COVID-19-associated seizure: Difference between revisions
No edit summary |
No edit summary |
||
| (17 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{SI}} | ||
{{CMG}}; {{AE}} {{Mandana.Sa}} [[User:Tayebah Chaudhry|Tayebah Chaudhry]][mailto:dr.thch@yahoo.com] {{sali}} | {{CMG}}; {{AE}} {{Mandana.Sa}} [[User:Tayebah Chaudhry|Tayebah Chaudhry]][mailto:dr.thch@yahoo.com], {{Fs}}, {{sali}} | ||
{{SK}} | {{SK}} | ||
| Line 13: | Line 13: | ||
*First case of seizure in [[COVID-19]] patient was a result of [[meningitis]]/[[encephalitis]] caused by [[SARS-CoV-2|SARS-CoV2]] and documented by Moriguchi et al in late February 2020 <ref name="pmid32251791">{{cite journal |vauthors=Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Ueno M, Sakata H, Kondo K, Myose N, Nakao A, Takeda M, Haro H, Inoue O, Suzuki-Inoue K, Kubokawa K, Ogihara S, Sasaki T, Kinouchi H, Kojin H, Ito M, Onishi H, Shimizu T, Sasaki Y, Enomoto N, Ishihara H, Furuya S, Yamamoto T, Shimada S |title=A first case of meningitis/encephalitis associated with SARS-Coronavirus-2 |journal=Int. J. Infect. Dis. |volume=94 |issue= |pages=55–58 |date=May 2020 |pmid=32251791 |pmc=7195378 |doi=10.1016/j.ijid.2020.03.062 |url=}}</ref>. | *First case of seizure in [[COVID-19]] patient was a result of [[meningitis]]/[[encephalitis]] caused by [[SARS-CoV-2|SARS-CoV2]] and documented by Moriguchi et al in late February 2020 <ref name="pmid32251791">{{cite journal |vauthors=Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Ueno M, Sakata H, Kondo K, Myose N, Nakao A, Takeda M, Haro H, Inoue O, Suzuki-Inoue K, Kubokawa K, Ogihara S, Sasaki T, Kinouchi H, Kojin H, Ito M, Onishi H, Shimizu T, Sasaki Y, Enomoto N, Ishihara H, Furuya S, Yamamoto T, Shimada S |title=A first case of meningitis/encephalitis associated with SARS-Coronavirus-2 |journal=Int. J. Infect. Dis. |volume=94 |issue= |pages=55–58 |date=May 2020 |pmid=32251791 |pmc=7195378 |doi=10.1016/j.ijid.2020.03.062 |url=}}</ref>. | ||
* After that, more cases were reported with acute [[Seizure|seizures]] as a complication of COVID-19.<ref name="HepburnMullaguri2020">{{citejournal|last1=Hepburn|first1=Madihah|last2=Mullaguri|first2=Naresh|last3=George|first3=Pravin|last4=Hantus|first4=Stephen|last5=Punia|first5=Vineet|last6=Bhimraj|first6=Adarsh|last7=Newey|first7=Christopher R.|title=Acute Symptomatic Seizures in Critically Ill Patients with COVID-19: Is There an Association?|journal=Neurocritical Care|year=2020|issn=1541-6933|doi=10.1007/s12028-020-01006-1}}</ref><ref><nowiki>{{</nowiki>https://www.sciencedirect.com/science/article/pii/S1059131120301151<nowiki>}}</nowiki></ref> | *After that, more cases were reported with acute [[Seizure|seizures]] as a complication of COVID-19.<ref name="HepburnMullaguri2020">{{citejournal|last1=Hepburn|first1=Madihah|last2=Mullaguri|first2=Naresh|last3=George|first3=Pravin|last4=Hantus|first4=Stephen|last5=Punia|first5=Vineet|last6=Bhimraj|first6=Adarsh|last7=Newey|first7=Christopher R.|title=Acute Symptomatic Seizures in Critically Ill Patients with COVID-19: Is There an Association?|journal=Neurocritical Care|year=2020|issn=1541-6933|doi=10.1007/s12028-020-01006-1}}</ref><ref><nowiki>{{</nowiki>https://www.sciencedirect.com/science/article/pii/S1059131120301151<nowiki>}}</nowiki></ref> | ||
* In early February 2020, seizurelike activity was reported in two COVID-19 patients but the cause was acute [[anxiety]] disorder and [[electrolyte imbalance]] instead of viral damage by [[SARS-Cov-2]]<ref><nowiki>{{</nowiki>https://onlinelibrary.wiley.com/doi/full/10.1111/epi.16524<nowiki>}}</nowiki></ref> | *In early February 2020, seizurelike activity was reported in two COVID-19 patients but the cause was acute [[anxiety]] disorder and [[electrolyte imbalance]] instead of viral damage by [[SARS-Cov-2]]<ref><nowiki>{{</nowiki>https://onlinelibrary.wiley.com/doi/full/10.1111/epi.16524<nowiki>}}</nowiki></ref> | ||
*To view the historical perspective of COVID-19, [[COVID-19 historical perspective|click here]]. | *To view the historical perspective of COVID-19, [[COVID-19 historical perspective|click here]]. | ||
| Line 22: | Line 22: | ||
==Pathophysiology== | ==Pathophysiology== | ||
* [[Neurological]] complications caused by [[COVID-19]] are through direct or indirect pathways. | |||
*[[Neurological]] complications caused by [[COVID-19]] are through direct or indirect pathways. | |||
*This includes [[hematogenous]] pathway, [[neuronal]] [[retrograde]] dissemination through [[olfactory bulb]], entry into to [[glial]] cells and [[neurons]] via [[ACE2]] receptor and impairment of [[gas]] exchange in [[lung]]s leading to [[anemia]], hence increasing [[anaerobic]] metabolites in [[brain]] resulting in [[cellular]] and interstitial [[edema]] <ref><nowiki>{{</nowiki>https://pubmed.ncbi.nlm.nih.gov/32458193/<nowiki>}}</nowiki></ref> | *This includes [[hematogenous]] pathway, [[neuronal]] [[retrograde]] dissemination through [[olfactory bulb]], entry into to [[glial]] cells and [[neurons]] via [[ACE2]] receptor and impairment of [[gas]] exchange in [[lung]]s leading to [[anemia]], hence increasing [[anaerobic]] metabolites in [[brain]] resulting in [[cellular]] and interstitial [[edema]] <ref><nowiki>{{</nowiki>https://pubmed.ncbi.nlm.nih.gov/32458193/<nowiki>}}</nowiki></ref> | ||
* [[Seizures]] in a patient with [[COVID-19]] may be due to primary [[virus]] [[infection]] or due to reactivation of the latent [[virus]]. | *[[Seizures]] in a patient with [[COVID-19]] may be due to primary [[virus]] [[infection]] or due to reactivation of the latent [[virus]]. | ||
* Infiltration of the [[brain]] [[tissue]] by the [[virus]] and subsequent production of [[toxins]] by the [[virus]] is one of the several mechanisms that can cause [[seizures]] in a [[COVID-19]] [[patient]]. <ref name="KarimiSharifi Razavi2020">{{cite journal|last1=Karimi|first1=Narges|last2=Sharifi Razavi|first2=Athena|last3=Rouhani|first3=Nima|title=Frequent Convulsive Seizures in an Adult Patient with COVID-19: A Case Report|journal=Iranian Red Crescent Medical Journal|volume=22|issue=3|year=2020|issn=2074-1804|doi=10.5812/ircmj.102828}}</ref> | *Infiltration of the [[brain]] [[tissue]] by the [[virus]] and subsequent production of [[toxins]] by the [[virus]] is one of the several mechanisms that can cause [[seizures]] in a [[COVID-19]] [[patient]]. <ref name="KarimiSharifi Razavi2020">{{cite journal|last1=Karimi|first1=Narges|last2=Sharifi Razavi|first2=Athena|last3=Rouhani|first3=Nima|title=Frequent Convulsive Seizures in an Adult Patient with COVID-19: A Case Report|journal=Iranian Red Crescent Medical Journal|volume=22|issue=3|year=2020|issn=2074-1804|doi=10.5812/ircmj.102828}}</ref> | ||
* Production of [[inflammatory]] mediators by the brain may also trigger [[seizures]]. | *Production of [[inflammatory]] mediators by the brain may also trigger [[seizures]]. | ||
* [[Inflammatory]] [[cytokines]] that are released as a result of [[inflammatory cascade]] provoked by [[COVID-19]] include [[interleukin]] 2,6,7, and 10, [[TNF-α]] and [[granulocyte colony-stimulating factor]]. Consequently, activation of [[glutamate receptors]] by the cytokines causes [[neuronal]] [[hyperexcitability]] and development of [[seizures]]. <ref name="KarimiSharifi Razavi2020">{{cite journal|last1=Karimi|first1=Narges|last2=Sharifi Razavi|first2=Athena|last3=Rouhani|first3=Nima|title=Frequent Convulsive Seizures in an Adult Patient with COVID-19: A Case Report|journal=Iranian Red Crescent Medical Journal|volume=22|issue=3|year=2020|issn=2074-1804|doi=10.5812/ircmj.102828}}</ref> | *[[Inflammatory]] [[cytokines]] that are released as a result of [[inflammatory cascade]] provoked by [[COVID-19]] include [[interleukin]] 2,6,7, and 10, [[TNF-α]] and [[granulocyte colony-stimulating factor]]. Consequently, activation of [[glutamate receptors]] by the cytokines causes [[neuronal]] [[hyperexcitability]] and development of [[seizures]]. <ref name="KarimiSharifi Razavi2020">{{cite journal|last1=Karimi|first1=Narges|last2=Sharifi Razavi|first2=Athena|last3=Rouhani|first3=Nima|title=Frequent Convulsive Seizures in an Adult Patient with COVID-19: A Case Report|journal=Iranian Red Crescent Medical Journal|volume=22|issue=3|year=2020|issn=2074-1804|doi=10.5812/ircmj.102828}}</ref> | ||
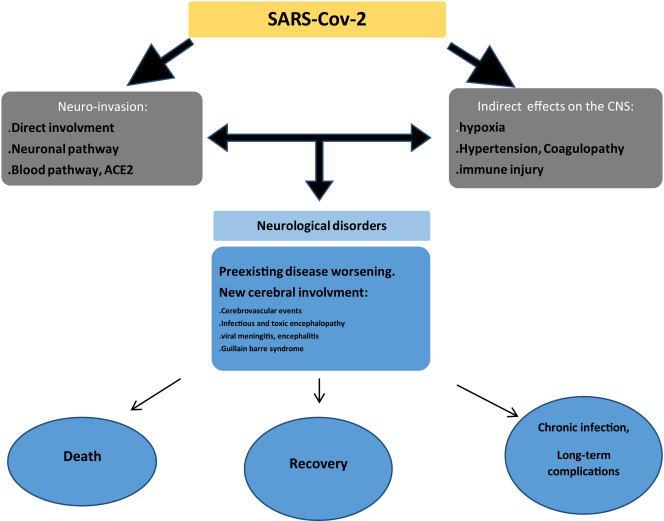
[[Image:covid 19 seizure.jpeg|500px|thumb|center|Pathophysiology]] | |||
[[Image:covid 19 seizure.jpeg|500px|thumb|center|Pathophysiology <ref name="AbboudAbboud2020">{{cite journal|last1=Abboud|first1=Hilal|last2=Abboud|first2=Fatima Zahra|last3=Kharbouch|first3=Hanane|last4=Arkha|first4=Yasser|last5=El Abbadi|first5=Najia|last6=El Ouahabi|first6=Abdessamad|title=COVID-19 and SARS-Cov-2 Infection: Pathophysiology and Clinical Effects on the Nervous System|journal=World Neurosurgery|volume=140|year=2020|pages=49–53|issn=18788750|doi=10.1016/j.wneu.2020.05.193}}</ref>]] | |||
==Causes== | ==Causes== | ||
* Cause of COVID-19-associated seizure is viral infection by [[SARS-CoV-2]] and its consequences which include:<ref name="pmid32416567">{{cite journal |vauthors=Asadi-Pooya AA |title=Seizures associated with coronavirus infections |journal=Seizure |volume=79 |issue= |pages=49–52 |date=July 2020 |pmid=32416567 |pmc=7212943 |doi=10.1016/j.seizure.2020.05.005 |url=}}</ref> | *Cause of COVID-19-associated seizure is viral infection by [[SARS-CoV-2]] and its consequences which include:<ref name="pmid32416567">{{cite journal |vauthors=Asadi-Pooya AA |title=Seizures associated with coronavirus infections |journal=Seizure |volume=79 |issue= |pages=49–52 |date=July 2020 |pmid=32416567 |pmc=7212943 |doi=10.1016/j.seizure.2020.05.005 |url=}}</ref> | ||
* [[Hypoxia]] | **[[Hypoxia]] | ||
* [[Metabolic]] derangement | **[[Metabolic]] derangement | ||
* [[Organ failure]] | **[[Organ failure]] | ||
* [[Cerebral]] damage.<ref><nowiki>{{</nowiki>https://www.ncbi.nlm.nih.gov/books/NBK430765/<nowiki>}}</nowiki></ref> | **[[Cerebral]] damage.<ref><nowiki>{{</nowiki>https://www.ncbi.nlm.nih.gov/books/NBK430765/<nowiki>}}</nowiki></ref> | ||
* To view causes of COVID-19, [[COVID-19 causes|click here]]. | **To view causes of COVID-19, [[COVID-19 causes|click here]]. | ||
==Differentiating COVID-19-associated seizure from other Diseases== | ==Differentiating COVID-19-associated seizure from other Diseases== | ||
* | *For further information about the differential diagnosis, [[COVID-19-associated seizure differential diagnosis|click here]]. | ||
*To view the differential diagnosis of COVID-19, [[COVID-19 differential diagnosis|click here]]. | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
* More data is required to comment on [[epidemiology]] and [[demographics]] of [[COVID-19]]-associated [[seizure]]. | *More data is required to comment on [[epidemiology]] and [[demographics]] of [[COVID-19]]-associated [[seizure]]. | ||
* One study, specifically investigated the neurological manifestations of [[COVID-19]] and documented [[CNS]] manifestations in 25% of the patients ([[headache]] (13%), [[dizziness]] (17%), impaired [[consciousness]] (8%), acute [[cerebrovascular]] problems (3%), [[ataxia]] (0.5), and [[seizures]] (0.5%)]<ref name="MaoJin2020">{{cite journal|last1=Mao|first1=Ling|last2=Jin|first2=Huijuan|last3=Wang|first3=Mengdie|last4=Hu|first4=Yu|last5=Chen|first5=Shengcai|last6=He|first6=Quanwei|last7=Chang|first7=Jiang|last8=Hong|first8=Candong|last9=Zhou|first9=Yifan|last10=Wang|first10=David|last11=Miao|first11=Xiaoping|last12=Li|first12=Yanan|last13=Hu|first13=Bo|title=Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China|journal=JAMA Neurology|volume=77|issue=6|year=2020|pages=683|issn=2168-6149|doi=10.1001/jamaneurol.2020.1127}}</ref> | *One study, specifically investigated the neurological manifestations of [[COVID-19]] and documented [[CNS]] manifestations in 25% of the patients ([[headache]] (13%), [[dizziness]] (17%), impaired [[consciousness]] (8%), acute [[cerebrovascular]] problems (3%), [[ataxia]] (0.5), and [[seizures]] (0.5%)]<ref name="MaoJin2020">{{cite journal|last1=Mao|first1=Ling|last2=Jin|first2=Huijuan|last3=Wang|first3=Mengdie|last4=Hu|first4=Yu|last5=Chen|first5=Shengcai|last6=He|first6=Quanwei|last7=Chang|first7=Jiang|last8=Hong|first8=Candong|last9=Zhou|first9=Yifan|last10=Wang|first10=David|last11=Miao|first11=Xiaoping|last12=Li|first12=Yanan|last13=Hu|first13=Bo|title=Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China|journal=JAMA Neurology|volume=77|issue=6|year=2020|pages=683|issn=2168-6149|doi=10.1001/jamaneurol.2020.1127}}</ref> | ||
==Risk Factors== | ==Risk Factors== | ||
* Several risk factors of [[seizure]] in [[COVID-19]] patients were considered in a multicenter [[restrospective]] study from Jan 18th to FEb 18th, 2020 in China.<ref><nowiki>{{</nowiki>https://onlinelibrary.wiley.com/doi/full/10.1111/epi.16524<nowiki>}}</nowiki></ref> | |||
* [[Risk factor]]s that were studied include acute [[cerebrovascular disease]], [[traumatic brain injury]] (TBI), [[central nervous system]] (CNS) [[infection]], [[shock]], [[hypoxia]], severe [[metabolic disturbance]], [[multiple‐organ dysfunction syndrome]], [[sepsis]], and exposure to drugs or [[toxic]] substances. | *Several risk factors of [[seizure]] in [[COVID-19]] patients were considered in a multicenter [[restrospective]] study from Jan 18th to FEb 18th, 2020 in China.<ref><nowiki>{{</nowiki>https://onlinelibrary.wiley.com/doi/full/10.1111/epi.16524<nowiki>}}</nowiki></ref> | ||
* According to the study, [[hypoxia]] and [[imipenem]] were shown to be important risk factors, among several others, for [[seizure]] in a [[COVID-19]] patient. | *[[Risk factor]]s that were studied include acute [[cerebrovascular disease]], [[traumatic brain injury]] (TBI), [[central nervous system]] (CNS) [[infection]], [[shock]], [[hypoxia]], severe [[metabolic disturbance]], [[multiple‐organ dysfunction syndrome]], [[sepsis]], and exposure to drugs or [[toxic]] substances. | ||
*According to the study, [[hypoxia]] and [[imipenem]] were shown to be important risk factors, among several others, for [[seizure]] in a [[COVID-19]] patient. | |||
*To view the risk factors of COVID-19, [[COVID-19 risk factors|click here]]. | *To view the risk factors of COVID-19, [[COVID-19 risk factors|click here]]. | ||
==Screening== | ==Screening== | ||
There is insufficient evidence to recommend routine screening for [[COVID-19]] associated [[seizure]]. | |||
*There is insufficient evidence to recommend routine screening for [[COVID-19]] associated [[seizure]]. | |||
==Natural History, Complications, and Prognosis== | ==Natural History, Complications, and Prognosis== | ||
'''Natural History''' | '''Natural History''' | ||
* [[Seizure]] activity in a patient with or without [[COVID-19]] usually lasts for a few seconds to less than 5 minutes with return to normal after the [[seizure]] episode. | |||
* If [[seizure]] episode lasts for more than 5 minutes it is called [[status epilepticus]]. | *[[Seizure]] activity in a patient with or without [[COVID-19]] usually lasts for a few seconds to less than 5 minutes with return to normal after the [[seizure]] episode. | ||
* This is followed by a period of [[confusion]], called [[postictal]] | *If [[seizure]] episode lasts for more than 5 minutes it is called [[status epilepticus]]. | ||
*This is followed by a period of [[confusion]], called [[Postictal state|postictal period]] that can last 3-15 minutes and sometimes hours. | |||
'''Complications''' | '''Complications''' | ||
Complications of seizure include: | *Complications of COVID-19-associated seizure include: | ||
* [[Headache]] | **[[Headache]] | ||
* [[Tiredness]] | **[[Tiredness]] | ||
* Difficulty [[speaking]] | **Difficulty [[speaking]] | ||
* [[Difficulty breathing]] (due to blockage of airway) | **[[Difficulty breathing]] (due to blockage of airway) | ||
* Abnormal behavior | **Abnormal behavior | ||
* [[Psychosis]] | **[[Psychosis]] | ||
* Injury to [[tongue]] due to [[bite]] during [[seizure]] activity | **Injury to [[tongue]] due to [[bite]] during [[seizure]] activity | ||
* [[Trauma]] due to sudden [[fall]] and/or [[loss of consciousness]] | **[[Trauma]] due to sudden [[fall]] and/or [[loss of consciousness]] | ||
'''Prognosis''' | '''Prognosis''' | ||
* In general, after the first seizure, subsequent seizure episodes can be predicted using [[EEG]] and [[brain imaging]].<ref name="pmid22963022">{{cite journal |vauthors=Wilden JA, Cohen-Gadol AA |title=Evaluation of first nonfebrile seizures |journal=Am Fam Physician |volume=86 |issue=4 |pages=334–40 |date=August 2012 |pmid=22963022 |doi= |url=}}</ref> | |||
* [[Prognosis]] of seizure in a [[COVID-19]] patient is not known. However, if left untreated, [[seizure]] caused by acute brain event is known to have low risk of recurrence but higher risk of death compared to those with [[epilepsy]]. <ref name="pmid8965090">{{cite journal |vauthors=Sander JW, Shorvon SD |title=Epidemiology of the epilepsies |journal=J. Neurol. Neurosurg. Psychiatry |volume=61 |issue=5 |pages=433–43 |date=November 1996 |pmid=8965090 |pmc=1074036 |doi=10.1136/jnnp.61.5.433 |url=}}</ref> | *In general, after the first [[seizure]], subsequent [[seizure]] episodes can be predicted using [[EEG]] and [[brain imaging]].<ref name="pmid22963022">{{cite journal |vauthors=Wilden JA, Cohen-Gadol AA |title=Evaluation of first nonfebrile seizures |journal=Am Fam Physician |volume=86 |issue=4 |pages=334–40 |date=August 2012 |pmid=22963022 |doi= |url=}}</ref> | ||
*[[Prognosis]] of seizure in a [[COVID-19]] patient is not known. | |||
*However, if left untreated, [[seizure]] caused by acute brain event is known to have low risk of recurrence but higher risk of death compared to those with [[epilepsy]]. <ref name="pmid8965090">{{cite journal |vauthors=Sander JW, Shorvon SD |title=Epidemiology of the epilepsies |journal=J. Neurol. Neurosurg. Psychiatry |volume=61 |issue=5 |pages=433–43 |date=November 1996 |pmid=8965090 |pmc=1074036 |doi=10.1136/jnnp.61.5.433 |url=}}</ref> | |||
==Diagnosis== | ==Diagnosis== | ||
===Diagnostic Study of Choice=== | ===Diagnostic Study of Choice=== | ||
The | *The diagnosis of COVID-19-associated seizure is made through [[Electroencephalography|electroencephalogram]] ([[EEG]], brain waive activity).<ref name="pmid32374647">{{cite journal| author=Haines S, Caccamo A, Chan F, Galaso G, Catinchi A, Gupta PK| title=Practical Considerations When Performing Neurodiagnostic Studies on Patients with COVID-19 and Other Highly Virulent Diseases. | journal=Neurodiagn J | year= 2020 | volume= 60 | issue= 2 | pages= 78-95 | pmid=32374647 | doi=10.1080/21646821.2020.1756132 | pmc=7212538 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32374647 }} </ref> | ||
Other diagnostic tests include: | *Other diagnostic tests include: | ||
**[[CT scan]] brain | |||
**[[MRI]] brain | |||
**Blood test | |||
**[[Lumbar puncture]] | |||
**[[Toxicology]] screening | |||
===Symptoms=== | |||
'''Common symptoms:''' | |||
*[[Staring]] | *[[Staring]] | ||
*[[Jerking]] movements of the [[arms]] and [[legs]] | *[[Jerking]] movements of the [[Arm|arms]] and [[legs]] | ||
*Stiffening of the [[body]] | *Stiffening of the [[body]] | ||
*Loss of [[consciousness]] | *Loss of [[consciousness]] | ||
*[[Breathing]] problems | *[[Breathing]] problems | ||
===== Loss of [[bowel]] or [[bladder]] control ===== | |||
*Falling suddenly for no apparent reason, especially when associated with [[loss of consciousness]] | *Falling suddenly for no apparent reason, especially when associated with [[loss of consciousness]] | ||
*Not responding to [[noise]] or words for brief periods | *Not responding to [[noise]] or words for brief periods | ||
*Appearing confused or in a haze | *Appearing confused or in a haze | ||
'''Less common symptoms:''' | |||
*Nodding of [[head]] rhythmically, associated with lack of awareness | *Nodding of [[head]] rhythmically, associated with lack of awareness | ||
*Periods of rapid [[eye]] [[blinking]] | *Periods of rapid [[eye]] [[blinking]] | ||
===Physical Examination=== | ===Physical Examination=== | ||
* Vital Signs: [[Tachycardia]] may be present. | |||
*Physical examination of a patient with COVID-19-associated seizure include: | |||
==== Vital Signs ==== | |||
*[[Vital signs]]: [[Tachycardia]] may be present. | |||
===== HEENT ===== | |||
* Finding a [[bite]] to the side of the [[tongue]] (when present, is helpful in making the diagnosis). | * Finding a [[bite]] to the side of the [[tongue]] (when present, is helpful in making the diagnosis). | ||
===== Neuromuscular ===== | |||
*[[Postictal state|Postictal]] [[drowsiness]] or [[confusion]]. | |||
===Laboratory Findings=== | ===Laboratory Findings=== | ||
[[Postictal]] levels of the following may be elevated in a patient with [[seizures]]: | *[[Postictal state|Postictal]] levels of the following may be elevated in a patient with [[seizures]]: | ||
* [[Prolactin]] (within 20 minutes after a convulsive event) | **[[Prolactin]] (within 20 minutes after a convulsive event) | ||
* [[Lactate]] (within 1 to 2 hours) | **[[Lactate]] (within 1 to 2 hours) | ||
* [[Ammonia]] (within several hours) | **[[Ammonia]] (within several hours) | ||
* [[Creatine kinase]] (especially 24 to 48 hours postictally) | **[[Creatine kinase]] (especially 24 to 48 hours postictally) | ||
* To view the laboratory findings on COVID-19, [[COVID-19 laboratory findings|click here]]. | **To view the laboratory findings on COVID-19, [[COVID-19 laboratory findings|click here]]. | ||
===Electrocardiogram=== | ===Electrocardiogram=== | ||
* There are no typical ECG findings associated with seizures in a [[COVID-19]] patient. | |||
* To view the electrocardiogram findings on COVID-19, [[COVID-19 electrocardiogram|click here]].<br /> | *There are no typical [[ECG]] findings associated with seizures in a [[COVID-19]] patient. | ||
*To view the [[electrocardiogram]] findings on COVID-19, [[COVID-19 electrocardiogram|click here]].<br /> | |||
===X-ray=== | ===X-ray=== | ||
* There are no x-ray findings associated with [[COVID-19]] associated [[seizure]]. | |||
* To view the x-ray finidings on COVID-19, [[COVID-19 x ray|click here]].<br /> | *There are no [[X-rays|x-ray]] findings associated with [[COVID-19]] associated [[seizure]]. | ||
*To view the [[X-rays|x-ray]] finidings on COVID-19, [[COVID-19 x ray|click here]].<br /> | |||
===Echocardiography or Ultrasound=== | ===Echocardiography or Ultrasound=== | ||
* There are no typical [[Echocardiography|echocardiographic]] findings for [[seizure]] related to [[COVID-19]]. | |||
* To view the echocardiographic findings on COVID-19, [[COVID-19 echocardiography and ultrasound|click here]].<br /> | *There are no typical [[Echocardiography|echocardiographic]] findings for [[seizure]] related to [[COVID-19]]. | ||
*To view the echocardiographic findings on COVID-19, [[COVID-19 echocardiography and ultrasound|click here]].<br /> | |||
===CT scan=== | ===CT scan=== | ||
* [[CT]] [[brain]] may show structural lesions but majority of patients will show nothing. | |||
* To view the CT scan findings on COVID-19, [[COVID-19 CT scan|click here]]. | *[[CT]] [[brain]] may show structural lesions but majority of patients will show nothing. | ||
*To view the [[CT scan]] findings on COVID-19, [[COVID-19 CT scan|click here]]. | |||
===MRI=== | ===MRI=== | ||
* MRI brain may show structural lesions but majority of patients will show nothing. | |||
* To view the MRI findings on COVID-19, [[COVID-19 MRI|click here]].<br /> | *[[MRI]] brain may show structural lesions but majority of patients will show nothing. | ||
*To view the MRI findings on COVID-19, [[COVID-19 MRI|click here]].<br /> | |||
===Other Imaging Findings=== | ===Other Imaging Findings=== | ||
* There are no other imaging findings associated with [[seizure]] related to [[COVID-19]]. | |||
* To view other imaging findings on COVID-19, [[COVID-19 other imaging findings|click here]].<br /> | *There are no other imaging findings associated with [[seizure]] related to [[COVID-19]]. | ||
*To view other imaging findings on COVID-19, [[COVID-19 other imaging findings|click here]].<br /> | |||
===Other Diagnostic Studies=== | ===Other Diagnostic Studies=== | ||
* To view other diagnostic studies for COVID-19, [[COVID-19 other diagnostic studies|click here]].<br /> | |||
*To view other diagnostic studies for COVID-19, [[COVID-19 other diagnostic studies|click here]].<br /> | |||
==Treatment== | ==Treatment== | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
* Development of [[seizures]] in a [[COVID-19]] patient requires urgent treatment. | *Development of [[seizures]] in a [[COVID-19]] patient requires urgent treatment.<ref name="pmid25174548">{{cite journal |vauthors=Ueda R, Saito Y, Ohno K, Maruta K, Matsunami K, Saiki Y, Sokota T, Sugihara S, Nishimura Y, Tamasaki A, Narita A, Imamura A, Maegaki Y |title=Effect of levetiracetam in acute encephalitis with refractory, repetitive partial seizures during acute and chronic phase |journal=Brain Dev. |volume=37 |issue=5 |pages=471–7 |date=May 2015 |pmid=25174548 |doi=10.1016/j.braindev.2014.08.003 |url=}}</ref><ref name="pmid32283294">{{cite journal |vauthors=Ye M, Ren Y, Lv T |title=Encephalitis as a clinical manifestation of COVID-19 |journal=Brain Behav. Immun. |volume= |issue= |pages= |date=April 2020 |pmid=32283294 |pmc=7146652 |doi=10.1016/j.bbi.2020.04.017 |url=}}</ref><ref name="pmid32416567" /> | ||
*After the cause of [[seizure]] is determined, medical therapy should be aimed at treating the cause immediately (for example, [[hypoxia]], [[fever]], metabolic imbalance). | |||
*Anti-seizure medication ([[levetiracetam]] 50-60 mg/kg/day) is often necessary. | |||
*Anti-epileptics therapy with [[mannitol]] has been documented in decreasing [[cerebral edema]]. | |||
* For a single [[seizure]] less than 5 min rescue treatment with [[benzodiazepine]] is not needed. [[Intravenous]] | *For a single [[seizure]] less than 5 min rescue treatment with [[benzodiazepine]] is not needed. | ||
* [[Brivaracetam]] and [[Levetiracetam]] have less adverse effects and drug interactions. | *[[Intravenous]] antiseizure medication are used with caution in [[COVID-19]] patients due to the adverse effects (e.g., [[Phenytoin]], [[Phenobarbital]] and [[Lacosamide]] in [[respiratory]] and [[cardiac]] problems) and [[drug]] interactions (e.g., [[Carbamazepine]], [[Phenytoin]], [[Phenobarbital]] and [[Valproic acid]]). | ||
* In patients with more than one [[seizure]] (either shorter or longer than 5 min) and in [[status epilepticus]] rescue treatment with [[benzodiazepines]] in addition to ASM is needed. | *[[Brivaracetam]] and [[Levetiracetam]] have less adverse effects and drug interactions. | ||
*In patients with more than one [[seizure]] (either shorter or longer than 5 min) and in [[status epilepticus]] rescue treatment with [[benzodiazepines]] in addition to ASM is needed. | |||
===Surgery=== | ===Surgery=== | ||
Surgical intervention is not recommended for the management of [[COVID-19]] associated [[seizure]]. | |||
* Surgical intervention is not recommended for the management of [[COVID-19]] associated [[seizure]]. | |||
===Primary Prevention=== | ===Primary Prevention=== | ||
There are no established measures for the primary prevention of [[seizures]] associated with [[COVID-19]]. | |||
* There are no established measures for the [[primary prevention]] of [[seizures]] associated with [[COVID-19]]. | |||
===Secondary Prevention=== | ===Secondary Prevention=== | ||
There are no established measures for the secondary prevention of [[seizures]] associated with [[COVID-19]]. | |||
* There are no established measures for the [[secondary prevention]] of [[seizures]] associated with [[COVID-19]]. | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Up-To-Date]] | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Latest revision as of 23:49, 12 December 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mandana Safakhah, MD[2] Tayebah Chaudhry[3], Fahimeh Shojaei, M.D., Syed Musadiq Ali M.B.B.S.[4]
Synonyms and keywords:
Overview
Seizure refers to an episode of symptoms due to abnormally excessive or synchronous neuronal activity in the brain followed by return to normal state. Seizures manifest as abnormal uncontrolled shaking movements that involve much of the body with loss of consciousness, shaking movements of part of the body with variable level of consciousness or a subtle momentary loss of consciousness. As COVID-19 (caused by SARS-Cov2) is now known to have several neurological complications, seizure is one of the complications seen in a few cases so far. Brain waive activity can be seen on EEG to confirm diagnosis since structural changes are very rarely seen on brain imaging. Anti-seizure medications are used for symptomatic treatment of seizure along with treatment of COVID-19.
Historical Perspective
- First case of seizure in COVID-19 patient was a result of meningitis/encephalitis caused by SARS-CoV2 and documented by Moriguchi et al in late February 2020 [1].
- After that, more cases were reported with acute seizures as a complication of COVID-19.[2][3]
- In early February 2020, seizurelike activity was reported in two COVID-19 patients but the cause was acute anxiety disorder and electrolyte imbalance instead of viral damage by SARS-Cov-2[4]
- To view the historical perspective of COVID-19, click here.
Classification
Pathophysiology
- Neurological complications caused by COVID-19 are through direct or indirect pathways.
- This includes hematogenous pathway, neuronal retrograde dissemination through olfactory bulb, entry into to glial cells and neurons via ACE2 receptor and impairment of gas exchange in lungs leading to anemia, hence increasing anaerobic metabolites in brain resulting in cellular and interstitial edema [5]
- Seizures in a patient with COVID-19 may be due to primary virus infection or due to reactivation of the latent virus.
- Infiltration of the brain tissue by the virus and subsequent production of toxins by the virus is one of the several mechanisms that can cause seizures in a COVID-19 patient. [6]
- Production of inflammatory mediators by the brain may also trigger seizures.
- Inflammatory cytokines that are released as a result of inflammatory cascade provoked by COVID-19 include interleukin 2,6,7, and 10, TNF-α and granulocyte colony-stimulating factor. Consequently, activation of glutamate receptors by the cytokines causes neuronal hyperexcitability and development of seizures. [6]
Causes
- Cause of COVID-19-associated seizure is viral infection by SARS-CoV-2 and its consequences which include:[8]
- Hypoxia
- Metabolic derangement
- Organ failure
- Cerebral damage.[9]
- To view causes of COVID-19, click here.
Differentiating COVID-19-associated seizure from other Diseases
- For further information about the differential diagnosis, click here.
- To view the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
- More data is required to comment on epidemiology and demographics of COVID-19-associated seizure.
- One study, specifically investigated the neurological manifestations of COVID-19 and documented CNS manifestations in 25% of the patients (headache (13%), dizziness (17%), impaired consciousness (8%), acute cerebrovascular problems (3%), ataxia (0.5), and seizures (0.5%)][10]
Risk Factors
- Several risk factors of seizure in COVID-19 patients were considered in a multicenter restrospective study from Jan 18th to FEb 18th, 2020 in China.[11]
- Risk factors that were studied include acute cerebrovascular disease, traumatic brain injury (TBI), central nervous system (CNS) infection, shock, hypoxia, severe metabolic disturbance, multiple‐organ dysfunction syndrome, sepsis, and exposure to drugs or toxic substances.
- According to the study, hypoxia and imipenem were shown to be important risk factors, among several others, for seizure in a COVID-19 patient.
- To view the risk factors of COVID-19, click here.
Screening
Natural History, Complications, and Prognosis
Natural History
- Seizure activity in a patient with or without COVID-19 usually lasts for a few seconds to less than 5 minutes with return to normal after the seizure episode.
- If seizure episode lasts for more than 5 minutes it is called status epilepticus.
- This is followed by a period of confusion, called postictal period that can last 3-15 minutes and sometimes hours.
Complications
- Complications of COVID-19-associated seizure include:
Prognosis
- In general, after the first seizure, subsequent seizure episodes can be predicted using EEG and brain imaging.[12]
- Prognosis of seizure in a COVID-19 patient is not known.
- However, if left untreated, seizure caused by acute brain event is known to have low risk of recurrence but higher risk of death compared to those with epilepsy. [13]
Diagnosis
Diagnostic Study of Choice
- The diagnosis of COVID-19-associated seizure is made through electroencephalogram (EEG, brain waive activity).[14]
- Other diagnostic tests include:
- CT scan brain
- MRI brain
- Blood test
- Lumbar puncture
- Toxicology screening
Symptoms
Common symptoms:
- Staring
- Jerking movements of the arms and legs
- Stiffening of the body
- Loss of consciousness
- Breathing problems
Loss of bowel or bladder control
- Falling suddenly for no apparent reason, especially when associated with loss of consciousness
- Not responding to noise or words for brief periods
- Appearing confused or in a haze
Less common symptoms:
Physical Examination
- Physical examination of a patient with COVID-19-associated seizure include:
Vital Signs
- Vital signs: Tachycardia may be present.
HEENT
Neuromuscular
Laboratory Findings
- Postictal levels of the following may be elevated in a patient with seizures:
- Prolactin (within 20 minutes after a convulsive event)
- Lactate (within 1 to 2 hours)
- Ammonia (within several hours)
- Creatine kinase (especially 24 to 48 hours postictally)
- To view the laboratory findings on COVID-19, click here.
Electrocardiogram
- There are no typical ECG findings associated with seizures in a COVID-19 patient.
- To view the electrocardiogram findings on COVID-19, click here.
X-ray
- There are no x-ray findings associated with COVID-19 associated seizure.
- To view the x-ray finidings on COVID-19, click here.
Echocardiography or Ultrasound
- There are no typical echocardiographic findings for seizure related to COVID-19.
- To view the echocardiographic findings on COVID-19, click here.
CT scan
- CT brain may show structural lesions but majority of patients will show nothing.
- To view the CT scan findings on COVID-19, click here.
MRI
- MRI brain may show structural lesions but majority of patients will show nothing.
- To view the MRI findings on COVID-19, click here.
Other Imaging Findings
- There are no other imaging findings associated with seizure related to COVID-19.
- To view other imaging findings on COVID-19, click here.
Other Diagnostic Studies
- To view other diagnostic studies for COVID-19, click here.
Treatment
Medical Therapy
- Development of seizures in a COVID-19 patient requires urgent treatment.[15][16][8]
- After the cause of seizure is determined, medical therapy should be aimed at treating the cause immediately (for example, hypoxia, fever, metabolic imbalance).
- Anti-seizure medication (levetiracetam 50-60 mg/kg/day) is often necessary.
- Anti-epileptics therapy with mannitol has been documented in decreasing cerebral edema.
- For a single seizure less than 5 min rescue treatment with benzodiazepine is not needed.
- Intravenous antiseizure medication are used with caution in COVID-19 patients due to the adverse effects (e.g., Phenytoin, Phenobarbital and Lacosamide in respiratory and cardiac problems) and drug interactions (e.g., Carbamazepine, Phenytoin, Phenobarbital and Valproic acid).
- Brivaracetam and Levetiracetam have less adverse effects and drug interactions.
- In patients with more than one seizure (either shorter or longer than 5 min) and in status epilepticus rescue treatment with benzodiazepines in addition to ASM is needed.
Surgery
Primary Prevention
- There are no established measures for the primary prevention of seizures associated with COVID-19.
Secondary Prevention
- There are no established measures for the secondary prevention of seizures associated with COVID-19.
References
- ↑ Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Ueno M, Sakata H, Kondo K, Myose N, Nakao A, Takeda M, Haro H, Inoue O, Suzuki-Inoue K, Kubokawa K, Ogihara S, Sasaki T, Kinouchi H, Kojin H, Ito M, Onishi H, Shimizu T, Sasaki Y, Enomoto N, Ishihara H, Furuya S, Yamamoto T, Shimada S (May 2020). "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2". Int. J. Infect. Dis. 94: 55–58. doi:10.1016/j.ijid.2020.03.062. PMC 7195378 Check
|pmc=value (help). PMID 32251791 Check|pmid=value (help). - ↑ Template:Citejournal
- ↑ {{https://www.sciencedirect.com/science/article/pii/S1059131120301151}}
- ↑ {{https://onlinelibrary.wiley.com/doi/full/10.1111/epi.16524}}
- ↑ {{https://pubmed.ncbi.nlm.nih.gov/32458193/}}
- ↑ 6.0 6.1 Karimi, Narges; Sharifi Razavi, Athena; Rouhani, Nima (2020). "Frequent Convulsive Seizures in an Adult Patient with COVID-19: A Case Report". Iranian Red Crescent Medical Journal. 22 (3). doi:10.5812/ircmj.102828. ISSN 2074-1804.
- ↑ Abboud, Hilal; Abboud, Fatima Zahra; Kharbouch, Hanane; Arkha, Yasser; El Abbadi, Najia; El Ouahabi, Abdessamad (2020). "COVID-19 and SARS-Cov-2 Infection: Pathophysiology and Clinical Effects on the Nervous System". World Neurosurgery. 140: 49–53. doi:10.1016/j.wneu.2020.05.193. ISSN 1878-8750.
- ↑ 8.0 8.1 Asadi-Pooya AA (July 2020). "Seizures associated with coronavirus infections". Seizure. 79: 49–52. doi:10.1016/j.seizure.2020.05.005. PMC 7212943 Check
|pmc=value (help). PMID 32416567 Check|pmid=value (help). - ↑ {{https://www.ncbi.nlm.nih.gov/books/NBK430765/}}
- ↑ Mao, Ling; Jin, Huijuan; Wang, Mengdie; Hu, Yu; Chen, Shengcai; He, Quanwei; Chang, Jiang; Hong, Candong; Zhou, Yifan; Wang, David; Miao, Xiaoping; Li, Yanan; Hu, Bo (2020). "Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China". JAMA Neurology. 77 (6): 683. doi:10.1001/jamaneurol.2020.1127. ISSN 2168-6149.
- ↑ {{https://onlinelibrary.wiley.com/doi/full/10.1111/epi.16524}}
- ↑ Wilden JA, Cohen-Gadol AA (August 2012). "Evaluation of first nonfebrile seizures". Am Fam Physician. 86 (4): 334–40. PMID 22963022.
- ↑ Sander JW, Shorvon SD (November 1996). "Epidemiology of the epilepsies". J. Neurol. Neurosurg. Psychiatry. 61 (5): 433–43. doi:10.1136/jnnp.61.5.433. PMC 1074036. PMID 8965090.
- ↑ Haines S, Caccamo A, Chan F, Galaso G, Catinchi A, Gupta PK (2020). "Practical Considerations When Performing Neurodiagnostic Studies on Patients with COVID-19 and Other Highly Virulent Diseases". Neurodiagn J. 60 (2): 78–95. doi:10.1080/21646821.2020.1756132. PMC 7212538 Check
|pmc=value (help). PMID 32374647 Check|pmid=value (help). - ↑ Ueda R, Saito Y, Ohno K, Maruta K, Matsunami K, Saiki Y, Sokota T, Sugihara S, Nishimura Y, Tamasaki A, Narita A, Imamura A, Maegaki Y (May 2015). "Effect of levetiracetam in acute encephalitis with refractory, repetitive partial seizures during acute and chronic phase". Brain Dev. 37 (5): 471–7. doi:10.1016/j.braindev.2014.08.003. PMID 25174548.
- ↑ Ye M, Ren Y, Lv T (April 2020). "Encephalitis as a clinical manifestation of COVID-19". Brain Behav. Immun. doi:10.1016/j.bbi.2020.04.017. PMC 7146652 Check
|pmc=value (help). PMID 32283294 Check|pmid=value (help).