Hydatidiform mole
| Hydatidiform mole | |
 | |
|---|---|
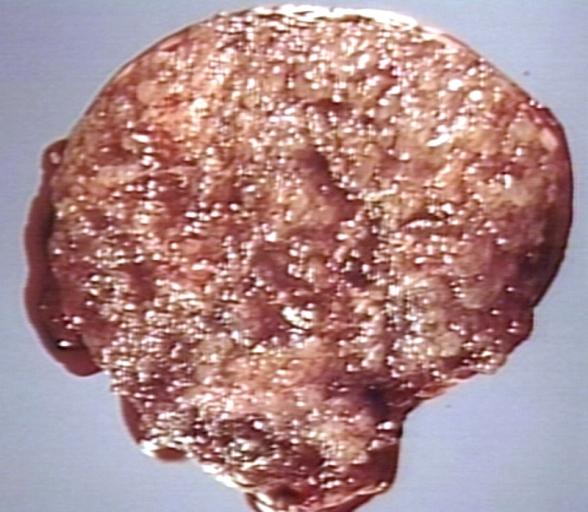
| MOLE, HYDATIDIFORM, HYSTERECTOMY SPECIMEN. VARIABLY SIZED VESICLES, NO NORMAL PLACENTA, NO FETUS. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | O01, D39.2 |
| ICD-9 | 630 |
| ICD-O: | M9100 |
| OMIM | 231090 |
| DiseasesDB | 6097 |
| MedlinePlus | 000909 |
| eMedicine | med/1047 med/866 |
| MeSH | D006828 |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Hydatidiform mole (or mola hydatidiforma) is a common complication of pregnancy, occurring once in every 1000 pregnancies in the US, with much higher rates in Asia (e.g. up to one in 100 pregnancies in Indonesia). It consists of a nonviable embryo which implants and proliferates within the uterus.[1] The term is derived from hydatidiform ("like a bunch of grapes") and mole (from Latin mola = millstone).
Most moles present with painless vaginal bleeding during the second trimester of pregnancy. They are diagnosed by ultrasound imaging. Extremely high levels of human chorionic gonadotropin (HCG) are suggestive, but not diagnostic, of molar pregnancy.[2] Today moles are surgically removed by curettage, in order to avoid the risks of choriocarcinoma.[3]
Pathophysiology
A mole is characterized by a conceptus of hyperplastic trophoblastic tissue attached to the placenta. The conceptus does not contain the inner cell mass (the mass of cells inside the primordial embryo that will eventually give rise to the fetus).
The hydatidiform mole can be of two types: a complete mole, in which the abnormal embryonic tissue is derived from the father only; and a partial mole, in which the abnormal tissue is derived from both parents.
- Complete moles usually occur when an empty ovum is fertilized by a sperm that then duplicates its own DNA (a process called androgenesis). This explains why most complete moles are of the 46,XX genotype. A 46, XY genotype may occur when 2 sperm (one 23, X and the other 23, Y) fertilize an empty egg. They grossly resemble a bunch of grapes ("cluster of grapes" or "honeycombed uterus" or "snow-storm"[4]). Their DNA is purely paternal in origin (since all chromosomes are derived from the sperm), and is diploid (i.e. there are two copies of every chromosome). Ninety percent are 46,XX, and 10% are 46,XY. In a complete mole, the fetus fails to develop, thus on gross examination there are no signs of fetal tissue. All of the chorionic villi are enlarged. The main complication of the complete mole is a 2% chance of progression to a cancer called choriocarcinoma.
- Partial moles can occur if a normal haploid ovum is fertilized by two sperm, or, if fertilized by one sperm, if the paternal chromosomes become duplicated. Thus their DNA is both maternal and paternal in origin. They can be triploid (e.g. 69 XXX, 69 XXY) or even tetraploid. Fetal parts are often seen on gross examination. There is also an increased risk of choriocarcinoma, but the risk is lower than with the complete mole.
Etiology
The etiology of this condition is not completely understood. Potential risk factors may include defects in the egg, abnormalities within the uterus, or nutritional deficiencies. Women under 20 or over 40 years of age have a higher risk. Other risk factors include diets low in protein, folic acid, and carotene.
Diagnosis
Molar pregnancies usually present with painless vaginal bleeding in the fourth to fifth month of pregnancy.[5] The uterus may be larger than expected, or the ovaries may be enlarged. There may also be more vomiting than would be expected (hyperemesis). Sometimes there is an increase in blood pressure along with protein in the urine. Blood tests will show very high levels of human chorionic gonadotropin (hCG).
The diagnosis is strongly suggested by ultrasound (sonogram), but definitive diagnosis requires histopathological examination.
Sometimes symptoms of hyperthyroidism are seen, due to the extremely high levels of hCG, which can mimic the normal Thyroid-stimulating hormone (TSH).[6]
Ultrasonography

Pathology
<youtube v=QO3QF6n4xuo/>
Treatment
Hydatidiform moles should be treated by evacuating the uterus by uterine suction or by surgical curettage as soon as possible after diagnosis. Patients are followed up until their serum human chorionic gonadotrophin (hCG) titre has fallen to an undetectable level. Invasive or metastatic moles often respond well to methotrexate. The response to treatment is nearly 100%. Patients are advised not to conceive for one year after a molar pregnancy. The chances of having another molar pregnancy are approximately 1%.
Prognosis
More than 80% of hydatidiform moles are benign. The outcome after treatment is usually excellent. Close follow-up is essential. Highly effective means of contraception are recommended to avoid pregnancy for at least 6 to 12 months.
In 10 to 15% of cases, hydatidiform moles may develop into invasive moles. These may intrude so far into the uterine wall that hemorrhage or other complications develop. It is for this reason that a post-operative full abdominal and chest x-ray will often be requested.
In 2 to 3% of cases, hydatidiform moles may develop into choriocarcinoma, which is a malignant, rapidly-growing, and metastatic (spreading) form of cancer. Despite these factors which normally indicate a poor prognosis, the rate of cure after treatment with chemotherapy is high.
Over 90% of women with malignant, non-spreading cancer are able to survive and retain their ability to have children. In those with metastatic (spreading) cancer, remission remains at 75 to 85%, although the ability to have children is usually lost.
References
- ↑ Robbins and Cotran's Pathological Basis of Disease, 7th ed., p. 1110
- ↑ McPhee S. and Ganong W.F. Pathophysiology of Disease, 5th ed., p. 639.
- ↑ Robbins and Cotran's Pathological Basis of Disease, 7th ed., p. 1112
- ↑ Woo J, Hsu C, Fung L, Ma H (1983). "Partial hydatidiform mole: ultrasonographic features". Aust N Z J Obstet Gynaecol. 23 (2): 103–7. PMID 6578773.
- ↑ Robbins and Cotran's Pathological Basis of Disease, 7th ed., p. 1110
- ↑ McPhee S. and Ganong W.F. Pathophysiology of Disease, 5th ed., p. 639.
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
External links
- Complete moles have paternal chromosomes but maternal mitochondrial DNA by Douglas C. Wallace, Urvashi Surti, Camellia W. Adams and A. E. Szulman, Volume 61, Number 2 of Human Genetics
- MyMolarPregnancy.com Support group, information, links and personal stories for women with molar pregnancies.
- Molar Pregnancy Early pregnancy loss
ar:حمل عنقودي de:Blasenmole nl:Mola-zwangerschap sv:Druvbörd