Atrial flutter resident survival guide: Difference between revisions
No edit summary |
|||
| (75 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{| class="infobox" style="float:right;" | {{CMG}}; {{AE}} {{Hilda}}; [[Priyamvada Singh|Priyamvada Singh, M.D.]] [mailto:psingh13579@gmail.com] | ||
{| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 200px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0"; | |||
|- | |||
! style="padding: 0 5px; font-size: 85%; background: #A8A8A8" align=center| {{fontcolor|#2B3B44|Atrial fibrillation resident survival guide Microchapters}} | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Atrial fibrillation resident survival guide#Overview|Overview]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Atrial flutter resident survival guide#Causes|Causes]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Atrial flutter resident survival guide#Diagnosis|Diagnosis]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Atrial flutter resident survival guide#Treatment|Treatment]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Atrial flutter resident survival guide#Heart Rate Control|Heart Rate Control]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Atrial flutter resident survival guide#Pharmacological Cardioversion|Pharmacological Cardioverion]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Atrial flutter resident survival guide#Antiarrhythmic Therapy|Antiarrhythmic Therapy]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Atrial flutter resident survival guide#Anticoagulation Therapy|Anticoagulation Therapy]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Atrial flutter resident survival guide#Do's|Do's]] | |||
|- | |- | ||
| [[ | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Atrial flutter resident survival guide#Dont's|Dont's]] | ||
|} | |} | ||
== | == Overview== | ||
[[Atrial flutter]] is a reenterant arrhythmia with atrial rates between | [[Atrial flutter]] is a [[AV nodal reentrant tachycardia|reenterant arrhythmia]], with atrial rates between 240 and 340/min, with a regular ventricular response and a saw tooth pattern on EKG. While it occurs mostly in patients with structural heart disease, it may also occur in patients with normal heart. It presents with [[palpitations]], [[dyspnea]], [[fatigue]], lightheadedness etc. A typical flutter rhythm on EKG consists of absent P waves, saw tooth pattern in leads II, III and aVF, an atrial rate of 240-340 beats/min and an atrial rate:ventricular rate ratio 2:1 (most commonly). The treatment consists of rate control, anticoagulation therapy and [[cardioversion]] if the flutter is well tolerated. In those with poorly tolerated flutter or hemodynamic instability direct [[Cardioversion|DC cardioversion]] is attempted, followed by rate control therapy. | ||
==Causes== | ==Causes== | ||
===Life Threatening Causes=== | ===Life Threatening Causes=== | ||
Life-threatening causes include conditions which result in death or permanent disability within 24 hours if left untreated. | Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. [[Atrial flutter]] can be a life-threatening condition and must be treated as such irrespective of the causes. | ||
===Common Causes=== | ===Common Causes=== | ||
*[[Acute coronary syndromes]] | *[[Acute coronary syndromes]] | ||
*[[Cardiomyopathy natural history, complications and prognosis|Cardiomyopathy]] | *[[Cardiomyopathy natural history, complications and prognosis|Cardiomyopathy]] | ||
*[[Carbon monoxide poisoning#Symptoms|Carbon monoxide poisoning]] | |||
*[[Congenital heart disease]] | *[[Congenital heart disease]] | ||
*[[Hypertensive heart disease]] | *[[Hypertensive heart disease]] | ||
*[[Hyperthyroidism history and symptoms|Hyperthyroidism]] | *[[Hyperthyroidism history and symptoms|Hyperthyroidism]] | ||
*[[Mitral stenosis|Mitral valve disease]]<ref name="pmid23280242">{{cite journal |author=Gutierrez SD, Earing MG, Singh AK, Tweddell JS, Bartz PJ |title=Atrial Tachyarrhythmias and the Cox-maze Procedure in Congenital Heart Disease |journal=Congenit Heart Dis |volume= |issue= |pages= |year=2012 |month=December |pmid=23280242 |doi=10.1111/chd.12031 |url=}}</ref> <ref name="Granada-2000">{{Cite journal | last1 = Granada | first1 = J. | last2 = Uribe | first2 = W. | last3 = Chyou | first3 = PH. | last4 = Maassen | first4 = K. | last5 = Vierkant | first5 = R. | last6 = Smith | first6 = PN. | last7 = Hayes | first7 = J. | last8 = Eaker | first8 = E. | last9 = Vidaillet | first9 = H. | title = Incidence and predictors of atrial flutter in the general population. | journal = J Am Coll Cardiol | volume = 36 | issue = 7 | pages = 2242-6 | month = Dec | year = 2000 | doi = | PMID = 11127467 }}</ref> | *[[Mitral stenosis|Mitral valve disease]]<ref name="pmid23280242">{{cite journal |author=Gutierrez SD, Earing MG, Singh AK, Tweddell JS, Bartz PJ |title=Atrial Tachyarrhythmias and the Cox-maze Procedure in Congenital Heart Disease |journal=Congenit Heart Dis |volume= |issue= |pages= |year=2012 |month=December |pmid=23280242 |doi=10.1111/chd.12031 |url=}}</ref> <ref name="Granada-2000">{{Cite journal | last1 = Granada | first1 = J. | last2 = Uribe | first2 = W. | last3 = Chyou | first3 = PH. | last4 = Maassen | first4 = K. | last5 = Vierkant | first5 = R. | last6 = Smith | first6 = PN. | last7 = Hayes | first7 = J. | last8 = Eaker | first8 = E. | last9 = Vidaillet | first9 = H. | title = Incidence and predictors of atrial flutter in the general population. | journal = J Am Coll Cardiol | volume = 36 | issue = 7 | pages = 2242-6 | month = Dec | year = 2000 | doi = | PMID = 11127467 }}</ref> | ||
*[[Pulmonary embolism natural history, complications and prognosis|Pulmonary embolism]] | |||
*[[ST elevation myocardial infarction complications|Myocardial infarction]] | |||
== Management== | == Management== | ||
Shown below is an algorithm summarizing the approach to [[atrial flutter]]. | |||
===Diagnostic Approach=== | |||
Shown below is an algorithm summarizing the initial approach to [[atrial flutter]]. | |||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | {{familytree | | A01 | | A01=<div style="text-align: left; width: 30em; padding:1em;">'''Characterize the symptoms:'''<br> | ||
❑ Asymptomatic <br>❑ [[Palpitations]]<br>❑ [[Dyspnea]] <br>❑ [[Fatigue]] <br> ❑ [[Chest pain|Chest discomfort]] <br>❑ [[Lightheadedness]] <br>❑ [[Syncope|Syncope/Presyncope]] <br>❑ [[Tachycardia]]<br>❑ Weakness <br> | |||
'''Characterize the timing of the symptoms:'''<br> | |||
❑ Onset <br> | |||
:❑ First episode | |||
:❑ Recurrent | |||
❑ Duration <br> | |||
❑ Frequency<br> | |||
{{familytree | | | ❑ Termination of the episode | ||
:❑ Spontaneous | |||
:❑ Medication use | |||
:❑ Not terminated | |||
</div> }} | |||
{{familytree | | |!| | | }} | |||
{{familytree | | B01 | | | B01= <div style="text-align: left; width: 30em; padding:1em;"> '''Identify possible triggers:'''<br> ❑ [[Infection]] <br> ❑ [[Caffeine]] <br> ❑ [[Alcohol]] <br> ❑ [[Nicotine]] <br> ❑ [[Recreational drugs]] <br> ❑ [[Hypovolemia]] <br> ❑ [[Hyperthyroidism]] <br> ❑ [[Hypoxia]] <br> ❑ [[Acidosis]] <br> ❑ [[Hypokalemia]] <br> ❑ [[Hyperkalemia]] <br> ❑ [[Hypoglycemia]] <br> ❑ [[AF|Treatment of Atrial fibrillation]] <br> ❑ [[MI|Acute myocardial infarction]] <br> ❑ [[Digitalis toxicity]] <br> ❑ [[Hypothermia]] <br> ❑ [[Toxins]] <br> ❑ [[Cardiac tamponade]] <br> ❑ Post cardiac surgery <br> ❑ [[Coronary thrombosis]] <br> ❑ [[Trauma]] <br> ❑ [[Pulmonary embolism]] | |||
</div>}} | |||
{{familytree | | |!| | | }} | |||
{{familytree | | C01 | | C01=<div style="text-align: left; width: 30em; padding:1em;"> '''Examine the patient:''' <br> ❑ [[Tachycardia]] <br> ❑ [[Hypotension]] - suggestive of [[ventricular dysfunction]] <br> ❑ [[Diaphoresis]] <br> ❑ [[Congestive heart failure physical examination|Evidence of congestive heart failure]] <br> ❑ Flutter waves in [[jugular vein]] <br> ❑ Signs of [[embolization]] | |||
[[Pulmonary]]: | |||
:❑ [[Dyspnea]] <br> ❑ [[Tachypnea]] <br> ❑ [[Chest pain]] <br> ❑ [[Hemoptysis]] | |||
[[Arterial]]: | |||
:❑ Cold extremities <br> ❑ Loss of distal pulsations <br> ❑ [[Pallor]] of the extremity <br> ❑ Muscle pain/spasm in concerned area <br> ❑ Weakness/lack of movement <br> ❑ [[Paresthesia|Tingling and numbness]] | |||
---- | |||
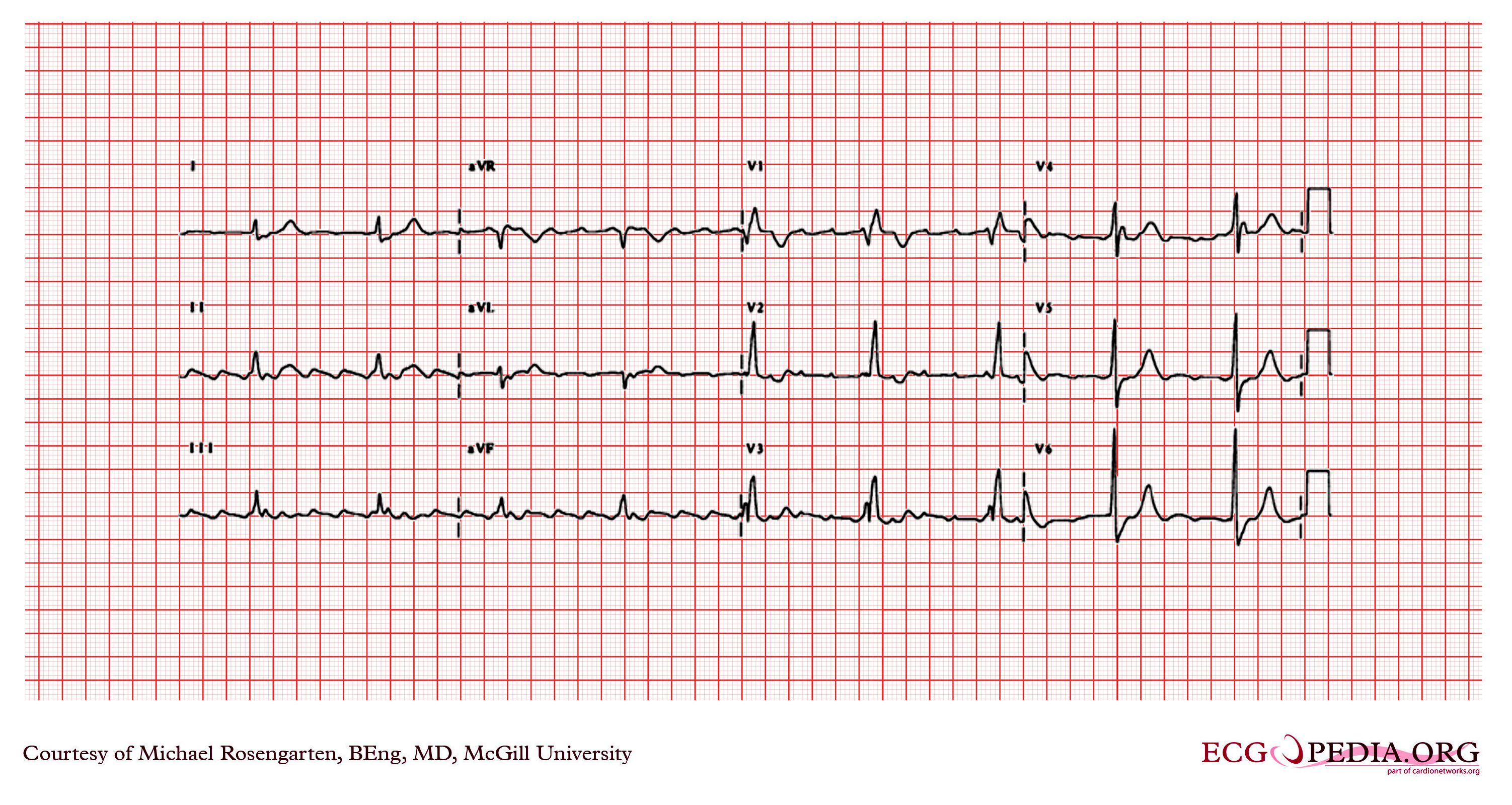
❑ Order an [[ECG]] <br> | |||
♦ Atrial flutter rhythm | |||
:❑ Absent [[P waves]] | |||
:❑ Atrial rate 240-340 beats/minute | |||
:❑ Atrial rate:ventricular rate ratio 2:1 (most commonly) | |||
:❑ Saw tooth pattern in leads II, III, and aVF | |||
[[Image:Atrial flutter and RBBB.jpg|350px]] | |||
♦ Other signs on [[ECG]] | |||
:❑ [[LVH|Left ventricular hypertrophy]] | |||
:❑ [[Preexcitation]] | |||
:❑ [[Bundle branch block]] | |||
:❑ Previous [[myocardial infarction]] | |||
:❑ Other types of [[arrhythmias]] | |||
</div>}} | |||
{{familytree | | |!| | | }} | |||
{{familytree | | D01 | | D01= <div style="text-align: left; width: 30em; padding:1em;"> | |||
'''Order labs:''' <br> | |||
❑ Order a [[TTE|transthoracic echocardiogram]]<br> | |||
❑ [[Holter monitoring]] <br> | |||
❑ Exercise testing <br> | |||
❑ Order [[blood tests]] (if Atrial flutter has not been investigated before) | |||
:❑ [[Thyroid function tests|Thyroid function]] | |||
:❑ [[Renal function]] | |||
:❑ [[LFT|Hepatic function]] </div>}} | |||
{{familytree/end}} <br> | |||
===Therapeutic Approach=== | |||
Shown below is an algorithm summarizing the therapeutic approach to [[atrial flutter]].<ref name="circ.ahajournals.org">{{Cite web | last = | first = | title = ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary | url = http://circ.ahajournals.org/content/108/15/1871 | publisher = | date = | accessdate = 15 August 2013 }}</ref> | |||
{{familytree/start}} | |||
{{familytree | | | | | | | A01 | | | | | | | | | | |A01=[[Atrial flutter]]}} | |||
{{familytree | | | |,|-|-|-|^|-|-|-|.| | | | | | | | }} | |||
{{familytree | | | B01 | | | | | | B02 | | | | | | |B01=Unstable |B02=Stable }} | |||
{{familytree | | | |!| | | | | | | |!| | | | | | | | }} | |||
{{familytree | | | C01 | | | | | | C02 | | | | | | |C01=<div style="float: left; text-align: left; width:28em; padding:1em ">❑ Look for the presence of any of these: <br> | |||
:❑ [[Chronic heart failure]] | |||
:❑ [[Hypotension]] | |||
:❑ [[Acute myocardial infarction]] <br> | |||
❑ If present, attempt direct [[Cardioversion|DC cardioversion]] and then rate control measures as shown in the table below: | |||
<table class="wikitable"> | |||
<tr><td>▸ '''''[[Cardioversion|Conversion]]'''''</td><td> ▸ '''''[[Cardioversion|DC cardioversion]] < 50 J energy with monophasic shocks ([[ACC AHA guidelines classification scheme|class I, level of evidence C]])'''''</td></tr> | |||
<tr><td>▸ '''''Rate control'''''</td><td>▸ '''''[[Beta blockers]] ([[ACC AHA guidelines classification scheme|class IIa, level of evidence C]])'''''<br> or <br>▸ '''''[[Verapamil]] or [[diltiazem]] ([[ACC AHA guidelines classification scheme|class IIa, level of evidence C]])'''''<br> or <br>▸ '''''[[Digitalis]] ([[ACC AHA guidelines classification scheme|class IIb, level of evidence C]])'''''<br> or <br>▸ '''''[[Amiodarone]] ([[ACC AHA guidelines classification scheme|class IIb, level of evidence C]])'''''</td></tr> | |||
</table></div>|C02=<div style="float: left; text-align: left; width:28em;padding:1em "> ❑ Administer [[Atrial flutter resident survival guide#Anticoagulation Therapy|anticoagulation therapy]] based on the risk of [[stroke]], if total duration of flutter > 48 hours <br> ❑ Administer rate control therapy as shown in table below: | |||
<table class="wikitable"> | |||
<tr><td>▸ '''''Rate control'''''</td><td>▸ '''''[[Beta blockers]] ([[ACC AHA guidelines classification scheme|class IIa, level of evidence C]])'''''<br> or <br>▸ '''''[[Verapamil]] or [[diltiazem]] ([[ACC AHA guidelines classification scheme|class IIa, level of evidence C]])'''''<br> or <br>▸ '''''[[Digitalis]] ([[ACC AHA guidelines classification scheme|class IIb, level of evidence C]])'''''<br> or <br>▸ '''''[[Amiodarone]] ([[ACC AHA guidelines classification scheme|class IIb, level of evidence C]])'''''</td></tr> | |||
</table> </div> }} | |||
{{familytree | | | |!| | | | | | | |!| | | | | | | | | }} | |||
{{familytree | | | |!| | | | | | | G01 | | | | | | | |G01=<div style="float: left; text-align: left; width:28em;padding:1em "> ❑ Attempt [[Cardioversion|Conversion]] as shown in table below: <br> | |||
<table class="wikitable"> | |||
<tr><td>▸ '''''[[Cardioversion|Conversion]]'''''</td><td>▸ '''''[[Artificial pacemaker|Atrial or transesophageal pacing]] ([[ACC AHA guidelines classification scheme|class I, level of evidence A]])'''''<br> or <br>▸ '''''[[Cardioversion|DC cardioversion]] ([[ACC AHA guidelines classification scheme|class I, level of evidence C]])'''''<br> or <br>▸ '''''[[Ibutilide]] ([[ACC AHA guidelines classification scheme|class IIa, level of evidence A]])'''''<br> or <br> '''''[[Flecainide]] ([[ACC AHA guidelines classification scheme|class IIb, level of evidence A]])'''''<br> or <br> '''''[[Propafenone]] ([[ACC AHA guidelines classification scheme|class IIb, level of evidence A]])'''''<br> or <br> '''''[[Sotalol]] ([[ACC AHA guidelines classification scheme|class IIb, level of evidence C]])'''''<br> or <br> '''''[[Procainamide]] ([[ACC AHA guidelines classification scheme|class IIb, level of evidence A]])'''''<br> or <br> '''''[[Amiodarone]] ([[ACC AHA guidelines classification scheme|class IIb, level of evidence C]])''''' </td></tr> | |||
</table> </div> }} | |||
{{familytree | | | |`|-|-|-|v|-|-|-|'| | | | | | | | }} | |||
{{familytree | | | | | | | D01 | | | | | | | | | | |D01=<div style="float: left; text-align: left;padding:1em "> ❑ Assess need for therapy to prevent recurrence </div> |}} | |||
{{familytree | | | | | | | |!| | | | | | | | | | | | }} | |||
{{familytree | | | | | | | E01 | | | | | | | | | | |E01=<div style="float: left; text-align: left; width:25em; padding:1em "> ❑ Administer [[antiarrhythmic therapy]] to prevent recurrences as shown below: <br> | |||
<table class="wikitable"> | |||
<tr><td>▸ '''''First episode and well-tolerated atrial flutter'''''</td><td>▸ '''''[[Cardioversion]] alone ([[ACC AHA guidelines classification scheme|class I, level of evidence B]])''''' <br> or <br> ▸ '''''[[Catheter ablation]] ([[ACC AHA guidelines classification scheme|class IIa, level of evidence B]])'''''</td></tr> | |||
<tr><td>▸ '''''Recurrent and well-tolerated atrial flutter'''''</td><td>▸ '''''[[Catheter ablation]]([[ACC AHA guidelines classification scheme|class I, level of evidence B]])'''''<br> or <br>▸ '''''[[Dofetilide]] ([[ACC AHA guidelines classification scheme|class IIa, level of evidence C]])'''''<br> or <br>▸ '''''[[Amiodarone]] ([[ACC AHA guidelines classification scheme|class IIb, level of evidence C]]) <br>or<br> [[Sotalol]] <br>or<br> [[Flecainide]] <br>or<br> [[Quinidine]] <br>or<br> [[Propafenone]] <br>or<br> [[Procainamide]] <br>or<br> [[Disopyramide]]''''' </td></tr> | |||
<tr><td>▸ '''''Poorly tolerated atrial flutter'''''</td><td> ▸ '''''[[Catheter ablation]] ([[ACC AHA guidelines classification scheme|class I, level of evidence B]])'''''</td></tr> | |||
<tr><td>▸ '''''Atrial flutter appearing after use of [[Antiarrhythmic agent#Class Ic agents|class Ic agents]] or [[amiodarone]] for treatment of AF'''''</td><td>▸ '''''[[Catheter ablation]] ([[ACC AHA guidelines classification scheme|class I, level of evidence B]])''''' <br> or <br>▸ '''''Stop current drug and use another ([[ACC AHA guidelines classification scheme|class IIa, level of evidence C]])'''''</td></tr> | |||
<tr><td>▸ '''''Symptomatic non–cavotricuspid isthmus-dependent flutter after failed [[antiarrhythmic therapy]]'''''</td><td>'''''[[Catheter ablation]] ([[ACC AHA guidelines classification scheme|class IIa, level of evidence B]])'''''</td></tr> | |||
</table> | |||
---- | |||
❑ Consider [[Catheter ablation]] if [[antiarrhythmic therapy]] fails </div>}}{{familytree/end}} | |||
==Heart Rate Control== | |||
Shown below is a table summarizing the list of recommended agents for control of heart rate and their dosages.<ref name="Fuster-2011">{{Cite journal | last1 = Fuster | first1 = V. | last2 = Rydén | first2 = LE. | last3 = Cannom | first3 = DS. | last4 = Crijns | first4 = HJ. | last5 = Curtis | first5 = AB. | last6 = Ellenbogen | first6 = KA. | last7 = Halperin | first7 = JL. | last8 = Kay | first8 = GN. | last9 = Le Huezey | first9 = JY. | title = 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. | journal = Circulation | volume = 123 | issue = 10 | pages = e269-367 | month = Mar | year = 2011 | doi = 10.1161/CIR.0b013e318214876d | PMID = 21382897 }}</ref> | |||
{| style="background: #FFFFFF;" | |||
| valign=top | | |||
{| style="float: left; cellpadding=0; cellspacing= 0; width: 600px;" | |||
! style="height: 30px; line-height: 30px; background: #4479BA; border: 0px; font-size: 100%; text-shadow: 0 -1px 0 rgba(0, 0, 0, 0.5);" align=center; colspan="3"| {{fontcolor|#FFF|Heart Rate Control in Acute Setting}} | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''Drug'''|| style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''Loading dose''' || style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''Maintenance dose''' | |||
|- | |||
| style="padding: 0 5px; font-size: 90%; background: #F5F5F5;" align=center; colspan="3" | '''''Heart rate control in patients without [[accessory pathway]]''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Esmolol]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence C]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''500 mcg/kg IV over 1 min''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''60 to 200 mcg/kg/min IV''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Propanolol]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence C]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''0.15 mg/kg IV''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''NA''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Metoprolol]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence C]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''2.5 to 5 mg IV bolus over 2 min; up to 3 doses''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''NA''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Diltiazem]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence B]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''0.25 mg/kg IV over 2 min''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''5 to 15 mg/h IV''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Verapamil]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence B]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''0.075 to 0.15 mg/kg IV over 2 min''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''NA''''' | |||
|- | |||
| style="padding: 0 5px; font-size: 90%; background: #F5F5F5;" align=center; colspan="3" | '''''Heart rate control in patients with [[accessory pathway]]''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Amiodarone]] <br>([[ACC AHA guidelines classification scheme|class IIa, level of evidence C]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''150 mg over 10 min''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''0.5 to 1 mg/min IV''''' | |||
|- | |||
| style="padding: 0 5px; font-size: 90%; background: #F5F5F5;" align=center; colspan="3" | '''''Heart Rate Control in patients with [[heart failure]] and without [[accessory pathway]]''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Digoxin]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence B]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''0.25 mg IV each 2 h, up to 1.5 mg''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''0.125 to 0.375 mg daily IV or orally''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Amiodarone]] <br>([[ACC AHA guidelines classification scheme|class IIa, level of evidence C]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''150 mg over 10 min''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''0.5 to 1 mg/min IV''''' | |||
|- | |||
| style="height: 30px; line-height: 30px; background: #4479BA; border: 0px; font-size: 100%; text-shadow: 0 -1px 0 rgba(0, 0, 0, 0.5);" align=center colspan="3"| {{fontcolor|#FFF|'''Heart Rate Control in Non Acute Setting and Long Term Maintenance'''}} | |||
|- | |||
| style="padding: 0 5px; font-size: 90%; background: #F5F5F5;" align=center; colspan="3" | '''''Heart rate control''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Metoprolol]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence C]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''25 to 100 mg twice a day, orally''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''25 to 100 mg twice a day, orally''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Propanolol]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence C]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''80 to 240 mg daily in divided doses, orally''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''80 to 240 mg daily in divided doses, orally''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Verapamil]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence B]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''120 to 360 mg daily in divided doses, orally''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''120 to 360 mg daily in divided doses, orally''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Diltiazem]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence B]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''120 to 360 mg daily in divided doses, orally''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''120 to 360 mg daily in divided doses, orally''''' | |||
|- | |||
| style="padding: 0 5px; font-size: 90%; background: #F5F5F5;" align=center; colspan="3" | '''''Heart Rate Control in patients with heart failure and without accessory pathway''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Digoxin]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence B]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''0.5 mg by mouth daily''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''0.125 to 0.375 mg daily, orally''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Amiodarone]] <br>([[ACC AHA guidelines classification scheme|class IIb, level of evidence C]])''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''800 mg daily for 1 week, orally <br> 600 mg daily for 1 week, orally <br> 400 mg daily for 4 to 6 week, orally''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''200 mg daily, orally''''' | |||
|- | |||
|} | |||
|} | |||
===Pharmacological cardioversion=== | |||
{| style="background: #FFFFFF;" | |||
| valign=top | | |||
{| style="float: left; cellpadding=0; cellspacing= 0; width: 600px;" | |||
! style="height: 30px; line-height: 30px; background: #4479BA; border: 0px; font-size: 100%; text-shadow: 0 -1px 0 rgba(0, 0, 0, 0.5);" align=center; colspan="2"| {{fontcolor|#FFF|Pharmacological Cardioversion for Atrial Flutter}} | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''Drug''' || style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''Dosage''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Flecainide]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence A]]) ''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ ''''' Oral: 200 to 300 mg <br> ▸ Intravenous: 1.5 to 3.0 mg/kg, over 10 to 20 min''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Ibutilide]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence A]]) ''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''Intravenous: 1 mg over 10 min, repeat 1 mg if necessary''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Propafenone]] <br>([[ACC AHA guidelines classification scheme|class I, level of evidence A]]) ''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ ''''' Oral: 600 mg <br> ▸ Intravenous: 1.5 to 2.0 mg/kg, over 10 to 20 min''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Amiodarone]] <br>([[ACC AHA guidelines classification scheme|class IIa, level of evidence A]]) ''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ ''''' Oral:''''' | |||
: '''''Inpatient'''''<br> | |||
:▸ '''''1.2 to 1.8 g per day in divided dose until a maximum of 10 g '''''<br> | |||
:▸ '''''Followed by a maintenance dose of 200 to 400 mg per day or 30 mg/kg''''' <br> | |||
: '''''Outpatient''''' | |||
:▸ '''''600 to 800 mg per day divided dose until a maximum of 10 g'''''<br> | |||
:▸ '''''Followed by a maintenance dose of 200 to 400 mg per day ''''' <br> | |||
▸ '''''Intravenous:''''' | |||
: '''''5 to 7 mg/kg, over 30 to 60 min''''' <br> '''''Followed by 1.2 to 1.8 g per day continuous IV''''' <br> ''OR''<br> | |||
: '''''5 to 7 mg/kg, in divided oral doses until a maximum of 10 g <br> Followe by a maintenance dose of 200 to 400 mg per day''''' | |||
|- | |||
|} | |||
|} | |||
===Antiarrhythmic Therapy=== | |||
{| style="background: #FFFFFF;" | |||
'' | | valign=top | | ||
{| style="float: left; cellpadding=0; cellspacing= 0; width: 600px;" | |||
! style="height: 30px; line-height: 30px; background: #4479BA; border: 0px; font-size: 100%; text-shadow: 0 -1px 0 rgba(0, 0, 0, 0.5);" align=center; colspan="2"| {{fontcolor|#FFF|Maintenance of Sinus Rhythm}} | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Amiodarone]] (100 to 400 mg)'''''<BR>''OR''<BR>▸ '''''[[Disopyramide]] (400 to 750 mg)'''''<BR>''OR''<BR> ▸ '''''[[Dofetilide]] (500 to 1000 mcg)'''''<BR>''OR''<BR>▸ '''''[[Flecainide]] (200 to 300 mg)'''''<BR>''OR''<BR>▸ '''''[[Procainamide]] (1000 to 4000 mcg)'''''<BR>''OR''<BR>▸ '''''[[Propafenone]] (450 to 900 mg)'''''<BR>''OR''<BR>▸ '''''[[Quinidine]] (600 to 1500 mg)'''''<BR>''OR''<BR>▸ '''''[[Sotalol]] (160 to 320 mg)''''' | |||
|- | |||
|} | |||
|} | |||
==Anticoagulation Therapy== | |||
Shown below are tables depicting the assessment of risk of stroke and the appropriate anticoagulation therapy among patients with Atrial flutter.<ref name="Fuster-2011">{{Cite journal | last1 = Fuster | first1 = V. | last2 = Rydén | first2 = LE. | last3 = Cannom | first3 = DS. | last4 = Crijns | first4 = HJ. | last5 = Curtis | first5 = AB. | last6 = Ellenbogen | first6 = KA. | last7 = Halperin | first7 = JL. | last8 = Kay | first8 = GN. | last9 = Le Huezey | first9 = JY. | title = 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. | journal = Circulation | volume = 123 | issue = 10 | pages = e269-367 | month = Mar | year = 2011 | doi = 10.1161/CIR.0b013e318214876d | PMID = 21382897 }}</ref> | |||
{| style="background: #FFFFFF;" | |||
| valign=top | | |||
{| style="float: left; cellpadding=0; cellspacing= 0; width: 600px;" | |||
! style="height: 30px; line-height: 30px; background: #4479BA; border: 0px; font-size: 100%; text-shadow: 0 -1px 0 rgba(0, 0, 0, 0.5);" align=center; colspan="2"| {{fontcolor|#FFF|Anticoagulation Therapy}} | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | '''''No risk factors''''' ||style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''[[Aspirin]] 81-325 mg daily''''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |'''''1 Moderate risk factor''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |▸ '''''[[Aspirin]] 81-325 mg daily''''' <br> ''OR'' <br> ▸ '''''[[Warfarin]] (INR 2.0 to 3.0, target 2.5)''''' | |||
|- | |||
|style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |'''''Any high risk factor or <br> more than 1 moderate risk factor''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |▸ '''''[[Warfarin]] (INR 2.0 to 3.0, target 2.5)''''' | |||
|- | |||
|} | |||
|} | |||
<br> | |||
{| style="background: #FFFFFF;" | |||
| valign=top | | |||
{| style="float: left; cellpadding=0; cellspacing= 0; width: 600px;" | |||
! style="height: 30px; line-height: 30px; background: #4479BA; border: 0px; font-size: 100%; text-shadow: 0 -1px 0 rgba(0, 0, 0, 0.5);" align=center; colspan="2"| {{fontcolor|#FFF|Risk Factors for Stroke}} | |||
|- | |||
{| style="cellpadding=0; cellspacing= 0; width: 600px;" | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''Low Risk Factors'''|| style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''Moderate Risk Factors'''|| style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''High Risk Factors''' | |||
|- | |||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ▸ '''''Female gender'''''<BR>▸ '''''Age 65-74 years'''''<BR> ▸ '''''[[Coronary artery disease]]'''''<BR>▸ '''''[[Thyrotoxicosis]]'''''|| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |▸ '''''Age ≥ 75 years'''''<BR>▸ '''''[[Hypertension]]'''''<BR> ▸ '''''[[Heart failure]]'''''<BR>▸ '''''LV [[ejection fraction]] ≤ 35%'''''<BR>▸ '''''[[Diabetes mellitus]]''''' || style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |▸ '''''Previous [[stroke]], [[TIA]] or [[embolism]]'''''<BR>▸ '''''[[Mitral stenosis]]'''''<BR> ▸ '''''[[Prosthetic heart valve]]''''' | |||
|- | |||
|} | |||
|} | |||
==Do's== | |||
* [[Antiarrhythmic therapy|Class Ic drugs]] can enhance AV conduction by slowing the atrial rate, so combine them with [[Atrial flutter resident survival guide#heart Rate Control|AV nodal blocking agents]] such as [[beta blockers]] or [[calcium channel blockers]]. | |||
* Prefer [[dofetilide]] or [[ibutilide]] over [[sotalol]] or [[Antiarrhythmic therapy|class I agents]], though the former have a slightly higher rate of [[torsades de pointes]]. | |||
* Prefer direct current [[cardioversion|DC cardioversion]] when rapid termination of flutter is needed. | |||
* Prefer overdrive [[Cardiac pacing|pacing]] in patients with flutter after cardiac surgery, it also facilitates conversion by drugs. | |||
==Don'ts== | |||
* Do not use IV [[ibutilide]] in patients with structural cardiac diseases or prolonged QT interval or in those with [[sinus node]] disease. | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
==References== | |||
{{Reflist|2}} | |||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Resident survival guide]] | [[Category:Resident survival guide]] | ||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Latest revision as of 17:45, 31 March 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Hilda Mahmoudi M.D., M.P.H.[2]; Priyamvada Singh, M.D. [3]
| Atrial fibrillation resident survival guide Microchapters |
|---|
| Overview |
| Causes |
| Diagnosis |
| Treatment |
| Heart Rate Control |
| Pharmacological Cardioverion |
| Antiarrhythmic Therapy |
| Anticoagulation Therapy |
| Do's |
| Dont's |
Overview
Atrial flutter is a reenterant arrhythmia, with atrial rates between 240 and 340/min, with a regular ventricular response and a saw tooth pattern on EKG. While it occurs mostly in patients with structural heart disease, it may also occur in patients with normal heart. It presents with palpitations, dyspnea, fatigue, lightheadedness etc. A typical flutter rhythm on EKG consists of absent P waves, saw tooth pattern in leads II, III and aVF, an atrial rate of 240-340 beats/min and an atrial rate:ventricular rate ratio 2:1 (most commonly). The treatment consists of rate control, anticoagulation therapy and cardioversion if the flutter is well tolerated. In those with poorly tolerated flutter or hemodynamic instability direct DC cardioversion is attempted, followed by rate control therapy.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. Atrial flutter can be a life-threatening condition and must be treated as such irrespective of the causes.
Common Causes
- Acute coronary syndromes
- Cardiomyopathy
- Carbon monoxide poisoning
- Congenital heart disease
- Hypertensive heart disease
- Hyperthyroidism
- Mitral valve disease[1] [2]
- Pulmonary embolism
- Myocardial infarction
Management
Diagnostic Approach
Shown below is an algorithm summarizing the initial approach to atrial flutter.
Characterize the symptoms: ❑ Asymptomatic
❑ Duration
| |||||||||||
Identify possible triggers: ❑ Infection ❑ Caffeine ❑ Alcohol ❑ Nicotine ❑ Recreational drugs ❑ Hypovolemia ❑ Hyperthyroidism ❑ Hypoxia ❑ Acidosis ❑ Hypokalemia ❑ Hyperkalemia ❑ Hypoglycemia ❑ Treatment of Atrial fibrillation ❑ Acute myocardial infarction ❑ Digitalis toxicity ❑ Hypothermia ❑ Toxins ❑ Cardiac tamponade ❑ Post cardiac surgery ❑ Coronary thrombosis ❑ Trauma ❑ Pulmonary embolism | |||||||||||
Examine the patient: ❑ Tachycardia ❑ Hypotension - suggestive of ventricular dysfunction ❑ Diaphoresis ❑ Evidence of congestive heart failure ❑ Flutter waves in jugular vein ❑ Signs of embolization
❑ Order an ECG
| |||||||||||
Order labs: | |||||||||||
Therapeutic Approach
Shown below is an algorithm summarizing the therapeutic approach to atrial flutter.[3]
Heart Rate Control
Shown below is a table summarizing the list of recommended agents for control of heart rate and their dosages.[4]
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Pharmacological cardioversion
| ||||||||||||
Antiarrhythmic Therapy
| |||
Anticoagulation Therapy
Shown below are tables depicting the assessment of risk of stroke and the appropriate anticoagulation therapy among patients with Atrial flutter.[4]
| ||||||||
| ||||||||
Do's
- Class Ic drugs can enhance AV conduction by slowing the atrial rate, so combine them with AV nodal blocking agents such as beta blockers or calcium channel blockers.
- Prefer dofetilide or ibutilide over sotalol or class I agents, though the former have a slightly higher rate of torsades de pointes.
- Prefer direct current DC cardioversion when rapid termination of flutter is needed.
- Prefer overdrive pacing in patients with flutter after cardiac surgery, it also facilitates conversion by drugs.
Don'ts
- Do not use IV ibutilide in patients with structural cardiac diseases or prolonged QT interval or in those with sinus node disease.
References
- ↑ Gutierrez SD, Earing MG, Singh AK, Tweddell JS, Bartz PJ (2012). "Atrial Tachyarrhythmias and the Cox-maze Procedure in Congenital Heart Disease". Congenit Heart Dis. doi:10.1111/chd.12031. PMID 23280242. Unknown parameter
|month=ignored (help) - ↑ Granada, J.; Uribe, W.; Chyou, PH.; Maassen, K.; Vierkant, R.; Smith, PN.; Hayes, J.; Eaker, E.; Vidaillet, H. (2000). "Incidence and predictors of atrial flutter in the general population". J Am Coll Cardiol. 36 (7): 2242–6. PMID 11127467. Unknown parameter
|month=ignored (help) - ↑ "ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary". Retrieved 15 August 2013.
- ↑ 4.0 4.1 Fuster, V.; Rydén, LE.; Cannom, DS.; Crijns, HJ.; Curtis, AB.; Ellenbogen, KA.; Halperin, JL.; Kay, GN.; Le Huezey, JY. (2011). "2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines". Circulation. 123 (10): e269–367. doi:10.1161/CIR.0b013e318214876d. PMID 21382897. Unknown parameter
|month=ignored (help)