De Quervain's thyroiditis pathophysiology: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (32 intermediate revisions by 4 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}} {{MMF}} | {{CMG}}; {{AE}} {{MMF}} | ||
==Overview== | ==Overview== | ||
The exact pathogenesis of de Quervain's thyroiditis is unclear. It is proposed that [[cytotoxic T cell]] recognition of complex viral and cell [[antigens]] presentation leads to the [[thyroid follicular cell]] damage which is responsible for the [[pathogenesis]] of de Quervain's thyroiditis. De Quervain's thyroiditis is usually preceded by a viral prodrome and also have a [[genetic predisposition]]. [[HLA]] | The exact [[pathogenesis]] of de Quervain's thyroiditis is unclear. It is proposed that [[cytotoxic T cell]] recognition of complex [[viral]] and cell [[antigens]] presentation leads to the [[thyroid follicular cell]] damage which is responsible for the [[pathogenesis]] of de Quervain's thyroiditis. De Quervain's thyroiditis is usually preceded by a [[viral]] prodrome and also have a [[genetic predisposition]]. [[HLA-B|HLA B]]35 and [[HLA-B|HLA B]]15/62 are associated with de Quervain's thyroiditis. | ||
==Pathophysiology== | ==Pathophysiology== | ||
{| | |||
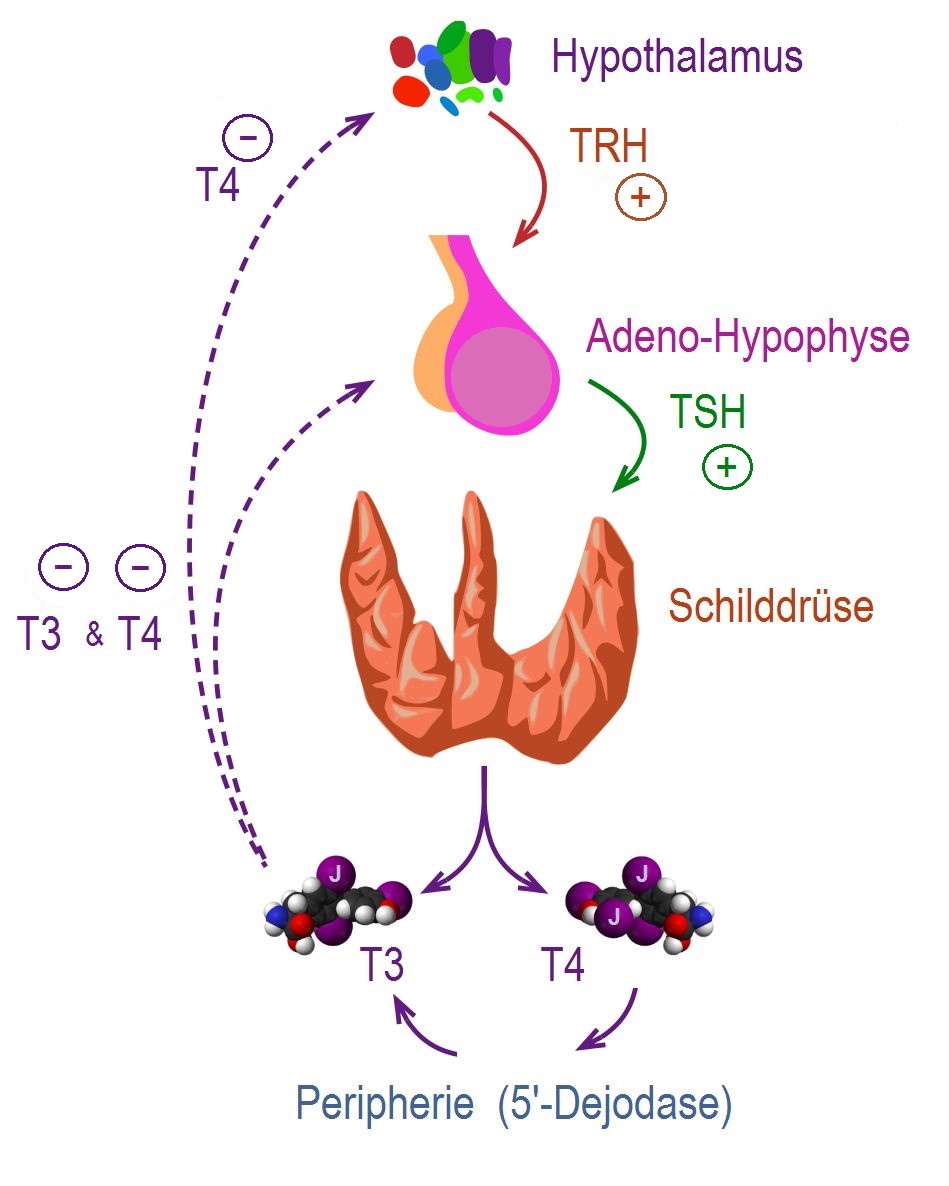
|The control, synthesis, and release of the thyroid hormone is usually controlled by [[hypothalamus]] and [[pituitary gland]].<ref name="pmid25905405">{{cite journal |vauthors=De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, Rousset B, Dupuy C, Miot F, Dumont J |title=Thyroid Hormone Synthesis And Secretion |journal= |volume= |issue= |pages= |year= |pmid=25905405 |doi= |url=}}</ref><ref name="pmid11949270">{{cite journal |vauthors=Kirsten D |title=The thyroid gland: physiology and pathophysiology |journal=Neonatal Netw |volume=19 |issue=8 |pages=11–26 |year=2000 |pmid=11949270 |doi=10.1891/0730-0832.19.8.11 |url=}}</ref> | |||
* [[Thyroid hormone|Thyroid hormones (T3 and T4)]] are regulating [[basal metabolic rate]], influence [[oxygen]] consumption by tissues. They are crucial for normal development of the [[brain]] and growth of the body. | |||
* Secretion of [[thyroid hormones]] follows upper control from the [[hypothalamus]] and the [[pituitary]]. [[Thyrotropin-releasing hormone|Thyroid releasing hormone (TRH)]] acts on [[thyrotropes]] releasing cells in the [[pituitary]] causing them to release [[Thyroid-stimulating hormone|thyroid stimulating hormone (TSH)]]. | |||
* [[TSH]] acts on [[thyroid gland]] by binding to specific membrane receptors and activating an [[intracellular]] pathway involving [[cAMP]] that ends in the formation and secretion of [[thyroid hormones]]. | |||
* [[Iodine]] is essential for the synthesis of [[thyroid hormones]]. [[Iodide]] is uptaken through a special Na/I transporter found in the membrane of [[thyroid]] follicular cell. After the [[iodide]] uptake, it goes through a series of organic reactions ending in the formation of the two forms of [[thyroid hormones]]: [[T3]] and [[T4]]. [[T3]] and [[T4]] remain stored in the [[thyroglobulin]] of the follicles and are released in response to further stimulation by [[TSH]] to the [[Thyroid follicle|thyroid follicles]]. | |||
* While [[T3]] is 3 to 5 times more potent than [[T4]], it represents only one-fourth of the total hormone secretion. [[T3]] is thought to be the biologically active form of the hormone. Most of the circulating [[T3]] is due to peripheral conversion of [[T4]] in the liver and peripheral tissues while only a small percentage is secreted directly from the [[thyroid gland]] itself. | |||
* [[T3]] and [[T4]] act on nuclear receptors ([[DNA]] binding [[proteins]]) and cause the regulate the [[transcription]] of many [[proteins]] to regulate the [[metabolic rate]] of the body. | |||
* The higher regulation of [[thyroxine]] secretion follows the [[negative feedback]] role, meaning that high levels of [[T3]] and [[T4]] will suppress [[TRH]] and [[TSH]] secretion and vice versa (Low levels of [[Thyroxin|thyroxine]] will stimulate [[TRH]] and [[TSH]] secretion). This is useful in diagnosing the cause of [[hyperthyroidism]]. | |||
* [[TSH]] will be low in primary [[hyperthyroidism]] where the gland is the source of the excess hormones. In secondary [[hyperthyroidism]], [[TSH]] will be high as the [[pituitary]] or the [[hypothalamus]] are the sources of the disease. | |||
| | |||
[[Image: Regulation der Schilddrüsenfunktion .jpg|right|300px|thumb|'''Regulation of thyroid hormone secretion.''' <small>Source:By CFCF; slightly modified by Geo-Science-International - This file was derived from Thyroid vector.svg:, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=47043638</small>]] | |||
|} | |||
===Pathogenesis=== | ===Pathogenesis=== | ||
The exact [[pathogenesis]] of de Quervain's thyroiditis is unclear, but [[autoimmunity]] mechanism is proposed.<ref name="pmid12608662">{{cite journal |vauthors=Kojima M, Nakamura S, Oyama T, Sugihara S, Sakata N, Masawa N |title=Cellular composition of subacute thyroiditis. an immunohistochemical study of six cases |journal=Pathol. Res. Pract. |volume=198 |issue=12 |pages=833–7 |year=2002 |pmid=12608662 |doi=10.1078/0344-0338-00344 |url=}}</ref><ref name="pmid17848836">{{cite journal |vauthors=Erdem N, Erdogan M, Ozbek M, Karadeniz M, Cetinkalp S, Ozgen AG, Saygili F, Yilmaz C, Tuzun M, Kabalak T |title=Demographic and clinical features of patients with subacute thyroiditis: results of 169 patients from a single university center in Turkey |journal=J. Endocrinol. Invest. |volume=30 |issue=7 |pages=546–50 |year=2007 |pmid=17848836 |doi= |url=}}</ref> | The exact [[pathogenesis]] of de Quervain's thyroiditis is unclear, but [[autoimmunity]] mechanism is proposed.<ref name="pmid12608662">{{cite journal |vauthors=Kojima M, Nakamura S, Oyama T, Sugihara S, Sakata N, Masawa N |title=Cellular composition of subacute thyroiditis. an immunohistochemical study of six cases |journal=Pathol. Res. Pract. |volume=198 |issue=12 |pages=833–7 |year=2002 |pmid=12608662 |doi=10.1078/0344-0338-00344 |url=}}</ref><ref name="pmid17848836">{{cite journal |vauthors=Erdem N, Erdogan M, Ozbek M, Karadeniz M, Cetinkalp S, Ozgen AG, Saygili F, Yilmaz C, Tuzun M, Kabalak T |title=Demographic and clinical features of patients with subacute thyroiditis: results of 169 patients from a single university center in Turkey |journal=J. Endocrinol. Invest. |volume=30 |issue=7 |pages=546–50 |year=2007 |pmid=17848836 |doi= |url=}}</ref><ref name="pmid19138419">{{cite journal |vauthors=Desailloud R, Hober D |title=Viruses and thyroiditis: an update |journal=Virol. J. |volume=6 |issue= |pages=5 |year=2009 |pmid=19138419 |pmc=2654877 |doi=10.1186/1743-422X-6-5 |url=}}</ref> | ||
*De Quervain's thyroiditis is usually preceded by a viral prodrome. Various viral infections are associated with the de Quervain's thyroiditis including [[mumps]], [[Adenoviridae|adenovirus]], [[Epstein Barr virus|Epstein–Barr virus]], [[coxsackievirus]], [[cytomegalovirus]], [[influenza]], [[echovirus]], and [[enterovirus]]. | *De Quervain's thyroiditis is usually preceded by a viral prodrome. Various viral infections are associated with the de Quervain's thyroiditis including [[mumps]], [[Adenoviridae|adenovirus]], [[Epstein Barr virus|Epstein–Barr virus]], [[coxsackievirus]], [[cytomegalovirus]], [[influenza]], [[echovirus]], and [[enterovirus]]. | ||
*De Quervain's thyroiditis is associated with [[HLA-B|HLA B]]B35. It is postulated that the [[antigen]] triggers the activation of [[HLA-B|HLA B]]35 positive [[inflammatory cells]] which in turn activates the [[cytotoxic T-lymphocytes]]. | |||
*[[Cytotoxic T cell]] recognition of viral and cell [[antigens]] presented in a complex leads to the [[thyroid follicular cell]] damage. | |||
*The [[autoimmune]] process leads to [[inflammatory cells]] infiltration of the gland. The changes may lead to [[granulomatous]] or non-granulomatous lesions. | |||
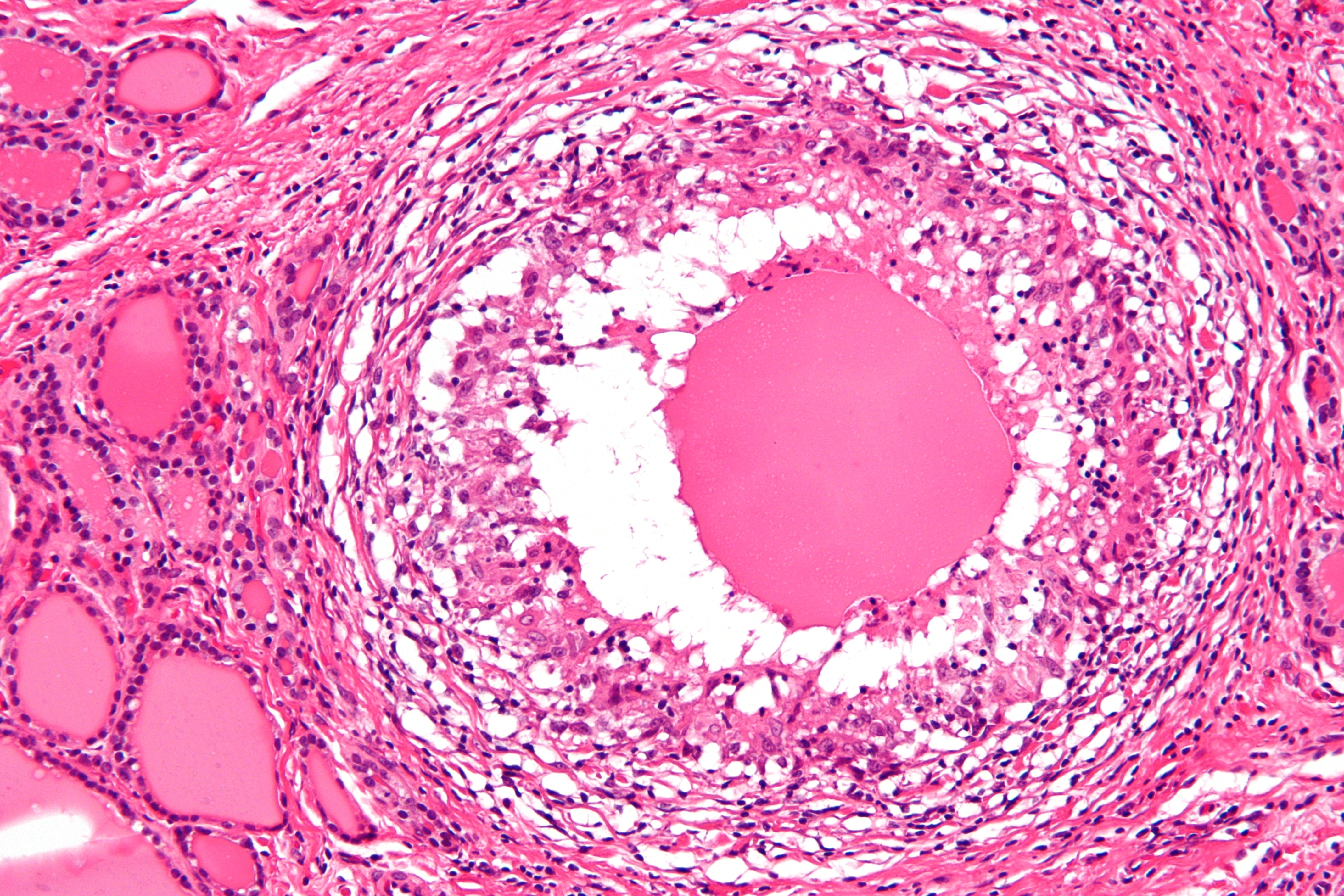
**'''Granulomatous lesion''' | |||
***[[Granulomatous|Granulomatous lesion]] comprises of colloid, small [[lymphocytes]], [[neutrophils]], [[macrophages]] with or without epithelioid features, and multinucleated giant cells of foreign body type. In the granulomatous lesion, the giant cells are usually CD68+, thyroglobulin– and cytokeratin–. Small lymphocytes in the granulomas are CD3+, [[CD8]]+, [[CD45]]RO+ [[cytotoxic T-cells]]. Numerous plasmacytoid [[monocytes]] were also closely associated with the [[granulomas]]. | |||
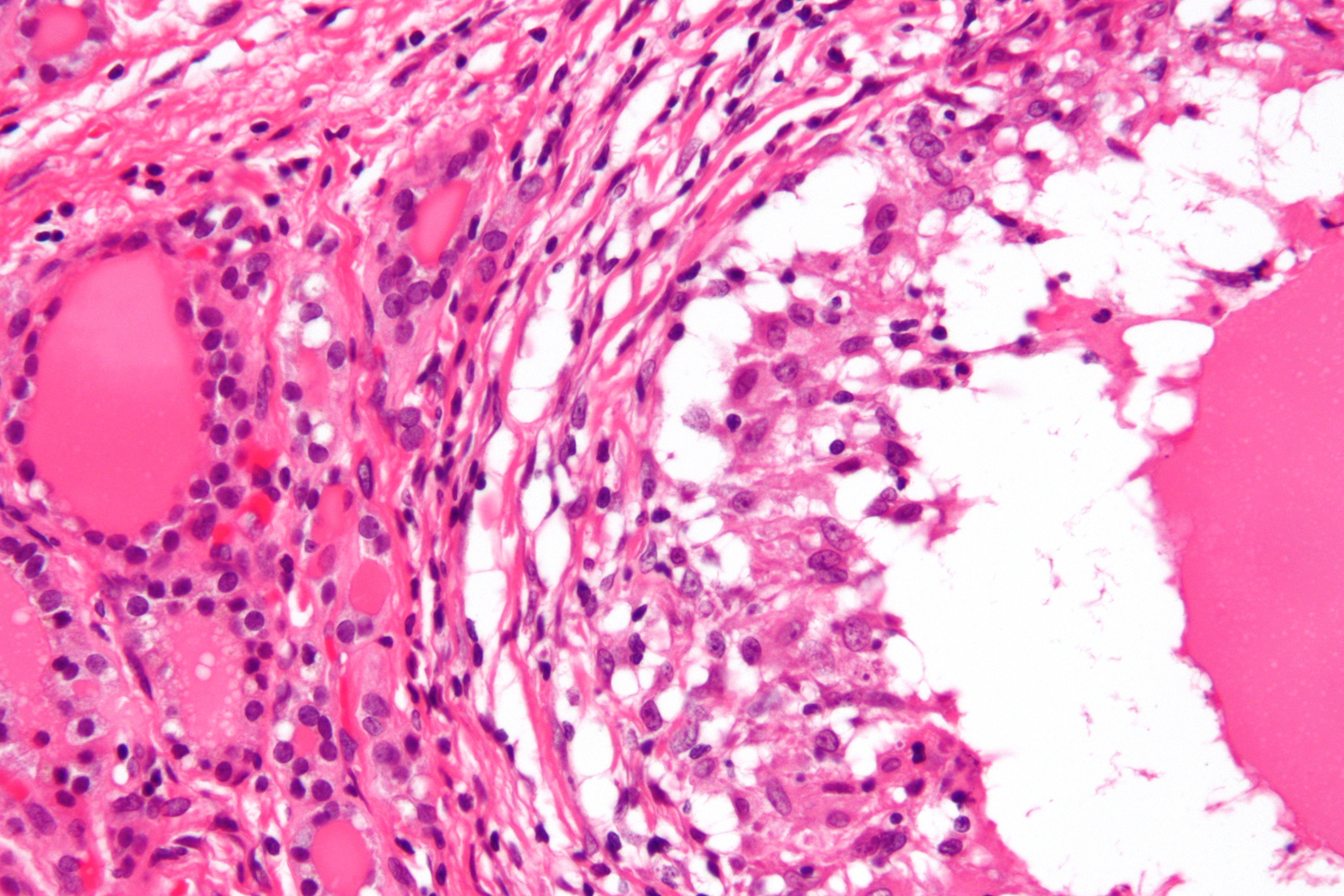
**'''Non-granulomatous lesion''' | |||
***Follicles in the non-granulomatous lesion are infiltrated by [[CD8+ T cells|CD8+ T-lymphocytes]], plasmacytoid [[monocytes]], and [[Histiocyte|histiocytes]], resulting in disrupted [[basement membrane]] and rupture of the follicles. | |||
==Genetics== | ==Genetics== | ||
*De Quervain's thyroiditis is associated with:<ref name="pmid885992">{{cite journal |vauthors=Nyulassy S, Hnilica P, Buc M, Guman M, Hirschová V, Stefanovic J |title=Subacute (de Quervain's) thyroiditis: association with HLA-Bw35 antigen and abnormalities of the complement system, immunoglobulins and other serum proteins |journal=J. Clin. Endocrinol. Metab. |volume=45 |issue=2 |pages=270–4 |year=1977 |pmid=885992 |doi=10.1210/jcem-45-2-270 |url=}}</ref><ref name="pmid2298855">{{cite journal |vauthors=de Bruin TW, Riekhoff FP, de Boer JJ |title=An outbreak of thyrotoxicosis due to atypical subacute thyroiditis |journal=J. Clin. Endocrinol. Metab. |volume=70 |issue=2 |pages=396–402 |year=1990 |pmid=2298855 |doi=10.1210/jcem-70-2-396 |url=}}</ref> | *De Quervain's thyroiditis is associated with:<ref name="pmid885992">{{cite journal |vauthors=Nyulassy S, Hnilica P, Buc M, Guman M, Hirschová V, Stefanovic J |title=Subacute (de Quervain's) thyroiditis: association with HLA-Bw35 antigen and abnormalities of the complement system, immunoglobulins and other serum proteins |journal=J. Clin. Endocrinol. Metab. |volume=45 |issue=2 |pages=270–4 |year=1977 |pmid=885992 |doi=10.1210/jcem-45-2-270 |url=}}</ref><ref name="pmid2298855">{{cite journal |vauthors=de Bruin TW, Riekhoff FP, de Boer JJ |title=An outbreak of thyrotoxicosis due to atypical subacute thyroiditis |journal=J. Clin. Endocrinol. Metab. |volume=70 |issue=2 |pages=396–402 |year=1990 |pmid=2298855 |doi=10.1210/jcem-70-2-396 |url=}}</ref> | ||
**The [[human leukocyte antigen]] (HLA | **The [[human leukocyte antigen]] ([[HLA-B|HLA B]]35 | ||
**[[HLA]] | **[[HLA-B|HLA B]]15/62 (in rare cases) | ||
==Associated conditions== | ==Associated conditions== | ||
The following conditions may be associated with De Quervain's thyroiditis:<ref name="pmid12727961">{{cite journal |vauthors=Fatourechi V, Aniszewski JP, Fatourechi GZ, Atkinson EJ, Jacobsen SJ |title=Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study |journal=J. Clin. Endocrinol. Metab. |volume=88 |issue=5 |pages=2100–5 |year=2003 |pmid=12727961 |doi=10.1210/jc.2002-021799 |url=}}</ref> | |||
*[[Rheumatoid arthritis]] | |||
*[[Sjogren syndrome]] | |||
*[[Ulcerative colitis]] | |||
*[[Urticaria]] | |||
*[[Thyroid malignancy]] | |||
==Gross Pathology== | ==Gross Pathology== | ||
On gross pathology, subacute thyroiditis frequently resembles thyroid malignancy. Subacute thyroiditis usually has the following features: | On gross pathology, subacute thyroiditis frequently resembles [[thyroid malignancy]]. Subacute thyroiditis usually has the following features:<ref name="Endotext">{{cite book|authors=Shrestha RT, Hennessey J. |title=Acute and Subacute, and Riedel’s Thyroiditis.|url=https://www.ncbi.nlm.nih.gov/books/NBK285553/}}</ref> | ||
*Firm to dense consistency | *Firm to dense consistency | ||
*Pale white color | *Pale white color | ||
*Poorly defined margins | *Poorly defined margins | ||
*Involvement of adjacent normal thyroid | *Involvement of adjacent normal [[thyroid]] | ||
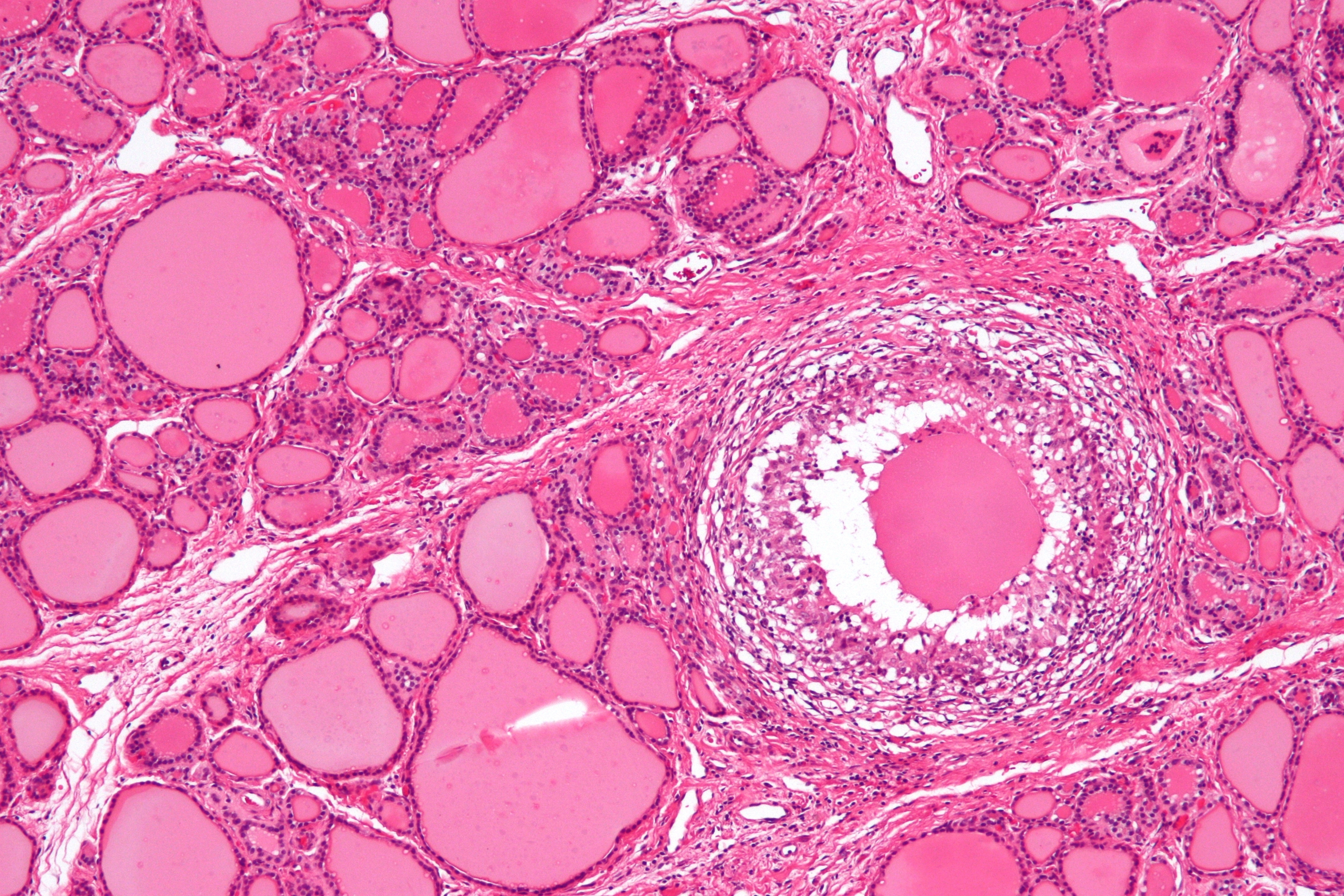
==Microscopic pathology== | ==Microscopic pathology== | ||
The primary pathology of de Quervain's thyroiditis is:<ref name="pmid12608662">{{cite journal |vauthors=Kojima M, Nakamura S, Oyama T, Sugihara S, Sakata N, Masawa N |title=Cellular composition of subacute thyroiditis. an immunohistochemical study of six cases |journal=Pathol. Res. Pract. |volume=198 |issue=12 |pages=833–7 |year=2002 |pmid=12608662 |doi=10.1078/0344-0338-00344 |url=}}</ref> | The primary pathology of de Quervain's thyroiditis is:<ref name="pmid12608662">{{cite journal |vauthors=Kojima M, Nakamura S, Oyama T, Sugihara S, Sakata N, Masawa N |title=Cellular composition of subacute thyroiditis. an immunohistochemical study of six cases |journal=Pathol. Res. Pract. |volume=198 |issue=12 |pages=833–7 |year=2002 |pmid=12608662 |doi=10.1078/0344-0338-00344 |url=}}</ref><ref name="Endotext">{{cite book|authors=Shrestha RT, Hennessey J. |title=Acute and Subacute, and Riedel’s Thyroiditis.|url=https://www.ncbi.nlm.nih.gov/books/NBK285553/}}</ref> | ||
*Infiltration with polymorphonuclear leukocytes initially | *Infiltration with polymorphonuclear leukocytes initially | ||
*Predominance of lymphocytes and macrophages in advanced form | *Predominance of lymphocytes and macrophages in advanced form | ||
| Line 41: | Line 65: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
| |||
[[Category:Medicine]] | |||
[[Category:Endocrinology]] | |||
[[Category:Up-To-Date]] | |||
Latest revision as of 21:14, 29 July 2020
|
De Quervain's thyroiditis Microchapters |
|
Differentiating De Quervain's thyroiditis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Furqan M M. M.B.B.S[2]
Overview
The exact pathogenesis of de Quervain's thyroiditis is unclear. It is proposed that cytotoxic T cell recognition of complex viral and cell antigens presentation leads to the thyroid follicular cell damage which is responsible for the pathogenesis of de Quervain's thyroiditis. De Quervain's thyroiditis is usually preceded by a viral prodrome and also have a genetic predisposition. HLA B35 and HLA B15/62 are associated with de Quervain's thyroiditis.
Pathophysiology
The control, synthesis, and release of the thyroid hormone is usually controlled by hypothalamus and pituitary gland.[1][2]
|
 |
Pathogenesis
The exact pathogenesis of de Quervain's thyroiditis is unclear, but autoimmunity mechanism is proposed.[3][4][5]
- De Quervain's thyroiditis is usually preceded by a viral prodrome. Various viral infections are associated with the de Quervain's thyroiditis including mumps, adenovirus, Epstein–Barr virus, coxsackievirus, cytomegalovirus, influenza, echovirus, and enterovirus.
- De Quervain's thyroiditis is associated with HLA BB35. It is postulated that the antigen triggers the activation of HLA B35 positive inflammatory cells which in turn activates the cytotoxic T-lymphocytes.
- Cytotoxic T cell recognition of viral and cell antigens presented in a complex leads to the thyroid follicular cell damage.
- The autoimmune process leads to inflammatory cells infiltration of the gland. The changes may lead to granulomatous or non-granulomatous lesions.
- Granulomatous lesion
- Granulomatous lesion comprises of colloid, small lymphocytes, neutrophils, macrophages with or without epithelioid features, and multinucleated giant cells of foreign body type. In the granulomatous lesion, the giant cells are usually CD68+, thyroglobulin– and cytokeratin–. Small lymphocytes in the granulomas are CD3+, CD8+, CD45RO+ cytotoxic T-cells. Numerous plasmacytoid monocytes were also closely associated with the granulomas.
- Non-granulomatous lesion
- Follicles in the non-granulomatous lesion are infiltrated by CD8+ T-lymphocytes, plasmacytoid monocytes, and histiocytes, resulting in disrupted basement membrane and rupture of the follicles.
- Granulomatous lesion
Genetics
- De Quervain's thyroiditis is associated with:[6][7]
- The human leukocyte antigen (HLA B35
- HLA B15/62 (in rare cases)
Associated conditions
The following conditions may be associated with De Quervain's thyroiditis:[8]
Gross Pathology
On gross pathology, subacute thyroiditis frequently resembles thyroid malignancy. Subacute thyroiditis usually has the following features:[9]
- Firm to dense consistency
- Pale white color
- Poorly defined margins
- Involvement of adjacent normal thyroid
Microscopic pathology
The primary pathology of de Quervain's thyroiditis is:[3][9]
- Infiltration with polymorphonuclear leukocytes initially
- Predominance of lymphocytes and macrophages in advanced form
- Destruction of the follicular epithelium
- Parenchymal destruction and scar tissue
- Loss of the follicular integrity
Gallery
-
De Quervain's thyroiditis (By Nephron - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=18491382)
-
De Quervain's thyroiditis (By Nephron - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=18491421)
-
De Quervain's thyroiditis (By Nephron - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=18491421)
References
- ↑ De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, Rousset B, Dupuy C, Miot F, Dumont J. "Thyroid Hormone Synthesis And Secretion". PMID 25905405.
- ↑ Kirsten D (2000). "The thyroid gland: physiology and pathophysiology". Neonatal Netw. 19 (8): 11–26. doi:10.1891/0730-0832.19.8.11. PMID 11949270.
- ↑ 3.0 3.1 Kojima M, Nakamura S, Oyama T, Sugihara S, Sakata N, Masawa N (2002). "Cellular composition of subacute thyroiditis. an immunohistochemical study of six cases". Pathol. Res. Pract. 198 (12): 833–7. doi:10.1078/0344-0338-00344. PMID 12608662.
- ↑ Erdem N, Erdogan M, Ozbek M, Karadeniz M, Cetinkalp S, Ozgen AG, Saygili F, Yilmaz C, Tuzun M, Kabalak T (2007). "Demographic and clinical features of patients with subacute thyroiditis: results of 169 patients from a single university center in Turkey". J. Endocrinol. Invest. 30 (7): 546–50. PMID 17848836.
- ↑ Desailloud R, Hober D (2009). "Viruses and thyroiditis: an update". Virol. J. 6: 5. doi:10.1186/1743-422X-6-5. PMC 2654877. PMID 19138419.
- ↑ Nyulassy S, Hnilica P, Buc M, Guman M, Hirschová V, Stefanovic J (1977). "Subacute (de Quervain's) thyroiditis: association with HLA-Bw35 antigen and abnormalities of the complement system, immunoglobulins and other serum proteins". J. Clin. Endocrinol. Metab. 45 (2): 270–4. doi:10.1210/jcem-45-2-270. PMID 885992.
- ↑ de Bruin TW, Riekhoff FP, de Boer JJ (1990). "An outbreak of thyrotoxicosis due to atypical subacute thyroiditis". J. Clin. Endocrinol. Metab. 70 (2): 396–402. doi:10.1210/jcem-70-2-396. PMID 2298855.
- ↑ Fatourechi V, Aniszewski JP, Fatourechi GZ, Atkinson EJ, Jacobsen SJ (2003). "Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study". J. Clin. Endocrinol. Metab. 88 (5): 2100–5. doi:10.1210/jc.2002-021799. PMID 12727961.
- ↑ 9.0 9.1 Shrestha RT, Hennessey J. Acute and Subacute, and Riedel’s Thyroiditis.