COVID-19-associated myocarditis: Difference between revisions
| (104 intermediate revisions by the same user not shown) | |||
| Line 5: | Line 5: | ||
{{SI}} | {{SI}} | ||
{{CMG}}; {{AE}} {{MRV}} | {{CMG}}; {{AE}} {{Sara.Zand}} {{MRV}} | ||
{{SK}} Novel coronavirus, COVID-19, Wuhan coronavirus, coronavirus disease-19, coronavirus disease 2019, SARS-CoV-2, COVID-19, COVID-19, 2019-nCoV, 2019 novel coronavirus, cardiovascular finding in COVID-19, myocardial injury in COVID-19, myocarditis, myocarditis in COVID-19, COVID-19-associated myocarditis, SARS-CoV2-associated myocarditis, myocardial injury in COVID-19, COVID-19 myocarditis | {{SK}} Novel coronavirus, COVID-19, Wuhan coronavirus, coronavirus disease-19, coronavirus disease 2019, SARS-CoV-2, COVID-19, COVID-19, 2019-nCoV, 2019 novel coronavirus, cardiovascular finding in COVID-19, myocardial injury in COVID-19, myocarditis, myocarditis in COVID-19, COVID-19-associated myocarditis, SARS-CoV2-associated myocarditis, myocardial injury in COVID-19, COVID-19 myocarditis | ||
==Overview== | ==Overview== | ||
[[COVID-19]] caused by the [[novel coronavirus]], also known as [[SARS-CoV-2]] mainly affects the [[lungs]] | [[COVID-19]] caused by the [[novel coronavirus]], also known as [[SARS-CoV-2]] mainly affects the [[lungs]] may lead to [[severe acute respiratory syndrome]] ([[SARS]]). It invades through the [[angiotensin-converting enzyme 2]] (ACE2) receptors present abundantly not only in the [[lungs]] but also in the [[heart]], [[kidneys]], [[intestine]], [[brain]], [[skin]] thus causing [[multiorgan failure|multiorgan dysfunction]] including [[cardiovascular]] complications and [[death]]. [[Myocarditis]] is one of the [[cardiovascular]] manifestation of [[COVID-19]] which is the [[inflammation]] of [[myocardium]] without stenosis in [[coronary arteries]], with the risk of [[arrhythmia]] as well as progression to [[fulminant heart failure ]] and [[cardiogenic shock]]. The proposed mechanisms including direct invasion through [[angiotensin-converting enzyme 2|ACE2]] receptors and [[inflammatory response]] or [[cytokine storm]]. In literature, [[myocardial edema]] and/or [[scarring]] were detected on [[cardiac MRI]] of reported [[myocarditis]] associated [[COVID-19]]. | ||
==Historical Perspective== | ==Historical Perspective== | ||
*The [[novel coronavirus]], [[SARS-CoV-2]], is identified as the cause of an outbreak of [[respiratory illness]] first detected in Wuhan, China in late December 2019. It was named [[SARS-CoV-2]] for its similarity [[severe acute respiratory syndrome]] related [[coronaviruses]] such as [[SARS-CoV]], which caused [[acute respiratory distress syndrome]] ([[ARDS]]) in 2002–2003.<ref name="LuCui2020">{{cite journal|last1=Lu|first1=Jian|last2=Cui|first2=Jie|last3=Qian|first3=Zhaohui|last4=Wang|first4=Yirong|last5=Zhang|first5=Hong|last6=Duan|first6=Yuange|last7=Wu|first7=Xinkai|last8=Yao|first8=Xinmin|last9=Song|first9=Yuhe|last10=Li|first10=Xiang|last11=Wu|first11=Changcheng|last12=Tang|first12=Xiaolu|title=On the origin and continuing evolution of SARS-CoV-2|journal=National Science Review|year=2020|issn=2095-5138|doi=10.1093/nsr/nwaa036}}</ref><ref name="HuangWang2020">{{cite journal|last1=Huang|first1=Chaolin|last2=Wang|first2=Yeming|last3=Li|first3=Xingwang|last4=Ren|first4=Lili|last5=Zhao|first5=Jianping|last6=Hu|first6=Yi|last7=Zhang|first7=Li|last8=Fan|first8=Guohui|last9=Xu|first9=Jiuyang|last10=Gu|first10=Xiaoying|last11=Cheng|first11=Zhenshun|last12=Yu|first12=Ting|last13=Xia|first13=Jiaan|last14=Wei|first14=Yuan|last15=Wu|first15=Wenjuan|last16=Xie|first16=Xuelei|last17=Yin|first17=Wen|last18=Li|first18=Hui|last19=Liu|first19=Min|last20=Xiao|first20=Yan|last21=Gao|first21=Hong|last22=Guo|first22=Li|last23=Xie|first23=Jungang|last24=Wang|first24=Guangfa|last25=Jiang|first25=Rongmeng|last26=Gao|first26=Zhancheng|last27=Jin|first27=Qi|last28=Wang|first28=Jianwei|last29=Cao|first29=Bin|title=Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China|journal=The Lancet|volume=395|issue=10223|year=2020|pages=497–506|issn=01406736|doi=10.1016/S0140-6736(20)30183-5}}</ref> | *The [[novel coronavirus]], [[SARS-CoV-2]], is identified as the cause of an outbreak of [[respiratory illness]] first detected in Wuhan, China in late December 2019. It was named [[SARS-CoV-2]] for its similarity [[severe acute respiratory syndrome]] related [[coronaviruses]] such as [[SARS-CoV]], which caused [[acute respiratory distress syndrome]] ([[ARDS]]) in 2002–2003.<ref name="LuCui2020">{{cite journal|last1=Lu|first1=Jian|last2=Cui|first2=Jie|last3=Qian|first3=Zhaohui|last4=Wang|first4=Yirong|last5=Zhang|first5=Hong|last6=Duan|first6=Yuange|last7=Wu|first7=Xinkai|last8=Yao|first8=Xinmin|last9=Song|first9=Yuhe|last10=Li|first10=Xiang|last11=Wu|first11=Changcheng|last12=Tang|first12=Xiaolu|title=On the origin and continuing evolution of SARS-CoV-2|journal=National Science Review|year=2020|issn=2095-5138|doi=10.1093/nsr/nwaa036}}</ref><ref name="HuangWang2020">{{cite journal|last1=Huang|first1=Chaolin|last2=Wang|first2=Yeming|last3=Li|first3=Xingwang|last4=Ren|first4=Lili|last5=Zhao|first5=Jianping|last6=Hu|first6=Yi|last7=Zhang|first7=Li|last8=Fan|first8=Guohui|last9=Xu|first9=Jiuyang|last10=Gu|first10=Xiaoying|last11=Cheng|first11=Zhenshun|last12=Yu|first12=Ting|last13=Xia|first13=Jiaan|last14=Wei|first14=Yuan|last15=Wu|first15=Wenjuan|last16=Xie|first16=Xuelei|last17=Yin|first17=Wen|last18=Li|first18=Hui|last19=Liu|first19=Min|last20=Xiao|first20=Yan|last21=Gao|first21=Hong|last22=Guo|first22=Li|last23=Xie|first23=Jungang|last24=Wang|first24=Guangfa|last25=Jiang|first25=Rongmeng|last26=Gao|first26=Zhancheng|last27=Jin|first27=Qi|last28=Wang|first28=Jianwei|last29=Cao|first29=Bin|title=Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China|journal=The Lancet|volume=395|issue=10223|year=2020|pages=497–506|issn=01406736|doi=10.1016/S0140-6736(20)30183-5}}</ref> | ||
| Line 26: | Line 27: | ||
*The exact mechanisms of [[COVID-19]] induced [[myocarditis]] are not yet well known, although several have been proposed based on the limited data outside of case reports. | *The exact mechanisms of [[COVID-19]] induced [[myocarditis]] are not yet well known, although several have been proposed based on the limited data outside of case reports. | ||
===Proposed pathophysiologies of COVID-19 associated myocarditis=== | ===Proposed pathophysiologies of COVID-19 associated myocarditis=== | ||
* Direct [[myocardial injury]] by binding of [[SARS-COV-2 virus]] through [[ACE2]] [[receptors]] | |||
* [[Systemic inflammatory response syndrome]] ([[SIRS]]) | |||
* Increased level of [[metabolic]] requirement along with lower [[supply]] due to [[hypoxia]] leading to [[supply-demand mismatch]] | |||
* Diffuse vasculitis and [[endothelial inflammation]] in the [[heart]]<ref name="pmid34235815">{{cite journal |vauthors=Rathore SS, Rojas GA, Sondhi M, Pothuru S, Pydi R, Kancherla N, Singh R, Ahmed NK, Shah J, Tousif S, Baloch UT, Wen Q |title=Myocarditis associated with Covid-19 disease: A systematic review of published case reports and case series |journal=Int J Clin Pract |volume= |issue= |pages=e14470 |date=July 2021 |pmid=34235815 |doi=10.1111/ijcp.14470 |url=}}</ref> | |||
*'''Direct invasion of the virus into cardiomyocytes''': | *'''Direct invasion of the virus into cardiomyocytes''': | ||
**[[COVID-19]] infection is caused by [[receptor-mediated endocytosis]] via binding of the [[viral]] [[surface spike]] [[protein]] (primed by [[TMPRSS2]] - [[TMPRSS2|Transmembrane Protease Serine 2]]) to the human [[angiotensin-converting enzyme 2]] ([[angiotensin-converting enzyme 2|ACE2]]) [[receptor]].<ref name="HoffmannKleine-Weber2020">{{cite journal|last1=Hoffmann|first1=Markus|last2=Kleine-Weber|first2=Hannah|last3=Schroeder|first3=Simon|last4=Krüger|first4=Nadine|last5=Herrler|first5=Tanja|last6=Erichsen|first6=Sandra|last7=Schiergens|first7=Tobias S.|last8=Herrler|first8=Georg|last9=Wu|first9=Nai-Huei|last10=Nitsche|first10=Andreas|last11=Müller|first11=Marcel A.|last12=Drosten|first12=Christian|last13=Pöhlmann|first13=Stefan|title=SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor|journal=Cell|volume=181|issue=2|year=2020|pages=271–280.e8|issn=00928674|doi=10.1016/j.cell.2020.02.052}}</ref><ref name="WanShang2020">{{cite journal|last1=Wan|first1=Yushun|last2=Shang|first2=Jian|last3=Graham|first3=Rachel|last4=Baric|first4=Ralph S.|last5=Li|first5=Fang|last6=Gallagher|first6=Tom|title=Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade-Long Structural Studies of SARS Coronavirus|journal=Journal of Virology|volume=94|issue=7|year=2020|issn=0022-538X|doi=10.1128/JVI.00127-20}}</ref> | **[[COVID-19]] infection is caused by [[receptor-mediated endocytosis]] via binding of the [[viral]] [[surface spike]] [[protein]] (primed by [[TMPRSS2]] - [[TMPRSS2|Transmembrane Protease Serine 2]]) to the human [[angiotensin-converting enzyme 2]] ([[angiotensin-converting enzyme 2|ACE2]]) [[receptor]].<ref name="HoffmannKleine-Weber2020">{{cite journal|last1=Hoffmann|first1=Markus|last2=Kleine-Weber|first2=Hannah|last3=Schroeder|first3=Simon|last4=Krüger|first4=Nadine|last5=Herrler|first5=Tanja|last6=Erichsen|first6=Sandra|last7=Schiergens|first7=Tobias S.|last8=Herrler|first8=Georg|last9=Wu|first9=Nai-Huei|last10=Nitsche|first10=Andreas|last11=Müller|first11=Marcel A.|last12=Drosten|first12=Christian|last13=Pöhlmann|first13=Stefan|title=SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor|journal=Cell|volume=181|issue=2|year=2020|pages=271–280.e8|issn=00928674|doi=10.1016/j.cell.2020.02.052}}</ref><ref name="WanShang2020">{{cite journal|last1=Wan|first1=Yushun|last2=Shang|first2=Jian|last3=Graham|first3=Rachel|last4=Baric|first4=Ralph S.|last5=Li|first5=Fang|last6=Gallagher|first6=Tom|title=Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade-Long Structural Studies of SARS Coronavirus|journal=Journal of Virology|volume=94|issue=7|year=2020|issn=0022-538X|doi=10.1128/JVI.00127-20}}</ref> | ||
| Line 47: | Line 54: | ||
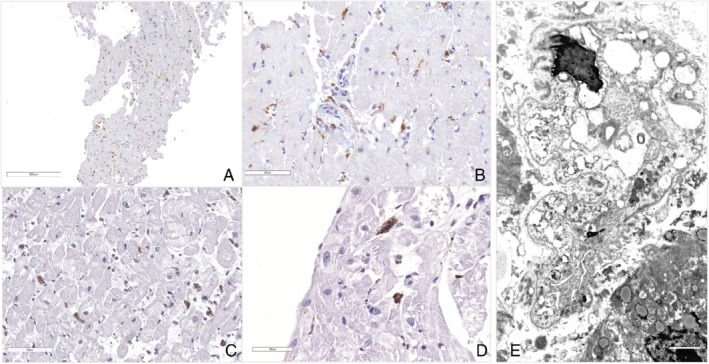
[[File:Endomyocardial biopsy in covid patients .jpg|center|thumb|709x709px|[[Light microscopy|Light microscop]]<nowiki/>y immunostaining of the inflammatory infiltrate. (''A'',''B'') Low‐ and high‐power views of endomyocardial biopsy, with sparse CD45RO positive interstitial cells. (''C'',''D'') Large, vacuolated macrophages immunostained with anti‐CD68 antibodies. (''E'') Ultrastructural morphology of a large and cytopathic macrophage. (''A–D'': the bar scale is in the left low corner of each panel. ''E'': the bar scale is in the right low corner of the panel and corresponds to 2 μm). Case courtesy by Guido Tavazzi<ref>{{Cite web|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7262276/|title=Myocardial localization of coronavirus in COVID‐19 cardiogenic shock|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref>]] | [[File:Endomyocardial biopsy in covid patients .jpg|center|thumb|709x709px|[[Light microscopy|Light microscop]]<nowiki/>y immunostaining of the inflammatory infiltrate. (''A'',''B'') Low‐ and high‐power views of endomyocardial biopsy, with sparse CD45RO positive interstitial cells. (''C'',''D'') Large, vacuolated macrophages immunostained with anti‐CD68 antibodies. (''E'') Ultrastructural morphology of a large and cytopathic macrophage. (''A–D'': the bar scale is in the left low corner of each panel. ''E'': the bar scale is in the right low corner of the panel and corresponds to 2 μm). Case courtesy by Guido Tavazzi<ref>{{Cite web|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7262276/|title=Myocardial localization of coronavirus in COVID‐19 cardiogenic shock|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref>]] | ||
<br /> | <br /> | ||
*[[Diffuse lymphocytic inflammatory infiltration ]] was the most common histopathologic finding among 42 cases of [[myocarditis]] associated [[COVID-19]] in literature.<ref name="pmid34235815">{{cite journal |vauthors=Rathore SS, Rojas GA, Sondhi M, Pothuru S, Pydi R, Kancherla N, Singh R, Ahmed NK, Shah J, Tousif S, Baloch UT, Wen Q |title=Myocarditis associated with Covid-19 disease: A systematic review of published case reports and case series |journal=Int J Clin Pract |volume= |issue= |pages=e14470 |date=July 2021 |pmid=34235815 |doi=10.1111/ijcp.14470 |url=}}</ref> | |||
==Causes== | ==Causes== | ||
| Line 59: | Line 67: | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
*The [[ | * The [[incidence]] of [[myocarditis]] was 7000 per 100,000 [[patients]] who died of [[covid-19]]. <ref name="pmid32201335">{{cite journal |vauthors=Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA |title=Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic |journal=J Am Coll Cardiol |volume=75 |issue=18 |pages=2352–2371 |date=May 2020 |pmid=32201335 |pmc=7198856 |doi=10.1016/j.jacc.2020.03.031 |url=}}</ref> | ||
* | *The [[incidence]] of [[myocardial injury]] among [[patients]] with [[COVID-19]] was approximately 24,400 per 100,000 hospitalized [[COVID-19]] [[patients]].<ref name="pmid32838255">{{cite journal |vauthors=Zou F, Qian Z, Wang Y, Zhao Y, Bai J |title=Cardiac Injury and COVID-19: A Systematic Review and Meta-analysis |journal=CJC Open |volume=2 |issue=5 |pages=386–394 |date=September 2020 |pmid=32838255 |pmc=7308771 |doi=10.1016/j.cjco.2020.06.010 |url=}}</ref> | ||
* In a cohort study the [[incidence]] of [[myocardial injury|acute cardiac injury]] caused by [[COVID-19]] was 19.7% of [[patients]] out of 416 hospitalized [[covid-19]] [[patients]] whether the portion of them is believed to be [[myocarditis]].<ref name="ShiQin2020">{{cite journal|last1=Shi|first1=Shaobo|last2=Qin|first2=Mu|last3=Shen|first3=Bo|last4=Cai|first4=Yuli|last5=Liu|first5=Tao|last6=Yang|first6=Fan|last7=Gong|first7=Wei|last8=Liu|first8=Xu|last9=Liang|first9=Jinjun|last10=Zhao|first10=Qinyan|last11=Huang|first11=He|last12=Yang|first12=Bo|last13=Huang|first13=Congxin|title=Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China|journal=JAMA Cardiology|year=2020|issn=2380-6583|doi=10.1001/jamacardio.2020.0950}}</ref> | |||
*There are some [[case reports]] of [[myocarditis]] related to [[COVID-19]].<ref name="ShiQin2020">{{cite journal|last1=Shi|first1=Shaobo|last2=Qin|first2=Mu|last3=Shen|first3=Bo|last4=Cai|first4=Yuli|last5=Liu|first5=Tao|last6=Yang|first6=Fan|last7=Gong|first7=Wei|last8=Liu|first8=Xu|last9=Liang|first9=Jinjun|last10=Zhao|first10=Qinyan|last11=Huang|first11=He|last12=Yang|first12=Bo|last13=Huang|first13=Congxin|title=Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China|journal=JAMA Cardiology|year=2020|issn=2380-6583|doi=10.1001/jamacardio.2020.0950}}</ref><ref name="ZengLiu2020">{{cite journal|last1=Zeng|first1=Jia-Hui|last2=Liu|first2=Ying-Xia|last3=Yuan|first3=Jing|last4=Wang|first4=Fu-Xiang|last5=Wu|first5=Wei-Bo|last6=Li|first6=Jin-Xiu|last7=Wang|first7=Li-Fei|last8=Gao|first8=Hong|last9=Wang|first9=Yao|last10=Dong|first10=Chang-Feng|last11=Li|first11=Yi-Jun|last12=Xie|first12=Xiao-Juan|last13=Feng|first13=Cheng|last14=Liu|first14=Lei|title=First case of COVID-19 complicated with fulminant myocarditis: a case report and insights|journal=Infection|year=2020|issn=0300-8126|doi=10.1007/s15010-020-01424-5}}</ref><ref name="InciardiLupi2020">{{cite journal|last1=Inciardi|first1=Riccardo M.|last2=Lupi|first2=Laura|last3=Zaccone|first3=Gregorio|last4=Italia|first4=Leonardo|last5=Raffo|first5=Michela|last6=Tomasoni|first6=Daniela|last7=Cani|first7=Dario S.|last8=Cerini|first8=Manuel|last9=Farina|first9=Davide|last10=Gavazzi|first10=Emanuele|last11=Maroldi|first11=Roberto|last12=Adamo|first12=Marianna|last13=Ammirati|first13=Enrico|last14=Sinagra|first14=Gianfranco|last15=Lombardi|first15=Carlo M.|last16=Metra|first16=Marco|title=Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)|journal=JAMA Cardiology|year=2020|issn=2380-6583|doi=10.1001/jamacardio.2020.1096}}</ref><ref name="HanKim2020">{{cite journal|last1=Han|first1=Seongwook|last2=Kim|first2=Hyun Ah|last3=Kim|first3=Jin Young|last4=Kim|first4=In-Cheol|title=COVID-19-related myocarditis in a 21-year-old female patient|journal=European Heart Journal|volume=41|issue=19|year=2020|pages=1859–1859|issn=0195-668X|doi=10.1093/eurheartj/ehaa288}}</ref><ref name="EspositoGodino2020">{{cite journal|last1=Esposito|first1=Antonio|last2=Godino|first2=Cosmo|last3=Basso|first3=Cristina|last4=Cappelletti|first4=Alberto Maria|last5=Tresoldi|first5=Moreno|last6=De Cobelli|first6=Francesco|last7=Vignale|first7=Davide|last8=Villatore|first8=Andrea|last9=Palmisano|first9=Anna|last10=Gramegna|first10=Mario|last11=Peretto|first11=Giovanni|last12=Sala|first12=Simone|title=Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection|journal=European Heart Journal|volume=41|issue=19|year=2020|pages=1861–1862|issn=0195-668X|doi=10.1093/eurheartj/ehaa286}}</ref><ref name="FangWei2020">{{cite journal|last1=Fang|first1=Yuan|last2=Wei|first2=Xin|last3=Ma|first3=Fenglian|last4=Hu|first4=Hongde|title=Coronavirus fulminant myocarditis treated with glucocorticoid and human immunoglobulin|journal=European Heart Journal|year=2020|issn=0195-668X|doi=10.1093/eurheartj/ehaa190}}</ref><ref name="TavazziPellegrini2020">{{cite journal|last1=Tavazzi|first1=Guido|last2=Pellegrini|first2=Carlo|last3=Maurelli|first3=Marco|last4=Belliato|first4=Mirko|last5=Sciutti|first5=Fabio|last6=Bottazzi|first6=Andrea|last7=Sepe|first7=Paola Alessandra|last8=Resasco|first8=Tullia|last9=Camporotondo|first9=Rita|last10=Bruno|first10=Raffaele|last11=Baldanti|first11=Fausto|last12=Paolucci|first12=Stefania|last13=Pelenghi|first13=Stefano|last14=Iotti|first14=Giorgio Antonio|last15=Mojoli|first15=Francesco|last16=Arbustini|first16=Eloisa|title=Myocardial localization of coronavirus in COVID‐19 cardiogenic shock|journal=European Journal of Heart Failure|volume=22|issue=5|year=2020|pages=911–915|issn=1388-9842|doi=10.1002/ejhf.1828}}</ref><ref name="CoyleIgbinomwanhia2020">{{cite journal|last1=Coyle|first1=Justin|last2=Igbinomwanhia|first2=Efehi|last3=Sanchez-Nadales|first3=Alejandro|last4=Danciu|first4=Sorin|last5=Chu|first5=Chae|last6=Shah|first6=Nishit|title=A Recovered Case of COVID-19 Myocarditis and ARDS Treated With Corticosteroids, Tocilizumab, and Experimental AT-001|journal=JACC: Case Reports|year=2020|issn=26660849|doi=10.1016/j.jaccas.2020.04.025}}</ref><ref name="LuetkensIsaak2020">{{cite journal|last1=Luetkens|first1=Julian Alexander|last2=Isaak|first2=Alexander|last3=Zimmer|first3=Sebastian|last4=Nattermann|first4=Jacob|last5=Sprinkart|first5=Alois Martin|last6=Boesecke|first6=Christoph|last7=Rieke|first7=Gereon Jonas|last8=Zachoval|first8=Christian|last9=Heine|first9=Annkristin|last10=Velten|first10=Markus|last11=Duerr|first11=Georg Daniel|title=Diffuse Myocardial Inflammation in COVID-19 Associated Myocarditis Detected by Multiparametric Cardiac Magnetic Resonance Imaging|journal=Circulation: Cardiovascular Imaging|volume=13|issue=5|year=2020|issn=1941-9651|doi=10.1161/CIRCIMAGING.120.010897}}</ref><ref name="BeşlerArslan2020">{{cite journal|last1=Beşler|first1=Muhammed Said|last2=Arslan|first2=Halil|title=Acute myocarditis associated with COVID-19 infection|journal=The American Journal of Emergency Medicine|year=2020|issn=07356757|doi=10.1016/j.ajem.2020.05.100}}</ref> | |||
===Age=== | ===Age=== | ||
*[[ | * Among reported cases in the literature, [[myocarditis]] associated [[COVID-19]] was more commonly observed among [[patients]] with a median age of 43.4 years.<ref name="pmid34235815">{{cite journal |vauthors=Rathore SS, Rojas GA, Sondhi M, Pothuru S, Pydi R, Kancherla N, Singh R, Ahmed NK, Shah J, Tousif S, Baloch UT, Wen Q |title=Myocarditis associated with Covid-19 disease: A systematic review of published case reports and case series |journal=Int J Clin Pract |volume= |issue= |pages=e14470 |date=July 2021 |pmid=34235815 |doi=10.1111/ijcp.14470 |url=}}</ref> | ||
* [[Myocarditis]] after [[vaccination]] of [[covid-19]] was commonly observed in [[young]] [[male]].<ref name="pmid34347001">{{cite journal |vauthors=Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson IV, Robicsek A |title=Myocarditis and Pericarditis After Vaccination for COVID-19 |journal=JAMA |volume=326 |issue=12 |pages=1210–1212 |date=September 2021 |pmid=34347001 |doi=10.1001/jama.2021.13443 |url=}}</ref> | |||
===Gender=== | ===Gender=== | ||
* | *[[Male]]s are more commonly affected with [[myocarditis]] associated [[COVID-19]] than [[females]] based on the reported cases in literature. | ||
===Race=== | ===Race=== | ||
*There is no data on racial predilection to [[myocarditis]] in [[COVID-19]]. | *There is no data on racial predilection to [[myocarditis]] in [[COVID-19]]. | ||
==Risk Factors== | ==Risk Factors== | ||
*There are no established risk factors for [[myocarditis]] | *There are no established risk factors for [[myocarditis]] associated [[COVID-19]]. However, concomitant [[cardiac]] [[comorbidities]] may present with [[myocarditis]]. | ||
==Screening== | ==Screening== | ||
| Line 81: | Line 90: | ||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
===Natural history=== | ===Natural history=== | ||
* If left untreated, [[myocarditis]] | * In the presence of [[SARS-COV-2]] cells in the [[myocardium]], early clinical features include [[acute heart failure]], refractory [[ventricular tachycardia]], reduced [[left ventricular]] [[ejection fraction]] and rapidly develop to [[death]].<ref name="pmid33727695">{{cite journal |vauthors=Bearse M, Hung YP, Krauson AJ, Bonanno L, Boyraz B, Harris CK, Helland TL, Hilburn CF, Hutchison B, Jobbagy S, Marshall MS, Shepherd DJ, Villalba JA, Delfino I, Mendez-Pena J, Chebib I, Newton-Cheh C, Stone JR |title=Factors associated with myocardial SARS-CoV-2 infection, myocarditis, and cardiac inflammation in patients with COVID-19 |journal=Mod Pathol |volume=34 |issue=7 |pages=1345–1357 |date=July 2021 |pmid=33727695 |doi=10.1038/s41379-021-00790-1 |url=}}</ref> | ||
*[[Patients]] with the presentation of [[third-degree AV block]], [[ventricular tachycardia]], and [[ventricular fibrillation]] may progress to develope [[cardiac arrest]] and [[in-hospital death]] in the context of [[fulminant myocarditis]]. | |||
*In the course of [[covid-19]] [[infection]], [[myocarditis]] is often a relatively late event.<ref name="pmid33727695">{{cite journal |vauthors=Bearse M, Hung YP, Krauson AJ, Bonanno L, Boyraz B, Harris CK, Helland TL, Hilburn CF, Hutchison B, Jobbagy S, Marshall MS, Shepherd DJ, Villalba JA, Delfino I, Mendez-Pena J, Chebib I, Newton-Cheh C, Stone JR |title=Factors associated with myocardial SARS-CoV-2 infection, myocarditis, and cardiac inflammation in patients with COVID-19 |journal=Mod Pathol |volume=34 |issue=7 |pages=1345–1357 |date=July 2021 |pmid=33727695 |doi=10.1038/s41379-021-00790-1 |url=}}</ref> | |||
*[[Cardiac]] [[infection]] by [[SARS-CoV-2]] is associated with more [[electrocardiographic]] changes. | |||
* [[Atrial fibrillation]] was the most common [[arrhythmia]] in such [[patients]] and was associated with poor outcome.<ref name="pmid33017083">{{cite journal |vauthors=Peltzer B, Manocha KK, Ying X, Kirzner J, Ip JE, Thomas G, Liu CF, Markowitz SM, Lerman BB, Safford MM, Goyal P, Cheung JW |title=Outcomes and mortality associated with atrial arrhythmias among patients hospitalized with COVID-19 |journal=J Cardiovasc Electrophysiol |volume=31 |issue=12 |pages=3077–3085 |date=December 2020 |pmid=33017083 |pmc=7675597 |doi=10.1111/jce.14770 |url=}}</ref><ref name="pmid33727695">{{cite journal |vauthors=Bearse M, Hung YP, Krauson AJ, Bonanno L, Boyraz B, Harris CK, Helland TL, Hilburn CF, Hutchison B, Jobbagy S, Marshall MS, Shepherd DJ, Villalba JA, Delfino I, Mendez-Pena J, Chebib I, Newton-Cheh C, Stone JR |title=Factors associated with myocardial SARS-CoV-2 infection, myocarditis, and cardiac inflammation in patients with COVID-19 |journal=Mod Pathol |volume=34 |issue=7 |pages=1345–1357 |date=July 2021 |pmid=33727695 |doi=10.1038/s41379-021-00790-1 |url=}}</ref> | |||
* If left untreated, [[myocarditis]] in [[patients]] with [[COVID-19]] may progress to [[cardiogenic shock]], [[heart failure]], and eventually may lead to [[death]].<ref name="CoyleIgbinomwanhia2020">{{cite journal|last1=Coyle|first1=Justin|last2=Igbinomwanhia|first2=Efehi|last3=Sanchez-Nadales|first3=Alejandro|last4=Danciu|first4=Sorin|last5=Chu|first5=Chae|last6=Shah|first6=Nishit|title=A Recovered Case of COVID-19 Myocarditis and ARDS Treated With Corticosteroids, Tocilizumab, and Experimental AT-001|journal=JACC: Case Reports|year=2020|issn=26660849|doi=10.1016/j.jaccas.2020.04.025}}</ref><ref name="RuanYang2020">{{cite journal|last1=Ruan|first1=Qiurong|last2=Yang|first2=Kun|last3=Wang|first3=Wenxia|last4=Jiang|first4=Lingyu|last5=Song|first5=Jianxin|title=Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China|journal=Intensive Care Medicine|volume=46|issue=5|year=2020|pages=846–848|issn=0342-4642|doi=10.1007/s00134-020-05991-x}}</ref> | |||
===Complications=== | ===Complications=== | ||
Common complications of [[myocarditis]] include: | Common complications of [[myocarditis]] include: | ||
| Line 93: | Line 108: | ||
===Prognosis=== | ===Prognosis=== | ||
*[[Prognosis]] | *[[Prognosis]] was generally good and the majority of [[patients]] (81%) of reported cases survived, and [[mortality rate]] was 19% among reported cases.<ref name="pmid32847728">{{cite journal |vauthors=Sawalha K, Abozenah M, Kadado AJ, Battisha A, Al-Akchar M, Salerno C, Hernandez-Montfort J, Islam AM |title=Systematic Review of COVID-19 Related Myocarditis: Insights on Management and Outcome |journal=Cardiovasc Revasc Med |volume=23 |issue= |pages=107–113 |date=February 2021 |pmid=32847728 |pmc=7434380 |doi=10.1016/j.carrev.2020.08.028 |url=}}</ref> | ||
{| style="border: 2px solid #4479BA; align="left" | |||
! style="width: 200px; background: #4479BA;" | {{fontcolor|#FFF|Age, sex}} | |||
! style="width: 300px; background: #4479BA;" | {{fontcolor|#FFF|Cardiovascular history}} | |||
! style="width: 400px; background: #4479BA;" | {{fontcolor|#FFF|Symptoms}} | |||
! style="width: 200px; background: #4479BA;" | {{fontcolor|#FFF|Laboratory findings}} | |||
! style="width: 200px; background: #4479BA;" | {{fontcolor|#FFF|Timing according to covid-19 infection }} | |||
! style="width: 200px; background: #4479BA;" | {{fontcolor|#FFF|Concomitant covid-19 complications}} | |||
! style="width: 200px; background: #4479BA;" | {{fontcolor|#FFF|Covid-19 severity}} | |||
! style="width: 200px; background: #4479BA;" | {{fontcolor|#FFF|Diagnosis}} | |||
! style="width: 200px; background: #4479BA;" | {{fontcolor|#FFF| Pathology}} | |||
! style="width: 200px; background: #4479BA;" | {{fontcolor|#FFF|Treatment}} | |||
! style="width: 200px; background: #4479BA;" | {{fontcolor|#FFF|Outcome}} | |||
|- | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | 45 years, [[male]]<ref name="pmid34651099">{{cite journal |vauthors=Fiore G, Sanvito F, Fragasso G, Spoladore R |title=Case report of cardiogenic shock in COVID-19 myocarditis: peculiarities on diagnosis, histology, and treatment |journal=Eur Heart J Case Rep |volume=5 |issue=10 |pages=ytab357 |date=October 2021 |pmid=34651099 |pmc=8502841 |doi=10.1093/ehjcr/ytab357 |url=}}</ref> | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Hypertension]], [[diabetes mellitus]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | First [[symptoms]]: [[fever]], [[mild dyspnea]], [[fatigue]] turned to [[severe dyspnea]], [[confusion]] and [[cardiogenic shock]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | High levels of [[troponin]], [[CRP]], [[NT-Pro BNP]], mild [[leukocytosis]], [[thrombocytopenia]], | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | 5 days | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Sinus tachycardia]], [[low peripheral voltage]], diffuse repolarization abnormalities | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Mild ground glass opacification]] in [[chest CT scan]], severe [[biventricular dysfunction]] in [[echocardiography]], absent of [[late gadolinium enhancement]] on [[cardiac MRI]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Myocarditis]] due to massive [[cytokine storm]] of [[COVID-19]] regardless the absence of [[SARS-COV-2 RNA]] in [[EBM]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | Mild [[lymphohistiocytic inflammatory infiltration]], without [[myocardial necrosis]], positive parvovirus B19, but not [[SARS-COV-2 RNA]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[IABP]], [[noradrenalin]], [[hydroxychloroquine]], [[steroid]] therapy, [[antibiotic]]s, [[Levosimendan]], IL-1inhibitor ([[anakinra]]), | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | Improving [[LVEF]] to 40-45% , [[TAPSE]]=18mm few day later and normalized biventricular function on [[CMR]] after 3 months, discharged with standard medications for [[heart failure]] therapy and a 6 month therapy with [[Anakinra]] 100 mg daily | |||
|- | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | 48 years, [[male]]<ref name="pmid33437916">{{cite journal |vauthors=Hudowenz O, Klemm P, Lange U, Rolf A, Schultheiss HP, Hamm C, Müller-Ladner U, Wegner F |title=Case report of severe PCR-confirmed COVID-19 myocarditis in a European patient manifesting in mid January 2020 |journal=Eur Heart J Case Rep |volume=4 |issue=6 |pages=1–6 |date=December 2020 |pmid=33437916 |pmc=7665439 |doi=10.1093/ehjcr/ytaa286 |url=}}</ref> | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Hypertension]], [[diabetes mellitus]], [[hyperlipidemia]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Fever]], [[dyspnea]], [[hemoptesia]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | High levels of [[inflammatory]] and [[cardiac]] damage markers | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | unknown | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | No [[ischemia]] sign on [[ECG]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | Bilateral patchy peripheral [[ground glass]] with [[crazy-paving pattern]] in [[chest CT scan]], reduced [[biventricular function]] in [[echocardiography]], [[myocardial edema]] and [[late gadolinium enhancement]] in [[CMR]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Myocarditis]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Acute lymphocytic myocarditis]], [[rheumatic vasculitis]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Cyclophosphamide]], [[steroide]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | Improvement | |||
|- | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | 81 years, [[male]]<ref name="pmid33111813">{{cite journal |vauthors=Yokoo P, Fonseca EKUN, Sasdelli Neto R, Ishikawa WY, Silva MMA, Yanata E, Chate RC, Nunes Filho ACB, Bettega M, Fernandes JRC, Tarasoutchi F, Szarf G |title=COVID-19 myocarditis: a case report |journal=Einstein (Sao Paulo) |volume=18 |issue= |pages=eRC5876 |date=2020 |pmid=33111813 |pmc=7575039 |doi=10.31744/einstein_journal/2020RC5876 |url=}}</ref> | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Hypertension]], [[ischemic stroke]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Fever]], [[dyspnea]], [[oxygen saturation of 91%]], [[ARDS]], [[acute cardiac dysfunction]] during admission | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | High levels of [[inflammatory]] and [[cardiac]] damage markers | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | 1 day | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | Small round ground glass opacities with multifocal distribution in both lungs field, specially in left perihilar region in [[chest CT scan]], reduced [[LVEF]] in [[echocardiography]], late gadolinium enhancement, [[ischemic]] pattern on base [[LV]] septum in [[CMR]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Myocarditis]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | [[Antibiotic]], [[steroid]], [[hemodynamic monitoring]] | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | Improvement, discharged with [[anticoagulant]] | |||
|} | |||
== Diagnosis == | == Diagnosis == | ||
| Line 120: | Line 187: | ||
=== Physical Examination === | === Physical Examination === | ||
*Physical examination of patients with severe [[myocarditis]] may find: | *Physical examination of [[patients]] with severe [[myocarditis]] may find: | ||
:*[[Tachycardia]] | :*[[Tachycardia]] | ||
:*Raised [[jugular venous pressure]] | :*Raised [[jugular venous pressure]] | ||
| Line 145: | Line 212: | ||
=== Electrocardiogram === | === Electrocardiogram === | ||
*[[ | *Findings of [[ECG]] in reported [[myocarditis]] associated [[covid-19]] include:<ref name="pmid32363336">{{cite journal |vauthors=Juusela A, Nazir M, Gimovsky M |title=Two cases of coronavirus 2019-related cardiomyopathy in pregnancy |journal=Am J Obstet Gynecol MFM |volume=2 |issue=2 |pages=100113 |date=May 2020 |pmid=32363336 |pmc=7194868 |doi=10.1016/j.ajogmf.2020.100113 |url=}}</ref><ref name="pmid32282027">{{cite journal |vauthors=Kim IC, Kim JY, Kim HA, Han S |title=COVID-19-related myocarditis in a 21-year-old female patient |journal=Eur Heart J |volume=41 |issue=19 |pages=1859 |date=May 2020 |pmid=32282027 |pmc=7184491 |doi=10.1093/eurheartj/ehaa288 |url=}}</ref><ref name="pmid32838265">{{cite journal |vauthors=Favre G, Pomar L, Baud D |title=Coronavirus disease 2019 during pregnancy: do not underestimate the risk of maternal adverse outcomes |journal=Am J Obstet Gynecol MFM |volume=2 |issue=3 |pages=100160 |date=August 2020 |pmid=32838265 |pmc=7367790 |doi=10.1016/j.ajogmf.2020.100160 |url=}}</ref><ref name="pmid32462177">{{cite journal |vauthors=Sardari A, Tabarsi P, Borhany H, Mohiaddin R, Houshmand G |title=Myocarditis detected after COVID-19 recovery |journal=Eur Heart J Cardiovasc Imaging |volume=22 |issue=1 |pages=131–132 |date=January 2021 |pmid=32462177 |pmc=7574602 |doi=10.1093/ehjci/jeaa166 |url=}}</ref><ref name="pmid32397816">{{cite journal |vauthors=Luetkens JA, Isaak A, Zimmer S, Nattermann J, Sprinkart AM, Boesecke C, Rieke GJ, Zachoval C, Heine A, Velten M, Duerr GD |title=Diffuse Myocardial Inflammation in COVID-19 Associated Myocarditis Detected by Multiparametric Cardiac Magnetic Resonance Imaging |journal=Circ Cardiovasc Imaging |volume=13 |issue=5 |pages=e010897 |date=May 2020 |pmid=32397816 |doi=10.1161/CIRCIMAGING.120.010897 |url=}}</ref><ref name="pmid33111813">{{cite journal |vauthors=Yokoo P, Fonseca EKUN, Sasdelli Neto R, Ishikawa WY, Silva MMA, Yanata E, Chate RC, Nunes Filho ACB, Bettega M, Fernandes JRC, Tarasoutchi F, Szarf G |title=COVID-19 myocarditis: a case report |journal=Einstein (Sao Paulo) |volume=18 |issue= |pages=eRC5876 |date=2020 |pmid=33111813 |pmc=7575039 |doi=10.31744/einstein_journal/2020RC5876 |url=}}</ref><ref name="pmid32817822">{{cite journal |vauthors=Khalid Y, Dasu N, Dasu K |title=A case of novel coronavirus (COVID-19)-induced viral myocarditis mimicking a Takotsubo cardiomyopathy |journal=HeartRhythm Case Rep |volume=6 |issue=8 |pages=473–476 |date=August 2020 |pmid=32817822 |pmc=7424304 |doi=10.1016/j.hrcr.2020.05.020 |url=}}</ref> | ||
* Normal [[ECG]] | |||
* [[Sinus tachycardia]] | |||
* [[ST-segment elevation]] | |||
* [[T wave inversion]] | |||
* | * [[ST depression]] | ||
* [[Atrial fibrillation]] | |||
* [[PVCs]] | |||
* [[Supraventricular tachycardia]] | |||
=== Echocardiography === | === Echocardiography === | ||
* | * Common findings of [[echocardiography]] among reported cases of [[myocarditis]] associated [[covid-19]] are:<ref name="pmid32986861">{{cite journal |vauthors=Ejarque M, Sabadell-Basallote J, Beiroa D, Calvo E, Keiran N, Nuñez-Roa C, Rodríguez MDM, Sabench F, Del Castillo D, Jimenez V, Bosch F, Nogueiras R, Vendrell J, Fernández-Veledo S |title=Adipose tissue is a key organ for the beneficial effects of GLP-2 metabolic function |journal=Br J Pharmacol |volume=178 |issue=10 |pages=2131–2145 |date=May 2021 |pmid=32986861 |doi=10.1111/bph.15278 |url=}}</ref><ref name="pmid32835276">{{cite journal |vauthors=Garot J, Amour J, Pezel T, Dermoch F, Messadaa K, Felten ML, Raymond V, Baubillier E, Sanguineti F, Garot P |title=SARS-CoV-2 Fulminant Myocarditis |journal=JACC Case Rep |volume=2 |issue=9 |pages=1342–1346 |date=July 2020 |pmid=32835276 |pmc=7274592 |doi=10.1016/j.jaccas.2020.05.060 |url=}}</ref><ref name="pmid34235815">{{cite journal |vauthors=Rathore SS, Rojas GA, Sondhi M, Pothuru S, Pydi R, Kancherla N, Singh R, Ahmed NK, Shah J, Tousif S, Baloch UT, Wen Q |title=Myocarditis associated with Covid-19 disease: A systematic review of published case reports and case series |journal=Int J Clin Pract |volume= |issue= |pages=e14470 |date=July 2021 |pmid=34235815 |doi=10.1111/ijcp.14470 |url=}}</ref><ref name="HanKim2020">{{cite journal|last1=Han|first1=Seongwook|last2=Kim|first2=Hyun Ah|last3=Kim|first3=Jin Young|last4=Kim|first4=In-Cheol|title=COVID-19-related myocarditis in a 21-year-old female patient|journal=European Heart Journal|volume=41|issue=19|year=2020|pages=1859–1859|issn=0195-668X|doi=10.1093/eurheartj/ehaa288}}</ref><ref name="InciardiLupi2020">{{cite journal|last1=Inciardi|first1=Riccardo M.|last2=Lupi|first2=Laura|last3=Zaccone|first3=Gregorio|last4=Italia|first4=Leonardo|last5=Raffo|first5=Michela|last6=Tomasoni|first6=Daniela|last7=Cani|first7=Dario S.|last8=Cerini|first8=Manuel|last9=Farina|first9=Davide|last10=Gavazzi|first10=Emanuele|last11=Maroldi|first11=Roberto|last12=Adamo|first12=Marianna|last13=Ammirati|first13=Enrico|last14=Sinagra|first14=Gianfranco|last15=Lombardi|first15=Carlo M.|last16=Metra|first16=Marco|title=Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)|journal=JAMA Cardiology|year=2020|issn=2380-6583|doi=10.1001/jamacardio.2020.1096}}</ref><ref name="ZengLiu2020">{{cite journal|last1=Zeng|first1=Jia-Hui|last2=Liu|first2=Ying-Xia|last3=Yuan|first3=Jing|last4=Wang|first4=Fu-Xiang|last5=Wu|first5=Wei-Bo|last6=Li|first6=Jin-Xiu|last7=Wang|first7=Li-Fei|last8=Gao|first8=Hong|last9=Wang|first9=Yao|last10=Dong|first10=Chang-Feng|last11=Li|first11=Yi-Jun|last12=Xie|first12=Xiao-Juan|last13=Feng|first13=Cheng|last14=Liu|first14=Lei|title=First case of COVID-19 complicated with fulminant myocarditis: a case report and insights|journal=Infection|year=2020|issn=0300-8126|doi=10.1007/s15010-020-01424-5}}</ref><ref name="pmid32219357">{{cite journal |vauthors=Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M |title=Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19) |journal=JAMA Cardiol |volume=5 |issue=7 |pages=819–824 |date=July 2020 |pmid=32219357 |pmc=7364333 |doi=10.1001/jamacardio.2020.1096 |url=}}</ref> | ||
*: [[Decreased ]] [[left ventricular ejection fraction]] with mean [[LVEF]] about 37% (the most common finding) | |||
*:[[Left ventricular hypokinesia]] | |||
*:[[Left ventricular dilation]] | |||
*:[[Pericardial effusion]] | |||
*:[[Mitral regurgitation]] | |||
*:Increased [[left ventricular]] wall thickness | |||
*: [[Right ventricular dilation]] | |||
=== Cardiac Magnetic Resonance === | === Cardiac Magnetic Resonance === | ||
*[[Cardiovascular magnetic resonance imaging (CMR)|Cardiac Magnetic Resonance (CMR)]] imaging is a | *[[Cardiovascular magnetic resonance imaging (CMR)|Cardiac Magnetic Resonance (CMR)]] imaging is useful as a noninvasive goldstandard technique in the diagnosis of [[myocarditis]].<ref name="EzekowitzO'Meara2017">{{cite journal|last1=Ezekowitz|first1=Justin A.|last2=O'Meara|first2=Eileen|last3=McDonald|first3=Michael A.|last4=Abrams|first4=Howard|last5=Chan|first5=Michael|last6=Ducharme|first6=Anique|last7=Giannetti|first7=Nadia|last8=Grzeslo|first8=Adam|last9=Hamilton|first9=Peter G.|last10=Heckman|first10=George A.|last11=Howlett|first11=Jonathan G.|last12=Koshman|first12=Sheri L.|last13=Lepage|first13=Serge|last14=McKelvie|first14=Robert S.|last15=Moe|first15=Gordon W.|last16=Rajda|first16=Miroslaw|last17=Swiggum|first17=Elizabeth|last18=Virani|first18=Sean A.|last19=Zieroth|first19=Shelley|last20=Al-Hesayen|first20=Abdul|last21=Cohen-Solal|first21=Alain|last22=D'Astous|first22=Michel|last23=De|first23=Sabe|last24=Estrella-Holder|first24=Estrellita|last25=Fremes|first25=Stephen|last26=Green|first26=Lee|last27=Haddad|first27=Haissam|last28=Harkness|first28=Karen|last29=Hernandez|first29=Adrian F.|last30=Kouz|first30=Simon|last31=LeBlanc|first31=Marie-Hélène|last32=Masoudi|first32=Frederick A.|last33=Ross|first33=Heather J.|last34=Roussin|first34=Andre|last35=Sussex|first35=Bruce|title=2017 Comprehensive Update of the Canadian Cardiovascular Society Guidelines for the Management of Heart Failure|journal=Canadian Journal of Cardiology|volume=33|issue=11|year=2017|pages=1342–1433|issn=0828282X|doi=10.1016/j.cjca.2017.08.022}}</ref> | ||
*Common findings of [[CMR]] in T2-Weighted images in [[myocarditis ]] associated [[COVID-19]] among reported cases include:<ref name="pmid34235815">{{cite journal |vauthors=Rathore SS, Rojas GA, Sondhi M, Pothuru S, Pydi R, Kancherla N, Singh R, Ahmed NK, Shah J, Tousif S, Baloch UT, Wen Q |title=Myocarditis associated with Covid-19 disease: A systematic review of published case reports and case series |journal=Int J Clin Pract |volume= |issue= |pages=e14470 |date=July 2021 |pmid=34235815|doi=10.1111/ijcp.14470 |url=}}</ref> | |||
*:[[Myocardial edema]] | |||
*:Sub-epicardial late gadolinium enhancement | |||
* Above findings in [[CMR]] are indicativeve of [[myocardial injury]] leading to [[necrosis]] and [[fibrosis]]. | |||
*[[Cardiovascular magnetic resonance imaging (CMR)|Cardiac Magnetic resonance (CMR)]] has major imaging advantages with highest diagnostic accuracy over [[echocardiography]].<ref name="FriedrichStrohm1998">{{cite journal|last1=Friedrich|first1=Matthias G.|last2=Strohm|first2=Oliver|last3=Schulz-Menger|first3=Jeanette|last4=Marciniak|first4=Heinz|last5=Luft|first5=Friedrich C.|last6=Dietz|first6=Rainer|title=Contrast Media–Enhanced Magnetic Resonance Imaging Visualizes Myocardial Changes in the Course of Viral Myocarditis|journal=Circulation|volume=97|issue=18|year=1998|pages=1802–1809|issn=0009-7322|doi=10.1161/01.CIR.97.18.1802}}</ref> | *[[Cardiovascular magnetic resonance imaging (CMR)|Cardiac Magnetic resonance (CMR)]] has major imaging advantages with highest diagnostic accuracy over [[echocardiography]].<ref name="FriedrichStrohm1998">{{cite journal|last1=Friedrich|first1=Matthias G.|last2=Strohm|first2=Oliver|last3=Schulz-Menger|first3=Jeanette|last4=Marciniak|first4=Heinz|last5=Luft|first5=Friedrich C.|last6=Dietz|first6=Rainer|title=Contrast Media–Enhanced Magnetic Resonance Imaging Visualizes Myocardial Changes in the Course of Viral Myocarditis|journal=Circulation|volume=97|issue=18|year=1998|pages=1802–1809|issn=0009-7322|doi=10.1161/01.CIR.97.18.1802}}</ref> | ||
<ref name="FriedrichSechtem2009">{{cite journal|last1=Friedrich|first1=Matthias G.|last2=Sechtem|first2=Udo|last3=Schulz-Menger|first3=Jeanette|last4=Holmvang|first4=Godtfred|last5=Alakija|first5=Pauline|last6=Cooper|first6=Leslie T.|last7=White|first7=James A.|last8=Abdel-Aty|first8=Hassan|last9=Gutberlet|first9=Matthias|last10=Prasad|first10=Sanjay|last11=Aletras|first11=Anthony|last12=Laissy|first12=Jean-Pierre|last13=Paterson|first13=Ian|last14=Filipchuk|first14=Neil G.|last15=Kumar|first15=Andreas|last16=Pauschinger|first16=Matthias|last17=Liu|first17=Peter|title=Cardiovascular Magnetic Resonance in Myocarditis: A JACC White Paper|journal=Journal of the American College of Cardiology|volume=53|issue=17|year=2009|pages=1475–1487|issn=07351097|doi=10.1016/j.jacc.2009.02.007}}</ref> | |||
*[[Cardiovascular magnetic resonance imaging (CMR)|CMR]] using the revised Lake Louise consensus criteria to interpret the results has a [[specificity]] of up to 91% and a [[sensitivity]] of 67% for diagnosing [[myocarditis]] | *[[Cardiovascular magnetic resonance imaging (CMR)|CMR]] using the revised Lake Louise consensus criteria to interpret the results has a [[specificity]] of up to 91% and a [[sensitivity]] of 67% for diagnosing [[myocarditis]] with the findings of:<ref name="FriedrichSechtem2009">{{cite journal|last1=Friedrich|first1=Matthias G.|last2=Sechtem|first2=Udo|last3=Schulz-Menger|first3=Jeanette|last4=Holmvang|first4=Godtfred|last5=Alakija|first5=Pauline|last6=Cooper|first6=Leslie T.|last7=White|first7=James A.|last8=Abdel-Aty|first8=Hassan|last9=Gutberlet|first9=Matthias|last10=Prasad|first10=Sanjay|last11=Aletras|first11=Anthony|last12=Laissy|first12=Jean-Pierre|last13=Paterson|first13=Ian|last14=Filipchuk|first14=Neil G.|last15=Kumar|first15=Andreas|last16=Pauschinger|first16=Matthias|last17=Liu|first17=Peter|title=Cardiovascular Magnetic Resonance in Myocarditis: A JACC White Paper|journal=Journal of the American College of Cardiology|volume=53|issue=17|year=2009|pages=1475–1487|issn=07351097|doi=10.1016/j.jacc.2009.02.007}}</ref> | ||
**1) [[Edema]] | **1) [[Edema]] | ||
**2) Irreversible [[Cell (biology)|cell]] injury | **2) Irreversible [[Cell (biology)|cell]] injury | ||
**3) [[Hyperemia]] or [[capillary]] leak | **3) [[Hyperemia]] or [[capillary]] leak.<ref name="HanChen2020">{{cite journal|last1=Han|first1=Yuchi|last2=Chen|first2=Tiffany|last3=Bryant|first3=Jennifer|last4=Bucciarelli-Ducci|first4=Chiara|last5=Dyke|first5=Christopher|last6=Elliott|first6=Michael D.|last7=Ferrari|first7=Victor A.|last8=Friedrich|first8=Matthias G.|last9=Lawton|first9=Chris|last10=Manning|first10=Warren J.|last11=Ordovas|first11=Karen|last12=Plein|first12=Sven|last13=Powell|first13=Andrew J.|last14=Raman|first14=Subha V.|last15=Carr|first15=James|title=Society for Cardiovascular Magnetic Resonance (SCMR) guidance for the practice of cardiovascular magnetic resonance during the COVID-19 pandemic|journal=Journal of Cardiovascular Magnetic Resonance|volume=22|issue=1|year=2020|issn=1532-429X|doi=10.1186/s12968-020-00628-w}}</ref>.<ref name="InciardiLupi2020">{{cite journal|last1=Inciardi|first1=Riccardo M.|last2=Lupi|first2=Laura|last3=Zaccone|first3=Gregorio|last4=Italia|first4=Leonardo|last5=Raffo|first5=Michela|last6=Tomasoni|first6=Daniela|last7=Cani|first7=Dario S.|last8=Cerini|first8=Manuel|last9=Farina|first9=Davide|last10=Gavazzi|first10=Emanuele|last11=Maroldi|first11=Roberto|last12=Adamo|first12=Marianna|last13=Ammirati|first13=Enrico|last14=Sinagra|first14=Gianfranco|last15=Lombardi|first15=Carlo M.|last16=Metra|first16=Marco|title=Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)|journal=JAMA Cardiology|year=2020|issn=2380-6583|doi=10.1001/jamacardio.2020.1096}}</ref><ref name="HanKim2020">{{cite journal|last1=Han|first1=Seongwook|last2=Kim|first2=Hyun Ah|last3=Kim|first3=Jin Young|last4=Kim|first4=In-Cheol|title=COVID-19-related myocarditis in a 21-year-old female patient|journal=European Heart Journal|volume=41|issue=19|year=2020|pages=1859–1859|issn=0195-668X|doi=10.1093/eurheartj/ehaa288}}</ref><ref name="EspositoGodino2020">{{cite journal|last1=Esposito|first1=Antonio|last2=Godino|first2=Cosmo|last3=Basso|first3=Cristina|last4=Cappelletti|first4=Alberto Maria|last5=Tresoldi|first5=Moreno|last6=De Cobelli|first6=Francesco|last7=Vignale|first7=Davide|last8=Villatore|first8=Andrea|last9=Palmisano|first9=Anna|last10=Gramegna|first10=Mario|last11=Peretto|first11=Giovanni|last12=Sala|first12=Simone|title=Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection|journal=European Heart Journal|volume=41|issue=19|year=2020|pages=1861–1862|issn=0195-668X|doi=10.1093/eurheartj/ehaa286}}</ref><ref name="CoyleIgbinomwanhia2020">{{cite journal|last1=Coyle|first1=Justin|last2=Igbinomwanhia|first2=Efehi|last3=Sanchez-Nadales|first3=Alejandro|last4=Danciu|first4=Sorin|last5=Chu|first5=Chae|last6=Shah|first6=Nishit|title=A Recovered Case of COVID-19 Myocarditis and ARDS Treated With Corticosteroids, Tocilizumab, and Experimental AT-001|journal=JACC: Case Reports|year=2020|issn=26660849|doi=10.1016/j.jaccas.2020.04.025}}</ref><ref name="DoyenMoceri2020">{{cite journal|last1=Doyen|first1=Denis|last2=Moceri|first2=Pamela|last3=Ducreux|first3=Dorothée|last4=Dellamonica|first4=Jean|title=Myocarditis in a patient with COVID-19: a cause of raised troponin and ECG changes|journal=The Lancet|volume=395|issue=10235|year=2020|pages=1516|issn=01406736|doi=10.1016/S0140-6736(20)30912-0}}</ref><ref name="LuetkensIsaak2020">{{cite journal|last1=Luetkens|first1=Julian Alexander|last2=Isaak|first2=Alexander|last3=Zimmer|first3=Sebastian|last4=Nattermann|first4=Jacob|last5=Sprinkart|first5=Alois Martin|last6=Boesecke|first6=Christoph|last7=Rieke|first7=Gereon Jonas|last8=Zachoval|first8=Christian|last9=Heine|first9=Annkristin|last10=Velten|first10=Markus|last11=Duerr|first11=Georg Daniel|title=Diffuse Myocardial Inflammation in COVID-19 Associated Myocarditis Detected by Multiparametric Cardiac Magnetic Resonance Imaging|journal=Circulation: Cardiovascular Imaging|volume=13|issue=5|year=2020|issn=1941-9651|doi=10.1161/CIRCIMAGING.120.010897}}</ref> | ||
*Among reported cases in [[CMR]], [[myocardial edema]] and/or [[scarring]] were detected in all of the [[COVID-19]] associated [[myocarditis]]. | |||
=== Cardiac Computed Tomography === | === Cardiac Computed Tomography === | ||
Cardiac Computed Tomography cab be useful for [[diagnosis]] of [[myocarditis]] in [[covid-19]]. | |||
*[[ | :*Findings of [[myocarditis]] associated [[covid-19]] in [[cardiac CT scan]] include:<ref name="HanKim2020">{{cite journal|last1=Han|first1=Seongwook|last2=Kim|first2=Hyun Ah|last3=Kim|first3=Jin Young|last4=Kim|first4=In-Cheol|title=COVID-19-related myocarditis in a 21-year-old female patient|journal=European Heart Journal|volume=41|issue=19|year=2020|pages=1859–1859|issn=0195-668X|doi=10.1093/eurheartj/ehaa288}}</ref> | ||
* Lung involvement such as multifocal [[consolidation]], ground-glass opacification, peripheral dominant distribution | |||
*[[Hypertrophy]] of [[myocardium]] due to [[edema]] and [[subendocardium perfusion defect ]] | |||
* Coronary arteries patency or [[obstruction]] | |||
=== Endomyocardial biopsy === | === Endomyocardial biopsy === | ||
| Line 183: | Line 267: | ||
=== Medical Therapy === | === Medical Therapy === | ||
* | *The mainstay of therapy is supportive care. | ||
*As per [[American Heart Association|AHA]] recommendations, in the patients of [[fulminant myocarditis]], initial management includes the protocol of [[cardiogenic shock]] which is the administration of [[inotropes]] and/[[vasopressors]] and [[mechanical ventilation]]; and use of [[extracorporeal membrane oxygenation]]([[ECMO]]), [[ventricular assist device|ventricular assistive devices]] ([[VAD]]) in severe cases.<ref name="ZengLiu2020">{{cite journal|last1=Zeng|first1=Jia-Hui|last2=Liu|first2=Ying-Xia|last3=Yuan|first3=Jing|last4=Wang|first4=Fu-Xiang|last5=Wu|first5=Wei-Bo|last6=Li|first6=Jin-Xiu|last7=Wang|first7=Li-Fei|last8=Gao|first8=Hong|last9=Wang|first9=Yao|last10=Dong|first10=Chang-Feng|last11=Li|first11=Yi-Jun|last12=Xie|first12=Xiao-Juan|last13=Feng|first13=Cheng|last14=Liu|first14=Lei|title=First case of COVID-19 complicated with fulminant myocarditis: a case report and insights|journal=Infection|year=2020|issn=0300-8126|doi=10.1007/s15010-020-01424-5}}</ref><ref name="RaoSasser2014">{{cite journal|last1=Rao|first1=Sangeetha|last2=Sasser|first2=William|last3=Diaz|first3=Franco|last4=Sharma|first4=Nirmal|last5=Alten|first5=Jeffrey|title=Coronavirus Associated Fulminant Myocarditis Successfully Treated With Intravenous Immunoglobulin and Extracorporeal Membrane Oxygenation|journal=Chest|volume=146|issue=4|year=2014|pages=336A|issn=00123692|doi=10.1378/chest.1992018}}</ref><ref name="Irabien-OrtizCarreras-Mora2020">{{cite journal|last1=Irabien-Ortiz|first1=Ángela|last2=Carreras-Mora|first2=José|last3=Sionis|first3=Alessandro|last4=Pàmies|first4=Julia|last5=Montiel|first5=José|last6=Tauron|first6=Manel|title=Fulminant myocarditis due to COVID-19|journal=Revista Española de Cardiología (English Edition)|volume=73|issue=6|year=2020|pages=503–504|issn=18855857|doi=10.1016/j.rec.2020.04.005}}</ref><ref name="InciardiLupi2020" /><ref name="FangWei2020" /> | *As per [[American Heart Association|AHA]] recommendations, in the patients of [[fulminant myocarditis]], initial management includes the protocol of [[cardiogenic shock]] which is the administration of [[inotropes]] and/[[vasopressors]] and [[mechanical ventilation]]; and use of [[extracorporeal membrane oxygenation]]([[ECMO]]), [[ventricular assist device|ventricular assistive devices]] ([[VAD]]) in severe cases.<ref name="ZengLiu2020">{{cite journal|last1=Zeng|first1=Jia-Hui|last2=Liu|first2=Ying-Xia|last3=Yuan|first3=Jing|last4=Wang|first4=Fu-Xiang|last5=Wu|first5=Wei-Bo|last6=Li|first6=Jin-Xiu|last7=Wang|first7=Li-Fei|last8=Gao|first8=Hong|last9=Wang|first9=Yao|last10=Dong|first10=Chang-Feng|last11=Li|first11=Yi-Jun|last12=Xie|first12=Xiao-Juan|last13=Feng|first13=Cheng|last14=Liu|first14=Lei|title=First case of COVID-19 complicated with fulminant myocarditis: a case report and insights|journal=Infection|year=2020|issn=0300-8126|doi=10.1007/s15010-020-01424-5}}</ref><ref name="RaoSasser2014">{{cite journal|last1=Rao|first1=Sangeetha|last2=Sasser|first2=William|last3=Diaz|first3=Franco|last4=Sharma|first4=Nirmal|last5=Alten|first5=Jeffrey|title=Coronavirus Associated Fulminant Myocarditis Successfully Treated With Intravenous Immunoglobulin and Extracorporeal Membrane Oxygenation|journal=Chest|volume=146|issue=4|year=2014|pages=336A|issn=00123692|doi=10.1378/chest.1992018}}</ref><ref name="Irabien-OrtizCarreras-Mora2020">{{cite journal|last1=Irabien-Ortiz|first1=Ángela|last2=Carreras-Mora|first2=José|last3=Sionis|first3=Alessandro|last4=Pàmies|first4=Julia|last5=Montiel|first5=José|last6=Tauron|first6=Manel|title=Fulminant myocarditis due to COVID-19|journal=Revista Española de Cardiología (English Edition)|volume=73|issue=6|year=2020|pages=503–504|issn=18855857|doi=10.1016/j.rec.2020.04.005}}</ref><ref name="InciardiLupi2020" /><ref name="FangWei2020" /> | ||
*This protocol has been the mainstay of treatment in [[COVID-19]]-associated [[myocarditis]] cases as well and proved beneficial in mitigating [[systolic dysfunction|ventricular systolic dysfunction]]. | *This protocol has been the mainstay of treatment in [[COVID-19]]-associated [[myocarditis]] cases as well and proved beneficial in mitigating [[systolic dysfunction|ventricular systolic dysfunction]]. | ||
| Line 197: | Line 281: | ||
===Primary Prevention=== | ===Primary Prevention=== | ||
*There are no established measures for the primary prevention of [[COVID-19]]-associated [[myocarditis]]. | *There are no established measures for the primary prevention of [[COVID-19]]-associated [[myocarditis]]. | ||
*For primary preventive measures of [COVID-19], [[COVID-19 primary prevention|click here]]. | *For primary preventive measures of [[COVID-19]], [[COVID-19 primary prevention|click here]]. | ||
===Secondary Prevention=== | ===Secondary Prevention=== | ||
*There are no established measures for the secondary prevention of [[COVID-19]]-associated [[myocarditis]]. | *There are no established measures for the secondary prevention of [[COVID-19]]-associated [[myocarditis]]. | ||
*For secondary preventive measures of [COVID-19], [[COVID-19 secondary prevention|click here]]. | *For secondary preventive measures of [[COVID-19]], [[COVID-19 secondary prevention|click here]]. | ||
==References== | ==References== | ||
Latest revision as of 06:27, 12 November 2021
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
For COVID-19 patient information, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Zand, M.D.[2] Mounika Reddy Vadiyala, M.B.B.S.[3]
Synonyms and keywords: Novel coronavirus, COVID-19, Wuhan coronavirus, coronavirus disease-19, coronavirus disease 2019, SARS-CoV-2, COVID-19, COVID-19, 2019-nCoV, 2019 novel coronavirus, cardiovascular finding in COVID-19, myocardial injury in COVID-19, myocarditis, myocarditis in COVID-19, COVID-19-associated myocarditis, SARS-CoV2-associated myocarditis, myocardial injury in COVID-19, COVID-19 myocarditis
Overview
COVID-19 caused by the novel coronavirus, also known as SARS-CoV-2 mainly affects the lungs may lead to severe acute respiratory syndrome (SARS). It invades through the angiotensin-converting enzyme 2 (ACE2) receptors present abundantly not only in the lungs but also in the heart, kidneys, intestine, brain, skin thus causing multiorgan dysfunction including cardiovascular complications and death. Myocarditis is one of the cardiovascular manifestation of COVID-19 which is the inflammation of myocardium without stenosis in coronary arteries, with the risk of arrhythmia as well as progression to fulminant heart failure and cardiogenic shock. The proposed mechanisms including direct invasion through ACE2 receptors and inflammatory response or cytokine storm. In literature, myocardial edema and/or scarring were detected on cardiac MRI of reported myocarditis associated COVID-19.
Historical Perspective
- The novel coronavirus, SARS-CoV-2, is identified as the cause of an outbreak of respiratory illness first detected in Wuhan, China in late December 2019. It was named SARS-CoV-2 for its similarity severe acute respiratory syndrome related coronaviruses such as SARS-CoV, which caused acute respiratory distress syndrome (ARDS) in 2002–2003.[1][2]
- On January 30, 2020,the World Health Organization(WHO) declared the outbreak as a Public Health Emergency of International Concern.
- On March 12, 2020, the World Health Organization declared the COVID-19 outbreak a pandemic.
- On March 27, 2020, Inciardi et al., from Italy, reported the first case of acute myocardial inflammation in a patient with COVID-19.[3]
Classification
- There is no established system for the classification of the myocarditis seen in COVID-19.
- For general classification of myocarditis, click here.
Pathophysiology
- Myocarditis is an inflammatory disease of the heart characterized by inflammatory infiltrates and myocardial injury without an ischemic cause.[4]
- The major cause of myocarditis in the United States and other developed countries is viral.[5] [6]
- The exact mechanisms of COVID-19 induced myocarditis are not yet well known, although several have been proposed based on the limited data outside of case reports.
Proposed pathophysiologies of COVID-19 associated myocarditis
- Direct myocardial injury by binding of SARS-COV-2 virus through ACE2 receptors
- Systemic inflammatory response syndrome (SIRS)
- Increased level of metabolic requirement along with lower supply due to hypoxia leading to supply-demand mismatch
- Diffuse vasculitis and endothelial inflammation in the heart[7]
- Direct invasion of the virus into cardiomyocytes:
- COVID-19 infection is caused by receptor-mediated endocytosis via binding of the viral surface spike protein (primed by TMPRSS2 - Transmembrane Protease Serine 2) to the human angiotensin-converting enzyme 2 (ACE2) receptor.[8][9]
- ACE2 is expressed in the lung, principally type II alveolar cells which appears to be the principal portal of entry.[10]
- ACE2 is highly expressed in the heart as well.[11]
- However, there are limited reports showing pathological evidence that COVID-19 directly invades the heart.[12]
- Hyperinflammation and Cytokine storm
- Naive T lymphocytes can be primed for viral antigens via antigen-presenting cells.[13]
- The primed CD8+ T lymphocytes migrate to the cardiomyocytes and through cell-mediated cytotoxicity, cause myocardial inflammation and cardio-tropism by heart-produced Hepatocyte Growth Factor (HGF) which interacts with c-Met, an HGF receptor on naïve T lymphocytes.[13]
- In the cytokine storm syndrome, proinflammatory cytokines such as Interleukin-6 (IL-6) are released into the circulation, which further augments T-lymphocyte activation and causes the release of more cytokines.[14]
- Cytokine storms result in increased vascular wall permeabilityand myocardial edema.[15][16]
- A positive feedback loop of immune activation and myocardial damage is established.[17][4]
- Thus cytokine storm activated by T helper cells (Th1 and Th2) and a systemic hyperinflammatory response is triggered.[18][19]
Pathological changes in the myocardium
- They could be due to viral replication in the myocardium or immune responses caused by the infection or due to systemic responses to respiratory failure.
- Interstitial mononuclear inflammatory infiltration has been observed in the heart tissue in COVID-19 autopsy studies.[20]
- In one of the autopsy studies of myocarditis in COVID-19, the viral particles were observed in interstitial cytopathic macrophages. Cardiac myocytes showed non‐specific features consisting of focal myofibrillar lysis, and lipid droplets but no viral particles in myocytes and endothelia; small intramural vessels were free from vasculitis and thrombosis.[12]
- Diffuse lymphocytic inflammatory infiltration was the most common histopathologic finding among 42 cases of myocarditis associated COVID-19 in literature.[7]
Causes
Myocarditis in COVID-19 is caused by:
- Direct invasion of endothelial cells by SARS-CoV-2
- Pro-inflammatory cytokine storm
Differentiating COVID-19 associated myocarditis from other Diseases
For further information about the differential diagnosis, click here.
For further information about the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
- The incidence of myocarditis was 7000 per 100,000 patients who died of covid-19. [22]
- The incidence of myocardial injury among patients with COVID-19 was approximately 24,400 per 100,000 hospitalized COVID-19 patients.[23]
- In a cohort study the incidence of acute cardiac injury caused by COVID-19 was 19.7% of patients out of 416 hospitalized covid-19 patients whether the portion of them is believed to be myocarditis.[24]
- There are some case reports of myocarditis related to COVID-19.[24][16][3][15][25][26][12][27][28][29]
Age
- Among reported cases in the literature, myocarditis associated COVID-19 was more commonly observed among patients with a median age of 43.4 years.[7]
- Myocarditis after vaccination of covid-19 was commonly observed in young male.[30]
Gender
- Males are more commonly affected with myocarditis associated COVID-19 than females based on the reported cases in literature.
Race
- There is no data on racial predilection to myocarditis in COVID-19.
Risk Factors
- There are no established risk factors for myocarditis associated COVID-19. However, concomitant cardiac comorbidities may present with myocarditis.
Screening
- There is insufficient evidence to recommend routine screening for myocarditis in COVID-19 patients.
Natural History, Complications and Prognosis
Natural history
- In the presence of SARS-COV-2 cells in the myocardium, early clinical features include acute heart failure, refractory ventricular tachycardia, reduced left ventricular ejection fraction and rapidly develop to death.[31]
- Patients with the presentation of third-degree AV block, ventricular tachycardia, and ventricular fibrillation may progress to develope cardiac arrest and in-hospital death in the context of fulminant myocarditis.
- In the course of covid-19 infection, myocarditis is often a relatively late event.[31]
- Cardiac infection by SARS-CoV-2 is associated with more electrocardiographic changes.
- Atrial fibrillation was the most common arrhythmia in such patients and was associated with poor outcome.[32][31]
- If left untreated, myocarditis in patients with COVID-19 may progress to cardiogenic shock, heart failure, and eventually may lead to death.[27][33]
Complications
Common complications of myocarditis include:
- Dilated cardiomyopathy
- Acute-onset heart failure
- Pericarditis
- Ventricular dysfunction
- Arrhythmias
- Sudden cardiac death
Prognosis
- Prognosis was generally good and the majority of patients (81%) of reported cases survived, and mortality rate was 19% among reported cases.[34]
| Age, sex | Cardiovascular history | Symptoms | Laboratory findings | Timing according to covid-19 infection | Concomitant covid-19 complications | Covid-19 severity | Diagnosis | Pathology | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 45 years, male[35] | Hypertension, diabetes mellitus | First symptoms: fever, mild dyspnea, fatigue turned to severe dyspnea, confusion and cardiogenic shock | High levels of troponin, CRP, NT-Pro BNP, mild leukocytosis, thrombocytopenia, | 5 days | Sinus tachycardia, low peripheral voltage, diffuse repolarization abnormalities | Mild ground glass opacification in chest CT scan, severe biventricular dysfunction in echocardiography, absent of late gadolinium enhancement on cardiac MRI | Myocarditis due to massive cytokine storm of COVID-19 regardless the absence of SARS-COV-2 RNA in EBM | Mild lymphohistiocytic inflammatory infiltration, without myocardial necrosis, positive parvovirus B19, but not SARS-COV-2 RNA | IABP, noradrenalin, hydroxychloroquine, steroid therapy, antibiotics, Levosimendan, IL-1inhibitor (anakinra), | Improving LVEF to 40-45% , TAPSE=18mm few day later and normalized biventricular function on CMR after 3 months, discharged with standard medications for heart failure therapy and a 6 month therapy with Anakinra 100 mg daily |
| 48 years, male[36] | Hypertension, diabetes mellitus, hyperlipidemia | Fever, dyspnea, hemoptesia | High levels of inflammatory and cardiac damage markers | unknown | No ischemia sign on ECG | Bilateral patchy peripheral ground glass with crazy-paving pattern in chest CT scan, reduced biventricular function in echocardiography, myocardial edema and late gadolinium enhancement in CMR | Myocarditis | Acute lymphocytic myocarditis, rheumatic vasculitis | Cyclophosphamide, steroide | Improvement |
| 81 years, male[37] | Hypertension, ischemic stroke | Fever, dyspnea, oxygen saturation of 91%, ARDS, acute cardiac dysfunction during admission | High levels of inflammatory and cardiac damage markers | 1 day | Small round ground glass opacities with multifocal distribution in both lungs field, specially in left perihilar region in chest CT scan, reduced LVEF in echocardiography, late gadolinium enhancement, ischemic pattern on base LV septum in CMR | Myocarditis | Antibiotic, steroid, hemodynamic monitoring | Improvement, discharged with anticoagulant |
Diagnosis
Diagnostic Criteria
- The diagnosis of myocarditis cannot be made with a single test or examination. When indicated, the diagnosis requires a combination of:
Signs and Symptoms
Clinical presentations have varied in the reported COVID-19 cases with myocarditis in the literature with potential overlap in symptomatology in patients with primary COVID-19 infection and COVID-19 patients with clinically suspected myocarditis. Clinical presentation of COVID-19 related myocarditis varies among cases from mild to severe to fulminant.
- Mild - fatigue and dyspnea, chest pain or chest tightness on exertion.[3][15][16][25]
- Severe - Many patients deteriorate and show symptoms of tachycardia and acute-onset heart failure with cardiogenic shock.[16][3][15]
- Patients may also present with signs of right-sided heart failure, including the following:[6]
- Fulminant - Fulminant myocarditis is defined as ventricular dysfunction and heart failure within 2–3 weeks of infection.[4][38][26][39]
- The early signs of fulminant myocarditis resemble those of sepsis: Fever, low pulse pressure, cold extremities, and sinus tachycardia.[6][16]
- According to a study, ventricular arrhythmia has also been known to occur in patients with myocarditis.[40]
Physical Examination
- Physical examination of patients with severe myocarditis may find:
- Physical examination of patients with fulminant myocarditis may find:
Laboratory Findings
Inflammatory biomarkers
- Elevated levels of inflammatory markers including erythrocyte sedimentation rate, C reactive protein, and procalcitonin are usually seen in myocarditis but they are not specific and do not confirm the diagnosis.
- Increases levels of Interleukin-6 (IL-6), d-dimer, serum ferritin, prothrombin time were seen in COVID-19 patients.[24][14]
Cardiac biomarkers
- Levels of cardiac enzymes such as cardiac troponins (cardiac troponin I(cTnI) and cardiac troponin T (cTnT)) and natriuretic peptides (N-terminal pro-B-type natriuretic peptide (NT-proBNP), and Brain natriuretic peptide (BNP)) usually are elevated in myocarditis due to acute myocardial injury and possible ventricular dilation.
- Elevations of both troponin and NT-proBNP levels were observed in the COVID-19–related myocarditis cases.[16][3][15][25][38][41]
- Elevated NT-proBNP level has been associated with worse clinical outcomes in severe COVID-19 patients.[42][43]
- Cardiac troponins and brain natriuretic peptides are sensitive but not specific in the diagnosis of myocarditis. It requires other supplementary findings and investigations.[44][45][46]
- Although a negative troponin result cannot exclude myocarditis, negative serial high-sensitivity cardiac troponin (hs-cTn) still is helpful in the acute phase and makes the diagnosis of acute myocarditis significantly less likely.[47]
Electrocardiogram
- Normal ECG
- Sinus tachycardia
- ST-segment elevation
- T wave inversion
- ST depression
- Atrial fibrillation
- PVCs
- Supraventricular tachycardia
Echocardiography
- Common findings of echocardiography among reported cases of myocarditis associated covid-19 are:[54][55][7][15][3][16][56]
- Decreased left ventricular ejection fraction with mean LVEF about 37% (the most common finding)
- Left ventricular hypokinesia
- Left ventricular dilation
- Pericardial effusion
- Mitral regurgitation
- Increased left ventricular wall thickness
- Right ventricular dilation
Cardiac Magnetic Resonance
- Cardiac Magnetic Resonance (CMR) imaging is useful as a noninvasive goldstandard technique in the diagnosis of myocarditis.[57]
- Common findings of CMR in T2-Weighted images in myocarditis associated COVID-19 among reported cases include:[7]
- Myocardial edema
- Sub-epicardial late gadolinium enhancement
- Above findings in CMR are indicativeve of myocardial injury leading to necrosis and fibrosis.
- Cardiac Magnetic resonance (CMR) has major imaging advantages with highest diagnostic accuracy over echocardiography.[58]
- CMR using the revised Lake Louise consensus criteria to interpret the results has a specificity of up to 91% and a sensitivity of 67% for diagnosing myocarditis with the findings of:[59]
- Among reported cases in CMR, myocardial edema and/or scarring were detected in all of the COVID-19 associated myocarditis.
Cardiac Computed Tomography
Cardiac Computed Tomography cab be useful for diagnosis of myocarditis in covid-19.
- Findings of myocarditis associated covid-19 in cardiac CT scan include:[15]
- Lung involvement such as multifocal consolidation, ground-glass opacification, peripheral dominant distribution
- Hypertrophy of myocardium due to edema and subendocardium perfusion defect
- Coronary arteries patency or obstruction
Endomyocardial biopsy
- Endomyocardial biopsy (EMB) has been recommended as the definitive diagnostic tool for myocarditis by the American Heart Association (AHA) and European Society of Cardiology (ESC).[61]
- In non–COVID-19 cases, endomyocardial biopsy has traditionally been recommended in fulminant presentations to exclude the rare presentation of eosinophilic, hypersensitive,and giant cell myocarditis.[62]
- However, in COVID-19, it may not be feasible because of the instability of the patient, requirement of expertise, false-negative rate and risk of contagiousness, especially if the biopsy results would not change clinical management.[5][6][58]
- EMB samples if obtained should be tested for inflammatory infiltrates and for the presence of viral genomes by DNA/RNA extraction.[5]
- In a COVID-19 case reported, EMB showed diffuse T-lymphocytic inflammatory infiltrates with huge interstitial edema and no replacement fibrosis, suggesting an acute inflammatory process. SARS-CoV-2 genome was absent within the myocardium in molecular analysis.[25]
Treatment
Medical Therapy
- The mainstay of therapy is supportive care.
- As per AHA recommendations, in the patients of fulminant myocarditis, initial management includes the protocol of cardiogenic shock which is the administration of inotropes and/vasopressors and mechanical ventilation; and use of extracorporeal membrane oxygenation(ECMO), ventricular assistive devices (VAD) in severe cases.[16][63][38][3][26]
- This protocol has been the mainstay of treatment in COVID-19-associated myocarditis cases as well and proved beneficial in mitigating ventricular systolic dysfunction.
- Though the European Society of Cardiology (ESC) did not approve the use of intravenous immunoglobulins (IVIG) and corticosteroids in active-infection myocarditis, COVID-19-associated myocarditis cases have been reported in which use of immunoglobulins and corticosteroids such as methylprednisolone and hydrocortisone have been beneficial.[26][16][3][41][27]
- Tocilizumab, an anti–IL-6 receptor monoclonal antibody, is being tested in a randomized controlled trial of COVID-19 patients with raised IL-6 levels.
- Tocilizumab, might be beneficial in the setting of cytokine storm syndrome and help reduce myocardial inflammation.[47]
- Although the cases of COVID-19 patients with myocarditis were treated with steroids and immunoglobulins, it is uncertain the incremental benefit these therapies might have provided over supportive care.
- Further evidence is needed to determine whether any combination of immunosuppression improves outcomes among patients with myocarditis in COVID-19.
Surgery
- Surgical intervention is not recommended for the management of COVID-19-associated myocarditis.
Primary Prevention
- There are no established measures for the primary prevention of COVID-19-associated myocarditis.
- For primary preventive measures of COVID-19, click here.
Secondary Prevention
- There are no established measures for the secondary prevention of COVID-19-associated myocarditis.
- For secondary preventive measures of COVID-19, click here.
References
- ↑ Lu, Jian; Cui, Jie; Qian, Zhaohui; Wang, Yirong; Zhang, Hong; Duan, Yuange; Wu, Xinkai; Yao, Xinmin; Song, Yuhe; Li, Xiang; Wu, Changcheng; Tang, Xiaolu (2020). "On the origin and continuing evolution of SARS-CoV-2". National Science Review. doi:10.1093/nsr/nwaa036. ISSN 2095-5138.
- ↑ Huang, Chaolin; Wang, Yeming; Li, Xingwang; Ren, Lili; Zhao, Jianping; Hu, Yi; Zhang, Li; Fan, Guohui; Xu, Jiuyang; Gu, Xiaoying; Cheng, Zhenshun; Yu, Ting; Xia, Jiaan; Wei, Yuan; Wu, Wenjuan; Xie, Xuelei; Yin, Wen; Li, Hui; Liu, Min; Xiao, Yan; Gao, Hong; Guo, Li; Xie, Jungang; Wang, Guangfa; Jiang, Rongmeng; Gao, Zhancheng; Jin, Qi; Wang, Jianwei; Cao, Bin (2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". The Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. ISSN 0140-6736.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Inciardi, Riccardo M.; Lupi, Laura; Zaccone, Gregorio; Italia, Leonardo; Raffo, Michela; Tomasoni, Daniela; Cani, Dario S.; Cerini, Manuel; Farina, Davide; Gavazzi, Emanuele; Maroldi, Roberto; Adamo, Marianna; Ammirati, Enrico; Sinagra, Gianfranco; Lombardi, Carlo M.; Metra, Marco (2020). "Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. doi:10.1001/jamacardio.2020.1096. ISSN 2380-6583.
- ↑ 4.0 4.1 4.2 Esfandiarei, Mitra; McManus, Bruce M. (2008). "Molecular Biology and Pathogenesis of Viral Myocarditis". Annual Review of Pathology: Mechanisms of Disease. 3 (1): 127–155. doi:10.1146/annurev.pathmechdis.3.121806.151534. ISSN 1553-4006.
- ↑ 5.0 5.1 5.2 Caforio, A. L. P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S. B.; Fu, M.; Helio, T.; Heymans, S.; Jahns, R.; Klingel, K.; Linhart, A.; Maisch, B.; McKenna, W.; Mogensen, J.; Pinto, Y. M.; Ristic, A.; Schultheiss, H.-P.; Seggewiss, H.; Tavazzi, L.; Thiene, G.; Yilmaz, A.; Charron, P.; Elliott, P. M. (2013). "Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases". European Heart Journal. 34 (33): 2636–2648. doi:10.1093/eurheartj/eht210. ISSN 0195-668X.
- ↑ 6.0 6.1 6.2 6.3 Kociol, Robb D.; Cooper, Leslie T.; Fang, James C.; Moslehi, Javid J.; Pang, Peter S.; Sabe, Marwa A.; Shah, Ravi V.; Sims, Daniel B.; Thiene, Gaetano; Vardeny, Orly (2020). "Recognition and Initial Management of Fulminant Myocarditis". Circulation. 141 (6). doi:10.1161/CIR.0000000000000745. ISSN 0009-7322.
- ↑ 7.0 7.1 7.2 7.3 7.4 Rathore SS, Rojas GA, Sondhi M, Pothuru S, Pydi R, Kancherla N, Singh R, Ahmed NK, Shah J, Tousif S, Baloch UT, Wen Q (July 2021). "Myocarditis associated with Covid-19 disease: A systematic review of published case reports and case series". Int J Clin Pract: e14470. doi:10.1111/ijcp.14470. PMID 34235815 Check
|pmid=value (help). - ↑ Hoffmann, Markus; Kleine-Weber, Hannah; Schroeder, Simon; Krüger, Nadine; Herrler, Tanja; Erichsen, Sandra; Schiergens, Tobias S.; Herrler, Georg; Wu, Nai-Huei; Nitsche, Andreas; Müller, Marcel A.; Drosten, Christian; Pöhlmann, Stefan (2020). "SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor". Cell. 181 (2): 271–280.e8. doi:10.1016/j.cell.2020.02.052. ISSN 0092-8674.
- ↑ Wan, Yushun; Shang, Jian; Graham, Rachel; Baric, Ralph S.; Li, Fang; Gallagher, Tom (2020). "Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade-Long Structural Studies of SARS Coronavirus". Journal of Virology. 94 (7). doi:10.1128/JVI.00127-20. ISSN 0022-538X.
- ↑ Zhao, Yu; Zhao, Zixian; Wang, Yujia; Zhou, Yueqing; Ma, Yu; Zuo, Wei (2020). doi:10.1101/2020.01.26.919985. Missing or empty
|title=(help) - ↑ Tikellis, Chris; Thomas, M. C. (2012). "Angiotensin-Converting Enzyme 2 (ACE2) Is a Key Modulator of the Renin Angiotensin System in Health and Disease". International Journal of Peptides. 2012: 1–8. doi:10.1155/2012/256294. ISSN 1687-9767.
- ↑ 12.0 12.1 12.2 Tavazzi, Guido; Pellegrini, Carlo; Maurelli, Marco; Belliato, Mirko; Sciutti, Fabio; Bottazzi, Andrea; Sepe, Paola Alessandra; Resasco, Tullia; Camporotondo, Rita; Bruno, Raffaele; Baldanti, Fausto; Paolucci, Stefania; Pelenghi, Stefano; Iotti, Giorgio Antonio; Mojoli, Francesco; Arbustini, Eloisa (2020). "Myocardial localization of coronavirus in COVID‐19 cardiogenic shock". European Journal of Heart Failure. 22 (5): 911–915. doi:10.1002/ejhf.1828. ISSN 1388-9842.
- ↑ 13.0 13.1 Komarowska, Izabela; Coe, David; Wang, Guosu; Haas, Robert; Mauro, Claudio; Kishore, Madhav; Cooper, Dianne; Nadkarni, Suchita; Fu, Hongmei; Steinbruchel, Daniel A.; Pitzalis, Costantino; Anderson, Graham; Bucy, Pat; Lombardi, Giovanna; Breckenridge, Ross; Marelli-Berg, Federica M. (2015). "Hepatocyte Growth Factor Receptor c-Met Instructs T Cell Cardiotropism and Promotes T Cell Migration to the Heart via Autocrine Chemokine Release". Immunity. 42 (6): 1087–1099. doi:10.1016/j.immuni.2015.05.014. ISSN 1074-7613.
- ↑ 14.0 14.1 Zhou, Fei; Yu, Ting; Du, Ronghui; Fan, Guohui; Liu, Ying; Liu, Zhibo; Xiang, Jie; Wang, Yeming; Song, Bin; Gu, Xiaoying; Guan, Lulu; Wei, Yuan; Li, Hui; Wu, Xudong; Xu, Jiuyang; Tu, Shengjin; Zhang, Yi; Chen, Hua; Cao, Bin (2020). "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study". The Lancet. 395 (10229): 1054–1062. doi:10.1016/S0140-6736(20)30566-3. ISSN 0140-6736.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 15.7 Han, Seongwook; Kim, Hyun Ah; Kim, Jin Young; Kim, In-Cheol (2020). "COVID-19-related myocarditis in a 21-year-old female patient". European Heart Journal. 41 (19): 1859–1859. doi:10.1093/eurheartj/ehaa288. ISSN 0195-668X.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 16.6 16.7 16.8 Zeng, Jia-Hui; Liu, Ying-Xia; Yuan, Jing; Wang, Fu-Xiang; Wu, Wei-Bo; Li, Jin-Xiu; Wang, Li-Fei; Gao, Hong; Wang, Yao; Dong, Chang-Feng; Li, Yi-Jun; Xie, Xiao-Juan; Feng, Cheng; Liu, Lei (2020). "First case of COVID-19 complicated with fulminant myocarditis: a case report and insights". Infection. doi:10.1007/s15010-020-01424-5. ISSN 0300-8126.
- ↑ Iakimov VP (1977). "[F. Engels' theory of the origin of man and modern anthropologic findings]". Arkh Anat Gistol Embriol. 72 (6): 5–11. PMID 409380.
- ↑ Mehta, Puja; McAuley, Daniel F; Brown, Michael; Sanchez, Emilie; Tattersall, Rachel S; Manson, Jessica J (2020). "COVID-19: consider cytokine storm syndromes and immunosuppression". The Lancet. 395 (10229): 1033–1034. doi:10.1016/S0140-6736(20)30628-0. ISSN 0140-6736.
- ↑ Chen, Guang; Wu, Di; Guo, Wei; Cao, Yong; Huang, Da; Wang, Hongwu; Wang, Tao; Zhang, Xiaoyun; Chen, Huilong; Yu, Haijing; Zhang, Xiaoping; Zhang, Minxia; Wu, Shiji; Song, Jianxin; Chen, Tao; Han, Meifang; Li, Shusheng; Luo, Xiaoping; Zhao, Jianping; Ning, Qin (2020). "Clinical and immunological features of severe and moderate coronavirus disease 2019". Journal of Clinical Investigation. 130 (5): 2620–2629. doi:10.1172/JCI137244. ISSN 0021-9738.
- ↑ Xu, Zhe; Shi, Lei; Wang, Yijin; Zhang, Jiyuan; Huang, Lei; Zhang, Chao; Liu, Shuhong; Zhao, Peng; Liu, Hongxia; Zhu, Li; Tai, Yanhong; Bai, Changqing; Gao, Tingting; Song, Jinwen; Xia, Peng; Dong, Jinghui; Zhao, Jingmin; Wang, Fu-Sheng (2020). "Pathological findings of COVID-19 associated with acute respiratory distress syndrome". The Lancet Respiratory Medicine. 8 (4): 420–422. doi:10.1016/S2213-2600(20)30076-X. ISSN 2213-2600.
- ↑ "Myocardial localization of coronavirus in COVID‐19 cardiogenic shock".
- ↑ Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA (May 2020). "Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic". J Am Coll Cardiol. 75 (18): 2352–2371. doi:10.1016/j.jacc.2020.03.031. PMC 7198856 Check
|pmc=value (help). PMID 32201335 Check|pmid=value (help). - ↑ Zou F, Qian Z, Wang Y, Zhao Y, Bai J (September 2020). "Cardiac Injury and COVID-19: A Systematic Review and Meta-analysis". CJC Open. 2 (5): 386–394. doi:10.1016/j.cjco.2020.06.010. PMC 7308771 Check
|pmc=value (help). PMID 32838255 Check|pmid=value (help). - ↑ 24.0 24.1 24.2 Shi, Shaobo; Qin, Mu; Shen, Bo; Cai, Yuli; Liu, Tao; Yang, Fan; Gong, Wei; Liu, Xu; Liang, Jinjun; Zhao, Qinyan; Huang, He; Yang, Bo; Huang, Congxin (2020). "Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China". JAMA Cardiology. doi:10.1001/jamacardio.2020.0950. ISSN 2380-6583.
- ↑ 25.0 25.1 25.2 25.3 25.4 Esposito, Antonio; Godino, Cosmo; Basso, Cristina; Cappelletti, Alberto Maria; Tresoldi, Moreno; De Cobelli, Francesco; Vignale, Davide; Villatore, Andrea; Palmisano, Anna; Gramegna, Mario; Peretto, Giovanni; Sala, Simone (2020). "Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection". European Heart Journal. 41 (19): 1861–1862. doi:10.1093/eurheartj/ehaa286. ISSN 0195-668X.
- ↑ 26.0 26.1 26.2 26.3 Fang, Yuan; Wei, Xin; Ma, Fenglian; Hu, Hongde (2020). "Coronavirus fulminant myocarditis treated with glucocorticoid and human immunoglobulin". European Heart Journal. doi:10.1093/eurheartj/ehaa190. ISSN 0195-668X.
- ↑ 27.0 27.1 27.2 27.3 Coyle, Justin; Igbinomwanhia, Efehi; Sanchez-Nadales, Alejandro; Danciu, Sorin; Chu, Chae; Shah, Nishit (2020). "A Recovered Case of COVID-19 Myocarditis and ARDS Treated With Corticosteroids, Tocilizumab, and Experimental AT-001". JACC: Case Reports. doi:10.1016/j.jaccas.2020.04.025. ISSN 2666-0849.
- ↑ 28.0 28.1 Luetkens, Julian Alexander; Isaak, Alexander; Zimmer, Sebastian; Nattermann, Jacob; Sprinkart, Alois Martin; Boesecke, Christoph; Rieke, Gereon Jonas; Zachoval, Christian; Heine, Annkristin; Velten, Markus; Duerr, Georg Daniel (2020). "Diffuse Myocardial Inflammation in COVID-19 Associated Myocarditis Detected by Multiparametric Cardiac Magnetic Resonance Imaging". Circulation: Cardiovascular Imaging. 13 (5). doi:10.1161/CIRCIMAGING.120.010897. ISSN 1941-9651.
- ↑ Beşler, Muhammed Said; Arslan, Halil (2020). "Acute myocarditis associated with COVID-19 infection". The American Journal of Emergency Medicine. doi:10.1016/j.ajem.2020.05.100. ISSN 0735-6757.
- ↑ Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson IV, Robicsek A (September 2021). "Myocarditis and Pericarditis After Vaccination for COVID-19". JAMA. 326 (12): 1210–1212. doi:10.1001/jama.2021.13443. PMID 34347001 Check
|pmid=value (help). - ↑ 31.0 31.1 31.2 Bearse M, Hung YP, Krauson AJ, Bonanno L, Boyraz B, Harris CK, Helland TL, Hilburn CF, Hutchison B, Jobbagy S, Marshall MS, Shepherd DJ, Villalba JA, Delfino I, Mendez-Pena J, Chebib I, Newton-Cheh C, Stone JR (July 2021). "Factors associated with myocardial SARS-CoV-2 infection, myocarditis, and cardiac inflammation in patients with COVID-19". Mod Pathol. 34 (7): 1345–1357. doi:10.1038/s41379-021-00790-1. PMID 33727695 Check
|pmid=value (help). - ↑ Peltzer B, Manocha KK, Ying X, Kirzner J, Ip JE, Thomas G, Liu CF, Markowitz SM, Lerman BB, Safford MM, Goyal P, Cheung JW (December 2020). "Outcomes and mortality associated with atrial arrhythmias among patients hospitalized with COVID-19". J Cardiovasc Electrophysiol. 31 (12): 3077–3085. doi:10.1111/jce.14770. PMC 7675597 Check
|pmc=value (help). PMID 33017083 Check|pmid=value (help). - ↑ Ruan, Qiurong; Yang, Kun; Wang, Wenxia; Jiang, Lingyu; Song, Jianxin (2020). "Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China". Intensive Care Medicine. 46 (5): 846–848. doi:10.1007/s00134-020-05991-x. ISSN 0342-4642.
- ↑ Sawalha K, Abozenah M, Kadado AJ, Battisha A, Al-Akchar M, Salerno C, Hernandez-Montfort J, Islam AM (February 2021). "Systematic Review of COVID-19 Related Myocarditis: Insights on Management and Outcome". Cardiovasc Revasc Med. 23: 107–113. doi:10.1016/j.carrev.2020.08.028. PMC 7434380 Check
|pmc=value (help). PMID 32847728 Check|pmid=value (help). - ↑ Fiore G, Sanvito F, Fragasso G, Spoladore R (October 2021). "Case report of cardiogenic shock in COVID-19 myocarditis: peculiarities on diagnosis, histology, and treatment". Eur Heart J Case Rep. 5 (10): ytab357. doi:10.1093/ehjcr/ytab357. PMC 8502841 Check
|pmc=value (help). PMID 34651099 Check|pmid=value (help). - ↑ Hudowenz O, Klemm P, Lange U, Rolf A, Schultheiss HP, Hamm C, Müller-Ladner U, Wegner F (December 2020). "Case report of severe PCR-confirmed COVID-19 myocarditis in a European patient manifesting in mid January 2020". Eur Heart J Case Rep. 4 (6): 1–6. doi:10.1093/ehjcr/ytaa286. PMC 7665439 Check
|pmc=value (help). PMID 33437916 Check|pmid=value (help). - ↑ 37.0 37.1 Yokoo P, Fonseca E, Sasdelli Neto R, Ishikawa WY, Silva M, Yanata E, Chate RC, Nunes Filho A, Bettega M, Fernandes J, Tarasoutchi F, Szarf G (2020). "COVID-19 myocarditis: a case report". Einstein (Sao Paulo). 18: eRC5876. doi:10.31744/einstein_journal/2020RC5876. PMC 7575039 Check
|pmc=value (help). PMID 33111813 Check|pmid=value (help). Vancouver style error: initials (help) - ↑ 38.0 38.1 38.2 Irabien-Ortiz, Ángela; Carreras-Mora, José; Sionis, Alessandro; Pàmies, Julia; Montiel, José; Tauron, Manel (2020). "Fulminant myocarditis due to COVID-19". Revista Española de Cardiología (English Edition). 73 (6): 503–504. doi:10.1016/j.rec.2020.04.005. ISSN 1885-5857.
- ↑ Wang, Daowen; Li, Sheng; Jiang, Jiangang; Yan, Jiangtao; Zhao, Chunxia; Wang, Yan; Ma, Yexin; Zeng, Hesong; Guo, Xiaomei; Wang, Hong; Tang, Jiarong; Zuo, Houjuan; Lin, Li; Cui, Guanglin (2018). "Chinese society of cardiology expert consensus statement on the diagnosis and treatment of adult fulminant myocarditis". Science China Life Sciences. 62 (2): 187–202. doi:10.1007/s11427-018-9385-3. ISSN 1674-7305.
- ↑ Peretto, Giovanni; Sala, Simone; Rizzo, Stefania; Palmisano, Anna; Esposito, Antonio; De Cobelli, Francesco; Campochiaro, Corrado; De Luca, Giacomo; Foppoli, Luca; Dagna, Lorenzo; Thiene, Gaetano; Basso, Cristina; Della Bella, Paolo (2020). "Ventricular Arrhythmias in Myocarditis". Journal of the American College of Cardiology. 75 (9): 1046–1057. doi:10.1016/j.jacc.2020.01.036. ISSN 0735-1097.
- ↑ 41.0 41.1 41.2 Doyen, Denis; Moceri, Pamela; Ducreux, Dorothée; Dellamonica, Jean (2020). "Myocarditis in a patient with COVID-19: a cause of raised troponin and ECG changes". The Lancet. 395 (10235): 1516. doi:10.1016/S0140-6736(20)30912-0. ISSN 0140-6736.
- ↑ Gao, Lei; Jiang, Dan; Wen, Xue-song; Cheng, Xiao-cheng; Sun, Min; He, Bin; You, Lin-na; Lei, Peng; Tan, Xiao-wei; Qin, Shu; Cai, Guo-qiang; Zhang, Dong-ying (2020). "Prognostic value of NT-proBNP in patients with severe COVID-19". Respiratory Research. 21 (1). doi:10.1186/s12931-020-01352-w. ISSN 1465-993X.
- ↑ Han, Huan; Xie, Linlin; Liu, Rui; Yang, Jie; Liu, Fang; Wu, Kailang; Chen, Lang; Hou, Wei; Feng, Yong; Zhu, Chengliang (2020). "Analysis of heart injury laboratory parameters in 273 COVID‐19 patients in one hospital in Wuhan, China". Journal of Medical Virology. 92 (7): 819–823. doi:10.1002/jmv.25809. ISSN 0146-6615.
- ↑ Lauer, Bernward; Niederau, Christoph; Kühl, Uwe; Schannwell, Mira; Pauschinger, Matthias; Strauer, Bodo-Eckhard; Schultheiss, Heinz-Peter (1997). "Cardiac Troponin T in Patients With Clinically Suspected Myocarditis". Journal of the American College of Cardiology. 30 (5): 1354–1359. doi:10.1016/S0735-1097(97)00317-3. ISSN 0735-1097.
- ↑ Heymans, S. (2007). "Myocarditis and heart failure: need for better diagnostic, predictive, and therapeutic tools". European Heart Journal. 28 (11): 1279–1280. doi:10.1093/eurheartj/ehm111. ISSN 0195-668X.
- ↑ Jensen, Juliana; Ma, Li-Ping; Fu, Michael L. X.; Svaninger, David; Lundberg, Per-Arne; Hammarsten, Ola (2010). "Inflammation increases NT-proBNP and the NT-proBNP/BNP ratio". Clinical Research in Cardiology. 99 (7): 445–452. doi:10.1007/s00392-010-0140-z. ISSN 1861-0684.
- ↑ 47.0 47.1 Siripanthong, Bhurint; Nazarian, Saman; Muser, Daniele; Deo, Rajat; Santangeli, Pasquale; Khanji, Mohammed Y.; Cooper, Leslie T.; Chahal, C. Anwar A. (2020). "Recognizing COVID-19–related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management". Heart Rhythm. doi:10.1016/j.hrthm.2020.05.001. ISSN 1547-5271.
- ↑ Juusela A, Nazir M, Gimovsky M (May 2020). "Two cases of coronavirus 2019-related cardiomyopathy in pregnancy". Am J Obstet Gynecol MFM. 2 (2): 100113. doi:10.1016/j.ajogmf.2020.100113. PMC 7194868 Check
|pmc=value (help). PMID 32363336 Check|pmid=value (help). - ↑ Kim IC, Kim JY, Kim HA, Han S (May 2020). "COVID-19-related myocarditis in a 21-year-old female patient". Eur Heart J. 41 (19): 1859. doi:10.1093/eurheartj/ehaa288. PMC 7184491 Check
|pmc=value (help). PMID 32282027 Check|pmid=value (help). - ↑ Favre G, Pomar L, Baud D (August 2020). "Coronavirus disease 2019 during pregnancy: do not underestimate the risk of maternal adverse outcomes". Am J Obstet Gynecol MFM. 2 (3): 100160. doi:10.1016/j.ajogmf.2020.100160. PMC 7367790 Check
|pmc=value (help). PMID 32838265 Check|pmid=value (help). - ↑ Sardari A, Tabarsi P, Borhany H, Mohiaddin R, Houshmand G (January 2021). "Myocarditis detected after COVID-19 recovery". Eur Heart J Cardiovasc Imaging. 22 (1): 131–132. doi:10.1093/ehjci/jeaa166. PMC 7574602 Check
|pmc=value (help). PMID 32462177 Check|pmid=value (help). - ↑ Luetkens JA, Isaak A, Zimmer S, Nattermann J, Sprinkart AM, Boesecke C, Rieke GJ, Zachoval C, Heine A, Velten M, Duerr GD (May 2020). "Diffuse Myocardial Inflammation in COVID-19 Associated Myocarditis Detected by Multiparametric Cardiac Magnetic Resonance Imaging". Circ Cardiovasc Imaging. 13 (5): e010897. doi:10.1161/CIRCIMAGING.120.010897. PMID 32397816 Check
|pmid=value (help). - ↑ Khalid Y, Dasu N, Dasu K (August 2020). "A case of novel coronavirus (COVID-19)-induced viral myocarditis mimicking a Takotsubo cardiomyopathy". HeartRhythm Case Rep. 6 (8): 473–476. doi:10.1016/j.hrcr.2020.05.020. PMC 7424304 Check
|pmc=value (help). PMID 32817822 Check|pmid=value (help). - ↑ Ejarque M, Sabadell-Basallote J, Beiroa D, Calvo E, Keiran N, Nuñez-Roa C, Rodríguez M, Sabench F, Del Castillo D, Jimenez V, Bosch F, Nogueiras R, Vendrell J, Fernández-Veledo S (May 2021). "Adipose tissue is a key organ for the beneficial effects of GLP-2 metabolic function". Br J Pharmacol. 178 (10): 2131–2145. doi:10.1111/bph.15278. PMID 32986861 Check
|pmid=value (help). Vancouver style error: initials (help) - ↑ Garot J, Amour J, Pezel T, Dermoch F, Messadaa K, Felten ML, Raymond V, Baubillier E, Sanguineti F, Garot P (July 2020). "SARS-CoV-2 Fulminant Myocarditis". JACC Case Rep. 2 (9): 1342–1346. doi:10.1016/j.jaccas.2020.05.060. PMC 7274592 Check
|pmc=value (help). PMID 32835276 Check|pmid=value (help). - ↑ Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M (July 2020). "Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiol. 5 (7): 819–824. doi:10.1001/jamacardio.2020.1096. PMC 7364333 Check
|pmc=value (help). PMID 32219357 Check|pmid=value (help). - ↑ Ezekowitz, Justin A.; O'Meara, Eileen; McDonald, Michael A.; Abrams, Howard; Chan, Michael; Ducharme, Anique; Giannetti, Nadia; Grzeslo, Adam; Hamilton, Peter G.; Heckman, George A.; Howlett, Jonathan G.; Koshman, Sheri L.; Lepage, Serge; McKelvie, Robert S.; Moe, Gordon W.; Rajda, Miroslaw; Swiggum, Elizabeth; Virani, Sean A.; Zieroth, Shelley; Al-Hesayen, Abdul; Cohen-Solal, Alain; D'Astous, Michel; De, Sabe; Estrella-Holder, Estrellita; Fremes, Stephen; Green, Lee; Haddad, Haissam; Harkness, Karen; Hernandez, Adrian F.; Kouz, Simon; LeBlanc, Marie-Hélène; Masoudi, Frederick A.; Ross, Heather J.; Roussin, Andre; Sussex, Bruce (2017). "2017 Comprehensive Update of the Canadian Cardiovascular Society Guidelines for the Management of Heart Failure". Canadian Journal of Cardiology. 33 (11): 1342–1433. doi:10.1016/j.cjca.2017.08.022. ISSN 0828-282X.
- ↑ 58.0 58.1 Friedrich, Matthias G.; Strohm, Oliver; Schulz-Menger, Jeanette; Marciniak, Heinz; Luft, Friedrich C.; Dietz, Rainer (1998). "Contrast Media–Enhanced Magnetic Resonance Imaging Visualizes Myocardial Changes in the Course of Viral Myocarditis". Circulation. 97 (18): 1802–1809. doi:10.1161/01.CIR.97.18.1802. ISSN 0009-7322.
- ↑ 59.0 59.1 Friedrich, Matthias G.; Sechtem, Udo; Schulz-Menger, Jeanette; Holmvang, Godtfred; Alakija, Pauline; Cooper, Leslie T.; White, James A.; Abdel-Aty, Hassan; Gutberlet, Matthias; Prasad, Sanjay; Aletras, Anthony; Laissy, Jean-Pierre; Paterson, Ian; Filipchuk, Neil G.; Kumar, Andreas; Pauschinger, Matthias; Liu, Peter (2009). "Cardiovascular Magnetic Resonance in Myocarditis: A JACC White Paper". Journal of the American College of Cardiology. 53 (17): 1475–1487. doi:10.1016/j.jacc.2009.02.007. ISSN 0735-1097.
- ↑ Han, Yuchi; Chen, Tiffany; Bryant, Jennifer; Bucciarelli-Ducci, Chiara; Dyke, Christopher; Elliott, Michael D.; Ferrari, Victor A.; Friedrich, Matthias G.; Lawton, Chris; Manning, Warren J.; Ordovas, Karen; Plein, Sven; Powell, Andrew J.; Raman, Subha V.; Carr, James (2020). "Society for Cardiovascular Magnetic Resonance (SCMR) guidance for the practice of cardiovascular magnetic resonance during the COVID-19 pandemic". Journal of Cardiovascular Magnetic Resonance. 22 (1). doi:10.1186/s12968-020-00628-w. ISSN 1532-429X.
- ↑ Dennert, R.; Crijns, H. J.; Heymans, S. (2008). "Acute viral myocarditis". European Heart Journal. 29 (17): 2073–2082. doi:10.1093/eurheartj/ehn296. ISSN 0195-668X.
- ↑ Cooper, Leslie T.; Baughman, Kenneth L.; Feldman, Arthur M.; Frustaci, Andrea; Jessup, Mariell; Kuhl, Uwe; Levine, Glenn N.; Narula, Jagat; Starling, Randall C.; Towbin, Jeffrey; Virmani, Renu (2007). "The Role of Endomyocardial Biopsy in the Management of Cardiovascular Disease". Circulation. 116 (19): 2216–2233. doi:10.1161/CIRCULATIONAHA.107.186093. ISSN 0009-7322.
- ↑ Rao, Sangeetha; Sasser, William; Diaz, Franco; Sharma, Nirmal; Alten, Jeffrey (2014). "Coronavirus Associated Fulminant Myocarditis Successfully Treated With Intravenous Immunoglobulin and Extracorporeal Membrane Oxygenation". Chest. 146 (4): 336A. doi:10.1378/chest.1992018. ISSN 0012-3692.