gastrointestinal bleeding
- Uremia
Epidemiology and Demographics
- Incidence: In the setting of myocardial infarction, Dressler's syndrome occurs in about 3 to 4% of MI cases.[8]
- Dressler's syndrome was more commonly seen in the era prior to reperfusion, but its incidence has markedly decreased in the reperfusion era, presumably because of smaller infarct sizes.[9]
- Age: Dressler's syndrome occurs more often in younger age groups.
- Gender: There is no gender predilection for Dressler's syndrome.
- Race: There is no racial predilection for Dressler's syndrome.
- Mortality rate: The mortality rate can reach up to 60% in hospital setting.
Risk Factors
- The risk of Dressler's syndrome increases with the size of the infarction.
- Further, a former episode of Dressler's syndrome increases the risk of relapse upon recurrent MI.
- Epidemiological studies showed a higher risk ratio of Dressler's syndrome with:
- Cardiac surgeries associated with greater myocardial damage as aortic valve replacement.
- Younger age
- Prior treatment with prednisone
- B -ve blood type
- Halothane anesthesia
- Viral infections that have been associated with Dressler's syndrome (based on the seasonal variations in incidence and elevated blood levels of viral components in Dressler's Syndrome patients) include:
Screening
- There is insufficient evidence to recommend routine screening for Dressler's syndrome.
Natural History, Complications, and Prognosis
- Pericardial effusion may result from the accumulation of fluids as a result of inflammation in the pericardial sac.
- Cardiac tamponade can occur if the accumulation of fluids in the pericardium is large enough and rapid enough.Classic findings of tamponade include Beck's triad:
- Low blood pressure
- Distended neck veins (JVD)
- Muffled/distant heart tones
- Constrictive pericarditis can occur if there is a chronic inflammatory response
Diagnosis
Diagnostic Study of Choice
2017 Revised ESC Guidelines for the Management of ST-Elevation Myocardial Infarction (DO NOT EDIT)
Diagnostic criteria do not differ from those for acute pericarditis including two of the following criteria: (i) pleuritic chest pain (85–90% of cases); (ii) pericardial friction rub (<_33% of cases); (iii) ECG changes (<_60% of cases), with new widespread ST-segment elevation, usually mild and progressive, or PR depression in the acute phase; and (iv) pericardial effusion (<_60% of cases and generally mild).
History and Symptoms
The syndrome consists of a persistent low-grade fever, and chest pain which is usually pleuritic in nature.The symptoms tend to occur after a few weeks or even months after myocardial infarction and tend to subside in a few days.
- Malaise
- Irritability
- Anorexia
- Dyspnea (with or without hypoxia)
- Palpitations
- Arthralgias
Physical Examination
- Pericardial friction rub: This characteristic sign may disappear secondary to either improvement in or worsening of accumulation of pericardial fluid
- Tachycardia
- Pulsus paradoxus (>10 mmHg decrease in blood pressure with inspiration and decreased pulse amplitude on the radial artery).
- Signs of pneumonitis (e.g., a cough, decreased oxygen saturation, fever).
- Minimal respiratory symptoms to significant respiratory distress with large pleural effusions.
Laboratory Findings
Blood cultures should be obtained early in the workup of DS as this will help differentiate between an inflammatory versus an infectious cause of the patient’s condition. In the case of true DS, blood cultures should be negative.
Laboratory studies that may help point toward a diagnosis of DS include an elevated white blood cell count (with a leftward shift) and elevated acute phase reactants (e.g., erythrocyte sedimentation rate and C-reactive protein). Additionally, there may be a high titer of anti-heart antibodies present in serology.
If it is possible, pericardial fluid (e.g., through a pericardial drain) should be examined for cell count, differential, cultures, Gram stain, cytology, total protein, and triglyceride levels
Electrocardiogram
An electrocardiograph (ECG) may demonstrate
- ST segment elevation
- T-wave inversion (as with pericarditis).
- PR depression
- Variations in the amplitude or directionality of QRS from beat to beat and/or a low voltage QRS.
X-ray
A chest x-ray will reveal flattening of the costophrenic angles and be employed if echocardiography is not available enlargement of the cardiac silhouette as a result of both pleural and pericardial effusions.[11]
Echocardiography or Ultrasound
- An echo will allow for evaluation of the pericardial fluid, if present, and help discern the exact cause of reduced cardiac output (i.e., determine whether truly DS or another condition such as congestive heart failure).
- An echo will further allow for evaluation of ventricular contractility, in addition to assessment of the potential risk of cardiac tamponade (i.e., if cardiac chambers appear compressed by pericardial fluid). The more pericardial fluid that is accumulated, the easier it is to detect its presence by echocardiography.[12]
- Whilst definitive evaluation with formal echocardiogram is the gold standard, bedside cardiac ultrasound.
CT Scan
MRI
If it is difficult to assess the posterior pericardium with an echo, cardiac magnetic resonance imaging (MRI) may employed to determine whether there is an effusion present. In some instances, fluid collections become loculated.[13]
Other Imaging Findings
There are no other imaging findings associated with Dressler's syndrome.
Other Diagnostic Studies
There are no other diagnostic studies associated with Dressler's syndrome.
Treatment
Medical Therapy
Dressler's syndrome is typically treated with high dose (up to 650 mg PO q 4 to 6 hours) enteric-coated aspirin. Acetaminophen can be added for pain management as this does not affect the coagulation system. Anticoagulants should be discontinued if the patient develops a pericardial effusion.[14]
2017 Revised ESC Guidelines for the Management of ST-Elevation Myocardial Infarction (DO NOT EDIT)
- Anti-inflammatory therapy is recommended in post-STEMI pericarditis as in post-cardiac injury pericardial syndromes for symptom relief and reduction of recurrences.
- Aspirin is recommended as first choice of anti-inflammatory therapy post-STEMI at a dose of 500–1000 mg every 6–8 h for 1–2 weeks, decreasing the total daily dose by 250–500 mg every 1–2 weeks in keeping with 2015 ESC Guidelines for the diagnosis and management of pericardial diseases.
- Colchicine is recommended as first-line therapy as an adjunct to aspirin/non-steroidal anti-inflammatory drug therapy (3 months) and is also recommended for the recurrent forms (6 months).
- Corticosteroids are not recommended due to the risk of scar thinning with aneurysm development or rupture.
- Pericardiocentesis is rarely required, except for cases of haemodynamic compromise with signs of tamponade.
2013 Revised ACCF/AHA Guidelines for the Management of ST-Elevation Myocardial Infarction
Management of Pericarditis After STEMI
| Class I |
| "1. Aspirin is recommended for treatment of pericarditis after STEMI.(Level of Evidence: B)" |
| Class III (Harm) |
| "1. Glucocorticoids and nonsteroidal antiinflammatory drugs are potentially harmful for treatment of pericarditis after STEMI. (Level of Evidence: B)" |
| Class IIb |
| "1. Administration of acetaminophen, colchicine, or narcotic analgesics may be reasonable if aspirin, even in higher doses, is not effective. (Level of Evidence: B)" |
Surgery
- No surgical intervention is recommended in the management of Dressler's syndrome.
- Pericardiocentesis is rarely required, except for cases of haemodynamic compromise with signs of tamponade.
Primary Prevention
Secondary Prevention
Recurrence of post-pericardiotomy syndrome, including DS, is common and relapses have been reported up to 1 year following the initial event. Some suggests that intravenous immunoglobulin therapy has some benefit in refractory cases, especially in children [19]. Remember the number one risk factor for developing DS is having had it before.
References
- ↑ Template:WhoNamedIt
- ↑ L. A. Dressler. Ein Fall von intermittirender Albuminurie und Chromaturie. Archiv für pathologische Anatomie und Physiologie und für klinische Medicin, 1854, 6: 264-266.
- ↑ DRESSLER W (1956). "A post-myocardial infarction syndrome; preliminary report of a complication resembling idiopathic, recurrent, benign pericarditis". J Am Med Assoc. 160 (16): 1379–83. PMID 13306560.
- ↑ Jerjes-Sánchez C, Ramírez-Rivera A, Ibarra-Pérez C (1996). "The Dressler syndrome after pulmonary embolism". Am J Cardiol. 78 (3): 343–5. PMID 8759817.
- ↑ http://www.peir.net/
- ↑ Krainin F, Flessas A, Spodick D (1984). "Infarction-associated pericarditis. Rarity of diagnostic electrocardiogram". N Engl J Med. 311 (19): 1211–4. PMID 6493274.
- ↑ Krainin F, Flessas A, Spodick D (1984). "Infarction-associated pericarditis. Rarity of diagnostic electrocardiogram". N Engl J Med. 311 (19): 1211–4. PMID 6493274.
- ↑ Krainin F, Flessas A, Spodick D (1984). "Infarction-associated pericarditis. Rarity of diagnostic electrocardiogram". N Engl J Med. 311 (19): 1211–4. PMID 6493274.
- ↑ Tofler GH, Muller JE, Stone PH, Willich SN, Davis VG, Poole WK; et al. (1989). "Pericarditis in acute myocardial infarction: characterization and clinical significance". Am Heart J. 117 (1): 86–92. PMID 2643287.
- ↑ https://litfl.com/wp-content/uploads/2018/08/ECG-Pericarditis.jpg
- ↑ Khandaker MH, Espinosa RE, Nishimura RA, Sinak LJ, Hayes SN, Melduni RM, Oh JK (June 2010). "Pericardial disease: diagnosis and management". Mayo Clin. Proc. 85 (6): 572–93. doi:10.4065/mcp.2010.0046. PMC 2878263. PMID 20511488.
- ↑ Wessman DE, Stafford CM (March 2006). "The postcardiac injury syndrome: case report and review of the literature". South. Med. J. 99 (3): 309–14. doi:10.1097/01.smj.0000203330.15503.0b. PMID 16553111.
- ↑ Scarfone RJ, Donoghue AJ, Alessandrini EA (August 2003). "Cardiac tamponade complicating postpericardiotomy syndrome". Pediatr Emerg Care. 19 (4): 268–71. doi:10.1097/01.pec.0000092573.40174.74. PMID 12972828.
- ↑ Jaworska-Wilczynska M, Abramczuk E, Hryniewiecki T (November 2011). "Postcardiac injury syndrome". Med. Sci. Monit. 17 (11): CQ13–14. doi:10.12659/msm.882029. PMID 22037738.