Pulmonary embolism history and symptoms: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (88 intermediate revisions by 13 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{| class="infobox" style="float:right;" | |||
|- | |||
| [[File:Siren.gif|30px|link=Pulmonary embolism resident survival guide]]|| <br> || <br> | |||
| [[Pulmonary embolism resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] | |||
|} | |||
{{Pulmonary embolism}} | {{Pulmonary embolism}} | ||
'''Editor(s)-In-Chief:''' [[C. Michael Gibson, M.S., M.D.]] [mailto:charlesmichaelgibson@gmail.com], {{ATI}}; {{AE}} {{Rim}} | |||
{{ | ==Overview== | ||
A proper history and physical exam is crucial to establish an accurate diagnosis of [[pulmonary embolism]] (PE). The [[symptoms]] of [[pulmonary embolism]] (PE) depend on the [[severity]] of the disease, ranging from mild [[dyspnea]], [[chest pain]], and [[cough]], to sustained [[hypotension]] and [[shock]].<ref name="pmid17904458">{{cite journal |author=Stein PD, Beemath A, Matta F, Weg JG, Yusen RD, Hales CA, Hull RD, Leeper KV, Sostman HD, Tapson VF, Buckley JD, Gottschalk A, Goodman LR, Wakefied TW, Woodard PK |title=Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II |journal=[[The American Journal of Medicine]] |volume=120 |issue=10 |pages=871–9 |year=2007 |month=October |pmid=17904458 |pmc=2071924 |doi=10.1016/j.amjmed.2007.03.024 |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9343(07)00463-9 |accessdate=2012-04-26}}</ref><ref name="pmid20592294">{{cite journal |author=Agnelli G, Becattini C |title=Acute pulmonary embolism |journal=[[The New England Journal of Medicine]] |volume=363 |issue=3 |pages=266–74 |year=2010 |month=July |pmid=20592294 |doi=10.1056/NEJMra0907731 |url=http://www.nejm.org/doi/abs/10.1056/NEJMra0907731?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed |accessdate=2012-04-26}}</ref> A [[PE]] may also be an incidental finding in so far as many patients are asymptomatic.<ref name="pmid20592294">{{cite journal |author=Agnelli G, Becattini C |title=Acute pulmonary embolism |journal=[[The New England Journal of Medicine]] |volume=363 |issue=3 |pages=266–74 |year=2010 |month=July |pmid=20592294 |doi=10.1056/NEJMra0907731 |url=http://www.nejm.org/doi/abs/10.1056/NEJMra0907731?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed |accessdate=2012-04-26}}</ref><ref name="pmid20399319">{{cite journal |author=Stein PD, Matta F, Musani MH, Diaczok B |title=Silent pulmonary embolism in patients with deep venous thrombosis: a systematic review |journal=[[The American Journal of Medicine]] |volume=123 |issue=5 |pages=426–31 |year=2010 |month=May |pmid=20399319 |doi=10.1016/j.amjmed.2009.09.037 |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9343(09)01111-5 |accessdate=2012-04-26}}</ref> [[Sudden death]] can be the initial presentation of PE. One of the first steps in the management of [[PE]] is the determination of the [[Wells score for PE]], whose criteria can be ascertained solely on the basis of history and physical exam. [[Deep vein thrombosis history and symptoms|Symptoms of DVT]] of the lower extremity may be present. | |||
==History and Symptoms== | |||
As depicted in the image below, the majority of patients with [[venous thromboembolism]] (VTE), that is [[DVT]], [[PE]], or both, are [[asymptomatic]]. | |||
[[File:Challenge of Assessing VTE.JPG|300x400px|The challenge in diagnosis of VTE]] | |||
===Symptoms of PE=== | |||
The Prospective Investigation Of Pulmonary Embolism Diagnosis II (PIOPED II) study identified the triad of [[symptoms]], [[dyspnea]], [[chest pain]], and [[tachypnea]], present in a majority of patients with a confirmed [[pulmonary embolism]].<ref name="pmid17904458">{{cite journal |author=Stein PD, Beemath A, Matta F, Weg JG, Yusen RD, Hales CA, Hull RD, Leeper KV, Sostman HD, Tapson VF, Buckley JD, Gottschalk A, Goodman LR, Wakefied TW, Woodard PK |title=Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II |journal=[[The American Journal of Medicine]] |volume=120 |issue=10 |pages=871–9 |year=2007 |month=October |pmid=17904458 |pmc=2071924 |doi=10.1016/j.amjmed.2007.03.024 |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9343(07)00463-9 |accessdate=2012-04-26}}</ref><ref name="pmid16738268">{{cite journal |author=Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, Leeper KV, Popovich J, Quinn DA, Sos TA, Sostman HD, Tapson VF, Wakefield TW, Weg JG, Woodard PK |title=Multidetector computed tomography for acute pulmonary embolism |journal=[[The New England Journal of Medicine]] |volume=354 |issue=22 |pages=2317–27 |year=2006 |month=June |pmid=16738268 |doi=10.1056/NEJMoa052367 |url=http://dx.doi.org/10.1056/NEJMoa052367 |accessdate=2012-04-26}}</ref> Symptoms of PE include: | |||
* [[Dyspnea]] (78–81%)<ref name="pmid24182642">{{cite journal| author=Cohen AT, Dobromirski M, Gurwith MM| title=Managing pulmonary embolism from presentation to extended treatment. | journal=Thromb Res | year= 2014 | volume= 133 | issue= 2 | pages= 139-48 | pmid=24182642 | doi=10.1016/j.thromres.2013.09.040 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24182642 }} </ref> <br> | |||
* [[Pleuritic chest pain]] (39–56%)<ref name="pmid24182642">{{cite journal| author=Cohen AT, Dobromirski M, Gurwith MM| title=Managing pulmonary embolism from presentation to extended treatment. | journal=Thromb Res | year= 2014 | volume= 133 | issue= 2 | pages= 139-48 | pmid=24182642 | doi=10.1016/j.thromres.2013.09.040 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24182642 }} </ref> <br> | |||
* [[Fainting]] (22–26%)<ref name="pmid24182642">{{cite journal| author=Cohen AT, Dobromirski M, Gurwith MM| title=Managing pulmonary embolism from presentation to extended treatment. | journal=Thromb Res | year= 2014 | volume= 133 | issue= 2 | pages= 139-48 | pmid=24182642 | doi=10.1016/j.thromres.2013.09.040 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24182642 }} </ref> <br> | |||
* [[Cough]] (20%)<ref name="pmid18757870">{{cite journal| author=Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P et al.| title=Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). | journal=Eur Heart J | year= 2008 | volume= 29 | issue= 18 | pages= 2276-315 | pmid=18757870 | doi=10.1093/eurheartj/ehn310 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18757870 }} </ref><br> | |||
* [[Substernal chest pain]] (12%)<ref name="pmid18757870">{{cite journal| author=Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P et al.| title=Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). | journal=Eur Heart J | year= 2008 | volume= 29 | issue= 18 | pages= 2276-315 | pmid=18757870 | doi=10.1093/eurheartj/ehn310 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18757870 }} </ref><br> | |||
* [[Hemoptysis]] (11%)<ref name="pmid18757870">{{cite journal| author=Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P et al.| title=Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). | journal=Eur Heart J | year= 2008 | volume= 29 | issue= 18 | pages= 2276-315 | pmid=18757870 | doi=10.1093/eurheartj/ehn310 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18757870 }} </ref><br> | |||
* [[Wheezing]] <br> | |||
* [[Cyanosis]] (11%)<ref name="pmid24182642">{{cite journal| author=Cohen AT, Dobromirski M, Gurwith MM| title=Managing pulmonary embolism from presentation to extended treatment. | journal=Thromb Res | year= 2014 | volume= 133 | issue= 2 | pages= 139-48 | pmid=24182642 | doi=10.1016/j.thromres.2013.09.040 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24182642 }} </ref> <br> | |||
* [[Fever]] (7%)<ref name="pmid24182642">{{cite journal| author=Cohen AT, Dobromirski M, Gurwith MM| title=Managing pulmonary embolism from presentation to extended treatment. | journal=Thromb Res | year= 2014 | volume= 133 | issue= 2 | pages= 139-48 | pmid=24182642 | doi=10.1016/j.thromres.2013.09.040 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24182642 }} </ref> <br> | |||
*[[Symptoms]] suggestive of [[shock]] (in case of massive PE) | |||
** [[Altered mental status]] | |||
** [[Cold extremities]] | |||
** [[Cyanosis]] | |||
** [[Oliguria]] | |||
* [[Sudden death]] may be the initial presentation of [[PE]]. | |||
== | ===Symptoms of [[DVT]]=== | ||
*[[ | Since [[VTE]] involves both [[DVT]] and [[PE]], the patient can present with complaints of either of the diseases. Therefore it is important to inquire about the [[symptoms]] of both diseases. | ||
* | |||
*[[ | ====Common Symptoms of [[DVT]]==== | ||
The classical symptoms of [[DVT]] include: | |||
* [[Pain and nociception|Pain]] in the affected area | |||
* [[Swelling]] of the affected area | |||
* [[Erythema]] around the affected area | |||
* [[Dilation]] of the surface [[veins]] and [[erythema]] of the overlying area | |||
However, sometimes there may be no symptoms referable to the location of the [[DVT]]. | |||
<gallery> | |||
Image:Extremities dvt.jpg|Front View:Edematous Right Leg | |||
Image:Extremities dvt2.jpg|Rear View:Left limb edema localized to calf. | |||
Image:Extremities dvt3.jpg|Front View:Left limb edema localized to calf. | |||
</gallery> | |||
=== | ====Less Common Symptoms of [[DVT]]==== | ||
* In [[phlegmasia alba dolens]], the leg is pale and cold with a diminished [[arterial]] pulse. | |||
* In [[phlegmasia cerulea dolens]], there is an [[acute]] and near-total [[venous]] occlusion of the entire extremity outflow, including the [[iliac vein|iliac]] and [[femoral vein]]s. The leg is usually painful, [[cyanosis|cyanosed]] and [[edema|edematous]]. | |||
===Complete History=== | |||
If [[VTE]] is suspected or diagnosed, a complete history should be elicited, including the following: | |||
* '''Risk factors'''<ref name="pmid12814980">{{cite journal| author=Anderson FA, Spencer FA| title=Risk factors for venous thromboembolism. | journal=Circulation | year= 2003 | volume= 107 | issue= 23 Suppl 1 | pages= I9-16 | pmid=12814980 | doi=10.1161/01.CIR.0000078469.07362.E6 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12814980 }} </ref><ref name="pmid18757870">{{cite journal| author=Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P et al.| title=Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). | journal=Eur Heart J | year= 2008 | volume= 29 | issue= 18 | pages= 2276-315 | pmid=18757870 | doi=10.1093/eurheartj/ehn310 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18757870 }} </ref> | |||
** [[Chemotherapy]]<br> | |||
** [[Chronic heart failure]]<br> | |||
** [[Respiratory failure]]<br> | |||
** [[Hormone replacement therapy]]<br> | |||
** [[Cancer]]<br> | |||
** [[Oral contraceptive pills]] <br> | |||
** [[Stroke]] <br> | |||
** [[Pregnancy]] <br> | |||
** [[Postpartum]] <br> | |||
** Prior history of [[VTE]] <br> | |||
** [[Thrombophilia]] <br> | |||
** Advanced [[age]] <br> | |||
** [[Laparoscopic surgery]] <br> | |||
** Prepartum <br> | |||
** [[Obesity]] <br> | |||
** [[Varicose veins]] | |||
* '''Triggers'''<ref name="pmid12814980">{{cite journal| author=Anderson FA, Spencer FA| title=Risk factors for venous thromboembolism. | journal=Circulation | year= 2003 | volume= 107 | issue= 23 Suppl 1 | pages= I9-16 | pmid=12814980 | doi=10.1161/01.CIR.0000078469.07362.E6 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12814980 }} </ref><ref name="pmid18757870">{{cite journal| author=Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P et al.| title=Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). | journal=Eur Heart J | year= 2008 | volume= 29 | issue= 18 | pages= 2276-315 | pmid=18757870 | doi=10.1093/eurheartj/ehn310 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18757870 }} </ref> | |||
** [[Bone fracture]] ([[hip]] or [[leg]]) <br> | |||
** [[Hip replacement surgery]]<br> | |||
** Knee replacement surgery<br> | |||
** [[General surgery|Major general surgery]]<br> | |||
** [[Trauma|Significant trauma]]<br> | |||
** [[Spinal cord injury]]<br> | |||
** Athroscopic knee surgery<br> | |||
** [[Central venous line]]s<br> | |||
** [[Chemotherapy]]<br> | |||
** Bed rest for more than 3 days <br> | |||
** Prolonged car or air travel <br> | |||
** [[Laparoscopic surgery]] <br> | |||
** Prepartum <br> | |||
* '''Previous episode of [[VTE]]''' | |||
** Age | |||
** Location | |||
* '''Past medical history of diseases associated with hyperviscosity''' | |||
** [[Atherosclerosis]] | |||
** [[Collagen vascular disease]] | |||
** [[Heart failure]] | |||
** [[Myeloproliferative disease]] | |||
** [[Nephrotic syndrome]] | |||
** [[Autoimmune diseases]] | |||
**[[Polycythemia vera]] | |||
** [[Hyperhomocysteinemia]] | |||
** [[Paroxysmal nocturnal hemoglobinuria]] | |||
** [[Waldenstrom macroglobulinemia]] | |||
** [[Multiple myeloma]] | |||
* '''History of [[thrombophilia]]''' | |||
** [[Factor V Leiden mutation]] | |||
** [[Prothrombin gene mutation G20210A]] | |||
** [[Protein C]] or [[Protein S]] deficiency | |||
** [[Antithrombin]] (AT) deficiency | |||
** [[Antiphospholipid syndrome]] (APS) | |||
* '''Abortion''' | |||
** [[Abortion]] at second or third trimester of [[pregnancy]] (suggestive of an inherited [[thrombophilia]] or APS) | |||
* '''Drugs that may increase the risk of [[VTE]]''' | |||
** [[Hydralazine]] | |||
** [[Phenothiazine]] | |||
** [[Procainamide]] | |||
** [[Tamoxifen]] | |||
** [[Bevacizumab]] | |||
** [[Glucocorticoids]] | |||
* '''Family history (suggestive of [[inherited thrombophilia]])''' | |||
** [[Deep vein thrombosis]] | |||
** [[Pulmonary embolism]] | |||
** Recurrent [[miscarriage]] | |||
* '''Social history''' | |||
** Heavy [[cigarette smoking]] (>25 cigarettes per day) | |||
** [[Intravenous drug use]] (if injected directly in [[femoral vein]]) | |||
** [[Alcohol]] | |||
==References== | ==References== | ||
{{ | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Hematology]] | [[Category:Hematology]] | ||
| Line 35: | Line 139: | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Intensive care medicine]] | |||
Latest revision as of 23:53, 29 July 2020
| Resident Survival Guide |
|
Pulmonary Embolism Microchapters |
|
Diagnosis |
|---|
|
Pulmonary Embolism Assessment of Probability of Subsequent VTE and Risk Scores |
|
Treatment |
|
Follow-Up |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Pulmonary embolism history and symptoms On the Web |
|
Directions to Hospitals Treating Pulmonary embolism history and symptoms |
|
Risk calculators and risk factors for Pulmonary embolism history and symptoms |
Editor(s)-In-Chief: C. Michael Gibson, M.S., M.D. [1], The APEX Trial Investigators; Associate Editor(s)-in-Chief: Rim Halaby, M.D. [2]
Overview
A proper history and physical exam is crucial to establish an accurate diagnosis of pulmonary embolism (PE). The symptoms of pulmonary embolism (PE) depend on the severity of the disease, ranging from mild dyspnea, chest pain, and cough, to sustained hypotension and shock.[1][2] A PE may also be an incidental finding in so far as many patients are asymptomatic.[2][3] Sudden death can be the initial presentation of PE. One of the first steps in the management of PE is the determination of the Wells score for PE, whose criteria can be ascertained solely on the basis of history and physical exam. Symptoms of DVT of the lower extremity may be present.
History and Symptoms
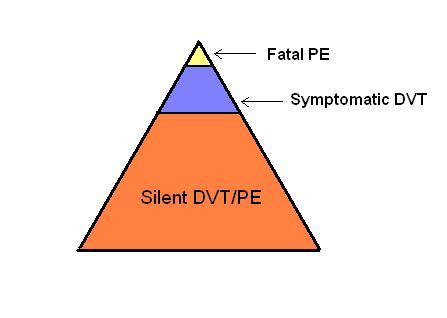
As depicted in the image below, the majority of patients with venous thromboembolism (VTE), that is DVT, PE, or both, are asymptomatic.
Symptoms of PE
The Prospective Investigation Of Pulmonary Embolism Diagnosis II (PIOPED II) study identified the triad of symptoms, dyspnea, chest pain, and tachypnea, present in a majority of patients with a confirmed pulmonary embolism.[1][4] Symptoms of PE include:
- Dyspnea (78–81%)[5]
- Pleuritic chest pain (39–56%)[5]
- Fainting (22–26%)[5]
- Cough (20%)[6]
- Substernal chest pain (12%)[6]
- Hemoptysis (11%)[6]
- Wheezing
- Cyanosis (11%)[5]
- Fever (7%)[5]
- Symptoms suggestive of shock (in case of massive PE)
- Sudden death may be the initial presentation of PE.
Symptoms of DVT
Since VTE involves both DVT and PE, the patient can present with complaints of either of the diseases. Therefore it is important to inquire about the symptoms of both diseases.
Common Symptoms of DVT
The classical symptoms of DVT include:
- Pain in the affected area
- Swelling of the affected area
- Erythema around the affected area
- Dilation of the surface veins and erythema of the overlying area
However, sometimes there may be no symptoms referable to the location of the DVT.
-
Front View:Edematous Right Leg
-
Rear View:Left limb edema localized to calf.
-
Front View:Left limb edema localized to calf.
Less Common Symptoms of DVT
- In phlegmasia alba dolens, the leg is pale and cold with a diminished arterial pulse.
- In phlegmasia cerulea dolens, there is an acute and near-total venous occlusion of the entire extremity outflow, including the iliac and femoral veins. The leg is usually painful, cyanosed and edematous.
Complete History
If VTE is suspected or diagnosed, a complete history should be elicited, including the following:
- Risk factors[7][6]
- Chemotherapy
- Chronic heart failure
- Respiratory failure
- Hormone replacement therapy
- Cancer
- Oral contraceptive pills
- Stroke
- Pregnancy
- Postpartum
- Prior history of VTE
- Thrombophilia
- Advanced age
- Laparoscopic surgery
- Prepartum
- Obesity
- Varicose veins
- Chemotherapy
- Triggers[7][6]
- Bone fracture (hip or leg)
- Hip replacement surgery
- Knee replacement surgery
- Major general surgery
- Significant trauma
- Spinal cord injury
- Athroscopic knee surgery
- Central venous lines
- Chemotherapy
- Bed rest for more than 3 days
- Prolonged car or air travel
- Laparoscopic surgery
- Prepartum
- Bone fracture (hip or leg)
- Previous episode of VTE
- Age
- Location
- Past medical history of diseases associated with hyperviscosity
- History of thrombophilia
- Factor V Leiden mutation
- Prothrombin gene mutation G20210A
- Protein C or Protein S deficiency
- Antithrombin (AT) deficiency
- Antiphospholipid syndrome (APS)
- Abortion
- Abortion at second or third trimester of pregnancy (suggestive of an inherited thrombophilia or APS)
- Drugs that may increase the risk of VTE
- Family history (suggestive of inherited thrombophilia)
- Social history
- Heavy cigarette smoking (>25 cigarettes per day)
- Intravenous drug use (if injected directly in femoral vein)
- Alcohol
References
- ↑ 1.0 1.1 Stein PD, Beemath A, Matta F, Weg JG, Yusen RD, Hales CA, Hull RD, Leeper KV, Sostman HD, Tapson VF, Buckley JD, Gottschalk A, Goodman LR, Wakefied TW, Woodard PK (2007). "Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II". The American Journal of Medicine. 120 (10): 871–9. doi:10.1016/j.amjmed.2007.03.024. PMC 2071924. PMID 17904458. Retrieved 2012-04-26. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 Agnelli G, Becattini C (2010). "Acute pulmonary embolism". The New England Journal of Medicine. 363 (3): 266–74. doi:10.1056/NEJMra0907731. PMID 20592294. Retrieved 2012-04-26. Unknown parameter
|month=ignored (help) - ↑ Stein PD, Matta F, Musani MH, Diaczok B (2010). "Silent pulmonary embolism in patients with deep venous thrombosis: a systematic review". The American Journal of Medicine. 123 (5): 426–31. doi:10.1016/j.amjmed.2009.09.037. PMID 20399319. Retrieved 2012-04-26. Unknown parameter
|month=ignored (help) - ↑ Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, Leeper KV, Popovich J, Quinn DA, Sos TA, Sostman HD, Tapson VF, Wakefield TW, Weg JG, Woodard PK (2006). "Multidetector computed tomography for acute pulmonary embolism". The New England Journal of Medicine. 354 (22): 2317–27. doi:10.1056/NEJMoa052367. PMID 16738268. Retrieved 2012-04-26. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 5.2 5.3 5.4 Cohen AT, Dobromirski M, Gurwith MM (2014). "Managing pulmonary embolism from presentation to extended treatment". Thromb Res. 133 (2): 139–48. doi:10.1016/j.thromres.2013.09.040. PMID 24182642.
- ↑ 6.0 6.1 6.2 6.3 6.4 Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P; et al. (2008). "Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC)". Eur Heart J. 29 (18): 2276–315. doi:10.1093/eurheartj/ehn310. PMID 18757870.
- ↑ 7.0 7.1 Anderson FA, Spencer FA (2003). "Risk factors for venous thromboembolism". Circulation. 107 (23 Suppl 1): I9–16. doi:10.1161/01.CIR.0000078469.07362.E6. PMID 12814980.