Aortic dissection overview: Difference between revisions
No edit summary |
|||
| Line 232: | Line 232: | ||
* Neurologic deficits such as [[coma]], altered mental status, [[Ddx:Cerebrovascular Accident|Cerebrovascular accident]] (CVA) and [[vagal episodes]] are seen in up to 20%. | * Neurologic deficits such as [[coma]], altered mental status, [[Ddx:Cerebrovascular Accident|Cerebrovascular accident]] (CVA) and [[vagal episodes]] are seen in up to 20%. | ||
*There can also be focal neurologic signs due to occlusion of a [[Anterior spinal artery|spinal artery]]. This condition is known as [[Anterior spinal artery syndrome]] or [[Anterior spinal artery syndrome|"Beck's syndrome"]]. | *There can also be focal neurologic signs due to occlusion of a [[Anterior spinal artery|spinal artery]]. This condition is known as [[Anterior spinal artery syndrome]] or [[Anterior spinal artery syndrome|"Beck's syndrome"]]. | ||
==Laboratory Findings== | |||
Routine blood work is usually not helpful and should not delay definitive diagnostic studies such as a CT scan and treatment. [[Hemolysis]] can be present as a result of blood in the false lumen. The presence of an elevated [[CK MB]] may indicate the presence of concomitant [[acute myocardial infarction]] (often a [[right coronary artery]] occlusion due to occlusion of the ostium of the [[RCA]] by the dissection). [[Hematuria]] may be present and may indicate the presence of [[renal infarction]]. | |||
==Electrocardiogram== | ==Electrocardiogram== | ||
[[ST elevation myocardial infarction]] ([[MI]]) due to occlusion by the dissection of the coronary artery at its ostium may be present. The [[right coronary artery]] tends to be involved more frequently than the [[left coronary artery]]. [[Electrical alternans]] may be present in the setting of a [[pericardial effusion]] should the dissection have extended into the pericardium. | [[ST elevation myocardial infarction]] ([[MI]]) due to occlusion by the dissection of the coronary artery at its ostium may be present. The [[right coronary artery]] tends to be involved more frequently than the [[left coronary artery]]. [[Electrical alternans]] may be present in the setting of a [[pericardial effusion]] should the dissection have extended into the pericardium. | ||
Revision as of 02:01, 29 October 2012
|
Aortic dissection Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenarios |
|
Case Studies |
|
|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Aortic dissection is a tear in the wall of the aorta that causes blood to flow between the layers of the wall of the aorta and force the layers apart. Aortic dissection is a medical emergency and can quickly lead to death, even with optimal treatment. If the dissection tears the aorta completely open (through all three layers) massive and rapid blood loss occurs. Aortic dissections resulting in rupture have a 90% mortality rate even if intervention is timely.
Acute aortic dissection is the most common fatal condition that involves the aorta. The mortality rate has been estimated to be as high as 1% per hour during the first 48 hours. Because of the diverse clinical manifestations of aortic dissection, one needs to maintain a high index of suspicion in patients with not just chest pain, but also those with stroke, congestive heart failure, hoarseness, hemoptysis, claudication, superior vena cava (SVC) syndrome, or upper airway obstruction. Despite the fact that a noninvasive diagnosis can be made in up to 90% of cases, the correct antemortem diagnosis is made less than 50% of the time. Recognition of the condition and vigorous pre-operative management are critical to survival.
Classification
Several different classification systems have been used to describe aortic dissections. The systems commonly in use are either based on either the anatomy of the dissection (proximal, distal) or the duration of onset of symptoms (acute, chronic) prior to presentation.
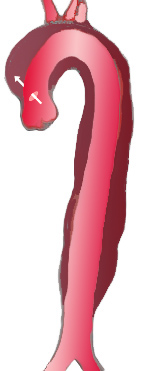
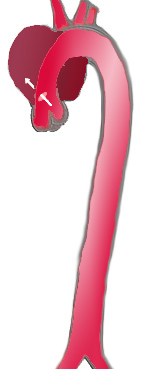
DeBakey classification system
The DeBakey system is an anatomical description of the aortic dissection. It categorizes the dissection based on where the original intimal tear is located and the extent of the dissection (localized to either the ascending aorta or descending aorta, or involves both the ascending and descending aorta.[1]
- Type I - Originates in ascending aorta, propagates at least to the aortic arch and often beyond it distally.
- Type II – Originates in and is confined to the ascending aorta.
- Type III – Originates in descending aorta, rarely extends proximally.
|
|

| |
| Percentage | 60 % | 10-15 % | 25-30 % |
| Type | DeBakey I | DeBakey II | DeBakey III |
| Stanford A | Stanford B | ||
| Proximal | Distal | ||
| Classification of aortic dissection | |||
Stanford Classification System
Divided into 2 groups; A and B depending on whether the ascending aorta is involved.[2]
- A = Type I and II DeBakey
- B = Type III Debakey
Pathophysiology
Initial Intimal Tear
- Aortic dissection begins as a tear in the aortic wall in > 95% of patients.
- It is usually transverse, extends through the intima and halfway through the media and involves ~50% of the aortic circumference.
- Location of dissections:
- The initial tear is usually within 100 mm of the aortic valve.
- 65% of dissections originate in the ascending aorta, distal to the aortic valve and coronary ostia
- 10% arise in the transverse aortic arch
- 20% in the proximal descending aorta
- 5% in the more distal descending aorta
Propagation of the Intimal Tear
In an aortic dissection, blood penetrates the intima and enters the media layer. The high pressure rips the tissue of the media apart, allowing more blood to enter. This can propagate along the length of the aorta for a variable distance, dissecting either towards or away from the heart or both. Once a tear develops, blood then passes into the media, and a false lumen is dissected in the outer layer of aortic media involving ~50% of the aortic circumference. This false lumen can enlarge, and compress the true lumen, as well as extend proximally or distally and occlude aortic branches. For some unknown reason, the right lateral wall of the ascending aorta is the most common site for dissection. The right coronary artery can become occluded as a result of this propagation.
Separating the false lumen from the true lumen is a layer of intimal tissue. This tissue is known as the intimal flap. As blood flows down the false lumen, it may cause secondary tears in the intima. Through these secondary tears, the blood can re-enter the true lumen.
Causes
Age related changes due to atherosclerosis and hypertension are associated with spontaneous dissection, while blunt trauma injury and sudden deceleration in a motor vehicle accident is a major cause of aortic dissection.
Other risk factors and conditions associated with the development of aortic dissection include:
- Aging
- Bicuspid aortic valve
- Chest trauma
- Coarctation of the aorta
- Connective tissue disorders
- Ehlers-Danlos syndrome
- Heart surgery or procedures
- Marfan syndrome
- Third trimester of pregnancy
- Pseudoxanthoma elasticum
- Tertiary syphilis
- Turner's syndrome
- Vascular inflammation due to conditions such as arteritis and syphilis
Differentiating Aortic Dissection from other Disorders
Aortic dissection is a life threatening entity that must be distinguished from other life threatening entities such as cardiac tamponade, cardiogenic shock, myocardial infarction, and pulmonary embolism. An aortic aneurysm is not synonymous with aortic dissection. Aneurysms are defined as a localized permanent dilation of the aorta to a diameter > 50% of normal. Other disorders that aortic dissection should be differentiated from include the following:
- Aortic Regurgitation
- Aortic Stenosis
- Cardiac Tamponade
- Cardiogenic Shock
- Gastroenteritis
- Hemorrhagic Shock
- Hernias
- Hypertensive Emergencies
- Hypovolemic Shock
- Mechanical Back Pain
- Myocardial Infarction
- Myocarditis
- Myopathies
- Pancreatitis
- Pericarditis
- Peripheral Vascular Injuries
- Pleural Effusion
- Pulmonary Embolism
- Thoracic Outlet Syndrome
Epidemiology and Demographics
There are approximately 2,000 cases of aortic dissection in the US per year, and aortic dissection accounts for 3-4% of sudden deaths. The peak incidence is in the sixth and seventh decades, and males predominate 2:1.
Risk Factors
- Aging. The highest incidence of aortic dissection is in individuals who are 50 to 70 years old.
- Atherosclerosis and its associated risk factors like diabetes
- Bicuspid aortic valve is present in approximately 7%-14% of patients. These individuals are prone to dissection in the ascending aorta. The risk of dissection in individuals with bicuspid aortic valve is not associated with the degree of stenosis of the valve.
- Chest trauma. Chest trauma leading to aortic dissection can be divided into two groups based on etiology: blunt chest trauma (commonly seen in car accidents) and iatrogenic. Iatrogenic causes include trauma during cardiac catheterization or due to an intra-aortic balloon pump.
- Cocaine abuse
- Coarctation of the aorta
- Cystic medial necrosis
- Deceleration trauma most commonly causes aortic rupture, not dissection
- Ehlers-Danlos syndrome
- Giant cell arteritis
- Heart surgery particularly aortic valve replacement; 18% of individuals who present with an acute aortic dissection have a history of open heart surgery. Individuals who have undergone aortic valve replacement for aortic insufficiency are at particularly high risk. This is because aortic insufficiency causes increased blood flow in the ascending aorta. This can cause dilatation and weakening of the walls of the ascending aorta.
- Hypertension is seen in 71-86% of patients. It occurs most frequently in those with type III dissection.
- Male gender. The incidence is twice as high in males as in females (male-to-female ratio is 2:1).
- Marfan’s syndrome is present in 5%-9% of patients. In this subset, there is an increased incidence in young individuals. Individuals with Marfan syndrome patients are more prone to proximal dissections of the aorta.
- Pseudoxanthoma elasticum
- Turner's syndrome. Turner syndrome increases the risk of aortic dissection as a result of aortic root dilatation[3].
- Tertiary syphilis
- Third trimester of pregnancy. Half of dissections in females before age 40 occur during pregnancy (typically in the 3rd trimester or early postpartum period).
- Vasculitis (inflammation of an artery) is rarely associated with aortic dissection.
Natural History
If the patient remains untreated, the mortality is:
- 1% per hour during the first day
- 75% at 2 weeks
- 90% at 1 year
Complications
The complications of aortic dissection include:
Cardiac
- Aortic rupture leading to massive blood loss, hypotension and shock often resulting in death. Indeed, aortic dissection accounts for 3-4% of sudden deaths.
- Pericardial tamponade due to extension of the dissection into the pericardium
- Acute aortic regurgitationdue to the aortic dilation and dissection into the valve structure which can then cause acute pulmonary edema
- Myocardial ischemia or myocardial infarction due to dissection into either the right or left coronary ostium (but most commonly the right coronary artery)
- Redissection and aortic diameter enlargement
- Aneurysmal dilatation and saccular aneurysm chronically
Kidney
- Mesenteric and renal ischemia due to dissection into the ostium of the parent vessels which can lead to hematuria, renal infarction, acute renal failure, or visceral ischemia
Peripheral Arterial
- Claudication due to an extension of the dissection into the iliac arteries
Neurologic
- Ischemic cerebrovascular accident (CVA) due to dissection into the head vessels
- Hemiplegia due to dissection into the spinal arteries
- Hemianesthesia due to dissection into the spinal arteries
Compression of Nearby Organs
- Swelling of the neck and face (compression of the superior vena cava or Superior vena cava syndrome)
- Horner syndrome (compression of the superior cervical ganglia)
- Dysphagia (compression of the esophagus)
- Stridor and wheezing (compression of the airway)
- Hemoptysis (compression of and erosion into the bronchus)
- Vocal cord paralysis and hoarseness (compression of the recurrent laryngeal nerve)
Prognosis
The mortality rate is in large part determined by the patient's age and comorbidities.
- 30% in hospital mortality
- 60% 10-year survival rate among treated patients
Type A aortic dissection
- Surgical treatment-30% mortality rate
- Medical treatment-60% mortality rate
Type B aortic dissection
- Surgical treatment-10% mortality rate
- Medical treatment- 30% mortality rate
Physical Examination
Blood Pressure
Blood Pressure Discrepancy
Pseudohypotension (falsely low blood pressure measurement) may occur due to involvement of the brachiocephalic artery (supplying the right arm) or the left subclavian artery (supplying the left arm).
Hypertension
While many patients with an aortic dissection have a history of hypertension, the blood pressure is quite variable among patients with acute aortic dissection, and tends to be higher in individuals with a distal dissection. In individuals with a proximal aortic dissection, 36% present with hypertension, while 25% present with hypotension. In those that present with distal aortic dissections, 70% present with hypertension while 4% present with hypotension.
Hypotension
Severe hypotension at presentation is a grave prognostic indicator. It is usually associated with pericardial tamponade, severe aortic insufficiency, or rupture of the aorta. Accurate measurement of the blood pressure is important.
Pulse
- Tachycardia may be present due to pain, anxiety, aortic rupture with massive bleeding, pericardial tamponade, aortic insufficiency with acute pulmonary edema and hypoxemia.
- A wide pulse pressure may be present if acute aortic insufficiency develops.
- Pulsus paradoxus (a drop of > 10 mmHg in arterial blood pressure on inspiration) may be present of pericardial tamponade develops.
General
The patient may be hoarse due to compression of the left recurrent laryngeal nerve
Head, Eyes, Ears, Nose, Throat
- Swelling of the neck and face may be present due to compression of the superior vena cava or Superior vena cava syndrome
- Horner syndrome may be present due to compression of the superior cervical ganglia
Heart
Aortic Insufficiency
Aortic insufficiency occurs in 1/2 to 2/3 of ascending aortic dissections, and the murmur of aortic insufficiency is audible in about 32% of proximal dissections. The intensity (loudness) of the murmur is dependent on the blood pressure and may be inaudible in the event of hypotension. Aortic insufficiency is more commonly associated with type I or type II dissection. The murmur of aortic insufficiency (AI) due to aortic dissection is best heard at the right 2nd intercostal space (ICS), as compared with the lower left sternal border for AI due to primary aortic valvular disease.
Cardiac Tamponade
- Beck's triad may be present:[4]
- Hypotension (due to decreased stroke volume)
- Jugular venous distension (due to impaired venous return to the heart)
- Muffled heart sounds (due to fluid inside the pericardium) [5]
- Distension of veins in the forehead and scalp
- Altered sensorium (decreasing Glasgow coma scale)
- Peripheral edema
In addition to the Beck's triad and pulsus paradoxus the following can be found on cardiovascular examination:
- Pericardial rub
- Clicks - As Ventricular volume shrinks disproportionately, there may be psuedoprolapse/true prolapse of mitral and/or tricuspid valvular structures that result in clicks.
- Kussmaul's sign - Decrease in jugular venous pressure with inspiration is uncommon.
Lungs
- Rales may be present due to cardiogenic pulmonary edema which may result from acute aortic regurgitation.
- Hemothorax and / or pleural effusion may cause dullness to percussion.
- Stridor and wheezing may be present due to compression of the airway
- Hemoptysis may be present due to compression of and erosion into the bronchus
Extremities
Diminution or absence of pulses is found in up to 40% of patients, and occurs due to occlusion of a major aortic branch. For this reason it is critical to assess the pulse and blood pressure in both arms. The iliac arteries may be affected as well.
Neurologic
- Neurologic deficits such as coma, altered mental status, Cerebrovascular accident (CVA) and vagal episodes are seen in up to 20%.
- There can also be focal neurologic signs due to occlusion of a spinal artery. This condition is known as Anterior spinal artery syndrome or "Beck's syndrome".
Laboratory Findings
Routine blood work is usually not helpful and should not delay definitive diagnostic studies such as a CT scan and treatment. Hemolysis can be present as a result of blood in the false lumen. The presence of an elevated CK MB may indicate the presence of concomitant acute myocardial infarction (often a right coronary artery occlusion due to occlusion of the ostium of the RCA by the dissection). Hematuria may be present and may indicate the presence of renal infarction.
Electrocardiogram
ST elevation myocardial infarction (MI) due to occlusion by the dissection of the coronary artery at its ostium may be present. The right coronary artery tends to be involved more frequently than the left coronary artery. Electrical alternans may be present in the setting of a pericardial effusion should the dissection have extended into the pericardium.
References
- ↑ DeBakey ME, Henly WS, Cooley DA, Morris GC Jr, Crawford ES, Beall AC Jr. Surgical management of dissecting aneurysms of the aorta. J Thorac Cardiovasc Surg 1965;49:130-49. PMID 14261867.
- ↑ Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE. Management of acute aortic dissections. Ann Thorac Surg 1970;10:237-47. PMID 5458238.
- ↑ Increased maternal cardiovascular mortality associated with pregnancy in women with Turner syndrome.
- ↑ Gwinnutt, C., Driscoll, P. (Eds) (2003) (2nd Ed.) Trauma Resuscitation: The Team Approach. Oxford: BIOS Scientific Publishers Ltd. ISBN 978-1859960097
- ↑ Dolan, B., Holt, L. (2000). Accident & Emergency: Theory into practice. London: Bailliere Tindall ISBN 978-0702022395