COVID-19-associated seizure: Difference between revisions
| Line 124: | Line 124: | ||
===Laboratory Findings=== | ===Laboratory Findings=== | ||
[[Postictal]] levels of the following may be elevated: | [[Postictal]] levels of the following may be elevated in a patient with seizures: | ||
* Prolactin (within 20 minutes after a convulsive event) | * Prolactin (within 20 minutes after a convulsive event) | ||
* Lactate (within 1 to 2 hours) | * Lactate (within 1 to 2 hours) | ||
* Ammonia (within several hours) | * Ammonia (within several hours) | ||
* Creatine kinase (especially 24 to 48 hours postictally) | * Creatine kinase (especially 24 to 48 hours postictally) | ||
* To view the laboratory findings on COVID-19, [[COVID-19 laboratory findings|click here]]. | |||
===Electrocardiogram=== | ===Electrocardiogram=== | ||
Revision as of 05:36, 11 July 2020
|
COVID-19 Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
COVID-19-associated seizure On the Web |
|
American Roentgen Ray Society Images of COVID-19-associated seizure |
|
Risk calculators and risk factors for COVID-19-associated seizure |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mandana Safakhah, MD[2]
Synonyms and keywords:
Overview
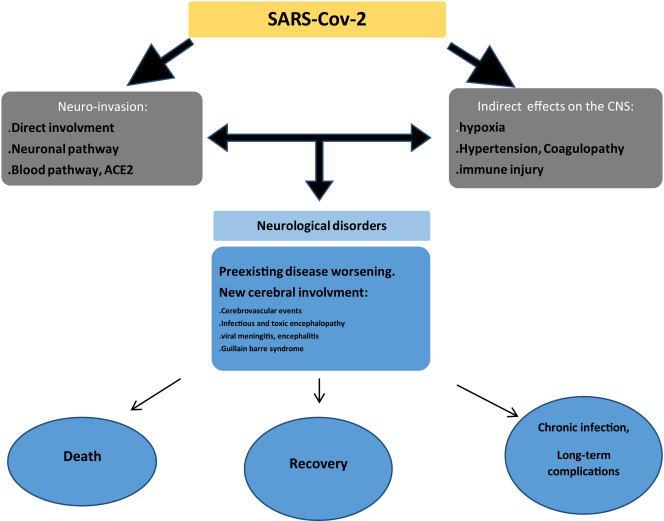
Coronaviruses impacts are not always restricted to respiratory system and they have potential for neuroinvasion under specific circumstances. Neurological manifestations such as dizziness,headache ,anosmia as well as case reports with encephalitis ,stroke,epileptic seizures associated with covid-19, have been reported.
Historical Perspective
- two male patients, non-epileptic were hospitalised with covid-19 signs and symptoms, March 2020 ,Ohio, U.S.A. During their hospital stay they developed encephalopathy and seizures, controlled by levetiracetam
- A women with the past medical history of seizure following herpetic encephalitis ,presented with a sudden focal myoclonus and positive test for covid 19 in Italy, 23rd of april 2020.[1]
- Also, a cohort multicentre study was done in China, April 2020, demonstrating that COVID 19 doesn't increase the risk of symptomatic seizure in patients hospitalized with the acute respiratory phase of COVID 19.Although ,some seizure-like reactions are seen because of acute reaction to stress or hypocalcemia .[2]
Classification
There isn't any established classification for covid-19 associated seizure.
Pathophysiology
- Neurological complications caused by COVID-19 are through direct or indirect pathways. This includes hematogenous pathway, neuronal retrograde dissemination through olfactory bulb, entry into to glial cells and neurons via ACE2 receptor and impairment of gas exchange in lungs leading to anemia, hence increasing anaerobic metabolites in brain resulting in cellular and interstitial edema [3]
- Seizures in a patient with COVID-19 may be due to primary virus infection or due to reactivation of the latent virus.
- Infiltration of the brain tissue by the virus and subsequent production of toxins by the virus is one of the several mechanisms that can cause seizures in a COVID-19 patient. [4]
- Production of inflammatory mediators by the brain may also trigger seizures.
- Inflammatory cytokines that are released as a result of inflammatory cascade provoked by COVID-19 include interleukin 2,6,7, and 10, TNF-α and granulocyte colony-stimulating factor. Consequently, activation of glutamate receptors by the cytokines causes neuronal hyperexcitability and development of seizures. [4]
Causes
The aetiology of seizure regardless whether it is covid-19 or not ,is divided into two categories:
- 'Provoked seizures : these seizures usually have a temporary trigger such as CNS infection,electrolytes disturbance, withdrawal syndrome,sepsis ,fever, sleep deprivation and stroke.
- Unprovoked seizures: In this catrgory ,there isn't any obvious cause or precipitating factor .[5]
Differentiating COVID-19-associated seizure from other Diseases
Apart from the viral cause of the seizure, the differential diagnosis for this disease is usually based on the presenting symptoms as below:
- Generalized convulsive movements:Epilepsy-syncope with secondary jerking movement-Involuntary movement disorders and other neurological conditions
- Drop attack:Epilepsy-Cardiac-Brainstem abnormalities-vertebrobasilar ischemia-Idiopathic
- Transient focal motor and sensory attack :tics-tonic spasms of multiple
- Facial muscles and eye movement:partial seizures-movement disorder-Other neurological conditions.[6]
Epidemiology and Demographics
By now there isn't any sufficient evidence for demographic and epidemiologic data about covid- 19 associated seizure.
Risk Factors
There are no established risk factors for covid-19 associated seizure.
Screening
There is insufficient evidence to recommend routine screening for covid-19 associated seizure.
Natural History, Complications, and Prognosis
The global case fatality rate is currently estimated to be 4.6% according to WHO , 9th,June.[7] Also neurological complications of covid-19 .The covid-19 fatality rate depends on several factors such as:
- patient demographics
- availability of health care
- test limitation
Also , the more comorbidities the patient has ,the poorer covid-19 clinical output. Some of the prognostic factor of covid-19 are listed as below:
- Above 65 years old
- smoking
- male sex
- elevated inflammatory markers
- elevated D-Dimer
- elevated interleukin 6
- thrombocytopenia
- high neutrophil to lymphocyte ratio
- higher acute physiology and chronic health evaluation score.[8]
Diagnosis
Diagnostic Study of Choice
The diagnosis of COVID-19-associated seizure is made through:
Other diagnostic tests include:
- CT scan brain
- MRI brain
- Blood test
- Lumbar puncture
- Toxicology screening
History and Symptoms
History
- Neurotropism is one common feature of coronaviruses[10][11].
- COVID-19 document CNS manifestations in 25% of the patients, headache (13%), dizziness (17%), impaired consciousness (8%), acute cerebrovascular problems (3%), ataxia (0.5), and seizures (0.5%)[12].
Symptoms
- General symptoms or warning signs of a seizure can include:
- Staring
- Jerking movements of the arms and legs
- Stiffening of the body
- Loss of consciousness
- Breathing problems or stopping breathing
- Loss of bowel or bladder control
- Falling suddenly for no apparent reason, especially when associated with loss of consciousness
- Not responding to noise or words for brief periods
- Appearing confused or in a haze
- Nodding your head rhythmically, when associated with loss of awareness or loss of consciousness
- Periods of rapid eye blinking and staring
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Laboratory Findings
Postictal levels of the following may be elevated in a patient with seizures:
- Prolactin (within 20 minutes after a convulsive event)
- Lactate (within 1 to 2 hours)
- Ammonia (within several hours)
- Creatine kinase (especially 24 to 48 hours postictally)
- To view the laboratory findings on COVID-19, click here.
Electrocardiogram
- There are no typical ECG findings associated with seizures in a COVID-19 patient.
- To view the electrocardiogram findings on COVID-19, click here.
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
- Development of seizures in a COVID-19 patient requires urgent treatment.
- After the cause of seizure is determined, medical therapy should be aimed at treating the cause immediately (for example, hypoxia, fever, metabolic imbalance).
- Anti-seizure medication (ASM) is often necessary.
- For a single seizure less than 5 min rescue treatment with benzodiazepine is not needed. Intravenous ASM are used with caution in COVID-19 patients due to the adverse effects (e.g., Phenytoin, Phenobarbital and Lacosamide in respiratory and cardiac problems) and drug interactions (e.g., Carbamazepine, Phenytoin, Phenobarbital and Valproic acid). [13]
- Brivaracetam and Levetiracetam have less adverse effects and drug interactions. [13]
- In patients with more than one seizure (either shorter or longer than 5 min) and in status epilepticus rescue treatment with benzodiazepines in addition to ASM is needed. [13]
Surgery
Surgical intervention is not recommended for the management of COVID-19 associated seizure.
Primary Prevention
There are no established measures for the primary prevention of [disease name].
OR
There are no available vaccines against [disease name].
OR
Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
OR
[Vaccine name] vaccine is recommended for [patient population] to prevent [disease name]. Other primary prevention strategies include [strategy 1], [strategy 2], and [strategy 3].
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
OR
Effective measures for the secondary prevention of [disease name] include [strategy 1], [strategy 2], and [strategy 3].
References
- ↑ {{https://www.seizure-journal.com/article/S1059-1311(20)30115-1/fulltext}}
- ↑ {{https://onlinelibrary.wiley.com/doi/full/10.1111/epi.16524}}
- ↑ {{https://pubmed.ncbi.nlm.nih.gov/32458193/}}
- ↑ 4.0 4.1 Karimi, Narges; Sharifi Razavi, Athena; Rouhani, Nima (2020). "Frequent Convulsive Seizures in an Adult Patient with COVID-19: A Case Report". Iranian Red Crescent Medical Journal. 22 (3). doi:10.5812/ircmj.102828. ISSN 2074-1804.
- ↑ {{https://www.ncbi.nlm.nih.gov/books/NBK430765/}}
- ↑ {{https://www.nice.org.uk/guidance/CG20/documents/appendix-a-a-differential-diagnosis-first-consultation2}}
- ↑ Template:Https://bestpractice.bmj.com/topics/en-gb/3000168/prognosis
- ↑ Template:Https://bestpractice.bmj.com/topics/en-gb/3000168/prognosis
- ↑ Haines S, Caccamo A, Chan F, Galaso G, Catinchi A, Gupta PK (2020). "Practical Considerations When Performing Neurodiagnostic Studies on Patients with COVID-19 and Other Highly Virulent Diseases". Neurodiagn J. 60 (2): 78–95. doi:10.1080/21646821.2020.1756132. PMC 7212538 Check
|pmc=value (help). PMID 32374647 Check|pmid=value (help). - ↑ Bohmwald K, Gálvez NMS, Ríos M, Kalergis AM (2018). "Neurologic Alterations Due to Respiratory Virus Infections". Front Cell Neurosci. 12: 386. doi:10.3389/fncel.2018.00386. PMC 6212673. PMID 30416428.
- ↑ Li YC, Bai WZ, Hashikawa T (2020). "The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients". J Med Virol. 92 (6): 552–555. doi:10.1002/jmv.25728. PMC 7228394 Check
|pmc=value (help). PMID 32104915 Check|pmid=value (help). - ↑ Montalvan V, Lee J, Bueso T, De Toledo J, Rivas K (2020). "Neurological manifestations of COVID-19 and other coronavirus infections: A systematic review". Clin Neurol Neurosurg. 194: 105921. doi:10.1016/j.clineuro.2020.105921. PMC 7227498 Check
|pmc=value (help). PMID 32422545 Check|pmid=value (help). - ↑ 13.0 13.1 13.2 Asadi-Pooya AA (July 2020). "Seizures associated with coronavirus infections". Seizure. 79: 49–52. doi:10.1016/j.seizure.2020.05.005. PMC 7212943 Check
|pmc=value (help). PMID 32416567 Check|pmid=value (help).