Congestive heart failure chest x ray: Difference between revisions
No edit summary |
|||
| (25 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | __NOTOC__ | ||
{{CMG}}; {{AOEIC}} {{LG}} | {| class="infobox" style="float:right;" | ||
|- | |||
| [[File:Siren.gif|30px|link= Heart failure resident survival guide]]|| <br> || <br> | |||
| [[Heart failure resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] | |||
|} | |||
{{Congestive heart failure}} | |||
{{CMG}}; {{AOEIC}} {{LG}} {{EdzelCo}} | |||
== Overview== | == Overview== | ||
[[Chest X-ray|Chest x-ray]] in a patient with [[heart failure]] shows [[cardiomegaly]] ([[cardiac enlargement]] and [[pulmonary congestion]] ([[Kerley B lines]], and in some cases [[pleural effusion]]). | |||
==Chest X | ==Chest X Ray== | ||
*Since the left ventricle often dilates in the anteroposterior direction, the cardiac silhouette may appear deceptively normal. | *Since the [[left ventricle]] often dilates in the anteroposterior direction, the [[cardiac silhouette]] may appear deceptively normal. | ||
*Chest x-ray findings include: | *[[Chest X-ray|Chest x-ray]] findings include: | ||
#[[Kerley B lines]] or thickening of the interlobular septa | #[[Kerley B lines]] or thickening of the interlobular septa | ||
#[[Peribronchial cuffing]] | #[[Peribronchial cuffing]] | ||
#Thickening of the fissures | #Thickening of the [[fissures]] | ||
#Cephalization | #[[Cephalization]] | ||
#Increased vascular markings | #Increased [[vascular markings]] | ||
#[[Interstitial edema]] | #[[Interstitial edema]] | ||
#[[Pleural effusion]]s | #[[Pleural effusion]]s | ||
====Kerley B Lines==== | ====Kerley B Lines==== | ||
[[Kerley B lines]] are short parallel lines at the lung periphery. These lines represent distended interlobular septa, which are usually less than 1 cm in length and parallel to one another at right angles to the [[pleura]]. They are located peripherally in contact with the pleura, but are generally absent along fissural surfaces. They may be seen in any zone but are most frequently observed at the lung bases at the costophrenic angles on the PA radiograph, and in the substernal region on lateral radiographs. | [[Kerley B lines]] are short parallel lines at the [[lung]] periphery. These lines represent distended [[interlobular septa]], which are usually less than 1 cm in length and parallel to one another at right angles to the [[pleura]]. They are located peripherally in contact with the [[pleura]], but are generally absent along [[fissural]] surfaces. They may be seen in any zone but are most frequently observed at the lung bases at the costophrenic angles on the PA radiograph, and in the substernal region on lateral radiographs. | ||
<gallery> | <gallery> | ||
Image:Kerley B 001.jpg|Plain film: [[Mitral stenosis]], Kerley B lines | Image:Kerley B 001.jpg|Plain film: [[Mitral stenosis]], [[Kerley B lines]] | ||
Image:Kerley B 002.jpg|Plain film: [[Mitral stenosis]], Kerley B lines | Image:Kerley B 002.jpg|Plain film: [[Mitral stenosis]], [[Kerley B lines]] | ||
Image:Kerley B 003.jpg|Plain film: [[Mitral stenosis]], Kerley B lines | Image:Kerley B 003.jpg|Plain film: [[Mitral stenosis]], [[Kerley B lines]] | ||
</gallery> | </gallery> | ||
<br clear="left"/> | <br clear="left"/> | ||
====Peribronchial Cuffing==== | ====[[Peribronchial]] Cuffing==== | ||
[[Image:Peribronchial cuffing.png|thumb|left|The red arrows point to thickened bronchial walls that have a doughnut-like appearance.]] [[Peribronchial cuffing]] is an abnormality on a chest x-ray whereby the usually thin bronchial walls are thickened and take on a doughnut-like appearance.<br clear="left"/> | [[Image:Peribronchial cuffing.png|thumb|left|The red arrows point to thickened [[bronchial]] walls that have a doughnut-like appearance.]] [[Peribronchial cuffing]] is an abnormality on a [[chest x-ray]] whereby the usually thin [[bronchial]] walls are thickened and take on a doughnut-like appearance.<br clear="left"/> | ||
====Cephalization==== | ====[[Cephalization]]==== | ||
[[Image:Cephalization.png|left|thumb]]Cephalization refers to the redistribution of blood into the upper lobe vessels. It has been hypothesized that once the hydrostatic pressure exceeds 10 mm Hg, then fluid begins to leak into the interstitium of the lung. This excess fluid initially compresses the lower lobe vessels, perhaps as a result of gravity. After this, the upper lobe vessels are recruited to distribute a greater volume of blood. In order to carry a greater volume of blood, the upper lobe vessels increase in size.<br clear="left"/> | [[Image:Cephalization.png|left|thumb]][[Cephalization on chest x-ray|Cephalization]] refers to the redistribution of [[blood]] into the [[upper lobe]] [[vessels]]. It has been hypothesized that once the [[hydrostatic pressure]] exceeds 10 mm Hg, then fluid begins to leak into the [[interstitium]] of the [[lung]]. This excess fluid initially compresses the lower lobe vessels, perhaps as a result of gravity. After this, the upper lobe [[vessels]] are recruited to distribute a greater volume of [[blood]]. In order to carry a greater volume of [[blood]], the upper lobe [[vessels]] increase in size.<br clear="left"/> | ||
==Differentiating Cardiogenic Versus Noncardiogenic Pulmonary Edema== | ==Differentiating [[Cardiogenic]] Versus [[Noncardiogenic]] [[Pulmonary Edema]]== | ||
===Cardiogenic Pulmonary Edema=== | ===[[Cardiogenic]] [[Pulmonary Edema]]=== | ||
[[Image:Interstitial edema.png|thumb|left]] Cardiogenic pulmonary edema can be distinguished from noncardiogenic pulmonary edema by the presence of redistribution of blood flow to the upper lobes (increased blood flow to the higher parts of the lung) and interstitial edema. | [[Image:Interstitial edema.png|thumb|left]] [[Cardiogenic]] [[pulmonary edema]] can be distinguished from noncardiogenic [[pulmonary edema]] by the presence of redistribution of [[blood flow]] to the upper lobes (increased blood flow to the higher parts of the lung) and interstitial edema. | ||
<br clear="left"/> | <br clear="left"/> | ||
===Noncardiogenic Pulmonary Edema=== | ===Noncardiogenic Pulmonary Edema=== | ||
[[Image:Pulmonary alveolar edema.png|left|thumb]] In contrast, patchy alveolar infiltrates with air bronchograms are more indicative of noncardiogenic edema. | [[Image:Pulmonary alveolar edema.png|left|thumb]] In contrast, patchy [[alveolar]] infiltrates with [[air bronchograms]] are more indicative of [[noncardiogenic edema]]. | ||
<br clear="left"/> | <br clear="left"/> | ||
==Correlation of Chest X-Ray Findings with Pulmonary Capillary Wedge Pressure== | ==Correlation of [[Chest X-Ray]] Findings with [[Pulmonary Capillary Wedge Pressure]]== | ||
*'''Normal''': 5-10 mm Hg | |||
*'''[[Cephalization]]''': 10-15 mm Hg | |||
*'''[[Kerley B Lines]]''': 15-20 mm Hg | |||
*'''[[Pulmonary Interstitial Edema]]''': 20-25 mm Hg | |||
* '''[[Pulmonary Alveolar Edema]]''': > 25 mm Hg | |||
==Evaluation With [[Cardiac Imaging]] 2022 AHA/ACC/HFSA Heart Failure Guideline (DO NOT EDIT) <ref name="pmid35363500">{{cite journal| author=Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM | display-authors=etal| title=2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. | journal=Circulation | year= 2022 | volume= 145 | issue= 18 | pages= e876-e894 | pmid=35363500 | doi=10.1161/CIR.0000000000001062 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=35363500 }} </ref> == | |||
{|class="wikitable" style="width:80%" | |||
|- | |||
|colspan="1" style="text-align:center; background:LightGreen"| [[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
= | |- | ||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' In [[patients]] with suspected or new-onset [[HF]], or those presenting with acute decompensated [[HF]], a [[chest]] [[X-ray]] should be performed to assess [[heart]] size and [[pulmonary congestion]] and to detect alternative [[cardiac]], [[pulmonary]], and other [[diseases]] that may cause or contribute to the [[patient]]'s [[symptoms]]. <ref name="pmid8945695">{{cite journal| author=Badgett RG, Mulrow CD, Otto PM, Ramírez G| title=How well can the chest radiograph diagnose left ventricular dysfunction? | journal=J Gen Intern Med | year= 1996 | volume= 11 | issue= 10 | pages= 625-34 | pmid=8945695 | doi=10.1007/BF02599031 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8945695 }} </ref><ref name="pmid15006584">{{cite journal| author=Knudsen CW, Omland T, Clopton P, Westheim A, Abraham WT, Storrow AB | display-authors=etal| title=Diagnostic value of B-Type natriuretic peptide and chest radiographic findings in patients with acute dyspnea. | journal=Am J Med | year= 2004 | volume= 116 | issue= 6 | pages= 363-8 | pmid=15006584 | doi=10.1016/j.amjmed.2003.10.028 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15006584 }} [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=&cmd=prlinks&id=15341468 Review in: ACP J Club. 2004 Sep-Oct;141(2):48] </ref>''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-LD]])'' <nowiki>"</nowiki> | |||
= | |} | ||
==Vote on and Suggest Revisions to the Current Guidelines== | ==Vote on and Suggest Revisions to the Current Guidelines== | ||
*[[The Living Guidelines: Diagnosis and Management of Chronic Heart Failure | The CHF Living Guidelines: Vote on current recommendations and suggest revisions to the guidelines]] | *[[The Living Guidelines: Diagnosis and Management of Chronic Heart Failure | The CHF Living Guidelines: Vote on current recommendations and suggest revisions to the guidelines]] | ||
==Guidelines | ==Sources== | ||
*[https://www.ahajournals.org/doi/epub/10.1161/CIR.0000000000001063.full.pdf 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines]<ref name="pmid35363499">{{cite journal |vauthors=Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, Deswal A, Drazner MH, Dunlay SM, Evers LR, Fang JC, Fedson SE, Fonarow GC, Hayek SS, Hernandez AF, Khazanie P, Kittleson MM, Lee CS, Link MS, Milano CA, Nnacheta LC, Sandhu AT, Stevenson LW, Vardeny O, Vest AR, Yancy CW |title=2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines |journal=Circulation |volume=145 |issue=18 |pages=e895–e1032 |date=May 2022 |pmid=35363499 |doi=10.1161/CIR.0000000000001063 |url=}} </ref> | |||
*[http://circ.ahajournals.org/content/112/12/e154.full.pdf The ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult] <ref name="Hunt"> Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B; American College of Cardiology; American Heart Association Task Force on Practice Guidelines; American College of Chest Physicians; International Society for Heart and Lung Transplantation; Heart Rhythm Society. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005 Sep 20; 112(12): e154-235. Epub 2005 Sep 13. PMID 16160202</ref> | *[http://circ.ahajournals.org/content/112/12/e154.full.pdf The ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult] <ref name="Hunt"> Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B; American College of Cardiology; American Heart Association Task Force on Practice Guidelines; American College of Chest Physicians; International Society for Heart and Lung Transplantation; Heart Rhythm Society. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005 Sep 20; 112(12): e154-235. Epub 2005 Sep 13. PMID 16160202</ref> | ||
| Line 65: | Line 80: | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
[[Category:Cardiology]] | |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Intensive care medicine]] | |||
[[Category:Medicine]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Up-To-Date cardiology]] | |||
Latest revision as of 20:46, 22 June 2022
| Resident Survival Guide |
| Congestive Heart Failure Microchapters |
|
Pathophysiology |
|---|
|
Differentiating Congestive heart failure from other Diseases |
|
Diagnosis |
|
Treatment |
|
Medical Therapy: |
|
Surgical Therapy: |
|
ACC/AHA Guideline Recommendations
|
|
Specific Groups: |
|
Congestive heart failure chest x ray On the Web |
|
Directions to Hospitals Treating Congestive heart failure chest x ray |
|
Risk calculators and risk factors for Congestive heart failure chest x ray |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Lakshmi Gopalakrishnan, M.B.B.S. [2] Edzel Lorraine Co, DMD, MD[3]
Overview
Chest x-ray in a patient with heart failure shows cardiomegaly (cardiac enlargement and pulmonary congestion (Kerley B lines, and in some cases pleural effusion).
Chest X Ray
- Since the left ventricle often dilates in the anteroposterior direction, the cardiac silhouette may appear deceptively normal.
- Chest x-ray findings include:
- Kerley B lines or thickening of the interlobular septa
- Peribronchial cuffing
- Thickening of the fissures
- Cephalization
- Increased vascular markings
- Interstitial edema
- Pleural effusions
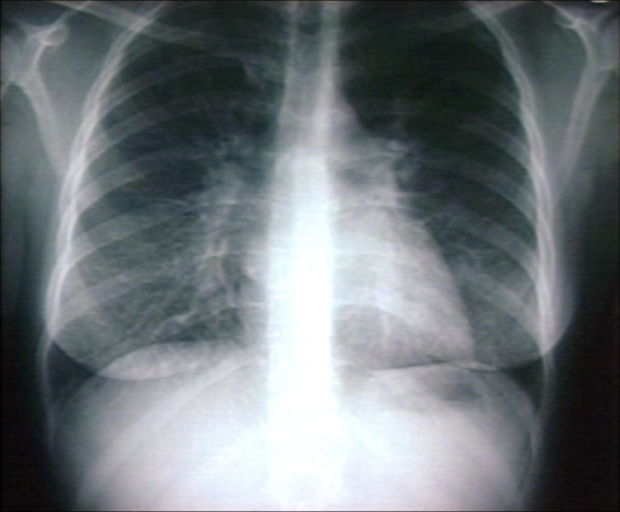
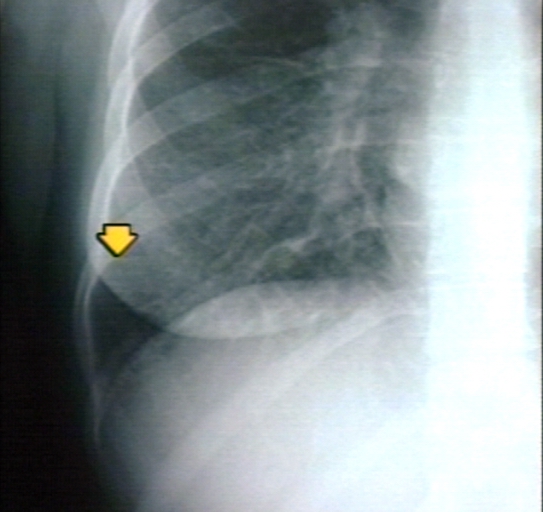
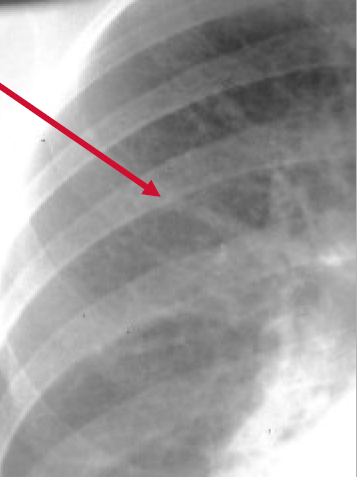
Kerley B Lines
Kerley B lines are short parallel lines at the lung periphery. These lines represent distended interlobular septa, which are usually less than 1 cm in length and parallel to one another at right angles to the pleura. They are located peripherally in contact with the pleura, but are generally absent along fissural surfaces. They may be seen in any zone but are most frequently observed at the lung bases at the costophrenic angles on the PA radiograph, and in the substernal region on lateral radiographs.
-
Plain film: Mitral stenosis, Kerley B lines
-
Plain film: Mitral stenosis, Kerley B lines
-
Plain film: Mitral stenosis, Kerley B lines
Peribronchial Cuffing

Peribronchial cuffing is an abnormality on a chest x-ray whereby the usually thin bronchial walls are thickened and take on a doughnut-like appearance.
Cephalization
Cephalization refers to the redistribution of blood into the upper lobe vessels. It has been hypothesized that once the hydrostatic pressure exceeds 10 mm Hg, then fluid begins to leak into the interstitium of the lung. This excess fluid initially compresses the lower lobe vessels, perhaps as a result of gravity. After this, the upper lobe vessels are recruited to distribute a greater volume of blood. In order to carry a greater volume of blood, the upper lobe vessels increase in size.
Differentiating Cardiogenic Versus Noncardiogenic Pulmonary Edema
Cardiogenic Pulmonary Edema

Cardiogenic pulmonary edema can be distinguished from noncardiogenic pulmonary edema by the presence of redistribution of blood flow to the upper lobes (increased blood flow to the higher parts of the lung) and interstitial edema.
Noncardiogenic Pulmonary Edema

In contrast, patchy alveolar infiltrates with air bronchograms are more indicative of noncardiogenic edema.
Correlation of Chest X-Ray Findings with Pulmonary Capillary Wedge Pressure
- Normal: 5-10 mm Hg
- Cephalization: 10-15 mm Hg
- Kerley B Lines: 15-20 mm Hg
- Pulmonary Interstitial Edema: 20-25 mm Hg
- Pulmonary Alveolar Edema: > 25 mm Hg
Evaluation With Cardiac Imaging 2022 AHA/ACC/HFSA Heart Failure Guideline (DO NOT EDIT) [1]
| Class I |
| "1. In patients with suspected or new-onset HF, or those presenting with acute decompensated HF, a chest X-ray should be performed to assess heart size and pulmonary congestion and to detect alternative cardiac, pulmonary, and other diseases that may cause or contribute to the patient's symptoms. [2][3](Level of Evidence: C-LD) " |
Vote on and Suggest Revisions to the Current Guidelines
Sources
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[4]
- The ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult [5]
- 2009 focused update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation [6]
References
- ↑ Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM; et al. (2022). "2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines". Circulation. 145 (18): e876–e894. doi:10.1161/CIR.0000000000001062. PMID 35363500 Check
|pmid=value (help). - ↑ Badgett RG, Mulrow CD, Otto PM, Ramírez G (1996). "How well can the chest radiograph diagnose left ventricular dysfunction?". J Gen Intern Med. 11 (10): 625–34. doi:10.1007/BF02599031. PMID 8945695.
- ↑ Knudsen CW, Omland T, Clopton P, Westheim A, Abraham WT, Storrow AB; et al. (2004). "Diagnostic value of B-Type natriuretic peptide and chest radiographic findings in patients with acute dyspnea". Am J Med. 116 (6): 363–8. doi:10.1016/j.amjmed.2003.10.028. PMID 15006584. Review in: ACP J Club. 2004 Sep-Oct;141(2):48
- ↑ Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, Deswal A, Drazner MH, Dunlay SM, Evers LR, Fang JC, Fedson SE, Fonarow GC, Hayek SS, Hernandez AF, Khazanie P, Kittleson MM, Lee CS, Link MS, Milano CA, Nnacheta LC, Sandhu AT, Stevenson LW, Vardeny O, Vest AR, Yancy CW (May 2022). "2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines". Circulation. 145 (18): e895–e1032. doi:10.1161/CIR.0000000000001063. PMID 35363499 Check
|pmid=value (help). - ↑ Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B; American College of Cardiology; American Heart Association Task Force on Practice Guidelines; American College of Chest Physicians; International Society for Heart and Lung Transplantation; Heart Rhythm Society. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005 Sep 20; 112(12): e154-235. Epub 2005 Sep 13. PMID 16160202
- ↑ Jessup M, Abraham WT, Casey DE, Feldman AM, Francis GS, Ganiats TG et al. (2009) 2009 focused update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation 119 (14):1977-2016. DOI:10.1161/CIRCULATIONAHA.109.192064 PMID: 19324967